A Comprehensive Review of Home Sleep Monitoring Technologies: Smartphone Apps, Smartwatches, and Smart Mattresses
Abstract
1. Introduction
1.1. Subsection Research Gaps and Questions
- Validation and Standardization: There is a lack of standardized validation methods for assessing the accuracy and reliability of consumer sleep-tracking devices compared to PSG.
- Transparency of Algorithms: The proprietary nature of many consumer-grade sleep-tracking algorithms limits their clinical validation and integration into healthcare systems.
- Integration with Clinical Settings: There is limited research on how consumer sleep technology can be effectively integrated with clinical sleep monitoring to improve diagnosis and treatment. This is due to regulatory challenges, data privacy concerns, and differences in measurement techniques.
- How do consumer sleep technologies compare to PSG in terms of accuracy, reliability, and usability?
- What are the primary limitations and challenges associated with consumer sleep-tracking devices?
- How can AI-driven analysis and sensor technologies enhance the effectiveness of home-based sleep monitoring?
1.2. Research Aim
1.3. Structure of the Paper
- This review paper is structured as follows:
- Section 2: Methodology.
- Section 3: Overview of Traditional Sleep Monitoring Methods—reviews established techniques like PSG and actigraphy, providing a benchmark for evaluating consumer sleep technologies.
- Section 4: Home-Based Sleep Monitoring Technologies—examines the three major categories of consumer sleep monitoring: smartphone apps, smartwatches, and smart mattresses.
- Section 6: Comparison of Consumer Sleep Technologies—compares these devices based on data categories.
- Section 7: Discussion and future advancements in home sleep monitoring technology—identifies ongoing challenges in algorithm validation, data privacy, and interoperability while exploring potential advancements in AI and sensor technologies.
- Section 8: Conclusion—summarizes key findings and provides recommendations for future research and consumer adoption
2. Materials and Methods
2.1. Selection Criteria
- Focus on Sleep Monitoring: Devices must primarily focus on sleep tracking rather than general fitness tracking.
- Availability: Devices must be commercially available on major platforms (iOS, Android, or retail channels) to ensure accessibility.
- Manufacturer Support: Excludes discontinued devices or those lacking English-language documentation.
- Smartphone App Functionality: Apps must function independently; smartwatches and smart mattresses must be integrated solutions.
- Release/Update Since 2015: Devices must be released or actively updated since 2015, reflecting technological improvements in sensor accuracy and AI analysis.
- Clinical Studies/Validation: Preference for devices supported by clinical studies or independent validation.
- AI Integration: Notes devices with AI-driven sleep analysis or integration with health ecosystems.
2.2. Data Collection Methods
- Academic literature (peer-reviewed articles and clinical studies) for scientific validation and effectiveness.
- Manufacturer websites for product specifications, features, and pricing.
- App stores (Google Play, Google LLC, Mountain View, CA, USA and Apple App Store, Apple Inc., Cupertino, CA, USA) and online review platforms for real-world user feedback.
- Industry reports for insights into trends, advancements, and market dynamics.
- A total of 46 smartphone applications, of which 21 met the selection criteria.
- A total of 28 smartwatches, with 16 qualifying for analysis.
- A total of 19 smart mattresses, resulting in 9 selected devices.
2.3. Evaluation and Analytical Approach
2.4. Data Visualization Across Sleep Technologies
2.5. Addressing Bias and Limitations
- Reliance on manufacturer claims: Some performance data were based on company-reported metrics, which may introduce bias.
- Limited access to proprietary algorithms: Many consumer-grade devices use black-box AI models, preventing independent verification of their sleep-stage classification accuracy.
- Demographic variability: Most validation studies focus on adult populations, with limited research on how these technologies perform across different age groups or individuals with sleep disorders.
3. Overview of Traditional Sleep Monitoring Methods
3.1. Polysomnography
3.2. Actigraphy
3.3. Comparison of PSG and Actigraphy
4. Home-Based Sleep Monitoring Technologies
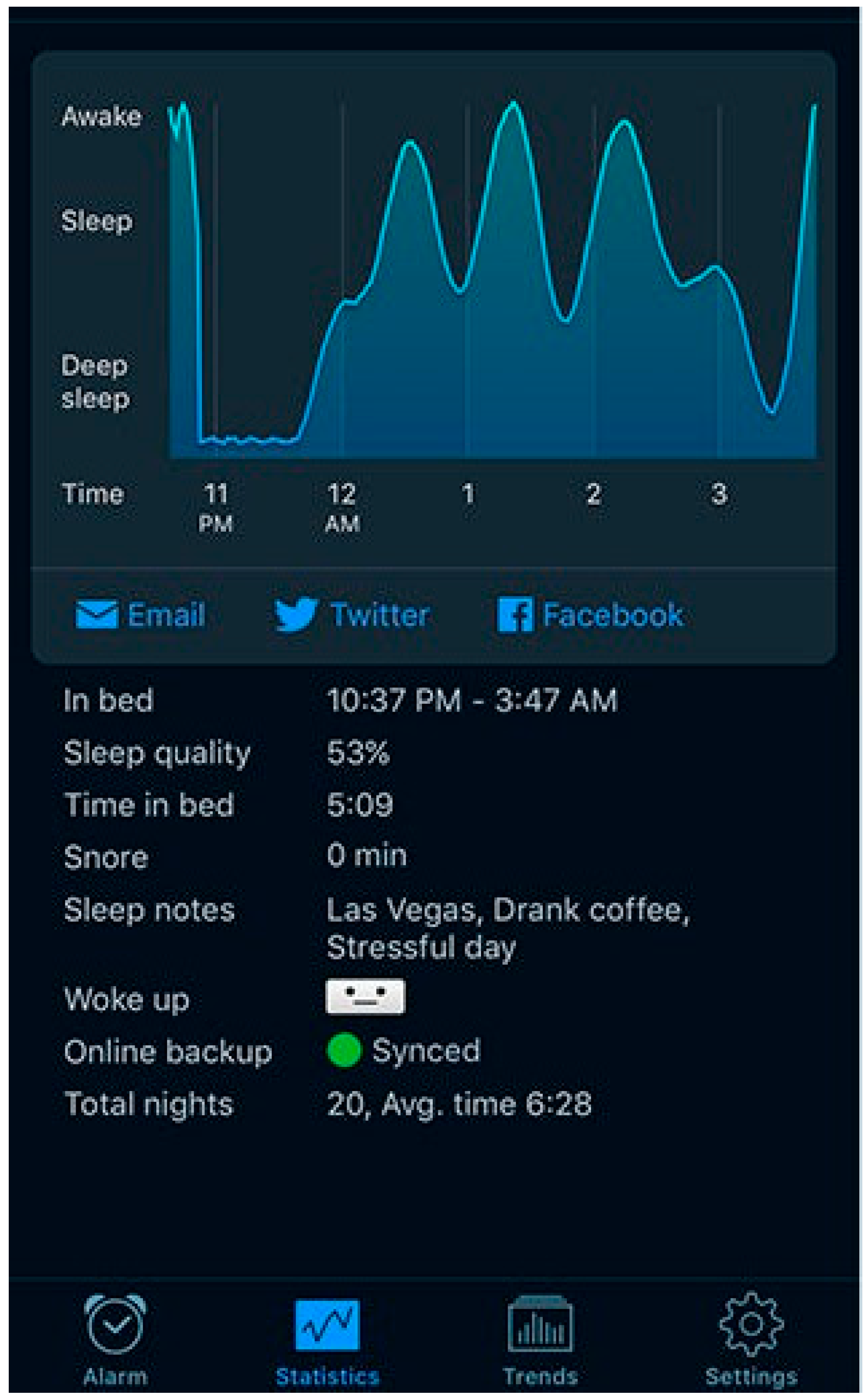
4.1. Sleep Monitoring Using Smartphone Applications
- The app must function independently without requiring external sensors or hardware.
- The app must track core sleep-tracking features including sleep duration, quality, and disturbances, rather than focusing solely on relaxation or meditation.
- The app should be available on either iOS, Android, or both.
- Apps with high user engagement, positive reviews, and substantial download counts.
- Apps with research-backed algorithms or clinical studies were favored whenever possible.
- Only actively maintained and updated apps were included to ensure relevance.
4.1.1. Limitations of Smartphone-Based Sleep Monitoring
4.1.2. Research on Smartphone-Based Sleep Monitoring
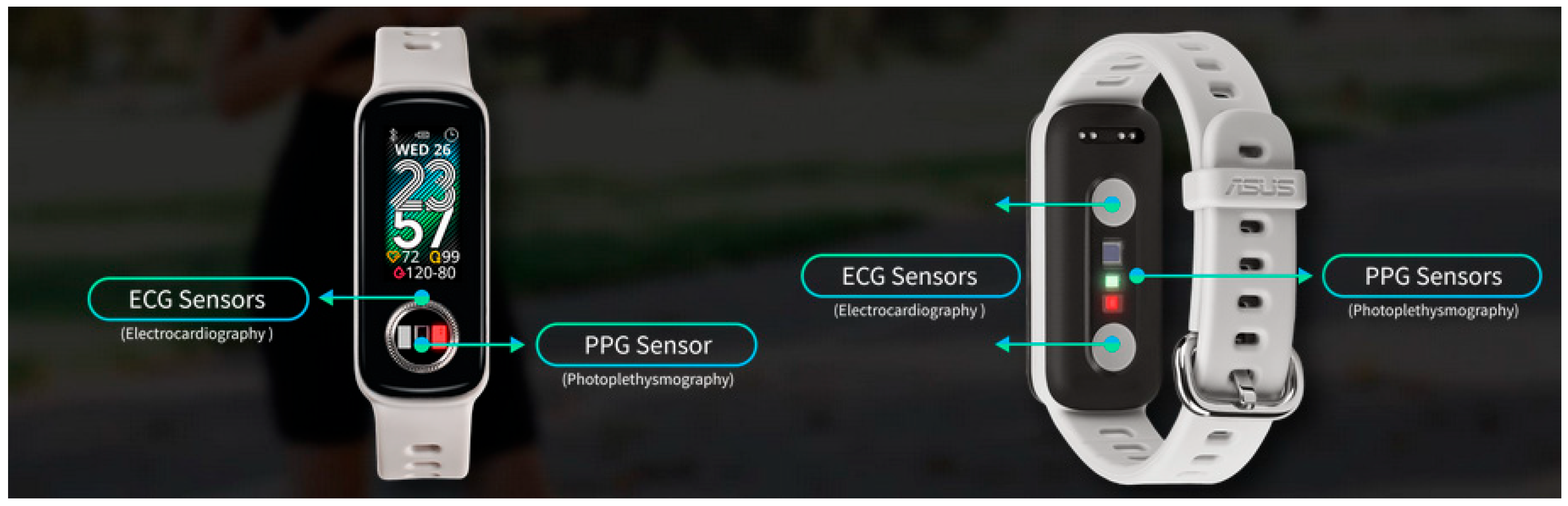
4.2. Sleep Monitoring Using Smartwatches
4.2.1. Selection Criteria for Wearable Devices
4.2.2. Key Features of Wearable Sleep Trackers
4.2.3. Strengths and Limitations of Wearables
4.2.4. Clinical Validation and Research Insights for Wearable Devices
4.3. Sleep Monitoring Using Smart Mattresses
4.3.1. Selection Criteria for Smart Mattresses
- Technological Sophistication—Devices needed to incorporate multi-sensor capabilities, including HR and RR monitoring, sleep-stage detection, and body movement analysis. Preference was given to mattresses featuring AI-driven insights and automatic sleep optimization adjustments.
- Market Availability and User Adoption—Only commercially available smart mattresses with established consumer use were included to ensure practical relevance.
- Integration with Health and Smart Home Ecosystems—Priority was given to devices that sync with mobile apps, wearable devices, or broader health-tracking platforms, enabling seamless data sharing and enhanced sleep management.
- Clinical Validation and Accuracy—Smart mattresses supported by peer-reviewed studies or manufacturer-provided validation reports were favored, while those lacking publicly available validation data were excluded.
4.3.2. Key Features of Smart Mattresses and Under-Mattress Sensors
4.3.3. Strengths and Limitations of Smart Mattresses
4.3.4. Clinical Validation and Research Insights for Smart Mattresses
5. Technology for Different Scenarios
5.1. General Usage
5.2. Individuals with Sleep Disorders
5.3. Athletes and High-Performance Users
5.4. Monitoring Sleep for Mental Health
5.5. Parents Monitoring Children’s Sleep
5.6. Elderly and Accessibility Considerations
5.7. Comparison of Sleep Monitoring Technologies by Scenario
6. Comparison Across Technology Categories
6.1. Cost–Benefit Analysis of Home Sleep Monitoring Devices
6.2. Trade-Offs Between Cost, Accuracy, and User Experience
6.3. Comparing Collected Data Types Across Device Categories
6.4. Applications and Use Cases
- Personalized Sleep Management: Apps like BetterSleep and devices such as Oura Ring provide tailored recommendations to help users improve sleep quality.
- Sleep Disorder Monitoring: Devices like the Sleep Number 360 and Fitbit Charge 6 are valuable for tracking conditions, such as sleep apnea or restless sleep patterns.
- Lifestyle Integration: Smartwatches like the Apple Watch Series 9 and Garmin Venu 3S combine sleep tracking with fitness and overall health monitoring, promoting a balanced lifestyle.
6.5. AI-Based Sleep-Stage Classification
- Smartphone apps primarily use sound and motion data, making their AI models more prone to false detections from external noises and movement.
- Wearables integrate HRV, motion, and respiration signals, allowing AI models to refine sleep-stage detection.
- Smart mattresses use ballistocardiography (BCG), which tracks subtle body movements, but AI models for these systems require calibration to avoid interference from bed sharing and external vibrations.
6.6. Choosing the Right Technology for Different Scenarios
- General Users: Smartphone apps provide a low-cost and accessible solution for those who want basic sleep duration tracking but lack advanced physiological data collection.
- Athletes and Individuals with Sleep Disorders: Wearables (e.g., smartwatches and fitness trackers) provide HRV, respiratory rate, and motion-based sleep staging with higher accuracy than smartphone apps.
- Elderly Individuals or Passive Monitoring Users: Smart mattresses offer an unobtrusive way to track sleep duration and physiological parameters like heart rate and breathing patterns without requiring a wearable device.
- Mental Health Applications: Wearables with HRV-based stress analysis (e.g., Oura Ring, Oura Health Oy, Oulu Finland and WHOOP, Boston, MA, USA) and AI-driven sleep coaching apps (e.g., Sleepio, Big Health, London, UK and Calm, Calm.com, San Francisco, CA, USA) provide valuable insights into the relationship between sleep quality and emotional well-being.
- Parents Monitoring Children’s Sleep: Smart baby monitors (e.g., Nanit, New York, USA and Owlet, Lehi, UT, USA) provide real-time safety alerts and oxygen-level tracking, offering peace of mind.
7. Discussion and Future Advancements in Home Sleep Technology
7.1. Current Strengths and Limitations
7.2. Accuracy and Validation Challenges
7.3. Integration with Healthcare Systems
- Data Accuracy and Standardization: Many consumer devices do not meet the rigorous formatting standards required for clinical decision-making [56].
- Proprietary Algorithms: A lack of transparency prevents healthcare providers from verifying the reliability of these devices [59].
- Regulatory Compliance: Ensuring compliance with HIPAA (U.S.) and GDPR (Europe) remains a significant challenge.
7.4. The Role of AI and Machine Learning
7.5. Emerging Trends and Future Directions
7.6. Data Privacy and Security in Home Sleep Monitoring
7.7. Implications for Users and Researchers
8. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Conflicts of Interest
References
- Zaki, N.F.; Spence, D.W.; Subramanian, P.; Bharti, V.K.; Karthikeyan, R.; BaHammam, A.S.; Pandi-Perumal, S.R. Basic chronobiology: What do sleep physicians need to know? Sleep Sci. 2020, 13, 256–266. [Google Scholar]
- Zielinski, M.R.; McKenna, J.T.; McCarley, R.W. Functions and mechanisms of sleep. AIMS Neurosci. 2016, 3, 67. [Google Scholar] [CrossRef] [PubMed]
- Luyster, F.S.; Strollo, P.J., Jr.; Zee, P.C.; Walsh, J.K. Sleep: A health imperative. Sleep 2012, 35, 727–734. [Google Scholar] [CrossRef] [PubMed]
- Ibáñez, V.; Silva, J.; Cauli, O. A survey on sleep assessment methods. PeerJ 2018, 6, e4849. [Google Scholar] [CrossRef] [PubMed]
- Markun, L.C.; Sampat, A. Clinician-focused overview and developments in polysomnography. Curr. Sleep Med. Rep. 2020, 6, 309–321. [Google Scholar] [CrossRef]
- Van de Water, A.T.; Holmes, A.; Hurley, D.A. Objective measurements of sleep for non-laboratory settings as alternatives to polysomnography–a systematic review. J. Sleep Res. 2011, 20 Pt 2, 183–200. [Google Scholar] [CrossRef]
- Hussain, Z.; Sheng, Q.Z.; Zhang, W.E.; Ortiz, J.; Pouriyeh, S. Non-invasive techniques for monitoring different aspects of sleep: A comprehensive review. ACM Trans. Comput. Healthc. (HEALTH) 2022, 3, 1–26. [Google Scholar] [CrossRef]
- Robbins, R.; Seixas, A.; Walton Masters, L.; Chanko, N.; Diaby, F.; Vieira, D.; Jean-Louis, G. Sleep tracking: A systematic review of the research using commercially available technology. Curr. Sleep Med. Rep. 2019, 5, 156–163. [Google Scholar] [CrossRef]
- Ameen, M.S.; Cheung, L.M.; Hauser, T.; Hahn, M.A.; Schabus, M. About the accuracy and problems of consumer devices in the assessment of sleep. Sensors 2019, 19, 4160. [Google Scholar] [CrossRef]
- Kainec, K.A.; Caccavaro, J.; Barnes, M.; Hoff, C.; Berlin, A.; Spencer, R.M. Evaluating Accuracy in Five Commercial Sleep-Tracking Devices Compared to Research-Grade Actigraphy and Polysomnography. Sensors 2024, 24, 635. [Google Scholar] [CrossRef]
- Kolla, B.P.; Mansukhani, S.; Mansukhani, M.P. Consumer sleep tracking devices: A review of mechanisms, validity and utility. Expert Rev. Med. Devices 2016, 13, 497–506. [Google Scholar] [CrossRef] [PubMed]
- de Zambotti, M.; Cellini, N.; Menghini, L.; Sarlo, M.; Baker, F.C. Sensors capabilities, performance, and use of consumer sleep technology. Sleep Med. Clin. 2020, 15, 1–30. [Google Scholar] [CrossRef] [PubMed]
- Cay, G.; Ravichandran, V.; Sadhu, S.; Zisk, A.H.; Salisbury, A.L.; Solanki, D.; Mankodiya, K. Recent advancement in sleep technologies: A literature review on clinical standards, sensors, apps, and AI methods. IEEE Access 2022, 10, 104737–104756. [Google Scholar] [CrossRef]
- Kwon, S.; Kim, H.; Yeo, W.-H. Recent advances in wearable sensors and portable electronics for sleep monitoring. iScience 2021, 24, 102461. [Google Scholar] [CrossRef]
- Djanian, S.; Bruun, A.; Nielsen, T.D. Sleep classification using Consumer Sleep Technologies and AI: A review of the current landscape. Sleep Med. 2022, 100, 390–403. [Google Scholar] [CrossRef]
- Kazemi, K.; Abiri, A.; Zhou, Y.; Rahmani, A.; Khayat, R.N.; Liljeberg, P.; Khine, M. Improved sleep stage predictions by deep learning of photoplethysmogram and respiration patterns. Comput. Biol. Med. 2024, 179, 108679. [Google Scholar] [CrossRef]
- Bianchi, M.T. Sleep devices: Wearables and nearables, informational and interventional, consumer and clinical. Metabolism 2018, 84, 99–108. [Google Scholar] [CrossRef]
- Menghini, L.; Cellini, N.; Goldstone, A.; Baker, F.C.; de Zambotti, M. A standardized framework for testing the performance of sleep-tracking technology: Step-by-step guidelines and open-source code. Sleep 2021, 44, zsaa170. [Google Scholar] [CrossRef]
- Kim, D.; Chen, H.; Lee, J.; An, Y.; Chang, H.H.; Kim, S.; Park, J.; Yang, S.; Bae, H.; Joo, E. Multi-sensor fusion approach for sleep stage analysis: A non-contact sensor study. Sleep 2024, 47, A481. [Google Scholar] [CrossRef]
- Caroppo, A.; Leone, A.; Rescio, G.; Diraco, G.; Siciliano, P. Sleep Disorder Evaluation Using Ambient and Wearable Sensor Technologies. In Proceedings of the Artificial Intelligence for Ambient Assisted Living 2016 Co-Located with 15th International Conference of the Italian Association for Artificial Intelligence (AIxIA 2016), Genova, Italy, 28 November 2016. [Google Scholar]
- Jun, W.-H.; Kim, H.-J.; Hong, Y.-S. Sleep pattern analysis in unconstrained and unconscious state. Sensors 2022, 22, 9296. [Google Scholar] [CrossRef]
- Katz, O.; Talmon, R.; Lo, Y.-L.; Wu, H.-T. Diffusion-based nonlinear filtering for multimodal data fusion with application to sleep stage assessment. arXiv 2017, arXiv:1701.03619. [Google Scholar]
- Mohamed, M.; Mohamed, N.; Kim, J.G. Advancements in Wearable EEG Technology for Improved Home-Based Sleep Monitoring and Assessment: A Review. Biosensors 2023, 13, 1019. [Google Scholar] [CrossRef] [PubMed]
- Ancoli-Israel, S.; Cole, R.; Alessi, C.; Chambers, M.; Moorcroft, W.; Pollak, C.P. The role of actigraphy in the study of sleep and circadian rhythms. Sleep 2003, 26, 342–392. [Google Scholar] [CrossRef] [PubMed]
- Tahmasian, M.; Khazaie, H.; Sepehry, A.A.; Russo, M.B. Ambulatory monitoring of sleep disorders. JPMA. J. Pak. Med. Assoc. 2010, 60, 480–487. [Google Scholar]
- Acker, J.G.; Becker-Carus, C.; Büttner-Teleaga, A.; Cassel, W.; Danker-Hopfe, H.; Dück, A.; Frohn, C.; Hein, H.; Penzel, T.; Rodenbeck, A. The role of actigraphy in sleep medicine. Somnologie 2021, 25, 89–98. [Google Scholar] [CrossRef]
- Kweon, Y.-S.; Shin, G.-H.; Kwak, H.-G.; Jo, H.-N. Multi-Signal Reconstruction Using Masked Autoencoder From EEG During Polysomnography. In Proceedings of the 2024 12th International Winter Conference on Brain-Computer Interface (BCI), Gangwon, Republic of Korea, 26–28 February 2024. [Google Scholar]
- Yin, J.; Xu, J.; Ren, T.-L. Recent progress in long-term sleep monitoring technology. Biosensors 2023, 13, 395. [Google Scholar] [CrossRef]
- Behar, J.; Roebuck, A.; Domingos, J.S.; Gederi, E.; Clifford, G.D. A review of current sleep screening applications for smartphones. Physiol. Meas. 2013, 34, R29. [Google Scholar] [CrossRef]
- Ong, A.A.; Gillespie, M.B. Overview of smartphone applications for sleep analysis. World J. Otorhinolaryngol.-Head Neck Surg. 2016, 2, 45–49. [Google Scholar] [CrossRef]
- Domingues, A. Smartphone based monitoring system for long-term sleep assessment. In Mobile Health Technologies: Methods and Protocols; Humana Press: New York, NY, USA, 2015; pp. 391–403. [Google Scholar]
- Hao, T.; Xing, G.; Zhou, G. iSleep: Unobtrusive sleep quality monitoring using smartphones. In Proceedings of the 11th ACM Conference on Embedded Networked Sensor Systems, Roma, Italy, 11–15 November 2013. [Google Scholar]
- The Best Sleep-Tracking App. Available online: https://www.nytimes.com/wirecutter/reviews/best-sleep-tracking-app/ (accessed on 7 December 2024).
- Sleep Cycle. Available online: https://www.sleepcycle.com/how-sleep-cycle-works/#:~:text=Why%20users%20love%20and%20trust,Never%20groggy%20anymore.%E2%80%9D (accessed on 7 December 2024).
- Sleep Score. Available online: https://www.sleepscore.com/ (accessed on 7 December 2024).
- Sleep Monitor. Available online: https://play.google.com/store/apps/details?id=com.sleepmonitor.aio&hl=en (accessed on 7 December 2024).
- Sleep as Android. Available online: https://sleep.urbandroid.org/ (accessed on 9 December 2024).
- Snore Recorder. Available online: https://apps.apple.com/us/app/snore-recorder-my-sleep-lab/id1570823441 (accessed on 7 December 2024).
- ShutEye. Available online: https://shuteye.ai/ (accessed on 7 November 2024).
- Pillow. Available online: https://pillow.app/ (accessed on 9 November 2024).
- Sleepbot: Sleep Tracker. Available online: https://apps.apple.com/us/app/sleepbot-sleep-tracker/id1202824148 (accessed on 7 December 2024).
- Sleep Tracker: Recorder, Sound. Available online: https://apps.apple.com/us/app/sleep-tracker-recorder-sound/id1551928101 (accessed on 8 December 2024).
- SnoreLab. Available online: https://www.snorelab.com/ (accessed on 13 November 2024).
- NapBot—Auto Sleep Tracker. Available online: https://apps.apple.com/us/app/napbot-auto-sleep-tracker/id1476436116 (accessed on 7 November 2024).
- Sleep Details. Available online: https://sleepdetails.com/ (accessed on 12 November 2024).
- Apple Health. Available online: https://apps.apple.com/us/app/apple-health/id1242545199 (accessed on 7 December 2024).
- Sleepia: Smart Sleep Tracker. Available online: https://apps.apple.com/us/app/sleepia-smart-sleep-tracker/id6449482091 (accessed on 7 December 2024).
- Mintal. Available online: https://mintal.com/blog/mintal-tracker-helps-you-get-the-best-sleep/ (accessed on 7 December 2024).
- Alarmy-Alarm Clock & Sleep. Available online: https://play.google.com/store/apps/details?id=droom.sleepIfUCan&hl=en (accessed on 7 December 2024).
- Sleep Time-Alarm Calculator. Available online: https://play.google.com/store/apps/details?id=ru.olegfilimonov.sleeptime&hl=en (accessed on 7 December 2024).
- Sleep solutions. Available online: https://www.sleepsolutions.com.au/sleepace-sleep-dot-mini-sleep-tracker (accessed on 7 December 2024).
- RISE: Sleep Tracker. Available online: https://apps.apple.com/us/app/rise-sleep-tracker/id1453884781 (accessed on 7 December 2024).
- Sleepzy-Sleep Cycle Tracker. Available online: https://apps.apple.com/us/app/sleepzy-sleep-cycle-tracker/id1064910141 (accessed on 7 December 2024).
- SlumberCycle+: Sleep Tracker. Available online: https://play.google.com/store/apps/details?id=com.appsky.slumbercycle.sleeptracker&hl=en (accessed on 7 December 2024).
- Fino, E.; Plazzi, G.; Filardi, M.; Marzocchi, M.; Pizza, F.; Vandi, S.; Mazzetti, M. (Not so) Smart sleep tracking through the phone: Findings from a polysomnography study testing the reliability of four sleep applications. J. Sleep Res. 2020, 29, e12935. [Google Scholar] [CrossRef]
- Kim, K.B.; Baek, H.J. Photoplethysmography in wearable devices: A comprehensive review of technological advances, current challenges, and future directions. Electronics 2023, 12, 2923. [Google Scholar] [CrossRef]
- Choi, Y.K.; Demiris, G.; Lin, S.-Y.; Iribarren, S.J.; Landis, C.A.; Thompson, H.J.; McCurry, S.M.; Heitkemper, M.M.; Ward, T.M. Smartphone applications to support sleep self-management: Review and evaluation. J. Clin. Sleep Med. 2018, 14, 1783–1790. [Google Scholar] [CrossRef] [PubMed]
- Sommer, J.U.; Lindner, L.; Kent, D.T.; Heiser, C. Evaluation of an OSA Risk Screening Smartphone App in a General, Non-Symptomatic Population Sample (ESOSA). J. Clin. Med. 2024, 13, 4664. [Google Scholar] [CrossRef]
- Bhat, S.; Ferraris, A.; Gupta, D.; Mozafarian, M.; DeBari, V.A.; Gushway-Henry, N.; Gowda, S.P.; Polos, P.G.; Rubinstein, M.; Seidu, H. Is there a clinical role for smartphone sleep apps? Comparison of sleep cycle detection by a smartphone application to polysomnography. J. Clin. Sleep Med. 2015, 11, 709–715. [Google Scholar] [CrossRef]
- Rentz, L.E.; Ulman, H.K.; Galster, S.M. Deconstructing commercial wearable technology: Contributions toward accurate and free-living monitoring of sleep. Sensors 2021, 21, 5071. [Google Scholar] [CrossRef] [PubMed]
- Phan, D.; Siong, L.Y.; Pathirana, P.N.; Seneviratne, A. Smartwatch: Performance evaluation for long-term heart rate monitoring. In Proceedings of the 2015 International Symposium on Bioelectronics and Bioinformatics (ISBB), Beijing, China, 14–17 October 2015; pp. 144–147. [Google Scholar]
- Pombo, N.; Garcia, N.M. ubiSleep: An ubiquitous sensor system for sleep monitoring. In Proceedings of the 2016 IEEE 12th International Conference on Wireless and Mobile Computing, Networking and Communications (WiMob), New York, NY, USA, 17–19 October 2016; pp. 1–4. [Google Scholar]
- Birrer, V.; Elgendi, M.; Lambercy, O.; Menon, C. Evaluating reliability in wearable devices for sleep staging. NPJ Digit. Med. 2024, 7, 74. [Google Scholar] [CrossRef] [PubMed]
- ASUS VivoWatch 5 Aero Plus. Available online: https://www.asus.com/tw/mobile-handhelds/wearable-healthcare/asus-vivowatch/vivowatch-5-aero-plus/ (accessed on 10 October 2024).
- Apple Watch Ultra 2. Available online: https://www.apple.com/apple-watch-ultra-2/#:~:text=Ultra%202%20can%20now%20monitor%20breathing%20disturbances,you%20need%20for%20better%20rest%20and%20recovery (accessed on 10 September 2024).
- Apple Watch Series 9-Technical Specifications. Available online: https://support.apple.com/en-nz/111833 (accessed on 12 October 2024).
- Sumsung. Available online: https://www.samsung.com/us/watches/galaxy-watch7/?CID=afl-ecomm-rkt-cha-040122-url_Skimlinks.com&utm_source=url_Skimlinks.com&utm_medium=affiliate&utm_campaign=1&utm_content=2116208&rktevent=Skimlinks.com_TnL5HPStwNw-rsPVmRtFzJKlmqAJMlnaTQ&ranMID=47773&ranEAID=TnL5HPStwNw&ranSiteID=TnL5HPStwNw-rsPVmRtFzJKlmqAJMlnaTQ (accessed on 20 October 2024).
- Fitbit Sense 2 Smartwatch. Available online: https://store.google.com/nz/product/fitbit_sense_2?hl=en-GB (accessed on 20 October 2024).
- Garmin. Available online: https://www.garmin.com.tw/minisite/vivo/venu-3/?utm_term=garmin%20venu%203s&utm_content=675239496425&gad_source=1&gclid=Cj0KCQiAlsy5BhDeARIsABRc6ZslntfFbr4XUcetBi9ViIsHuIEL6OnQ7e6mHpjkZBGeJE7U69_P9pcaAg2YEALw_wcB (accessed on 10 October 2024).
- Garmin. Available online: https://www.garmin.com/en-NZ/p/866191 (accessed on 10 October 2024).
- Withings. Available online: https://www.withings.com/eu/en/scanwatch-2 (accessed on 10 October 2024).
- Pixel Watch 3. Available online: https://store.google.com/tw/product/pixel_watch_3?hl=zh-TW (accessed on 10 October 2024).
- Huawei. Available online: https://consumer.huawei.com/nz/support/content/en-us15759715/#:~:text=Customizing%20sleep%20settings,touch%20it%20and%20then%20Delete (accessed on 20 October 2024).
- Polar. Available online: https://www.polar.com/en/ignite3?srsltid=AfmBOopmV6k78xS0ACdzfb1ONzArvS82sg6MRXN0I10WgMdYrRI1NcPz (accessed on 10 October 2024).
- Amazfit. Available online: https://tw.amazfit.com/products/amazfit-bip5-unity (accessed on 10 October 2024).
- Suunto. Available online: https://www.suunto.com/Products/sports-watches/suunto-9-peak-pro/suunto-9-peak-pro-all-black/ (accessed on 10 October 2024).
- ASUS VivoWatch 5 (HC-B05). Available online: https://www.asus.com/nz/mobile-handhelds/wearable-healthcare/asus-vivowatch/asus-vivowatch-5-hc-b05/#water-resistant-to-50-meters/ (accessed on 10 September 2024).
- OPPO Watch. Available online: https://www.oppo.com/nz/accessories/watch/convenience/ (accessed on 15 October 2024).
- Xiaomi Mi Watch Sport. Available online: https://www.mi.com/tw/product/mi-watch/ (accessed on 5 October 2024).
- Maimo. Available online: https://www.maimo.co/maimoWatch/ (accessed on 10 October 2024).
- Kim, D.; Joo, E.Y.; Choi, S.J. Validation of the Samsung Smartwatch for Sleep–Wake Determination and Sleep Stage Estimation. J. Sleep Med. 2023, 20, 28–34. [Google Scholar] [CrossRef]
- Li, L.; Yang, C.; Wang, Z.; Xiao, K.; Min, R. Stretchable polymer optical fiber embedded in the mattress for respiratory and heart rate monitoring. Opt. Laser Technol. 2024, 171, 110356. [Google Scholar] [CrossRef]
- Bandyopadhyay, A.; Oks, M.; Sun, H.; Prasad, B.; Rusk, S.; Jefferson, F.; Malkani, R.G.; Haghayegh, S.; Sachdeva, R.; Hwang, D. Strengths, weaknesses, opportunities, and threats of using AI-enabled technology in sleep medicine: A commentary. J. Clin. Sleep Med. 2024, 20, 1183–1191. [Google Scholar] [CrossRef]
- Paalasmaa, J.; Waris, M.; Toivonen, H.; Leppäkorpi, L.; Partinen, M. Unobtrusive online monitoring of sleep at home. In Proceedings of the 2012 Annual International Conference of the IEEE Engineering in Medicine and Biology Society, San Diego, CA, USA, 28 August–1 September 2012; pp. 3784–3788. [Google Scholar]
- Sleep8. Available online: https://sleep8.uk/products/isense-hybrid-premier-mattress (accessed on 11 October 2024).
- Sleep Number. Available online: https://www.sleepnumber.com/products/climate360 (accessed on 5 November 2024).
- ReST. Available online: https://restperformance.com/ (accessed on 9 November 2024).
- Withings Sleep Analyzer. Available online: https://www.withings.com/eu/en/sleep-analyzer?srsltid=AfmBOoqAowFb4zhDFP-dtICb0Ewzt2fUXzucsu8jLuvdjwbmx6J6GG0R (accessed on 12 November 2024).
- Tempur-Pedic. Available online: https://www.tempurpedic.com/shop-mattresses/breeze-collection/v/3934/ (accessed on 9 November 2024).
- Bryte. Available online: https://www.bryte.com/shop-bryte-balance (accessed on 15 September 2024).
- Bai, D.; Ho, M.-C.; Mathunjwa, B.M.; Hsu, Y.-L. Deriving Multiple-Layer Information from a Motion-Sensing Mattress for Precision Care. Sensors 2023, 23, 1736. [Google Scholar] [CrossRef]
- NordicTrack. Available online: https://www.appliancesonline.com.au/andoo/product/nordictrack-ntsmata219-queen-sleep-mattress/ (accessed on 5 November 2024).
- ERA, the New Dawn of Sleep. Available online: https://www.ces.tech/ces-innovation-awards/2025/era-the-new-dawn-of-sleep/?utm_source=chatgpt.com (accessed on 5 November 2024).
- Tal, A.; Shinar, Z.; Shaki, D.; Codish, S.; Goldbart, A. Validation of contact-free sleep monitoring device with comparison to polysomnography. J. Clin. Sleep Med. 2017, 13, 517–522. [Google Scholar] [CrossRef]
- Jaworski, D.J.; Park, A.; Park, E.J. Internet of things for sleep monitoring. IEEE Instrum. Meas. Mag. 2021, 24, 30–36. [Google Scholar] [CrossRef]
- Walsh, L.; McLoone, S. Non-contact under-mattress sleep monitoring. J. Ambient Intell. Smart Environ. 2014, 6, 385–401. [Google Scholar] [CrossRef]
- Hirshkowitz, M.; Whiton, K.; Albert, S.M.; Alessi, C.; Bruni, O.; DonCarlos, L.; Hazen, N.; Herman, J.; Hillard, P.J.A.; Katz, E.S. National Sleep Foundation’s updated sleep duration recommendations. Sleep Health 2015, 1, 233–243. [Google Scholar] [CrossRef]
- Desjardins, S.; Lapierre, S.; Hudon, C.; Desgagné, A. Factors involved in sleep efficiency: A population-based study of community-dwelling elderly persons. Sleep 2019, 42, zsz038. [Google Scholar] [CrossRef] [PubMed]
- Hoopes, E.K.; D’Agata, M.N.; Berube, F.R.; Ranadive, S.M.; Patterson, F.; Farquhar, W.B.; Edwards, D.G.; Witman, M.A. Consistency where it counts: Sleep regularity is associated with circulating white blood cell count in young adults. Brain Behav. Immun.-Health 2021, 13, 100233. [Google Scholar] [CrossRef]
- Epstein, L.J. Sleep disorders: Types and approach to evaluation. In Sleep, Health, and Society: From Aetiology to Public Health; Oxford University Press: Oxford, UK, 2018; Volume 54. [Google Scholar]
- e Cruz, M.M.; Kryger, M.H.; Morin, C.M.; Palombini, L.; Salles, C.; Gozal, D. Comorbid insomnia and sleep apnea: Mechanisms and implications of an underrecognized and misinterpreted sleep disorder. Sleep Med. 2021, 84, 283–288. [Google Scholar] [CrossRef]
- Humer, E.; Pieh, C.; Brandmayr, G. Metabolomics in sleep, insomnia and sleep apnea. Int. J. Mol. Sci. 2020, 21, 7244. [Google Scholar] [CrossRef]
- Alexander, M.; Ray, M.A.; Hébert, J.R.; Youngstedt, S.D.; Zhang, H.; Steck, S.E.; Bogan, R.K.; Burch, J.B. The national veteran sleep disorder study: Descriptive epidemiology and secular trends, 2000–2010. Sleep 2016, 39, 1399–1410. [Google Scholar] [CrossRef]
- Watson, A.M. Sleep and athletic performance. Curr. Sports Med. Rep. 2017, 16, 413–418. [Google Scholar] [CrossRef]
- Knufinke, M.; Nieuwenhuys, A.; Geurts, S.A.; Møst, E.I.; Maase, K.; Moen, M.H.; Coenen, A.M.; Kompier, M.A. Train hard, sleep well? Perceived training load, sleep quantity and sleep stage distribution in elite level athletes. J. Sci. Med. Sport 2018, 21, 427–432. [Google Scholar] [CrossRef]
- Costa, J.; Figueiredo, P.; Nakamura, F.Y.; Brito, J. The Importance of sleep in athletes. In Exercise Physiology; IntechOpen: London, UK, 2022. [Google Scholar]
- Driller, M.W.; Dunican, I.C.; Omond, S.E.; Boukhris, O.; Stevenson, S.; Lambing, K.; Bender, A.M. Pyjamas, polysomnography and professional athletes: The role of sleep tracking Technology in Sport. Sports 2023, 11, 14. [Google Scholar] [CrossRef]
- Rosales-Lagarde, A.; Armony, J.L.; del Río-Portilla, Y.; Trejo-Martínez, D.; Conde, R.; Corsi-Cabrera, M. Enhanced emotional reactivity after selective REM sleep deprivation in humans: An fMRI study. Front. Behav. Neurosci. 2012, 6, 25. [Google Scholar] [CrossRef] [PubMed]
- Dong, L.; Xie, Y.; Zou, X. Association between sleep duration and depression in US adults: A cross-sectional study. J. Affect. Disord. 2022, 296, 183–188. [Google Scholar] [CrossRef]
- Augner, C. Associations of subjective sleep quality with depression score, anxiety, physical symptoms and sleep onset latency in young students. Cent. Eur. J. Public Health 2011, 19, 115–117. [Google Scholar] [CrossRef] [PubMed]
- Liu, I.; Ni, S.; Peng, K. Happiness at your fingertips: Assessing mental health with smartphone photoplethysmogram-based heart rate variability analysis. Telemed. E-Health 2020, 26, 1483–1491. [Google Scholar] [CrossRef] [PubMed]
- Werner, G.G.; Ford, B.Q.; Mauss, I.B.; Schabus, M.; Blechert, J.; Wilhelm, F.H. High cardiac vagal control is related to better subjective and objective sleep quality. Biol. Psychol. 2015, 106, 79–85. [Google Scholar] [CrossRef]
- Paruthi, S.; Brooks, L.J.; D’Ambrosio, C.; Hall, W.A.; Kotagal, S.; Lloyd, R.M.; Malow, B.A.; Maski, K.; Nichols, C.; Quan, S.F. Consensus statement of the American Academy of Sleep Medicine on the recommended amount of sleep for healthy children: Methodology and discussion. J. Clin. Sleep Med. 2016, 12, 1549–1561. [Google Scholar] [CrossRef]
- Wu, K. Exploring the role of sleep stages in memory consolidation and cognitive function. Theor. Nat. Sci. 2023, 23, 40–43. [Google Scholar] [CrossRef]
- DelRosso, L.M.; Picchietti, D.L.; Spruyt, K.; Bruni, O.; Garcia-Borreguero, D.; Kotagal, S.; Owens, J.A.; Simakajornboon, N.; Ferri, R.; Group, I.R.L.S.S. Restless sleep in children: A systematic review. Sleep Med. Rev. 2021, 56, 101406. [Google Scholar] [CrossRef]
- Kay, M.; Choe, E.K.; Shepherd, J.; Greenstein, B.; Watson, N.; Consolvo, S.; Kientz, J.A. Lullaby: A capture & access system for understanding the sleep environment. In Proceedings of the 2012 ACM conference on Ubiquitous Computing, Pittsburgh, PA, USA, 5–8 September 2012; pp. 226–234. [Google Scholar]
- Lunsford-Avery, J.R.; Engelhard, M.M.; Navar, A.M.; Kollins, S.H. Validation of the sleep regularity index in older adults and associations with cardiometabolic risk. Sci. Rep. 2018, 8, 14158. [Google Scholar] [CrossRef]
- Qin, S.; Chee, M.W. The Emerging Importance of Sleep Regularity on Cardiovascular Health and Cognitive Impairment in Older Adults: A Review of the Literature. Nat. Sci. Sleep 2024, 16, 585–597. [Google Scholar] [CrossRef] [PubMed]
- Liu, W.; Ploderer, B.; Hoang, T. In bed with technology: Challenges and opportunities for sleep tracking. In Proceedings of the Annual Meeting of the Australian Special Interest Group for Computer Human Interaction, Parkville, Australia, 7–10 December 2015; pp. 142–151. [Google Scholar]
- Markov, K.; Elgendi, M.; Menon, C. EEG-based headset sleep wearable devices. NPJ Biosensing 2024, 1, 12. [Google Scholar] [CrossRef]
- Escobedo Araque, P.; Pousibet, A.; López Ruiz, N.; Carvajal, M.A.; Palma, A.J.; Martínez Olmos, A. Bed-based ballistocardiography system using flexible RFID sensors for non-invasive single- and dual-subject vital signs monitoring. IEEE Trans. Instrum. Meas. 2024, 73, 2002912. [Google Scholar]
- Ko, P.-R.T.; Kientz, J.A.; Choe, E.K.; Kay, M.; Landis, C.A.; Watson, N.F. Consumer sleep technologies: A review of the landscape. J. Clin. Sleep Med. 2015, 11, 1455–1461. [Google Scholar] [CrossRef] [PubMed]
- Cherenshchykova, A.; Miller, A.D. Family-based sleep technologies: Opportunities and challenges. In Proceedings of the Extended Abstracts of the 2019 CHI Conference on Human Factors in Computing Systems, Glasgow, UK, 4–9 May 2019; pp. 1–6. [Google Scholar]
- Ghazi, S.N.; Behrens, A.; Berner, J.; Sanmartin Berglund, J.; Anderberg, P. Objective sleep monitoring at home in older adults: A scoping review. J. Sleep Res. 2024, e14436. [Google Scholar] [CrossRef]
- Alanezi, K.; Mishra, S. Impact of Smartphone Position on Sensor Values and Context Discovery. University of Colorado Boulder. 2013. Available online: https://scholar.colorado.edu/concern/reports/6682x4651 (accessed on 9 March 2025).
- Alanezi, K.; Mishra, S. Design, implementation and evaluation of a smartphone position discovery service for accurate context sensing. Comput. Electr. Eng. 2015, 44, 307–323. [Google Scholar] [CrossRef]
- Moreno-Pino, F.; Porras-Segovia, A.; López-Esteban, P.; Artés, A.; Baca-García, E. Validation of Fitbit Charge 2 and Fitbit Alta HR against polysomnography for assessing sleep in adults with obstructive sleep apnea. J. Clin. Sleep Med. 2019, 15, 1645–1653. [Google Scholar] [CrossRef]
- Lee, X.K.; Chee, N.I.; Ong, J.L.; Teo, T.B.; van Rijn, E.; Lo, J.C.; Chee, M.W. Validation of a consumer sleep wearable device with actigraphy and polysomnography in adolescents across sleep opportunity manipulations. J. Clin. Sleep Med. 2019, 15, 1337–1346. [Google Scholar] [CrossRef]
- Chiang, A.A.; Khosla, S. Consumer wearable sleep trackers: Are they ready for clinical use? Sleep Med. Clin. 2023, 18, 311–330. [Google Scholar] [CrossRef]
- Schutte-Rodin, S.; Deak, M.C.; Khosla, S.; Goldstein, C.A.; Yurcheshen, M.; Chiang, A.; Gault, D.; Kern, J.; O’Hearn, D.; Ryals, S. Evaluating consumer and clinical sleep technologies: An American Academy of Sleep Medicine update. J. Clin. Sleep Med. 2021, 17, 2275–2282. [Google Scholar] [CrossRef]
- Kahawage, P.; Jumabhoy, R.; Hamill, K.; de Zambotti, M.; Drummond, S.P. Validity, potential clinical utility, and comparison of consumer and research-grade activity trackers in Insomnia Disorder I: In-lab validation against polysomnography. J. Sleep Res. 2020, 29, e12931. [Google Scholar] [CrossRef] [PubMed]
- Heneghan, C.; Gillard, R.; Niehaus, L.; Schneider, L.; Guerard, M. 0302 Sleep Staging Classification from Wearable Signals Using Deep Learning. Sleep 2024, 47 (Suppl. S1), A130. [Google Scholar] [CrossRef]
- Habib, A.; Motin, M.A.; Penzel, T.; Palaniswami, M.; Yearwood, J.; Karmakar, C. Performance of a convolutional neural network derived from PPG signal in classifying sleep stages. IEEE Trans. Biomed. Eng. 2022, 70, 1717–1728. [Google Scholar] [CrossRef] [PubMed]
- Olsen, M.; Zeitzer, J.M.; Richardson, R.N.; Davidenko, P.; Jennum, P.J.; Sørensen, H.B.; Mignot, E. A flexible deep learning architecture for temporal sleep stage classification using accelerometry and photoplethysmography. IEEE Trans. Biomed. Eng. 2022, 70, 228–237. [Google Scholar] [CrossRef]
- Gerke, S.; Shachar, C.; Chai, P.R.; Cohen, I.G. Regulatory, safety, and privacy concerns of home monitoring technologies during COVID-19. Nat. Med. 2020, 26, 1176–1182. [Google Scholar] [CrossRef] [PubMed]
- Müller, R.; Kuhn, E.; Ranisch, R.; Hunger, J.; Primc, N. Ethics of sleep tracking: Techno-ethical particularities of consumer-led sleep-tracking with a focus on medicalization, vulnerability, and relationality. Ethics Inf. Technol. 2023, 25, 4. [Google Scholar] [CrossRef]
- Tuovinen, L.; Smeaton, A.F. Unlocking the black box of wearable intelligence: Ethical considerations and social impact. In Proceedings of the 2019 IEEE Congress on Evolutionary Computation (CEC), Wellington, New Zealand, 10–13 June 2019; pp. 3235–3243. [Google Scholar]
- Watson, N.F.; Fernandez, C.R. Artificial intelligence and sleep: Advancing sleep medicine. Sleep Med. Rev. 2021, 59, 101512. [Google Scholar] [CrossRef]
- Alattar, M.; Govind, A.; Mainali, S. Artificial intelligence models for the automation of standard diagnostics in sleep medicine—A systematic review. Bioengineering 2024, 11, 206. [Google Scholar] [CrossRef]
- Bandyopadhyay, A.; Goldstein, C. Clinical applications of artificial intelligence in sleep medicine: A sleep clinician’s perspective. Sleep Breath. 2023, 27, 39–55. [Google Scholar] [CrossRef]
- Inukonda, J.; Tetala, V.R.R.; Hallur, J. Explainable Artificial Intelligence (XAI) in Healthcare: Enhancing Transparency and Trust. Int. J. Multidiscip. Res 2024, 6, 30010. [Google Scholar]
- Lötsch, J.; Kringel, D.; Ultsch, A. Explainable artificial intelligence (XAI) in biomedicine: Making AI decisions trustworthy for physicians and patients. BioMedInformatics 2021, 2, 1–17. [Google Scholar] [CrossRef]
- Goldstein, C.A.; Berry, R.B.; Kent, D.T.; Kristo, D.A.; Seixas, A.A.; Redline, S.; Westover, M.B. Artificial intelligence in sleep medicine: Background and implications for clinicians. J. Clin. Sleep Med. 2020, 16, 609–618. [Google Scholar] [CrossRef] [PubMed]
- Upadrista, V.; Nazir, S.; Tianfield, H. Secure data sharing with blockchain for remote health monitoring applications: A review. J. Reliab. Intell. Environ. 2023, 9, 349–368. [Google Scholar] [CrossRef] [PubMed]
- Hamida, S.T.-B.; Hamida, E.B.; Ahmed, B.; Abu-Dayya, A. Towards efficient and secure in-home wearable insomnia monitoring and diagnosis system. In Proceedings of the 13th IEEE International Conference on BioInformatics and BioEngineering, Chania, Greece, 10–13 November 2013. [Google Scholar]
- Sadek, I.; Rehman, S.U.; Codjo, J.; Abdulrazak, B. Privacy and security of IoT based healthcare systems: Concerns, solutions, and recommendations. In How AI Impacts Urban Living and Public Health: Proceedings of the 17th International Conference, ICOST 2019, New York City, NY, USA, 14–16 October 2019, Proceedings 17; Springer International Publishing: Cham, Switzerland, 2019. [Google Scholar]

| Category | Evaluation Metric | Description |
|---|---|---|
| Device Classification | Wearables, smartphone apps, or smart mattresses | Categorized for comparison |
| Sleep Metrics | Sleep duration, efficiency, and disturbances | Accuracy in measuring key sleep parameters |
| Physiological Data | HRV, respiratory rate, and SpO2 | Assessment of vital signs related to sleep health |
| Tracking Method | Actigraphy, ballistocardiography (BCG), sound analysis, and EEG-based sensors | The type of data collection mechanism used |
| Data Privacy and Security | Compliance with HIPAA, GDPR, and data encryption protocols | Evaluate how well the device protects user data |
| Cost and Affordability | Device purchase, subscription fees, and free | Financial accessibility of the technology |
| Device Type | Visualization Platform | Visualization Methods |
|---|---|---|
| Mobile Sleep Apps | Smartphone app | Interactive graphs, color-coded charts, trend analysis |
| Wearable Devices | Wearable screen, smartphone app | Bar/line graphs, color-coded stages, trend analysis |
| Smart Mattresses | Smartphone/tablet app | Segmented graphs, environmental data, trend tracking |
| Criteria | PSG (Polysomnography) | Actigraphy |
|---|---|---|
| Accuracy | High accuracy, gold standard for sleep disorder diagnosis. | Moderate accuracy, less precise in detecting sleep stages. |
| Data Collected | Multiple physiological signals (EEG, ECG, EMG, EOG, etc.). | Movement data (via accelerometer), often combined with sleep/wake status. |
| Sleep-Phase Detection | Precise detection of sleep stages (NREM, REM, etc.). | Limited to general sleep/wake detection, with basic phase detection. |
| Application | Diagnosing complex sleep disorders (e.g., sleep apnea, narcolepsy). | Long-term monitoring, behavioral sleep tracking, lifestyle intervention assessment. |
| Limitations | Requires a controlled environment (sleep lab), expensive, time-consuming. | Less accurate in diagnosing disorders, cannot detect complex physiological events. |
| Category | Technologies | Data Collected | Applications | Limitations |
|---|---|---|---|---|
| Smartphone Applications | Mobile apps | Movement, sound, heart rate (via sensor) | Basic sleep tracking, snoring, sleep quality | Limited precision, dependent on phone placement |
| Wearable Devices | Smartwatches, EEG headbands, chest straps | Movement, heart rate, EEG, SpO2 | Sleep stages, heart rate, sleep apnea detection | Accuracy limitations, discomfort, restricted sleep-stage detection |
| Smart Mattresses | Smart mattresses, multi-sensor systems | Movement, respiration, heart rate, EEG | Comprehensive sleep data (stages, health, disturbances) | Complex integration, higher cost, potential privacy concerns |
| Smartphone Apps | Key Features | Technology | Platform Rating and Number | AI Application | Device Integration |
|---|---|---|---|---|---|
| Sleep Cycle [34] | Sleep-stage tracking, smart alarm, snore detection, and movement. | Microphone, accelerometer | Android: 4.6 (206 K) iOS: 4.6 (2.6 K) | Uses patented AI | Yes |
| SleepScore [35] | Sleep tracking, sleep score, and sleep report. | Sonar technology | Android: 3.1 (902) iOS: 4.4 (7.3 K) | Uses patented AI | Yes |
| Sleep Monitor [36] | Track sleep talk, cycle, and analysis; smart alarm. | Not mentioned | Android: 4.6 (97 K) iOS: 4.5 (475) | No | No |
| Sleep as Android [37] | Monitor sleep cycle, sleep score, and sleep talk. | Accelerometer | Android: 4.5 (379 K) | No | Wearables, third-party apps |
| Snore Recorder [38] | Snore detection and sleep analysis. | Microphone | iOS: 4.5 (64) | No | Apple Health |
| ShutEye [39] | Sleep tracking, smart alarm, and snore detection. | Microphone | Android: 4.5 (86.9 K) iOS: 4.8 (316 K) | Yes | No |
| Pillow [40] | Sleep tracking, analysis, smart alarm, sleep aid, and insights. | Microphone, accelerometer | iOS: 4.4 (93.6 K) | No | Apple devices |
| SleepBot [41] | Sleep tracking, HR analysis, relaxing sound, sleep alerts, and timer. | Accelerometer | iOS: 4.6 (52) | Yes | iPhone |
| Sleep Tracker—Sleep Sounds [42] | Sleep tracking, insights, and goals. Sound therapy and smart alarm. | Accelerometer, gyroscope, microphone | Android: 4.6 (154 K) iOS: 4.8 (5.3 K) | Yes | Smart home devices, watches, voice assistance |
| SnoreLab [43] | Snore detection and sleep statistic. | Microphone | Android: 4.6 (47 K) iOS: 4.7 (53.8 K) | No | Apple Health |
| NapBot—Auto Sleep Tracker [44] | Sleep tracking, analysis, and history; HR monitor. | Accelerometer | iOS: 4.2 (6.2 K) | Yes | Apple Health |
| Sleep Details [45] | Sleep tracking, score, patterns, and insights. | Microphone, accelerometer | iOS: 4.4 (950) | Yes | Wearables, home devices, health apps, medical devices |
| iPhone Health [46] | Sleep, menstrual, activity, and medication tracking, mental health, Hearing test, Heart Health Monitoring, and ac. | Accelerometer, gyroscope | iOS: 3.0 (6.4 K) | No | Apple Watch, third-party devices |
| Sleepia [47] | Sleep analysis and programs, snore detection, environment sound analysis, and smart alarm. | Microphone | Android: iOS: 4.6 (119) | Yes | Apple Health |
| Mintal Tracker [48] | Sleep tracking, report, booster, aid, and talk recording; snore detection, alarm clock, and audio tracks. | Microphone | Android: 3.5 (609) iOS: 4.8 (38 K) | Yes | Apple Health |
| Alarmy [49] | Sleep analysis and sound; snore detection. | Microphone, accelerometer, camera | Android: 4.5 (1.78 M) iOS: 4.8 (199.2 K) | No | No |
| Sleep time [50] | Sleep analysis, history, smart alarm, and soundscapes. | Accelerometer | iOS: 4.7 (5.3 K) | No | Apple Health |
| Sleepace [51] | Sleep monitoring, aid, reports, and tips; smart alarm. | Microphone, motion sensors | iOS: 1.9 (27) | Yes | Apple Health |
| Rise [52] | Sleep tracking: duration, quality, stage, and deficit. | Accelerometer, microphone | Android: 4.2 (5.8 K) iOS: 4.6 (25.7 K) | AI and ML | Wearables, home devices, health apps |
| Sleepzy [53] | Sleep tracking: pattern, quality, and debt analysis; smart alarm. | Microphone | iOS: 4.3 (22.4 K) | AI to generate music | Apple Health and watch |
| SlumberCycle [54] | Sleep tracking, recording, and aid; smart alarm. | Smartphone’s built-in sensors | Android: 3.9 (6.7 K) | No | No |
| Smartwatch | Sleep Features Monitored | Technology (Sensors) | AI Usage | Visualization Platform | Other Features |
|---|---|---|---|---|---|
| Apple Watch Ultra 2 [65] | Track sleep stages, breathing disturbances, sleep duration | Accelerometer, HR sensor, SpO2, Skin temp, Mic | Machine learning for sleep-stage detection | Apple Health, Sleep app | 36 h battery, ECG, dual-frequency GPS |
| Apple Watch Series 9 [66] | Sleep stages, HR, SpO2, Resp. rate | Accelerometer, HR sensor, SpO2, Mic | Machine learning for sleep tracking | Apple Health, Sleep app | 18 h battery, ECG, fast charging |
| Samsung Galaxy Watch 6 [67] | Sleep stages, HR, SpO2, snoring detection, HRV | Accelerometer, BioActive sensor (HR, SpO2), Mic | AI-driven sleep coaching, snore pattern analysis | Samsung Health | 3-day battery, body composition tracking |
| Fitbit Sense 2 [68] | Sleep score, stages, HR, SpO2, Skin temp, HRV | Accelerometer, HR sensor, SpO2, Skin temp | AI-driven stress and sleep insights | Fitbit app (premium for full insights) | 6-day battery, EDA stress tracking |
| Garmin Venu 3 [69] | Sleep score, stages, HR, SpO2, Resp. rate, HRV | Accelerometer, HR sensor, SpO2, Barometer | AI-based Body Battery for recovery analysis | Garmin Connect | 14-day battery, advanced fitness tracking |
| Garmin Fenix 7 Pro [70] | Sleep score, HRV, stages, SpO2, Resp. rate | HR sensor, SpO2, Barometer, Altimeter | AI-based Body Battery and recovery tracking | Garmin Connect | Rugged design, solar charging option |
| Withings ScanWatch 2 [71] | Sleep stages, HR, SpO2, sleep apnea detection | ECG, HR sensor, SpO2, motion sensor | AI-based apnea detection, deep sleep analysis | Withings Health Mate | 30-day battery, hybrid smartwatch |
| Google Pixel Watch 2 [72] | Sleep stages, HR, SpO2, Resp. rate | Fitbit sensors: HR, SpO2, accelerometer | Fitbit AI for sleep trends and wellness coaching | Fitbit app, Google Health | 24-h battery, Wear OS 4 |
| Huawei Watch GT 3 [73] | Sleep stages, HR, SpO2, Resp. rate | TruSleep 3.0, HR sensor, SpO2, accelerometer | AI sleep coaching, personalized insights | Huawei Health | 14-day battery, built-in GPS |
| Polar Ignite 3 [74] | Sleep score, sleep stages, Nightly Recharge | Accelerometer, HR sensor, SpO2 | AI Nightly Recharge analysis | Polar Flow | 5-day battery, advanced training metrics |
| Amazfit Bip 5 Unity [75] | Sleep stages, HR, SpO2 | BioTracker PPG 4.0 sensor, accelerometer | AI-based sleep trends analysis | Zepp app | 10-day battery, lightweight design |
| Suunto 9 Peak Pro [76] | Sleep stages, HR, SpO2 | HR sensor, SpO2, Altimeter, Barometer | AI-based sleep and recovery tracking | Suunto App | 21-day battery, ultra-durable design |
| ASUS VivoWatch 5 plus [77] | Sleep stages, HR, SpO2 | ECG, HR sensor, SpO2, accelerometer | AI-based algorithm maximizes battery life | HealthConnect App | 14-day battery, built-in GPS, water resistant |
| Oppo Watch [78] | Sleep score, sleep stages, HR, SpO2 | PPG HR sensor, ECG, accelerometer, gyroscope, Barometer | AI imaging algorithm, AI-based sleep | Oppo Health App | 21-day battery, dual-chip endurance system |
| Mi Watch [79] | Sleep score, sleep stages, HR, SpO2 | PPG HR sensor, ECG, accelerometer, gyroscope, Barometer | AI-based algorithm battery life extension | Mi Fitness App | 16-day battery, built-in GPS |
| Maimo Watch [80] | Sleep score, sleep stages, HR, SpO2 | PPG HR sensor, ECG, accelerometer, gyroscope, Barometer | AI-based sleep, Running Competitor | Maimo fit App | 10-day battery, built-in Alexa, water resistant |
| Smart Mattresses | Key Sleep Monitoring Features | Other Features | Technology (Sensors) | AI Application | Sleep Visualization Method |
|---|---|---|---|---|---|
| Eight Sleep Pod Pro Cover [85] | Sleep tracking and temperature control. | Temperature Control, wake-up technology | Embedded sensors, active grid layer | Yes | Dedicated app |
| Sleep Number 360 [86] | Monitors sleep quality, HR, breathing, movement, and pressure. | Pressure Adjustments, Automatic Positioning, Temperature Control | Embedded sensors | Yes | SleepIQ app |
| ReST Bed [87] | Tracks sleep position, movement, and pressure. | Customizable firmness for 5 body zones | Smart fabric sensors | Yes | ReST Bed™ app |
| Withings Sleep Analyzer [88] | Sleep apnea detection, snore detection, sleep analysis, and heart rate monitoring. | Automatic Wi-Fi Sync | Pneumatic sensor, ballistocardiography | Yes | Withings Health Mate app |
| Tempur-Pedic LuxeBreeze with Ergo® Smart Base [89] | Tracks various sleep metrics: efficiency, duration, stages, etc. | Adjustable base, Pressure Relief, cooling tech | Sensors embedded in the Ergo® Smart Base | Yes | Tempur-Ergo Smart Base app |
| Bryte Balance Smart Bed [90] | Tracks sleep patterns, stages, duration, and has Sleep Concierge. | AI adjusts firmness, Zero Gravity Position | Embedded sensors | Yes | Bryte app |
| Whizpad Mattress [91] | Tracks movement and sleep activity. | Pressure Redistribution, Early Leave-Bed Alerts | Pressure sensors | Yes | Whizpad app |
| NordicTrack Sleep Mattress [92] | Tracks HR, respiration, awakenings, bed exits, and sleep metrics. | Sleep coaching, smart alarm | iFit Sleep HR sensor | No | iFit Sleep app |
| ERA Smart Layer [93] | Sleep pattern and heat rate and breathing analysis. | Active Spinal Alignment, Multizone Relaxation, Thermal Regulation | BCG sensors | Yes | ERA App |
| User Scenario | Recommended Technology | Key Features | Limitations |
|---|---|---|---|
| General Users | Smartphone apps, wearables | Cost-effective, widely available | Lower accuracy in sleep staging |
| Sleep Disorders | FDA-approved wearables, smart mattresses | Sleep apnea detection, long-term tracking | Less accurate than PSG |
| Athletes and Recovery | Smartwatches, smart mattresses | HRV analysis, deep sleep tracking, recovery monitoring | Smart mattresses are expensive, AI-based insights need validation |
| Elderly | Smart mattresses, non-contact sensors | Passive monitoring, caregiver alerts | High cost, limited health integration |
| Mental Health Applications | Wearables, smartphone apps | HRV-based stress analysis, AI sleep coaching | AI interpretation of HRV–sleep relationship still evolving |
| Children’s Sleep Monitoring | Smart baby monitors, wearables | Safety alerts, sleep duration tracking | Privacy concerns, limited sleep-stage accuracy |
| Device Type | Cost (USD) | Accuracy | Health Benefits | Best For |
|---|---|---|---|---|
| Smartphone Apps | Free–USD50 | Low | Basic sleep tracking, lack physiological data | Budget-conscious users |
| Wearables | USD100–USD500 + subscription | Medium–High | Track HRV, SpO2, sleep stages, AI coaching | Athletes, sleep-conscious individuals |
| Smart Mattresses | USD500–USD3000 + subscription | Medium | Passive tracking, sleep position adjustment | Long-term users, couples, hands-free use |
| Device Category | Device | Data Category | |||
|---|---|---|---|---|---|
| Sleep Metrics | Physiological Data | Movement Data | Environmental Data | ||
| Smartphone apps | Sleep Cycle [34] | ✔ | ✔ | ✔ | |
| SleepScore [35] | ✔ | ✔ | ✔ | ||
| Sleep Monitor [36] | ✔ | ✔ | ✔ | ||
| Sleep as Android [37] | ✔ | ✔ | ✔ | ||
| Snore Recorder [38] | ✔ | ✔ | |||
| ShutEye [39] | ✔ | ✔ | ✔ | ✔ | |
| Pillow [40] | ✔ | ✔ | ✔ | ||
| SleepBot [41] | ✔ | ✔ | ✔ | ||
| Sleep Tracker—Sleep Sounds [42] | ✔ | ✔ | ✔ | ||
| SnoreLab [43] | ✔ | ✔ | |||
| NapBot—Auto Sleep Tracker [44] | ✔ | ✔ | ✔ | ||
| Sleep Details [45] | ✔ | ✔ | ✔ | ||
| iPhone Health [46] | ✔ | ✔ | ✔ | ||
| Sleepia [47] | ✔ | ✔ | ✔ | ✔ | |
| Mintal Tracker [48] | ✔ | ✔ | ✔ | ||
| Alarmy [49] | ✔ | ✔ | |||
| Sleep time [50] | ✔ | ✔ | ✔ | ||
| Sleepace [51] | ✔ | ✔ | ✔ | ||
| Rise [52] | ✔ | ✔ | ✔ | ||
| Sleepzy [53] | ✔ | ✔ | ✔ | ||
| SlumberCycle [54] | ✔ | ✔ | ✔ | ||
| Smartwatches | Apple Watch Ultra 2 [65] | ✔ | ✔ | ✔ | ✔ |
| Apple Watch Series 9 [66] | ✔ | ✔ | ✔ | ✔ | |
| Samsung Galaxy Watch 6 [67] | ✔ | ✔ | ✔ | ✔ | |
| Fitbit Sense 2 [68] | ✔ | ✔ | ✔ | ✔ | |
| Garmin Venu 3 [69] | ✔ | ✔ | ✔ | ||
| Garmin Fenix 7 Pro [70] | ✔ | ✔ | ✔ | ||
| Withings ScanWatch 2 [71] | ✔ | ✔ | ✔ | ||
| Google Pixel Watch 2 [72] | ✔ | ✔ | ✔ | ✔ | |
| Huawei Watch GT 3 [73] | ✔ | ✔ | ✔ | ||
| Polar Ignite 3 [74] | ✔ | ✔ | ✔ | ||
| Amazfit Bip 5 Unity [75] | ✔ | ✔ | ✔ | ||
| Suunto 9 Peak Pro [76] | ✔ | ✔ | ✔ | ||
| ASUS VivoWatch 5 plus [77] | ✔ | ✔ | ✔ | ||
| Oppo Watch [78] | ✔ | ✔ | ✔ | ||
| Mi Watch [79] | ✔ | ✔ | ✔ | ||
| Maimo Watch [80] | ✔ | ✔ | ✔ | ||
| Smart mattresses | Eight Sleep Pod Pro Cover [85] | ✔ | ✔ | ✔ | ✔ |
| Sleep Number 360 [86] | ✔ | ✔ | ✔ | ✔ | |
| ReST Bed [87] | ✔ | ✔ | ✔ | ✔ | |
| Withings Sleep Analyzer [88] | ✔ | ✔ | ✔ | ✔ | |
| Tempur-Pedic LuxeBreeze with Ergo® Smart Base [89] | ✔ | ✔ | ✔ | ✔ | |
| Bryte Balance Smart Bed [90] | ✔ | ✔ | ✔ | ✔ | |
| Whizpad Mattress [91] | ✔ | ✔ | ✔ | ||
| NordicTrack Sleep Mattress [92] | ✔ | ✔ | ✔ | ✔ | |
| ERA Smart Layer [93] | ✔ | ✔ | ✔ | ✔ | |
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2025 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Mathunjwa, B.M.; Kor, R.Y.J.; Ngarnkuekool, W.; Hsu, Y.-L. A Comprehensive Review of Home Sleep Monitoring Technologies: Smartphone Apps, Smartwatches, and Smart Mattresses. Sensors 2025, 25, 1771. https://doi.org/10.3390/s25061771
Mathunjwa BM, Kor RYJ, Ngarnkuekool W, Hsu Y-L. A Comprehensive Review of Home Sleep Monitoring Technologies: Smartphone Apps, Smartwatches, and Smart Mattresses. Sensors. 2025; 25(6):1771. https://doi.org/10.3390/s25061771
Chicago/Turabian StyleMathunjwa, Bhekumuzi M., Randy Yan Jie Kor, Wanida Ngarnkuekool, and Yeh-Liang Hsu. 2025. "A Comprehensive Review of Home Sleep Monitoring Technologies: Smartphone Apps, Smartwatches, and Smart Mattresses" Sensors 25, no. 6: 1771. https://doi.org/10.3390/s25061771
APA StyleMathunjwa, B. M., Kor, R. Y. J., Ngarnkuekool, W., & Hsu, Y.-L. (2025). A Comprehensive Review of Home Sleep Monitoring Technologies: Smartphone Apps, Smartwatches, and Smart Mattresses. Sensors, 25(6), 1771. https://doi.org/10.3390/s25061771











