Establishing a 3-Tesla Magnetic Resonance Imaging Method for Assessing Diffuse Axonal Brain Injury in Rats
Abstract
1. Introduction
2. Results
2.1. Neurological Severity Score
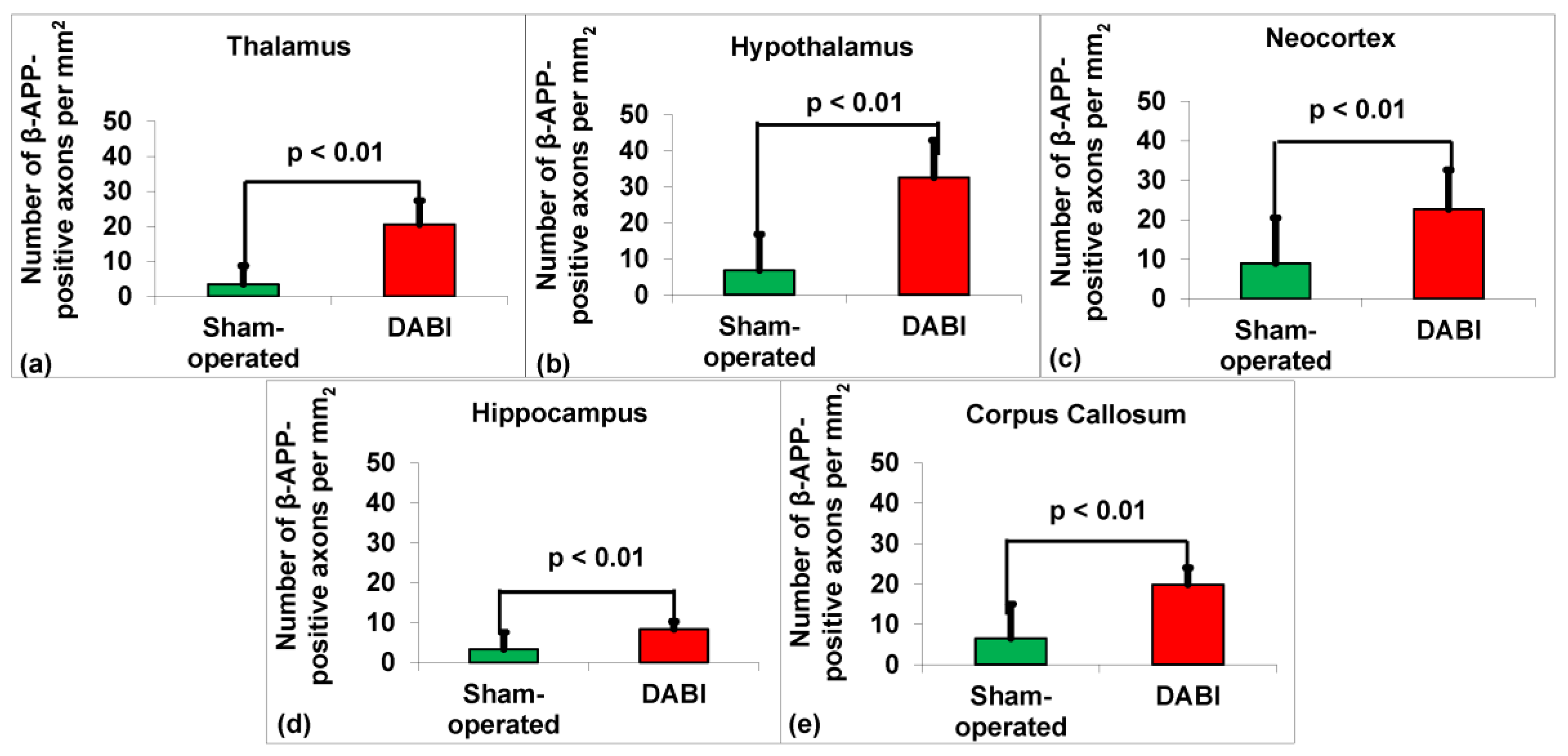
2.2. Analysis of the Immunohistochemistry for β-APP
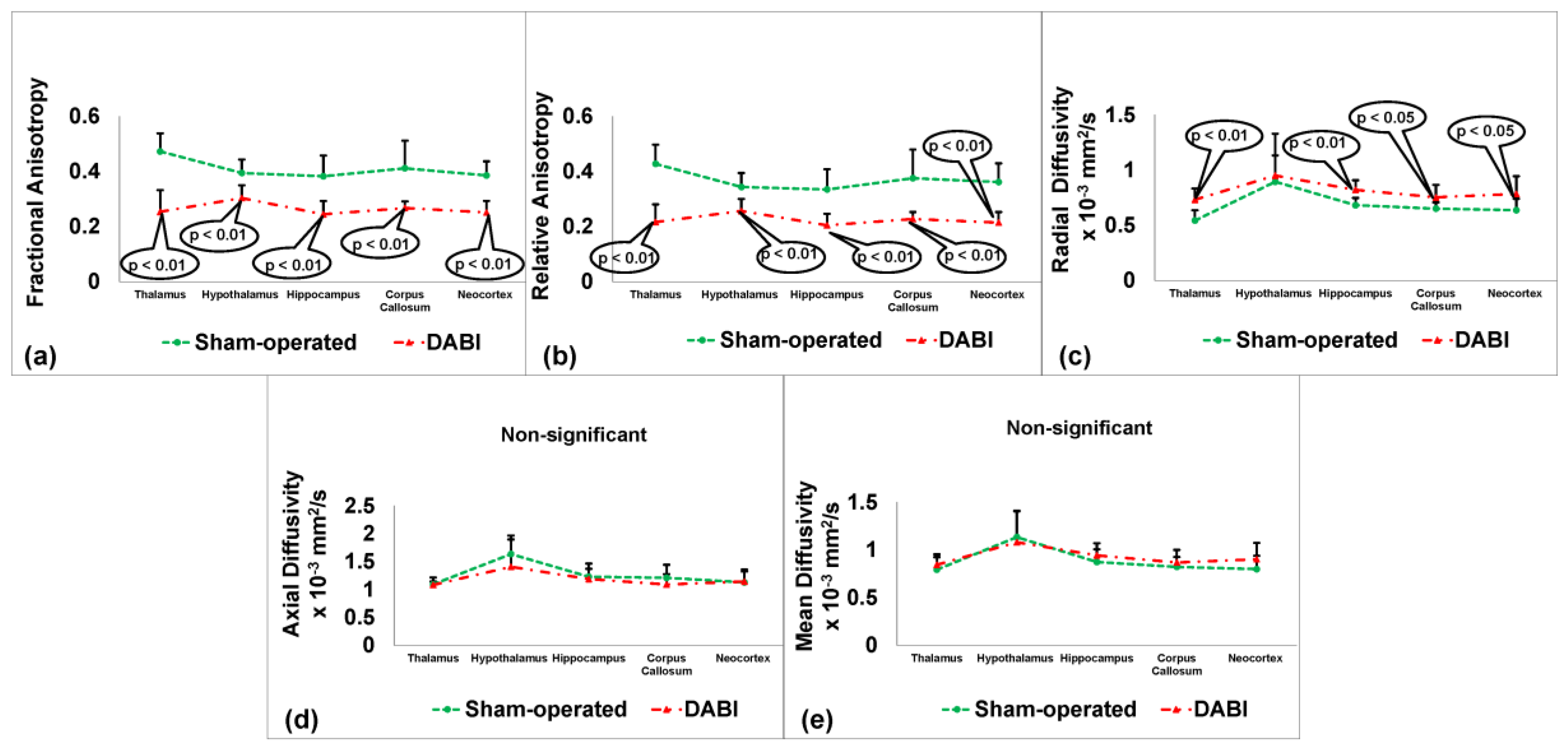
2.3. Analysis of the Neuroimaging Outcomes from MRI
2.4. Correlation Comparisons between the MRI Parameters in the DABI Rats
2.5. Sensitivity Analysis
2.6. Sensitivity Analysis for Different Experimental Models
3. Discussion
4. Materials and Methods
4.1. Animals
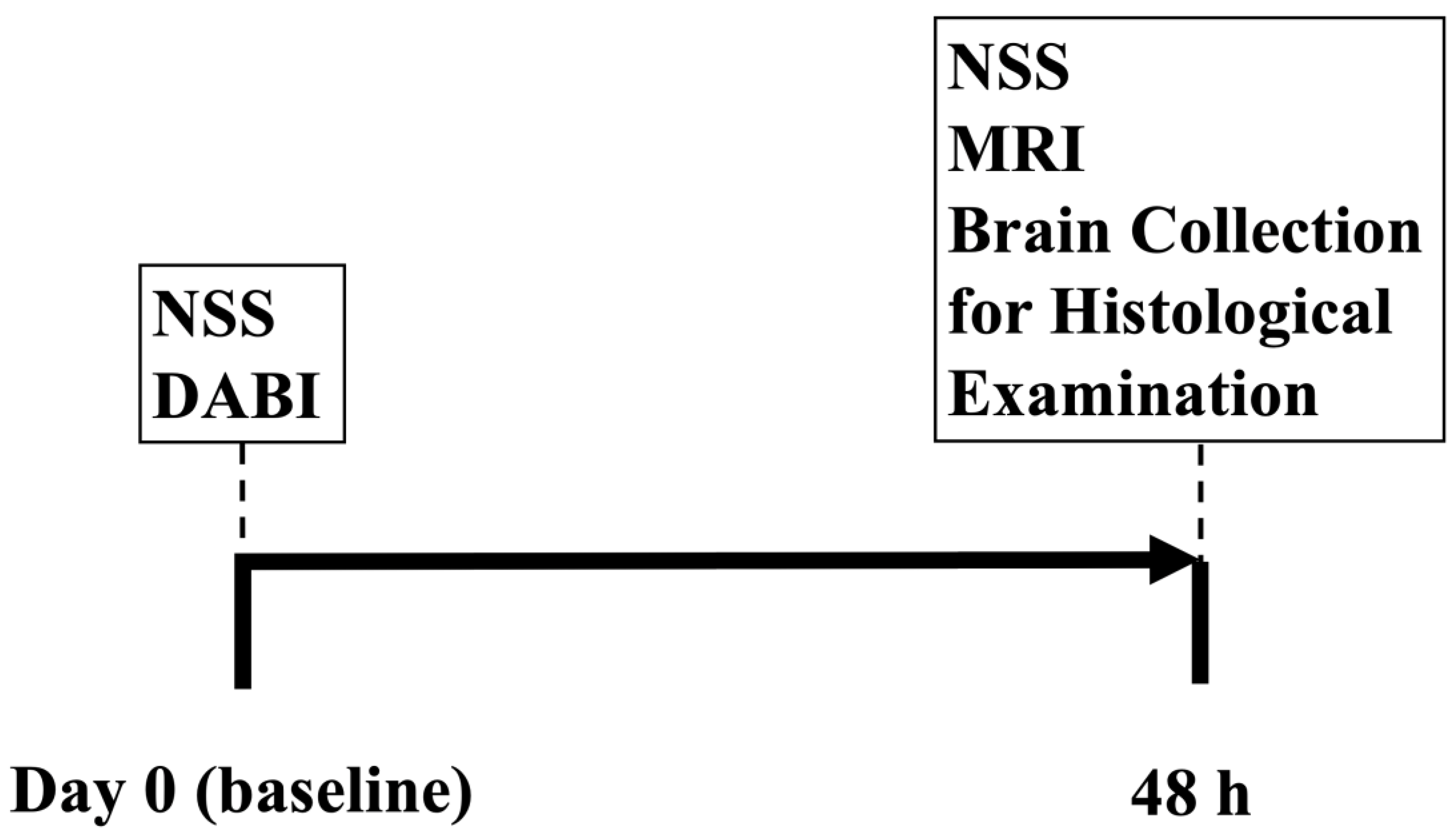
4.2. Experimental Design
4.3. Neurological Severity Score (NSS)
4.4. Induction of Moderate DABI
4.5. Histology
4.6. Diffusion-Weighted Imaging (DWI)
4.7. Regions of Interest (ROI)
4.8. DWI Parameter Map Analysis
4.9. Statistical Analysis
5. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Conflicts of Interest
References
- Roozenbeek, B.; Maas, A.I.; Menon, D.K. Changing patterns in the epidemiology of traumatic brain injury. Nat. Rev. Neurol. 2013, 9, 231. [Google Scholar] [CrossRef] [PubMed]
- Krug, E.G.; Sharma, G.K.; Lozano, R. The global burden of injuries. Am. J. Public Health 2000, 90, 523–526. [Google Scholar] [PubMed]
- Waxweiler, R.J.; Thurman, D.; Sniezek, J.; Sosin, D.; O’Neil, J. Monitoring the impact of traumatic brain injury: A review and update. J. Neurotrauma 1995, 12, 509–516. [Google Scholar] [CrossRef] [PubMed]
- Bruns, J., Jr.; Hauser, W.A. The epidemiology of traumatic brain injury: A review. Epilepsia 2003, 44, 2–10. [Google Scholar] [CrossRef] [PubMed]
- Corrigan, J.D.; Selassie, A.W.; Orman, J.A.L. The epidemiology of traumatic brain injury. J. Head Trauma Rehabil. 2010, 25, 72–80. [Google Scholar] [CrossRef] [PubMed]
- Faul, M.; Coronado, V. Epidemiology of traumatic brain injury. In Handbook of Clinical Neurology; Elsevier: Amsterdam, The Netherlands, 2015; Volume 127, pp. 3–13. [Google Scholar]
- Jennett, B. Epidemiology of head injury. Arch. Dis. Child. 1998, 78, 403–406. [Google Scholar] [CrossRef]
- Langlois, J.A.; Sattin, R.W. Traumatic brain injury in the United States: Research and programs of the Centers for Disease Control and Prevention (CDC)-Preface. J. Head Trauma Rehabil. 2005, 20, 187–188. [Google Scholar] [CrossRef]
- Chung, P.; Khan, F. Traumatic brain injury (TBI): Overview of diagnosis and treatment. J. Neurol. Neurophysiol. 2014, 5, 182–192. [Google Scholar]
- Warden, D.L.; Gordon, B.; McAllister, T.W.; Silver, J.M.; Barth, J.T.; Bruns, J.; Drake, A.; Gentry, T.; Jagoda, A.; Katz, D.I. Guidelines for the pharmacologic treatment of neurobehavioral sequelae of traumatic brain injury. J. Neurotrauma 2006, 23, 1468–1501. [Google Scholar] [CrossRef] [PubMed]
- Smith, D.H.; Meaney, D.F.; Shull, W.H. Diffuse axonal injury in head trauma. J. Head Trauma Rehabil. 2003, 18, 307–316. [Google Scholar] [CrossRef] [PubMed]
- Su, E.; Bell, M. Diffuse axonal injury. Transl. Res. Trauma. Brain Inj. 2016, 57, 41. [Google Scholar]
- Hammoud, D.A.; Wasserman, B.A. Diffuse axonal injuries: Pathophysiology and imaging. Neuroimaging Clin. 2002, 12, 205–216. [Google Scholar] [CrossRef]
- Adams, J.H.; Graham, D.I.; Gennarelli, T.A.; Maxwell, W.L. Diffuse axonal injury in non-missile head injury. J. Neurol. Neurosurg. Psychiatry 1991, 54, 481–483. [Google Scholar] [CrossRef] [PubMed]
- Slazinski, T.; Johnson, M.C. Severe diffuse axonal injury in adults and children. J. Neurosci. Nurs. 1994, 26, 151–154. [Google Scholar] [CrossRef] [PubMed]
- Gentleman, S.M.; Roberts, G.W.; Gennarelli, T.A.; Maxwell, W.L.; Adams, J.H.; Kerr, S.; Graham, D.I. Axonal injury: A universal consequence of fatal closed head injury? Acta Neuropathol. 1995, 89, 537–543. [Google Scholar] [CrossRef] [PubMed]
- He, X.-S.; Yi, S.-Y.; Zhang, X.; Fei, Z.; Zhang, J.-N.; Yang, L.-S. Diffuse axonal injury due to lateral head rotation in a rat model. J. Neurosurg. 2000, 93, 626–633. [Google Scholar] [CrossRef]
- Gennarelli, T.A.; Thibault, L.E.; Adams, J.H.; Graham, D.I.; Thompson, C.J.; Marcincin, R.P. Diffuse axonal injury and traumatic coma in the primate. Ann. Neurol. 1982, 12, 564–574. [Google Scholar] [CrossRef] [PubMed]
- Xiaoshengi, H.; Guitao, Y.; Xiang, Z.; Zhou, F. A morphological study of diffuse axonal injury in a rat model by lateral head rotation trauma. Acta Neurol. Belg. 2010, 110, 49–56. [Google Scholar]
- Ross, D.T.; Meaney, D.F.; Sabol, M.K.; Smith, D.H.; Gennarelli, T.A. Distribution of forebrain diffuse axonal injury following inertial closed head injury in miniature swine. Exp. Neurol. 1994, 126, 291–299. [Google Scholar] [CrossRef] [PubMed]
- Pillai, D.R.; Heidemann, R.M.; Kumar, P.; Shanbhag, N.; Lanz, T.; Dittmar, M.S.; Sandner, B.; Beier, C.P.; Weidner, N.; Greenlee, M.W. Comprehensive small animal imaging strategies on a clinical 3 T dedicated head MR-scanner; adapted methods and sequence protocols in CNS pathologies. PLoS ONE 2011, 6, e16091. [Google Scholar] [CrossRef] [PubMed]
- Frank, D.; Gruenbaum, B.F.; Shelef, I.; Zvenigorodsky, V.; Benjamin, Y.; Shapoval, O.; Gal, R.; Zlotnik, A.; Melamed, I.; Boyko, M. A novel histological technique to assess severity of traumatic brain injury in rodents: Comparisons to neuroimaging and neurological outcomes. Front. Neurosci. 2021, 15, 733115. [Google Scholar] [CrossRef] [PubMed]
- Kuts, R.; Frank, D.; Gruenbaum, B.F.; Grinshpun, J.; Melamed, I.; Knyazer, B.; Tarabrin, O.; Zvenigorodsky, V.; Shelef, I.; Zlotnik, A. A novel method for assessing cerebral edema, infarcted zone and blood-brain barrier breakdown in a single post-stroke rodent brain. Front. Neurosci. 2019, 13, 1105. [Google Scholar] [CrossRef] [PubMed]
- Gruenbaum, B.F.; Kutz, R.; Zlotnik, A.; Boyko, M. Blood glutamate scavenging as a novel glutamate-based therapeutic approach for post-stroke depression. Ther. Adv. Psychopharmacol. 2020, 10, 2045125320903951. [Google Scholar] [CrossRef] [PubMed]
- Frank, D.; Gruenbaum, B.F.; Shelef, I.; Zvenigorodsky, V.; Severynovska, O.; Gal, R.; Dubilet, M.; Zlotnik, A.; Kofman, O.; Boyko, M. Blood glutamate scavenging with pyruvate as a novel preventative and therapeutic approach for depressive-like behavior following traumatic brain injury in a rat model. Front. Neurosci. 2022, 16, 832478. [Google Scholar] [CrossRef] [PubMed]
- Boyko, M.; Gruenbaum, B.F.; Shelef, I.; Zvenigorodsky, V.; Severynovska, O.; Binyamin, Y.; Knyazer, B.; Frenkel, A.; Frank, D.; Zlotnik, A. Traumatic brain injury-induced submissive behavior in rats: Link to depression and anxiety. Transl. Psychiatry 2022, 12, 239. [Google Scholar] [CrossRef] [PubMed]
- Frank, D.; Kuts, R.; Tsenter, P.; Gruenbaum, B.F.; Grinshpun, Y.; Zvenigorodsky, V.; Shelef, I.; Natanel, D.; Brotfain, E.; Zlotnik, A. The effect of pyruvate on the development and progression of post-stroke depression: A new therapeutic approach. Neuropharmacology 2019, 155, 173–184. [Google Scholar] [CrossRef] [PubMed]
- Boyko, M.; Zlotnik, A.; Gruenbaum, B.F.; Gruenbaum, S.E.; Ohayon, S.; Kuts, R.; Melamed, I.; Regev, A.; Shapira, Y.; Teichberg, V.I. Pyruvate’s blood glutamate scavenging activity contributes to the spectrum of its neuroprotective mechanisms in a rat model of stroke. Eur. J. Neurosci. 2011, 34, 1432–1441. [Google Scholar] [CrossRef]
- Boyko, M.; Azab, A.N.; Kuts, R.; Gruenbaum, B.F.; Gruenbaum, S.E.; Melamed, I.; Brotfain, E.; Shapira, Y.; Cesnulis, E.; Zlotnik, A. The neuro-behavioral profile in rats after subarachnoid hemorrhage. Brain Res. 2013, 1491, 109–116. [Google Scholar] [CrossRef]
- Boyko, M.; Melamed, I.; Gruenbaum, B.F.; Gruenbaum, S.E.; Ohayon, S.; Leibowitz, A.; Brotfain, E.; Shapira, Y.; Zlotnik, A. The effect of blood glutamate scavengers oxaloacetate and pyruvate on neurological outcome in a rat model of subarachnoid hemorrhage. Neurotherapeutics 2012, 9, 649–657. [Google Scholar] [CrossRef] [PubMed]
- Rostami, E.; Davidsson, J.; Gyorgy, A.; Agoston, D.V.; Risling, M.; Bellander, B.-M. The terminal pathway of the complement system is activated in focal penetrating but not in mild diffuse traumatic brain injury. J. Neurotrauma 2013, 30, 1954–1965. [Google Scholar] [CrossRef]
- Van de Looij, Y.; Mauconduit, F.; Beaumont, M.; Valable, S.; Farion, R.; Francony, G.; Payen, J.F.; Lahrech, H. Diffusion tensor imaging of diffuse axonal injury in a rat brain trauma model. NMR Biomed. 2012, 25, 93–103. [Google Scholar] [CrossRef] [PubMed]
- Li, Y.; Zhang, L.; Kallakuri, S.; Zhou, R.; Cavanaugh, J.M. Quantitative relationship between axonal injury and mechanical response in a rodent head impact acceleration model. J. Neurotrauma 2011, 28, 1767–1782. [Google Scholar] [CrossRef] [PubMed]
- Frank, D.; Melamed, I.; Gruenbaum, B.F.; Grinshpun, J.; Kuts, R.; Shvartsur, R.; Azab, A.N.; Assadi, M.H.; Vinokur, M.; Boyko, M. Induction of diffuse axonal brain injury in rats based on rotational acceleration. JoVE (J. Vis. Exp.) 2020, 159, e61198. [Google Scholar]
- Losurdo, M.; Davidsson, J.; Sköld, M.K. Diffuse axonal injury in the rat brain: Axonal injury and oligodendrocyte activity following rotational injury. Brain Sci. 2020, 10, 229. [Google Scholar] [CrossRef]
- Paxinos, G.; Watson, C. The Rat Brain in Stereotaxic Coordinates: Hard Cover Edition; Elsevier: Amsterdam, The Netherlands, 2006. [Google Scholar]
- Majka, P.; Kublik, E.; Furga, G.; Wójcik, D.K. Common atlas format and 3D brain atlas reconstructor: Infrastructure for constructing 3D brain atlases. Neuroinformatics 2012, 10, 181–197. [Google Scholar] [CrossRef] [PubMed]
- Chen, X.; Chen, Y.; Xu, Y.; Gao, Q.; Shen, Z.; Zheng, W. Microstructural and neurochemical changes in the rat brain after diffuse axonal injury. J. Magn. Reson. Imaging 2019, 49, 1069–1077. [Google Scholar] [CrossRef]
- Mac Donald, C.L.; Dikranian, K.; Bayly, P.; Holtzman, D.; Brody, D. Diffusion tensor imaging reliably detects experimental traumatic axonal injury and indicates approximate time of injury. J. Neurosci. 2007, 27, 11869–11876. [Google Scholar] [CrossRef] [PubMed]
| NSS Values of the Study Groups | ||
|---|---|---|
| Animal Groups | N | Median (Range) |
| Sham-operated | 10 | 0(0–0) |
| DABI | 10 | 1(1–2.5) * |
| MRI | ||||||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|
| Fractional Anisotropy | Radial Diffusivity | |||||||||||
| T | Hy | N | Hi | CC | T | Hy | N | Hi | CC | |||
| MRI | Relative Anisotropy | T | R = 0.97 p < 0.01 | ns | ns | ns | ns | R = 0.87 p < 0.01 | R = 0.67 p < 0.05 | ns | ns | ns |
| Hy | ns | R = 0.99 p < 0.01 | ns | ns | ns | ns | R = 0.73 p < 0.05 | R = 0.65 p < 0.05 | ns | ns | ||
| N | ns | R = 0.72 p < 0.05 | R = 0.98 p < 0.01 | ns | ns | ns | ns | R = 0.78 p < 0.01 | ns | ns | ||
| Hi | ns | ns | ns | R = 0.99 p < 0.01 | ns | ns | ns | ns | ns | ns | ||
| CC | ns | ns | ns | ns | R = 0.93 p < 0.01 | ns | ns | ns | ns | ns | ||
| Radial Diffusivity | T | R = −0.87 p < 0.01 | ns | ns | ns | |||||||
| Hy | R = −0.65 p < 0.05 | R = −0.76 p < 0.01 | ns | ns | ||||||||
| N | ns | R = 0.68 p < 0.05 | R = 0.69 p < 0.05 | ns | ||||||||
| Hi | ns | ns | ns | ns | ||||||||
| CC | ns | ns | ns | ns | ||||||||
| Histological | MRI | NSS | |||
|---|---|---|---|---|---|
| Fractional Anisotropy | Relative Anisotropy | Radial Diffusivity | |||
| Thalamus | n = 6 20.5 ± 6.9 vs. 3.4 ± 5.3 | n = 6 0.25 ± 0.08 vs. 0.47 ± 0.07 | n = 5 0.22 ± 0.06 vs. 0.43 ± 0.07 | n = 8 0.73 ± 0.1 vs. 0.54 ± 0.09 | N = 8 1(1–2.5) vs. 0(0–0) |
| Hypothalamus | N = 6 32.5 ± 10.4 vs. 6.8 ± 10 | N = 10 0.3 ± 0.05 vs. 0.39 ± 0.05 | N = 10 0.26 ± 0.04 vs. 0.34 ± 0.05 | n-s | |
| Neocortex | N = 15 22.6 ± 10 vs. 8.1 ± 11.6 | N = 5 0.25 ± 0.04 vs. 0.39 ± 0.05 | N = 6 0.21 ± 0.04 vs. 0.36 ± 0.07 | N = 24 0.78 ± 0.16 vs. 0.64 ± 0.1 | |
| Hippocampus | N = 13 8.3 ± 2 vs. 3.3 ± 4.3 | N = 8 0.24 ± 0.05 vs. 0.38 ± 0.08 | N = 7 0.2 ± 0.04 vs. 0.33 ± 0.07 | N = 10 0.82 ± 0.09 vs. 0.68 ± 0.07 | |
| Corpus Callosum | N = 9 19.8 ± 4.2 vs. 6.5 ± 8.5 | N = 10 0.27 ± 0.02 vs. 0.41 ± 0.1 | N = 9 0.23 ± 0.03 vs. 0.38 ± 0.1 | N = 21 0.75 ± 0.11 vs. 0.65 ± 0.06 | |
| Calculated Sample Size per Group | N = 6–15 rats per group | N = 5–10 rats per group | N = 5–10 rats per group | N = 8–21 rats per group | N = 8 rats per group |
| Models of Brain Injury in Rats | Histological | MRI | NSS | ||||
|---|---|---|---|---|---|---|---|
| IZ | BE | BBB | ADC | T2 | Ktrans | ||
| Stroke | n = 10; 8.27 ± 5.9% vr. 0.31 ± 0.48% | n = 4; 12.5 ± 2.6% vr. 1.5 ± 2.3% | n = 5; 2352 ng/g ± 671 vs. 85 ng/g ± 26 | n = 6; 5.98 ± 2.1% vr. 0.58 ± 0.3% | n = 10; 3.46 ± 2.1% vr. 0.66 ± 0.3% | n = 15; 2.01 ± 1.5% vr. 0.46 ± 0.3% | n = 4; 3(2–4) vr. 0(0–0) |
| TBI | n = 11; 4.4 ± 2.07% vr. 1 ± 2% | n = 13; 8.8 ± 6.5% vr. 1.3 ± 1.1% | n = 9; 5.0 × 10−7 g ± 2.5 × 10−7g vr. 1.2 × 10−7 g ± 0.5 × 10−7 g | n = 8; 2.63 ± 1.3% vr. 0.4 ± 0.5% | n = 12; 6.1 ± 3.8% vr. 0.7 ± 3.3% | n = 9; 5.8 ± 3.2% vr. 1 ± 0.5% | n = 7; 4(2–6) vr. 0(0–0) |
| SAH | n = 20; 79.32 ± 0.3% vr. 78.95 ± 0.36% | n = 22; 9.7 × 10−7 g ± 8.2 × 10−7 g vr. 3.1 × 10−7 g ± 1.8 × 10−7 g | n = 2; 9(0–10) vr. 0(0–0) | ||||
| DABI | Immunohistochemistry for β-APP in the Thalamus | Fractional anisotropy in the neocortex | Relative anisotropy in the thalamus | Radial diffusivity in the thalamus | n = 8; 1(1–2.5) vs. 0(0–0) | ||
| n = 6; 20.5 ± 6.9% vs. 3.4 ± 5.3% | n = 5; 0.25 ± 0.04% vs. 0.39 ± 0.05% | n = 5; 0.22 ± 0.06% vs. 0.43 ± 0.07% | n = 8; 0.73 ± 0.1% vs. 0.54 ± 0.09% | ||||
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2024 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Frank, D.; Gruenbaum, B.F.; Zvenigorodsky, V.; Shelef, I.; Oleshko, A.; Matalon, F.; Tsafarov, B.; Zlotnik, A.; Frenkel, A.; Boyko, M. Establishing a 3-Tesla Magnetic Resonance Imaging Method for Assessing Diffuse Axonal Brain Injury in Rats. Int. J. Mol. Sci. 2024, 25, 4234. https://doi.org/10.3390/ijms25084234
Frank D, Gruenbaum BF, Zvenigorodsky V, Shelef I, Oleshko A, Matalon F, Tsafarov B, Zlotnik A, Frenkel A, Boyko M. Establishing a 3-Tesla Magnetic Resonance Imaging Method for Assessing Diffuse Axonal Brain Injury in Rats. International Journal of Molecular Sciences. 2024; 25(8):4234. https://doi.org/10.3390/ijms25084234
Chicago/Turabian StyleFrank, Dmitry, Benjamin F. Gruenbaum, Vladislav Zvenigorodsky, Ilan Shelef, Anna Oleshko, Frederic Matalon, Beatris Tsafarov, Alexander Zlotnik, Amit Frenkel, and Matthew Boyko. 2024. "Establishing a 3-Tesla Magnetic Resonance Imaging Method for Assessing Diffuse Axonal Brain Injury in Rats" International Journal of Molecular Sciences 25, no. 8: 4234. https://doi.org/10.3390/ijms25084234
APA StyleFrank, D., Gruenbaum, B. F., Zvenigorodsky, V., Shelef, I., Oleshko, A., Matalon, F., Tsafarov, B., Zlotnik, A., Frenkel, A., & Boyko, M. (2024). Establishing a 3-Tesla Magnetic Resonance Imaging Method for Assessing Diffuse Axonal Brain Injury in Rats. International Journal of Molecular Sciences, 25(8), 4234. https://doi.org/10.3390/ijms25084234





