Recommendations to Synthetize Old and New β-Lactamases Inhibitors: A Review to Encourage Further Production
Abstract
1. Introduction
2. β-Lactamase Enzymes (BLEs)
3. Old and Novel β-Lactamase Enzymes Inhibitors (BLEsIs)
4. BLAs/BLEsIs Combinations Currently Available on the Market and Clinically Applied
5. Marketed and Not Marketed BLEsIs: Guidelines for Their Synthesis
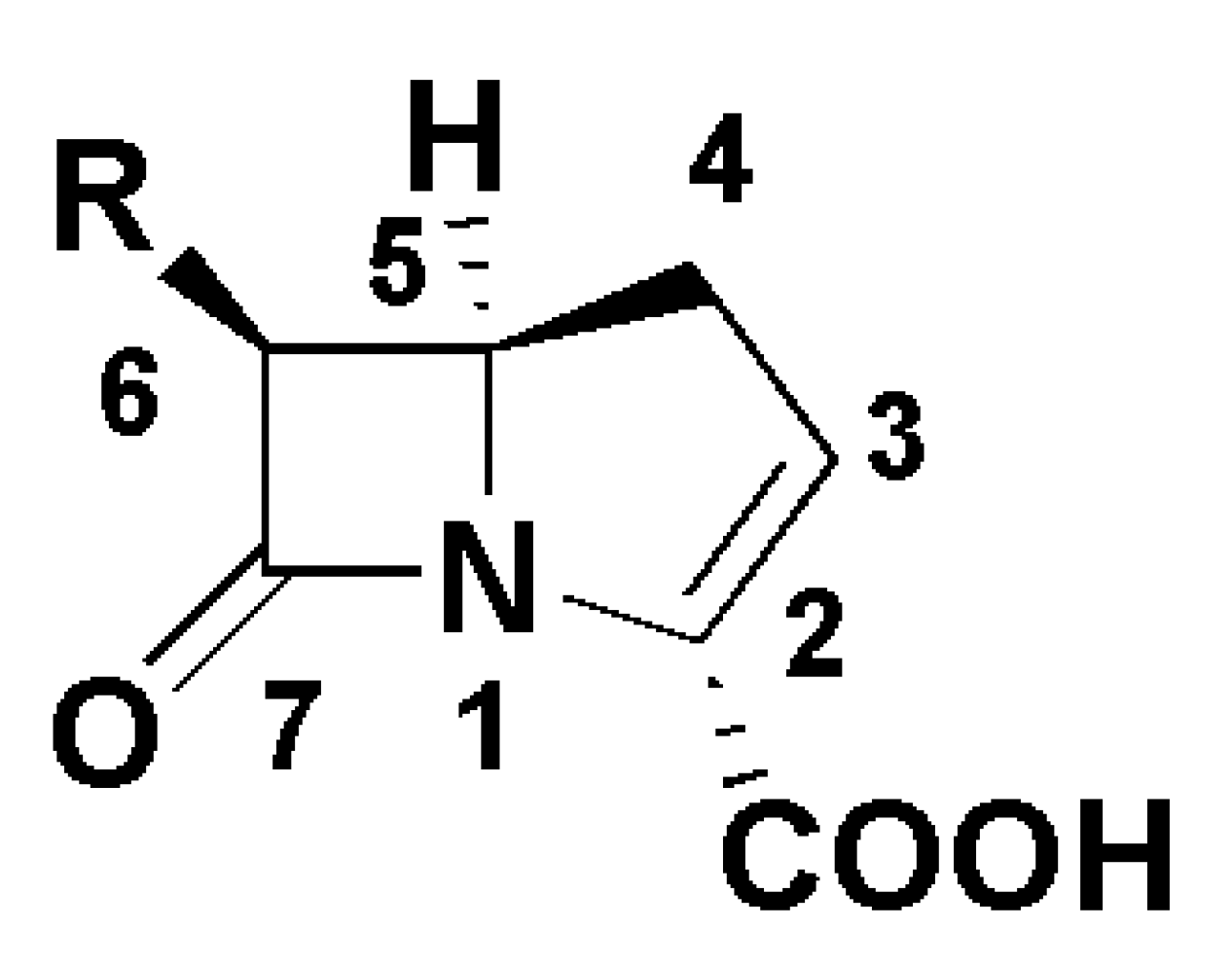
5.1. β-Lactams
5.1.1. Already Clinically Approved β-Lactams BLEsIs
Biosynthesis of Clavulanic Acid
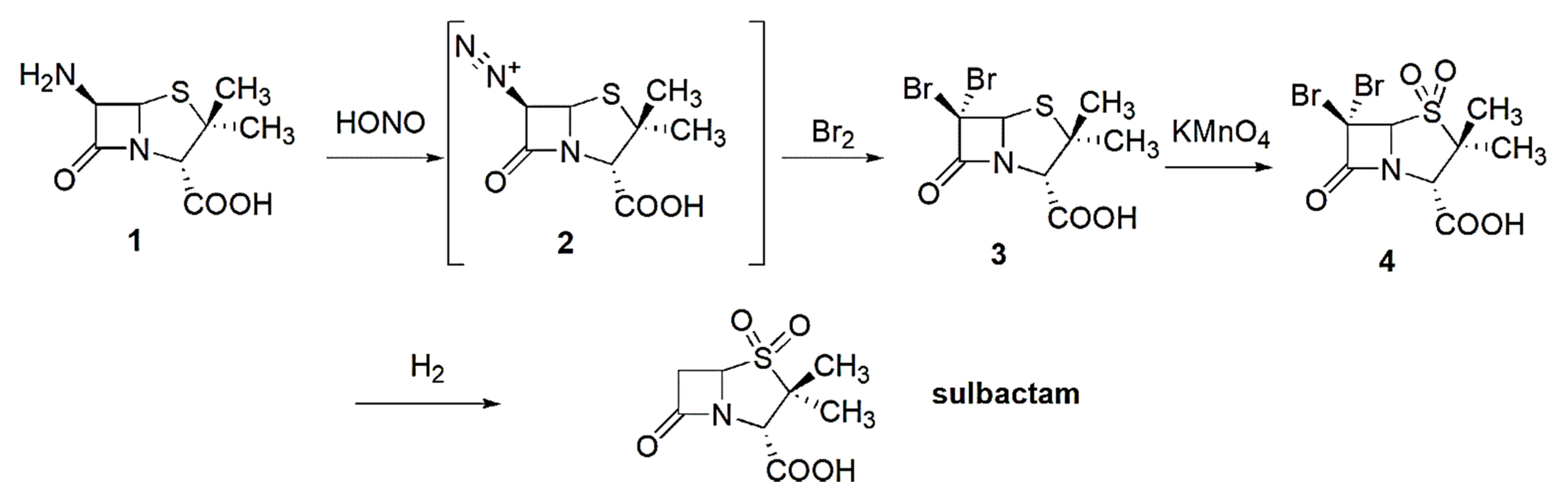
Synthesis of Sulbactam
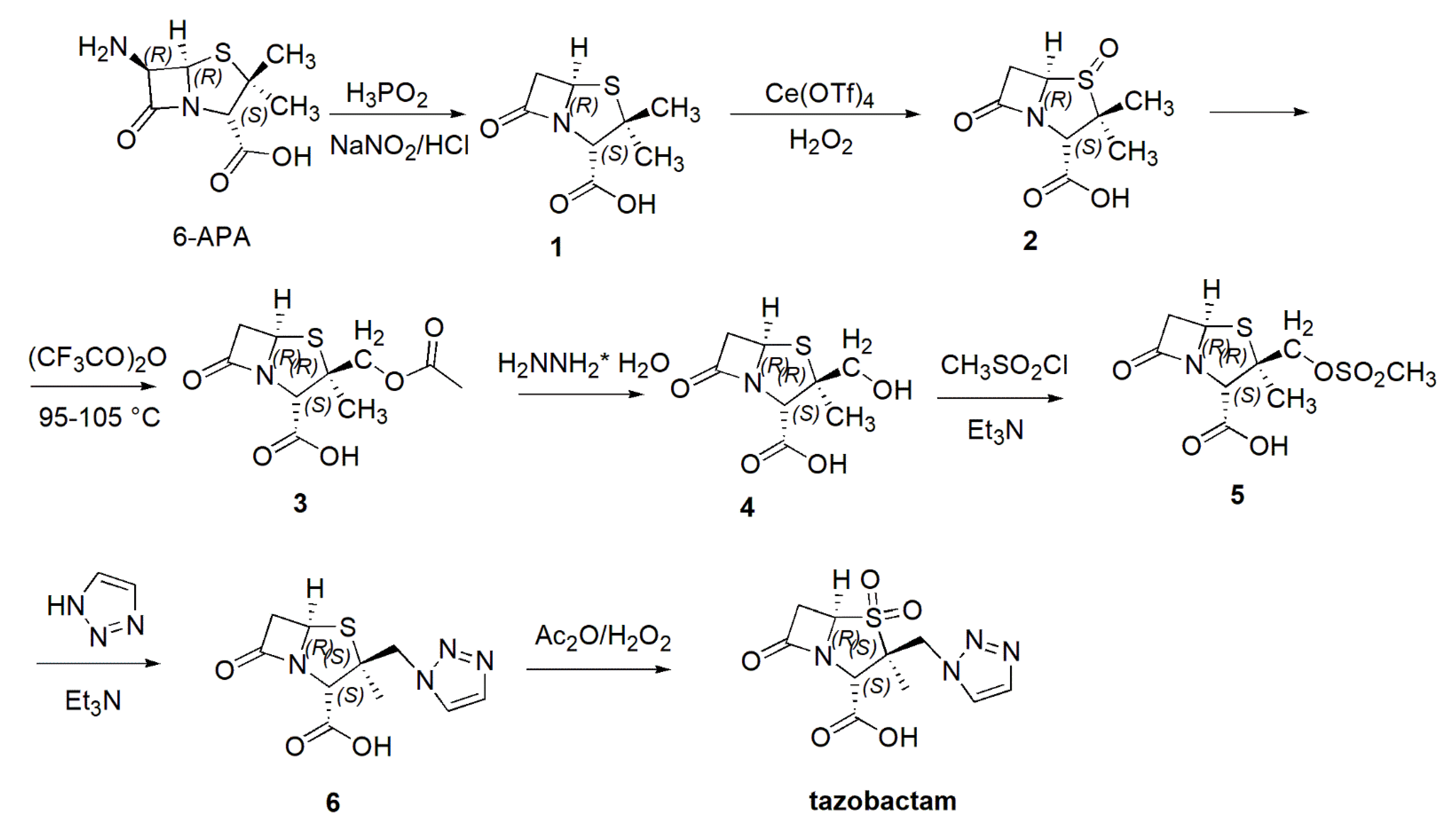
Synthesis of Tazobactam
Synthesis of Tebipenem Pivoxil
5.1.2. Not Yet Clinically Approved β-Lactam BLEsIs
Synthesis of Enmetazobactam
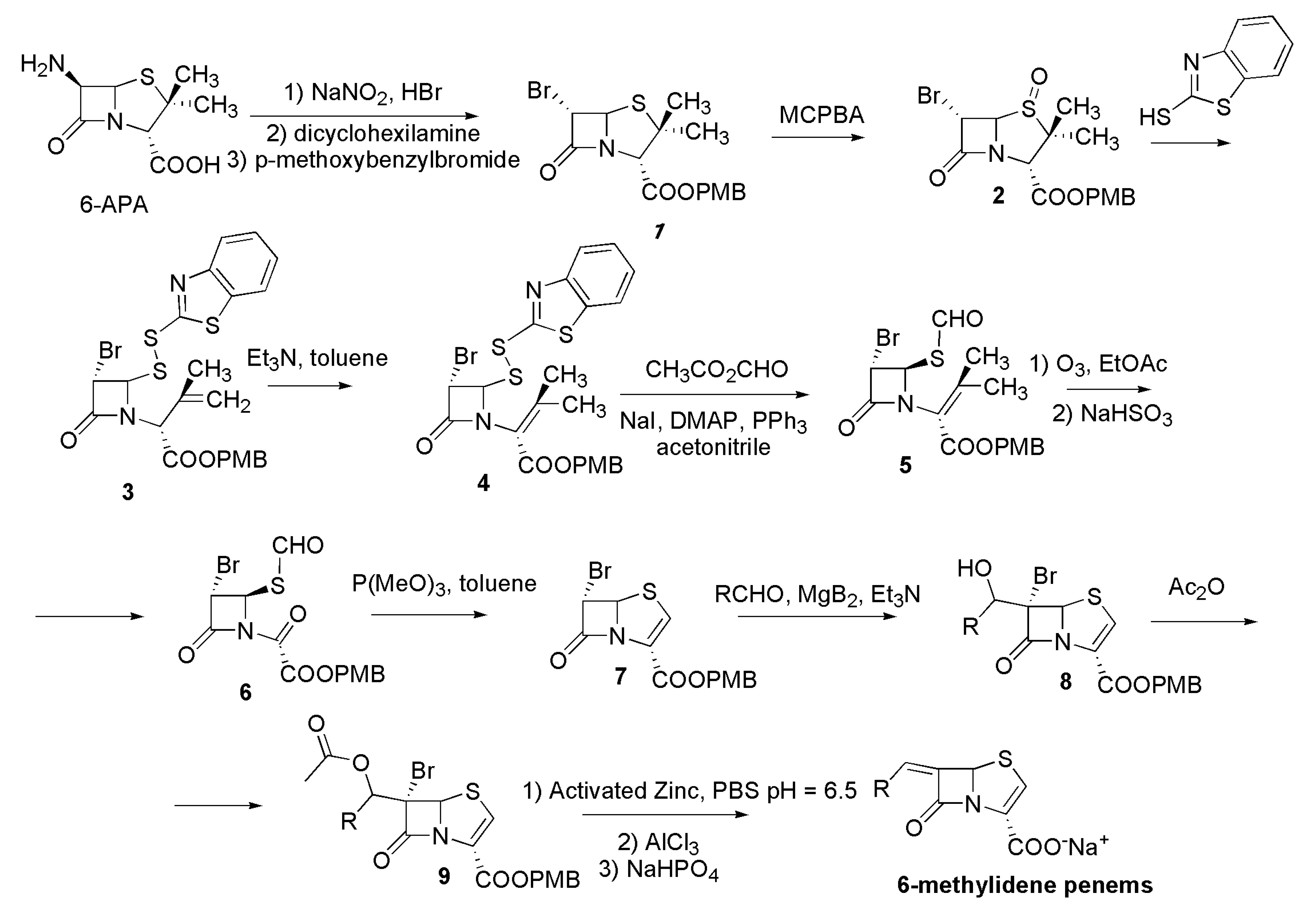
General Procedure to Synthetize 6-Methylidene-penem Carboxylic Acid Sodium Salts
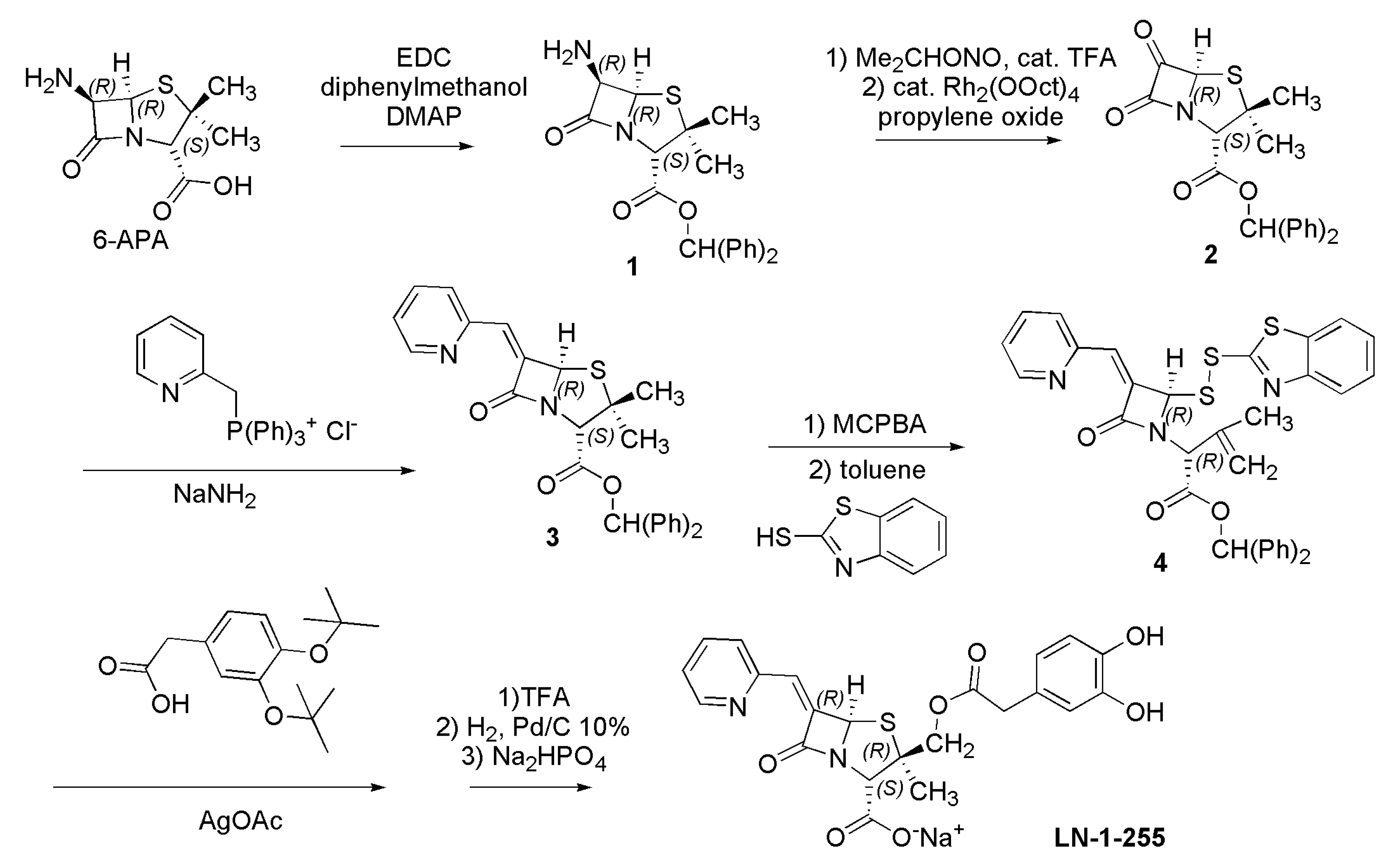
Synthesis of LN-1-255
5.2. Non-β-Lactam DBO BLEsIs
5.2.1. Clinically Approved DBO BLEsIs
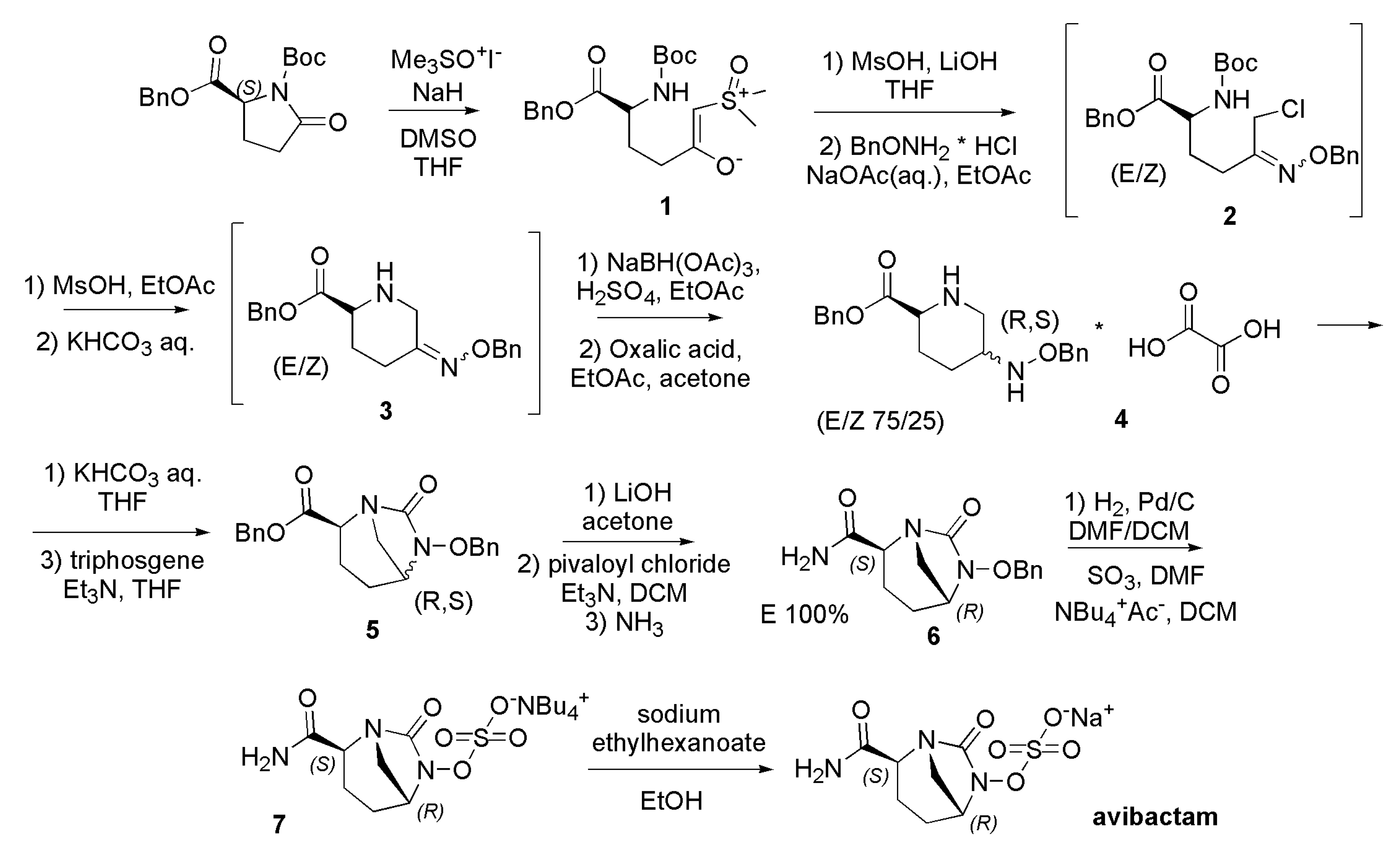
Synthesis of Avibactam
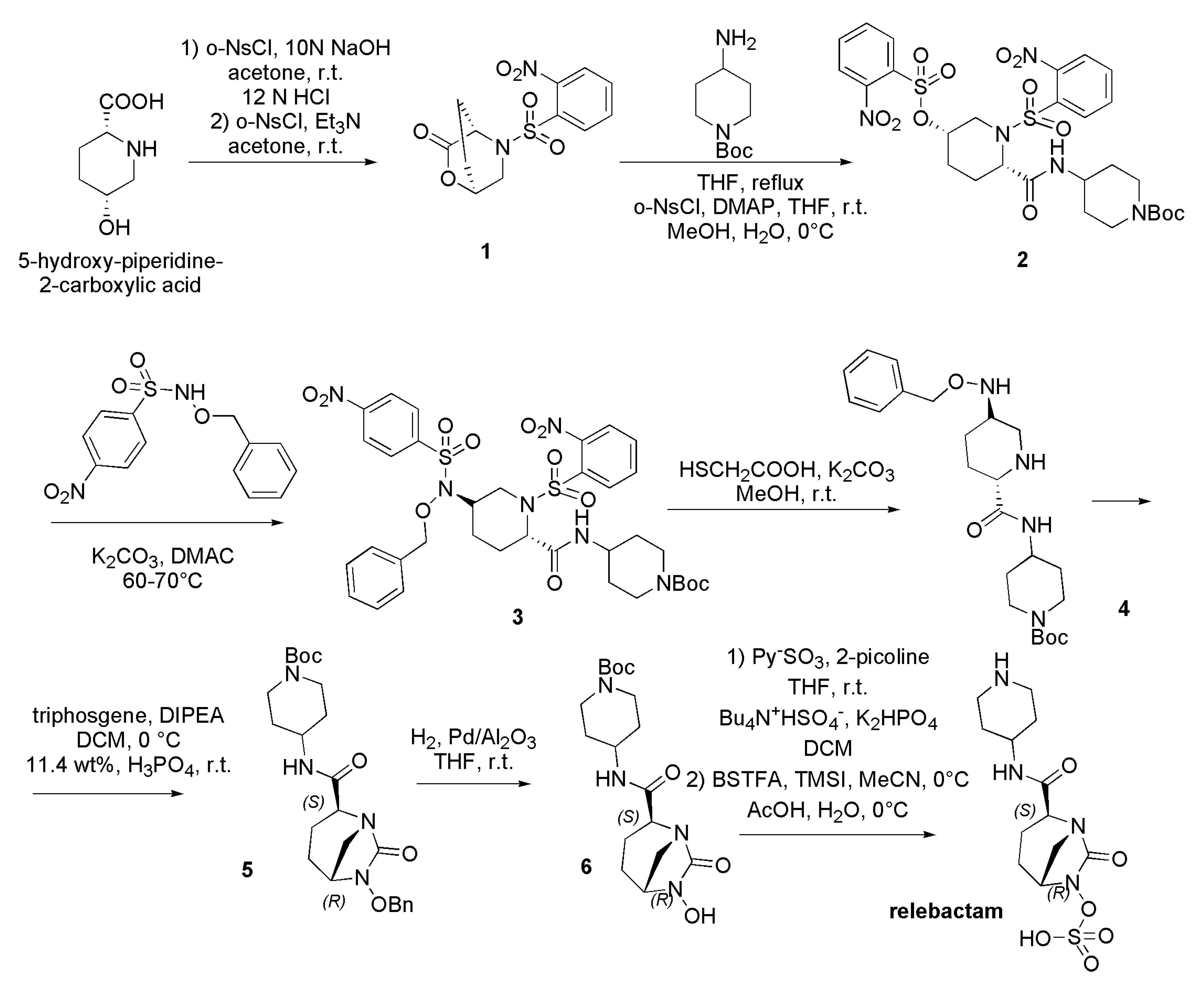
Synthesis of Relebactam
5.2.2. Not Yet Clinically Approved DBO BLEsIs
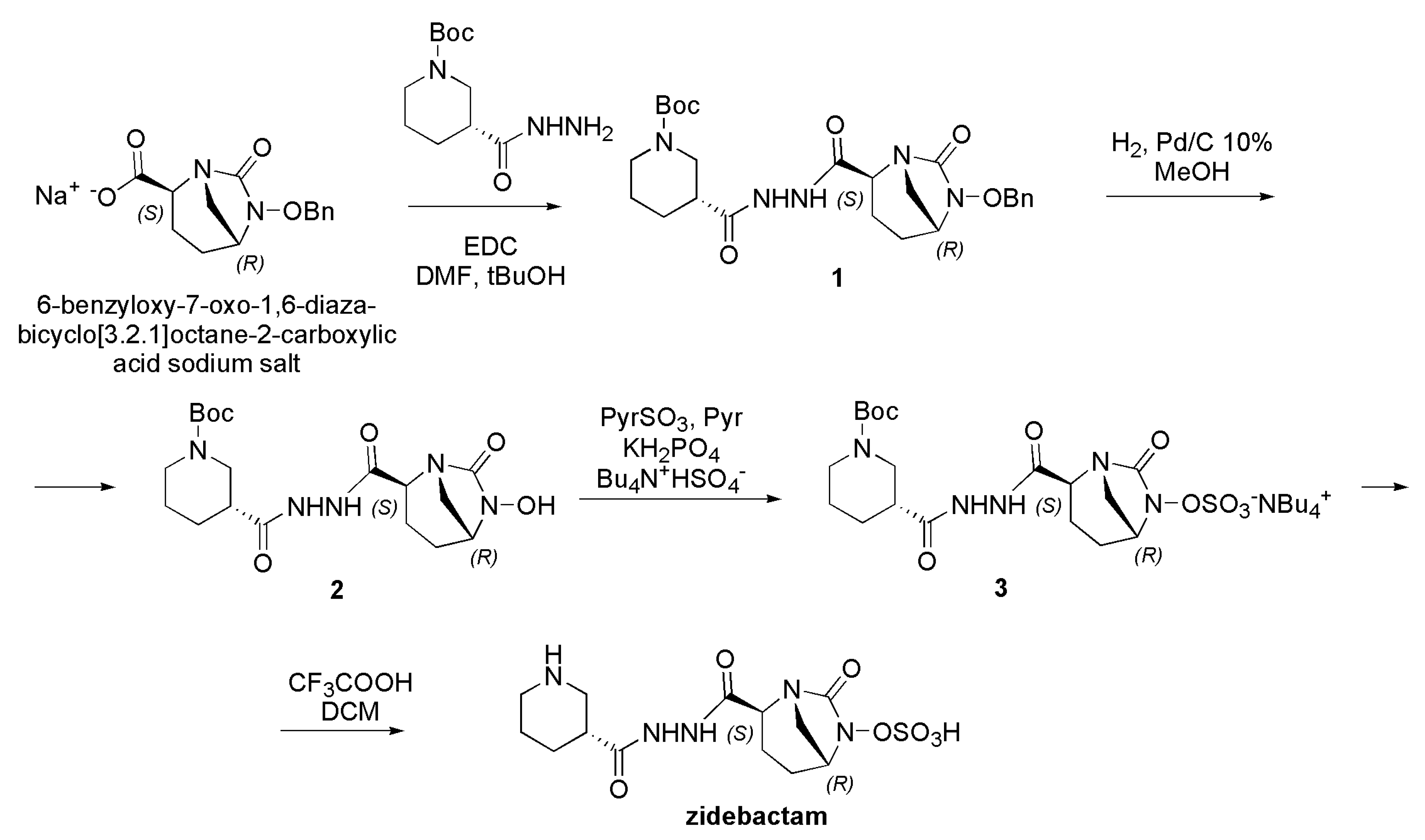
Synthesis of Zidebactam
Synthesis of WCK 5153
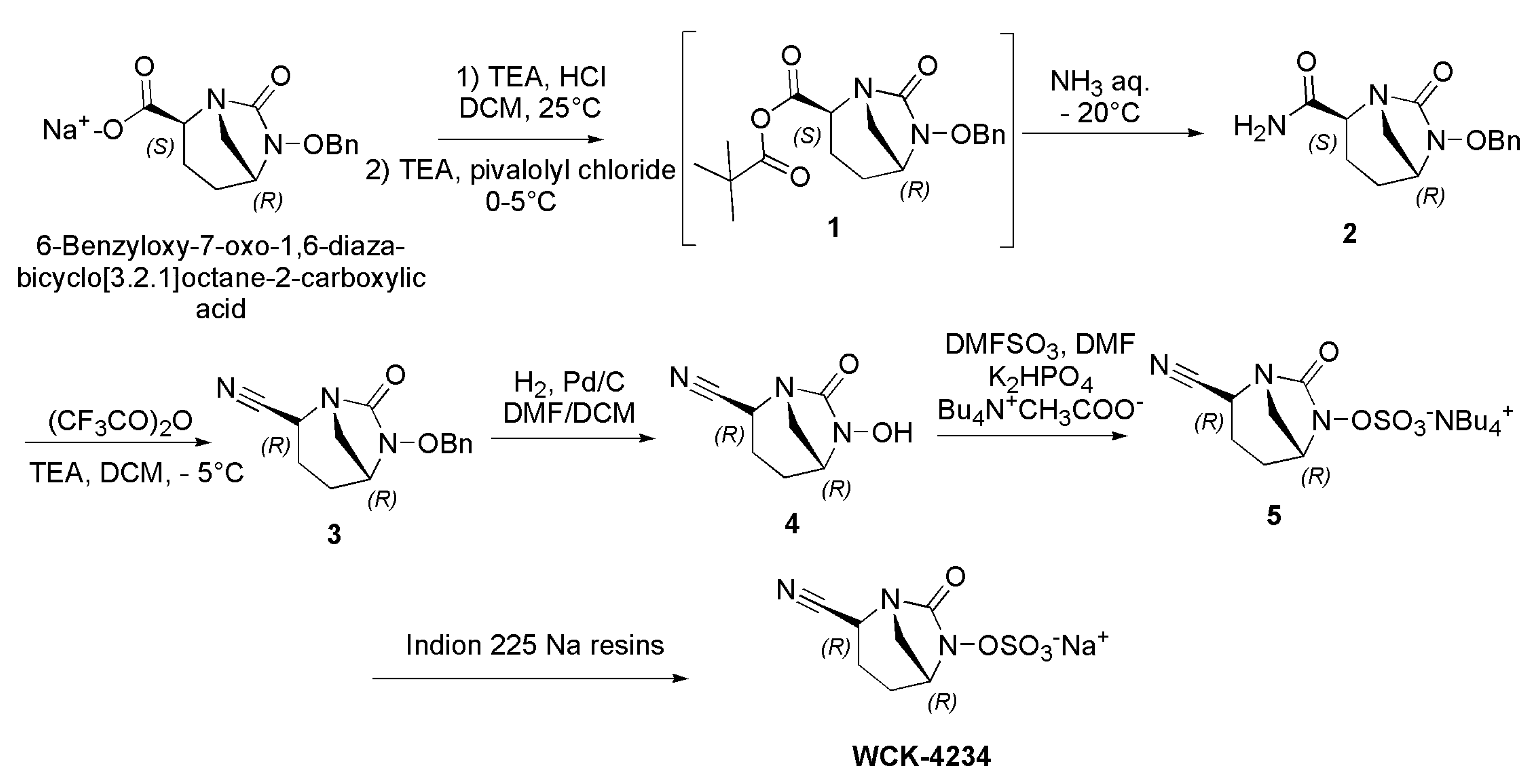
Synthesis of WCK-4234
Synthesis of ETX-1317 and of Its Orally Administrable Prodrug ETX-0282
Synthesis of Durlobactam
Synthesis of ANT-3310
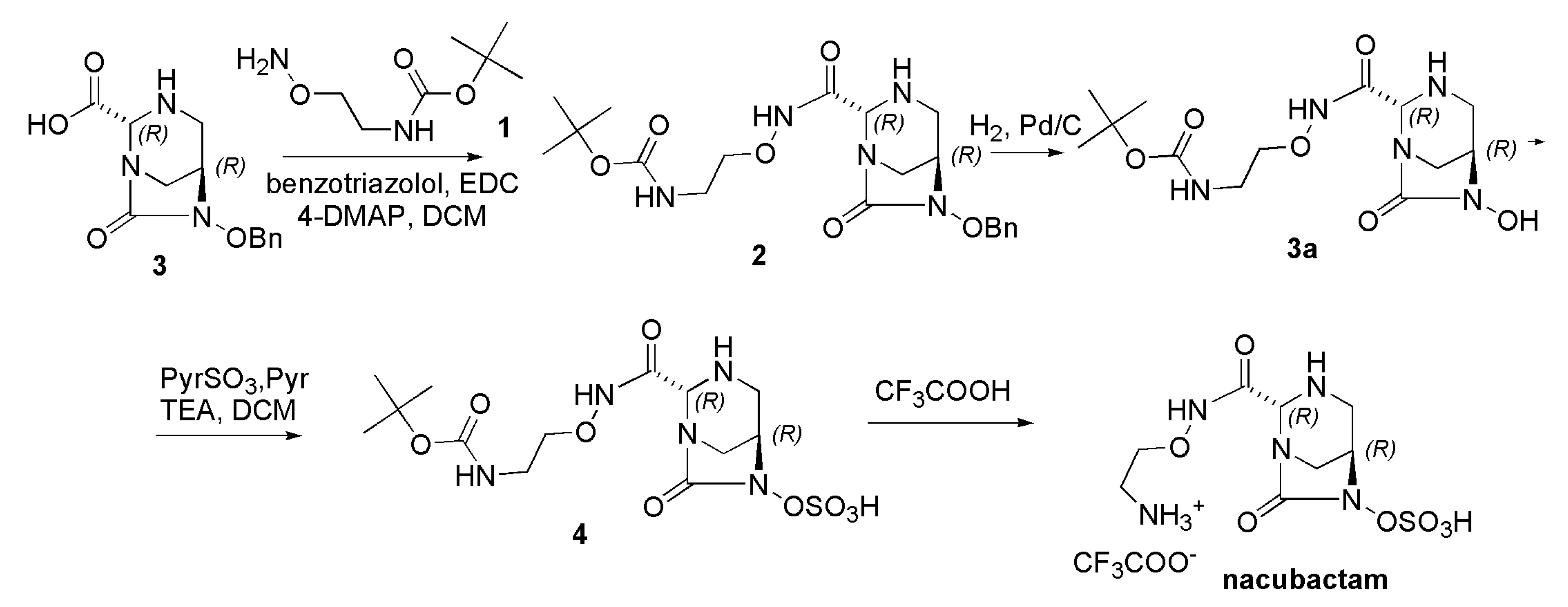
Synthesis of Nacubactam
Synthesis of GT-055
5.3. Non-β-Lactam Boronic Acid Derivatives
5.3.1. Clinically Approved Boronic Acid Derivative
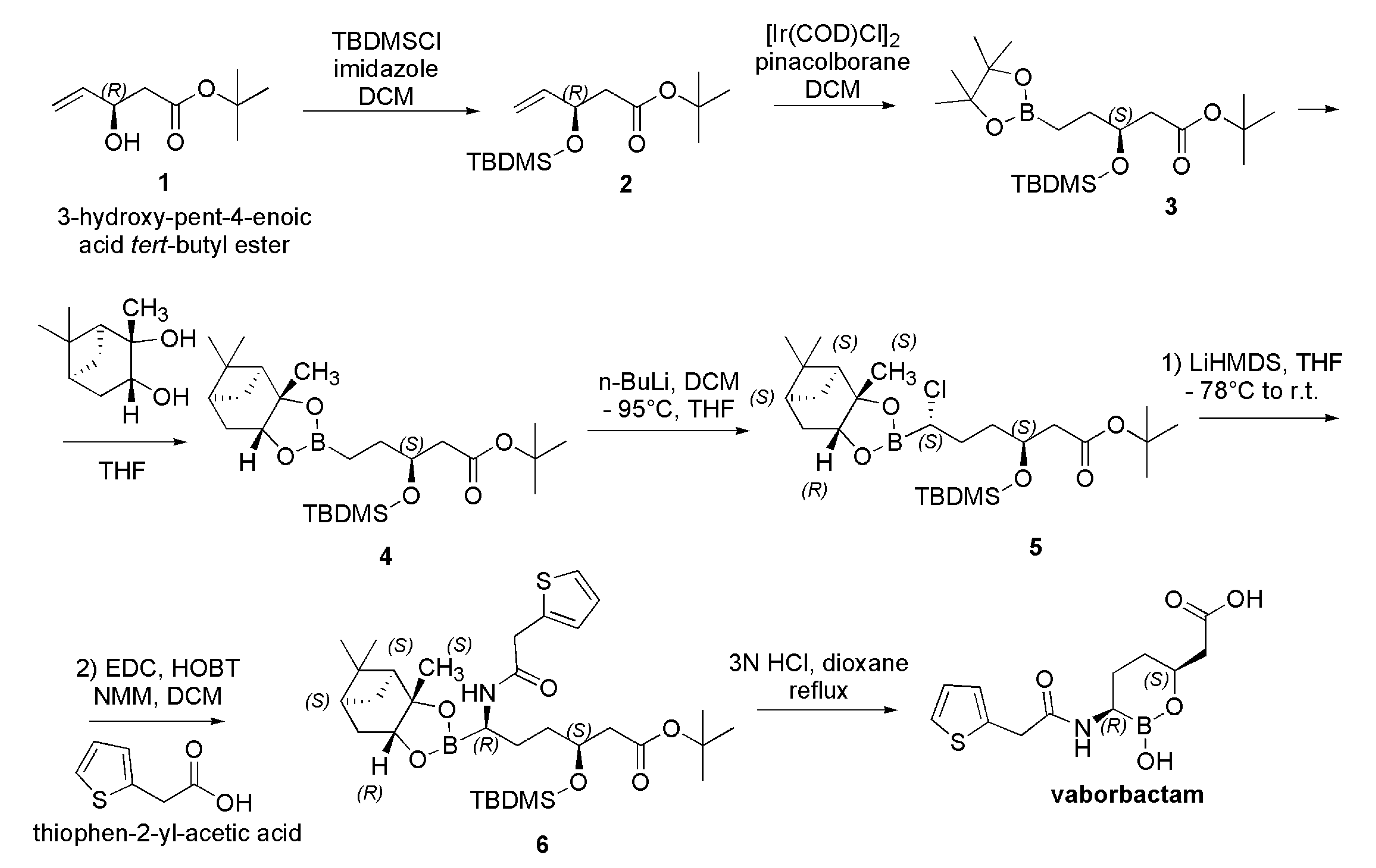
Synthesis of Vaborbactam
5.3.2. Not Yet Clinically Approved Boronic Acid Derivatives
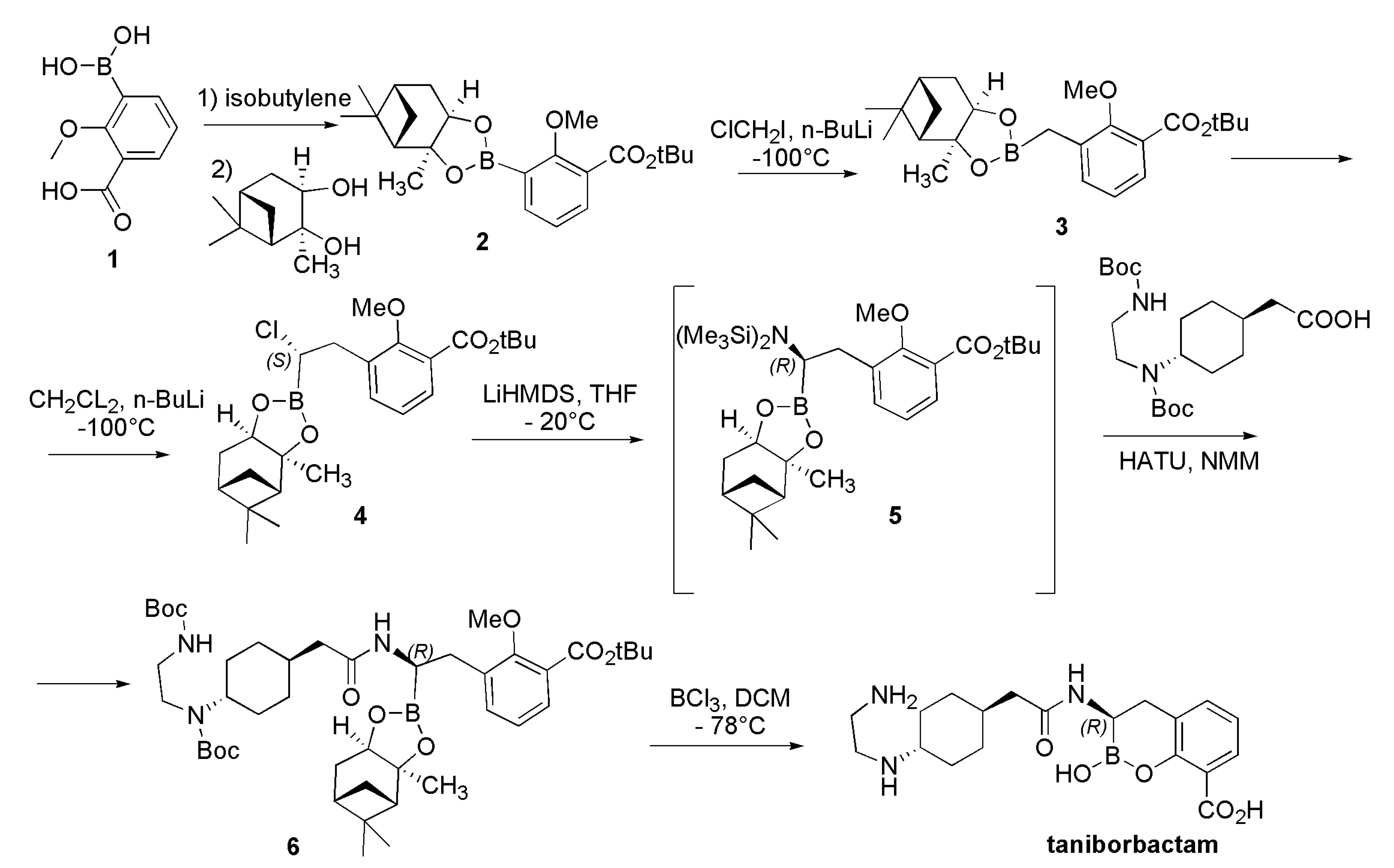
Synthesis of Taniborbactam
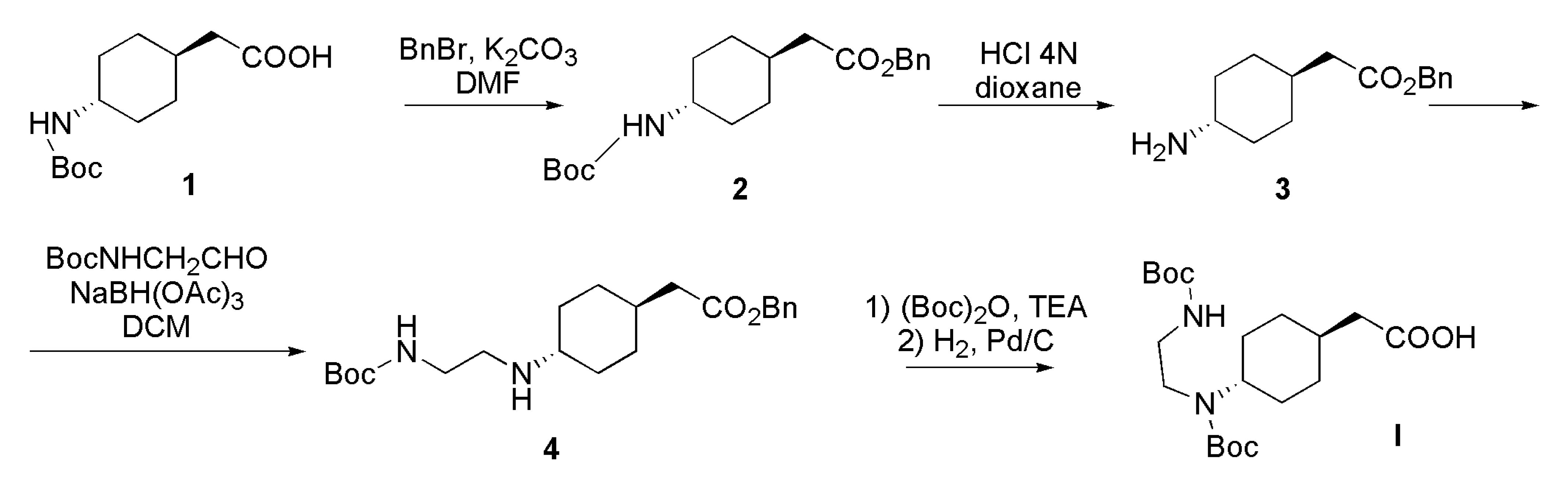
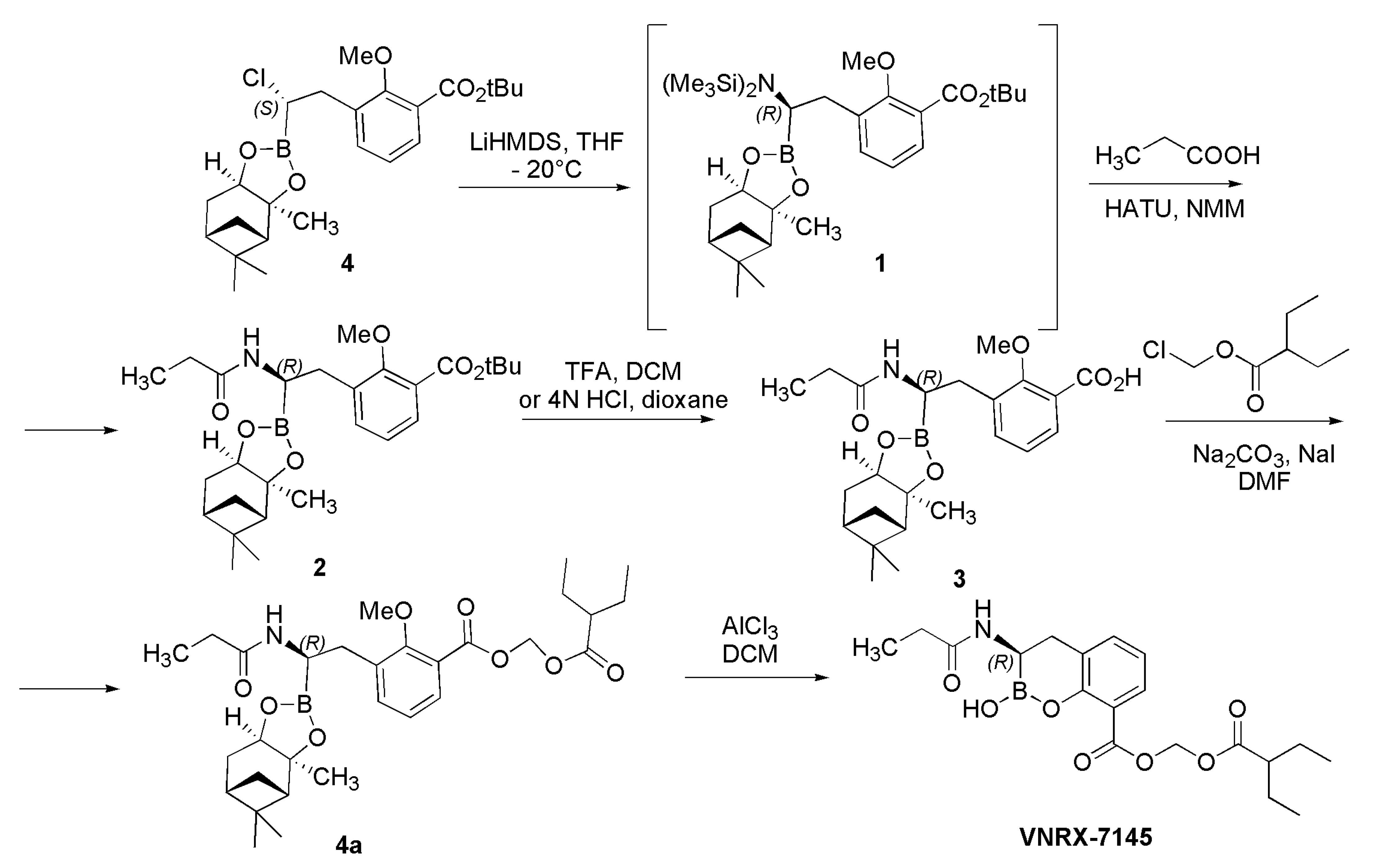
Synthesis of VNRX-7145
Synthesis of Xeruborbactam
5.4. Non-β-Lactam Thiazolyl Acid Derivatives
Synthesis of the Not Yet Approved ANT-2681
6. Conclusions and Authors Considerations
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Conflicts of Interest
References
- Tooke, C.L.; Hinchliffe, P.; Bragginton, E.C.; Colenso, C.K.; Hvievonen, V.H.A.; Takebayeshi, Y.; Spencer, J. β-Lactamases and β-Lactamase Inhibitors in the 21st Century. J. Mol. Biol. 2019, 431, 3472–3500. [Google Scholar] [CrossRef] [PubMed]
- Bush, K. Past and Present Perspectives on β-Lactamases. Antimicrob. Agents Chemother. 2018, 62, e01076-18. [Google Scholar] [CrossRef] [PubMed]
- List of β-lactam Antibiotics. From Wikipedia, the Free Encyclopedia. Available online: https://en.wikipedia.org/wiki/List_of_%CE%B2-lactam_antibiotics (accessed on 8 February 2022).
- Sauvage, E.; Kerff, F.; Terrak, M.; Ayala, J.A.; Charlier, P. The Penicillin-Binding Proteins: Structure and Role in Peptidoglycan Biosynthesis. FEMS Microbiol. Rev. 2008, 32, 234–258. [Google Scholar] [CrossRef] [PubMed]
- Palzkill, T. Metallo-β-Lactamase Structure and Function. Ann. N. Y. Acad. Sci. 2013, 1277, 91–104. [Google Scholar] [CrossRef]
- Neu, H.C. Aztreonam Activity, Pharmacology, and Clinical Uses. Am. J. Med. 1990, 88, S2–S6. [Google Scholar] [CrossRef]
- Sykes, R.B.; Bonner, D.P. Aztreonam: The First Monobactam. Am. J. Med. 1985, 78, 2–10. [Google Scholar] [CrossRef]
- Papp-Wallace, K.M.; Endimiani, A.; Taracila, M.A.; Bonomo, R.A. Carbapenems: Past, Present, and Future. Antimicrob. Agents Chemother. 2011, 55, 4943–4960. [Google Scholar] [CrossRef]
- Babic, M.; Hujer, A.M.; Bonomo, R.A. What’s New in Antibiotic Resistance? Focus on Beta-Lactamases. Drug Resist. Updates 2006, 9, 142–156. [Google Scholar] [CrossRef]
- Bush, K.; Fisher, J.F. Epidemiological Expansion, Structural Studies, and Clinical Challenges of New β-Lactamases from Gram-Negative Bacteria. Annu. Rev. Microbiol. 2011, 65, 455–478. [Google Scholar] [CrossRef]
- Ghuysen, J.-M. SERINE β-LACTAMASES AND PENICILLIN-BINDING PROTEINS. Annu. Rev. Microbiol. 1991, 45, 37–67. [Google Scholar] [CrossRef]
- Crowder, M.W.; Spencer, J.; Vila, A.J. Metallo-β-Lactamases: Novel Weaponry for Antibiotic Resistance in Bacteria. Acc. Chem. Res. 2006, 39, 721–728. [Google Scholar] [CrossRef] [PubMed]
- Wang, Z.; Fast, W.; Valentine, A.M.; Benkovic, S.J. Metallo-β-Lactamase: Structure and Mechanism. Curr. Opin. Chem. Biol. 1999, 3, 614–622. [Google Scholar] [CrossRef]
- Tehrani, K.H.M.E.; Martin, N.I. β-Lactam/β-Lactamase Inhibitor Combinations: An Update. Med. Chem. Commun. 2018, 9, 1439–1456. [Google Scholar] [CrossRef]
- Karaiskos, I.; Galani, I.; Papoutsaki, V.; Galani, L.; Giamarellou, H. Carbapenemase Producing Klebsiella Pneumoniae: Implication on Future Therapeutic Strategies. Expert Rev. Anti-Infect. Ther. 2021, 20, 53–69. [Google Scholar] [CrossRef] [PubMed]
- Khanna, N.R.; Gerriets, V. Beta Lactamase Inhibitors. In StatPearls; StatPearls Publishing: Treasure Island, FL, USA, January 2022. Available online: https://www.ncbi.nlm.nih.gov/books/NBK557592/#_NBK557592_pubdet_ (accessed on 8 February 2022).
- El-Gamal, M.I.; Brahim, I.; Hisham, N.; Aladdin, R.; Mohammed, H.; Bahaaeldin, A. Recent Updates of Carbapenem Antibiotics. Eur. J. Med. Chem. 2017, 131, 185–195. [Google Scholar] [CrossRef]
- Maveyraud, L.; Mourey, L.; Kotra, L.P.; Pedelacq, J.-D.; Guillet, V.; Mobashery, S.; Samama, J.-P. Structural Basis for Clinical Longevity of Carbapenem Antibiotics in the Face of Challenge by the Common Class A β-Lactamases from the Antibiotic-Resistant Bacteria. J. Am. Chem. Soc. 1998, 120, 9748–9752. [Google Scholar] [CrossRef]
- Nukaga, M.; Bethel, C.R.; Thomson, J.M.; Hujer, A.M.; Distler, A.; Anderson, V.E.; Knox, J.R.; Bonomo, R.A. Inhibition of Class A Beta-Lactamases by Carbapenems: Crystallographic Observation of Two Conformations of Meropenem in SHV-1. J. Am. Chem. Soc. 2008, 130, 12656–12662. [Google Scholar] [CrossRef]
- Tremblay, L.W.; Fan, F.; Blanchard, J.S. Biochemical and Structural Characterization of Mycobacterium Tuberculosis Beta-Lactamase with the Carbapenems Ertapenem and Doripenem. Biochemistry 2010, 49, 3766–3773. [Google Scholar] [CrossRef]
- Bush, K. Alarming β-Lactamase-Mediated Resistance in Multidrug-Resistant Enterobacteriaceae. Curr. Opin. Microbiol. 2010, 13, 558–564. [Google Scholar] [CrossRef]
- Carcione, D.; Siracusa, C.; Sulejmani, A.; Leoni, V.; Intra, J. Old and New Beta-Lactamase Inhibitors: Molecular Structure, Mechanism of Action, and Clinical Use. Antibiotics 2021, 10, 995. [Google Scholar] [CrossRef]
- Fernández, L.; Hancock, R.E.W. Adaptive and Mutational Resistance: Role of Porins and Efflux Pumps in Drug Resistance. Clin. Microbiol. Rev. 2012, 25, 661–681. [Google Scholar] [CrossRef] [PubMed]
- Li, H.; Luo, Y.-F.; Williams, B.J.; Blackwell, T.S.; Xie, C.-M. Structure and Function of OprD Protein in Pseudomonas Aeruginosa: From Antibiotic Resistance to Novel Therapies. Int. J. Med. Microbiol. 2012, 302, 63–68. [Google Scholar] [CrossRef]
- Ayoub Moubareck, C.; Hammoudi Halat, D. Insights into Acinetobacter Baumannii: A Review of Microbiological, Virulence, and Resistance Traits in a Threatening Nosocomial Pathogen. Antibiotics 2020, 9, 119. [Google Scholar] [CrossRef] [PubMed]
- Moyá, B.; Beceiro, A.; Cabot, G.; Juan, C.; Zamorano, L.; Alberti, S.; Oliver, A. Pan-β-Lactam Resistance Development in Pseudomonas Aeruginosa Clinical Strains: Molecular Mechanisms, Penicillin-Binding Protein Profiles, and Binding Affinities. Antimicrob. Agents Chemother. 2012, 56, 4771–4778. [Google Scholar] [CrossRef] [PubMed]
- Yamachika, S.; Sugihara, C.; Kamai, Y.; Yamashita, M. Correlation between Penicillin-Binding Protein 2 Mutations and Carbapenem Resistance in Escherichia Coli. J. Med. Microbiol. 2013, 62, 429–436. [Google Scholar] [CrossRef]
- World Health Organization. Global Priority List of Antibiotic-Resistant Bacteria to Guide Research, Discovery, and Development of New Antibiotics. Available online: https://www.who.int/news-room/detail/27-02-2017-who-publishes-list-of-bacteria-for-which-new-antibiotics-are-urgently-needed (accessed on 10 February 2022).
- Olsen, I. New Promising β-Lactamase Inhibitors for Clinical Use. Eur. J. Clin. Microbiol. Infect. Dis. 2015, 34, 1303–1308. [Google Scholar] [CrossRef]
- González-Bello, C.; Rodríguez, D.; Pernas, M.; Rodríguez, Á.; Colchón, E. β-Lactamase Inhibitors To Restore the Efficacy of Antibiotics against Superbugs. J. Med. Chem. 2020, 63, 1859–1881. [Google Scholar] [CrossRef]
- Wang, T.; Xu, K.; Zhao, L.; Tong, R.; Xiong, L.; Shi, J. Recent Research and Development of NDM-1 Inhibitors. Eur. J. Med. Chem. 2021, 223, 113667. [Google Scholar] [CrossRef]
- Ambler, R.P.; Coulson, A.F.; Frère, J.M.; Ghuysen, J.M.; Joris, B.; Forsman, M.; Levesque, R.C.; Tiraby, G.; Waley, S.G. A Standard Numbering Scheme for the Class A β-Lactamases. Biochem. J. 1991, 276, 269–270. [Google Scholar] [CrossRef]
- Rotondo, C.M.; Wright, G.D. Inhibitors of metallo-β-lactamases. Curr. Opin. Microbiol. 2017, 39, 96–105. [Google Scholar] [CrossRef]
- Dahiya, S.; Singla, P.; Chaudhary, U.; Singh, B. Prevalence of Klebsiella pneumoniae Carbapenemase (KPC), Metallo Beta Lactamases and AmpC beta Lactamases in Clinical Isolates of Klebsiella Species. Int. J. Curr. Microbiol. Appl. Sci. 2015, 4, 170. [Google Scholar]
- Sonda, T.; Kumburu, H.; van Zwetselaar, M.; Alifrangis, M.; Lund, O.; Kibiki, G.; Aarestrup, F.M. Meta-Analysis of Proportion Estimates of Extended-Spectrum-Beta-Lactamase-Producing Enterobacteriaceae in East Africa Hospitals. Antimicrob. Resist. Infect. Control 2016, 5, 18. [Google Scholar] [CrossRef] [PubMed]
- Onduru, O.G.; Mkakosya, R.S.; Aboud, S.; Rumisha, S.F. Genetic Determinants of Resistance among ESBL-Producing Enterobacteriaceae in Community and Hospital Settings in East, Central, and Southern Africa: A Systematic Review and Meta-Analysis of Prevalence. Can. J. Infect. Dis. Med. Microbiol. 2021, 2021, 5153237. [Google Scholar] [CrossRef]
- Varela, M.F.; Stephen, J.; Lekshmi, M.; Ojha, M.; Wenzel, N.; Sanford, L.M.; Hernandez, A.J.; Parvathi, A.; Kumar, S.H. Bacterial Resistance to Antimicrobial Agents. Antibiotics 2021, 10, 593. [Google Scholar] [CrossRef] [PubMed]
- Delgado, D.Y.C.; Barrigas, Z.P.T.; Astutillo, S.G.O.; Jaramillo, A.P.A.; Ausili, A. Detection and Molecular Characterization of β-Lactamase Genes in Clinical Isolates of Gram-Negative Bacteria in Southern Ecuador. Braz. J. Infect. Dis. 2016, 20, 627–630. [Google Scholar] [CrossRef]
- Poirel, L.; Naas, T.; Nordmann, P. Diversity, Epidemiology, and Genetics of Class D β-Lactamases. Antimicrob. Agents Chemother. 2010, 54, 24–38. [Google Scholar] [CrossRef]
- Evans, B.A.; Amyes, S.G.B. OXA β-Lactamases. Clin. Microbiol. Rev. 2014, 27, 241–263. [Google Scholar] [CrossRef]
- Jeon, J.H.; Lee, J.H.; Lee, J.J.; Park, K.S.; Karim, A.M.; Lee, C.-R.; Jeong, B.C.; Lee, S.H. Structural Basis for Carbapenem-Hydrolyzing Mechanisms of Carbapenemases Conferring Antibiotic Resistance. Int. J. Mol. Sci. 2015, 16, 9654–9692. [Google Scholar] [CrossRef]
- Boyd, S.E.; Livermore, D.M.; Hooper, D.C.; Hope, W.W. Metallo-β-Lactamases: Structure, Function, Epidemiology, Treatment Options, and the Development Pipeline. Antimicrob. Agents Chemother. 2020, 64, e00397-20. [Google Scholar] [CrossRef]
- Garau, G.; García-Sáez, I.; Bebrone, C.; Anne, C.; Mercuri, P.; Galleni, M.; Frère, J.-M.; Dideberg, O. Update of the Standard Numbering Scheme for Class B Beta-Lactamases. Antimicrob. Agents Chemother. 2004, 48, 2347–2349. [Google Scholar] [CrossRef]
- Poirel, L.; Lagrutta, E.; Taylor, P.; Pham, J.; Nordmann, P. Emergence of Metallo-β-Lactamase NDM-1-Producing Multidrug-Resistant Escherichia Coli in Australia. Antimicrob. Agents Chemother. 2010, 54, 4914–4916. [Google Scholar] [CrossRef] [PubMed]
- Guo, Y.; Wang, J.; Niu, G.; Shui, W.; Sun, Y.; Zhou, H.; Zhang, Y.; Yang, C.; Lou, Z.; Rao, Z. A structural view of the antibiotic degradation enzyme NDM-1 from a superbug. Protein Cell. 2011, 2, 384–394. [Google Scholar] [CrossRef] [PubMed]
- Thomas, P.W.; Zheng, M.; Wu, S.; Guo, H.; Liu, D.; Xu, D.; Fast, W. Characterization of Purified New Delhi Metallo-β-Lactamase-1. Biochemistry 2011, 50, 10102–10113. [Google Scholar] [CrossRef]
- Gibb, A.P.; McCallum, A.K. New Delhi Metallo-β-Lactamase 1. Lancet Infect. Dis. 2010, 10, 751–752. [Google Scholar] [CrossRef]
- Drawz, S.M.; Bonomo, R.A. Three Decades of β-Lactamase Inhibitors. Clin. Microbiol. Rev. 2010, 23, 160–201. [Google Scholar] [CrossRef] [PubMed]
- Shahid, M.; Sobia, F.; Singh, A.; Malik, A.; Khan, H.M.; Jonas, D.; Hawkey, P.M. Beta-Lactams and Beta-Lactamase-Inhibitors in Current- or Potential-Clinical Practice: A Comprehensive Update. Crit. Rev. Microbiol. 2009, 35, 81–108. [Google Scholar] [CrossRef]
- Hazra, S.; Xu, H.; Blanchard, J.S. Tebipenem, a New Carbapenem Antibiotic, Is a Slow Substrate That Inhibits the β-Lactamase from Mycobacterium Tuberculosis. Biochemistry 2014, 53, 3671–3678. [Google Scholar] [CrossRef]
- FDA Approves New Treatment for Complicated Urinary Tract and Complicated Intra-Abdominal Infections. Food and Drug Administration. 17 July 2019. Available online: https://www.fda.gov/news-events/press-announcements/fda-approves-new-treatment-complicated-urinary-tract-and-complicated-intra-abdominal-infections#:~:text=The%20U.S.%20Food%20and%20Drug%20Administration%20has%20approved,tract%20infections%20%28cUTI%29%20and%20complicated%20intra-abdominal%20infections%20%28cIAI%29 (accessed on 10 February 2022).
- Cilastatin/Imipenem/Relebactam. AdisInsight. Springer International Publishing AG. Retrieved 29 April 2016. Available online: https://adisinsight.springer.com/drugs/800042881 (accessed on 10 February 2022).
- FDA Approves New Antibacterial Drug (Press Release). Food and Drug Administration. 29 August 2017. Available online: https://www.pressreleasepoint.com/fda-approves-new-antibacterial-drug (accessed on 10 February 2022).
- Lahiri, S.D.; Mangani, S.; Durand-Reville, T.; Benvenuti, M.; Luca, F.D.; Sanyal, G.; Docquier, J.-D. Structural Insight into Potent Broad-Spectrum Inhibition with Reversible Recyclization Mechanism: Avibactam in Complex with CTX-M-15 and Pseudomonas Aeruginosa AmpC β-Lactamases. Antimicrob. Agents Chemother. 2013, 57, 2496–2505. [Google Scholar] [CrossRef]
- Drug Banck Online. Clavulanic Acid: Uses, Interactions, Mechanism of Action. Available online: https://go.drugbank.com/drugs/DB00766 (accessed on 10 February 2022).
- Saudagar, P.S.; Survase, S.A.; Singhal, R.S. Clavulanic Acid: A Review. Biotechnol. Adv. 2008, 26, 335–351. [Google Scholar] [CrossRef]
- Drug Banck Online. Sulbactam: Uses, Interactions, Mechanism of Action. Available online: https://go.drugbank.com/drugs/DB09324 (accessed on 10 February 2022).
- Totir, M.A.; Helfand, M.S.; Carey, M.P.; Sheri, A.; Buynak, J.D.; Bonomo, R.A.; Carey, P.R. Sulbactam Forms Only Minimal Amounts of Irreversible Acrylate-Enzyme with SHV-1 β-Lactamase. Biochemistry 2007, 46, 8980–8987. [Google Scholar] [CrossRef]
- Helfand, M.S.; Totir, M.A.; Carey, M.P.; Hujer, A.M.; Bonomo, R.A.; Carey, P.R. Following the Reactions of Mechanism-Based Inhibitors with β-Lactamase by Raman Crystallography. Biochemistry 2003, 42, 13386–13392. [Google Scholar] [CrossRef]
- Drug Banck Online. Tazobactam: Uses, Interactions, Mechanism of Action. Available online: https://go.drugbank.com/drugs/DB01606 (accessed on 10 February 2022).
- Papp-Wallace, K.M.; Bethel, C.R.; Caillon, J.; Barnes, M.D.; Potel, G.; Bajaksouzian, S.; Rutter, J.D.; Reghal, A.; Shapiro, S.; Taracila, M.A.; et al. Beyond Piperacillin-Tazobactam: Cefepime and AAI101 as a Potent β-Lactam-β-Lactamase Inhibitor Combination. Antimicrob. Agents Chemother. 2019, 63, e00105-19. [Google Scholar] [CrossRef] [PubMed]
- Vázquez-Ucha, J.C.; Arca-Suárez, J.; Bou, G.; Beceiro, A. New Carbapenemase Inhibitors: Clearing the Way for the β-Lactams. Int. J. Mol. Sci. 2020, 21, 9308. [Google Scholar] [CrossRef] [PubMed]
- Tebipenem. Available online: https://en.wikipedia.org/wiki/Tebipenem (accessed on 10 February 2022).
- Gallagher, G.M. Positive Results for Cefepime-Enmetazobactam in Phase 3 Trial. 28 February 2020. Available online: https://www.contagionlive.com/view/positive-results-for-cefepimeenmetazobactam-in-phase-3-trial (accessed on 10 February 2022).
- Crandon, J.L.; Nicolau, D.P. In Vitro Activity of Cefepime/AAI101 and Comparators against Cefepime Non-Susceptible Enterobacteriaceae. Pathogens 2015, 4, 620–625. [Google Scholar] [CrossRef] [PubMed]
- Morrissey, I.; Magnet, S.; Hawser, S.; Shapiro, S.; Knechtle, P. In Vitro Activity of Cefepime-Enmetazobactam against Gram-Negative Isolates Collected from U.S. and European Hospitals during 2014-2015. Antimicrob. Agents Chemother. 2019, 63, e00514-19. [Google Scholar] [CrossRef]
- Crandon, J.L.; Nicolau, D.P. In Vivo Activities of Simulated Human Doses of Cefepime and Cefepime-AAI101 against Multidrug-Resistant Gram-Negative Enterobacteriaceae. Antimicrob. Agents Chemother. 2015, 59, 2688–2694. [Google Scholar] [CrossRef]
- Weiss, W.J.; Petersen, P.J.; Murphy, T.M.; Tardio, L.; Yang, Y.; Bradford, P.A.; Venkatesan, A.M.; Abe, T.; Isoda, T.; Mihira, A.; et al. In Vitro and In Vivo Activities of Novel 6-Methylidene Penems as β-Lactamase Inhibitors. Antimicrob. Agents Chemother. 2004, 48, 4589–4596. [Google Scholar] [CrossRef]
- ProbeChem. LN-1-255. Available online: http://www.probechem.com/products_LN-1-255.aspx (accessed on 10 February 2022).
- Vázquez-Ucha, J.C.; Martínez-Guitián, M.; Maneiro, M.; Conde-Pérez, K.; Álvarez-Fraga, L.; Torrens, G.; Oliver, A.; Buynak, J.D.; Bonomo, R.A.; Bou, G.; et al. Therapeutic Efficacy of LN-1-255 in Combination with Imipenem in Severe Infection Caused by Carbapenem-Resistant Acinetobacter Baumannii. Antimicrob. Agents Chemother. 2019, 63, e01092-19. [Google Scholar] [CrossRef]
- Rodríguez, D.; Maneiro, M.; Vázquez-Ucha, J.C.; Beceiro, A.; González-Bello, C. 6-Arylmethylidene Penicillin-Based Sulfone Inhibitors for Repurposing Antibiotic Efficiency in Priority Pathogens. J. Med. Chem. 2020, 63, 3737–3755. [Google Scholar] [CrossRef]
- Drug Banck Online. Avibactam: Uses, Interactions, Mechanism of Action. Available online: https://go.drugbank.com/drugs/DB09060 (accessed on 10 February 2022).
- Livermore, D.M.; Meunier, D.; Hopkins, K.L.; Doumith, M.; Hill, R.; Pike, R.; Staves, P.; Woodford, N. Activity of Ceftazidime/Avibactam against Problem Enterobacteriaceae and Pseudomonas Aeruginosa in the UK, 2015–2016. J. Antimicrob. Chemother. 2018, 73, 648–657. [Google Scholar] [CrossRef]
- Ehmann, D.E.; Jahić, H.; Ross, P.L.; Gu, R.-F.; Hu, J.; Durand-Réville, T.F.; Lahiri, S.; Thresher, J.; Livchak, S.; Gao, N.; et al. Kinetics of Avibactam Inhibition against Class A, C, and D β-Lactamases. J. Biol. Chem. 2013, 288, 27960–27971. [Google Scholar] [CrossRef] [PubMed]
- Shirley, M. Ceftazidime-Avibactam: A Review in the Treatment of Serious Gram-Negative Bacterial Infections. Drugs 2018, 78, 675–692. [Google Scholar] [CrossRef] [PubMed]
- Karlowsky, J.A.; Kazmierczak, K.M.; de Jonge, B.L.M.; Hackel, M.A.; Sahm, D.F.; Bradford, P.A. In Vitro Activity of Aztreonam-Avibactam against Enterobacteriaceae and Pseudomonas Aeruginosa Isolated by Clinical Laboratories in 40 Countries from 2012 to 2015. Antimicrob. Agents Chemother. 2017, 61, e00472-17. [Google Scholar] [CrossRef] [PubMed]
- Shields, R.K.; Doi, Y. Aztreonam Combination Therapy: An Answer to Metallo-β-Lactamase–Producing Gram-Negative Bacteria? Clin. Infect. Dis. 2020, 71, 1099–1101. [Google Scholar] [CrossRef] [PubMed]
- Lee, M.; Abbey, T.; Biagi, M.; Wenzler, E. Activity of Aztreonam in Combination with Ceftazidime-Avibactam against Serine- and Metallo-β-Lactamase-Producing Pseudomonas Aeruginosa. Diagn. Microbiol. Infect. Dis. 2020, 99, 115227. [Google Scholar] [CrossRef]
- Drug Banck Online. Relebactam: Uses, Interactions, Mechanism of Action. Available online: https://go.drugbank.com/drugs/DB12377 (accessed on 10 February 2022).
- Campanella, T.A.; Gallagher, J.C. A Clinical Review and Critical Evaluation of Imipenem—Relebactam: Evidence to Date. Infect. Drug Resist. 2020, 13, 4297–4308. [Google Scholar] [CrossRef]
- McCarthy, M.W. Clinical Pharmacokinetics and Pharmacodynamics of Imipenem_Cilastatin/Relebactam Combination Therapy. Clin. Pharmacokinet. 2020, 59, 567–573. [Google Scholar] [CrossRef]
- PubChem. Zidebactam. Available online: https://pubchem.ncbi.nlm.nih.gov/compound/77846445 (accessed on 10 February 2022).
- Drug Banck Online. Zidebactam: Uses, Interactions, Mechanism of Action. Available online: https://go.drugbank.com/drugs/DB13090 (accessed on 10 February 2022).
- Karlowsky, J.A.; Hackel, M.A.; Bouchillon, S.K.; Sahm, D.F. In Vitro Activity of WCK 5222 (Cefepime-Zidebactam) against Worldwide Collected Gram-Negative Bacilli Not Susceptible to Carbapenems. Antimicrob. Agents Chemother. 2020, 64, e01432-20. [Google Scholar] [CrossRef]
- Preston, R.A.; Mamikonyan, G.; DeGraff, S.; Chiou, J.; Kemper, C.J.; Xu, A.; Mastim, M.; Yeole, R.; Chavan, R.; Patel, A.; et al. Single-Center Evaluation of the Pharmacokinetics of WCK 5222 (Cefepime-Zidebactam Combination) in Subjects with Renal Impairment. Antimicrob. Agents Chemother. 2018, 63, e01484-18. [Google Scholar] [CrossRef]
- Drug Banck Online. Durlobactam: Uses, Interactions, Mechanism of Action. Available online: https://go.drugbank.com/drugs/DB16704 (accessed on 10 February 2022).
- Shapiro, A.B.; Gao, N.; Jahić, H.; Carter, N.M.; Chen, A.; Miller, A.A. Reversibility of Covalent, Broad-Spectrum Serine β-Lactamase Inhibition by the Diazabicyclooctenone ETX2514. ACS Infect. Dis. 2017, 3, 833–844. [Google Scholar] [CrossRef]
- McLeod, S.M.; Shapiro, A.B.; Moussa, S.H.; Johnstone, M.; McLaughlin, R.E.; de Jonge, B.L.M.; Miller, A.A. Frequency and Mechanism of Spontaneous Resistance to Sulbactam Combined with the Novel β-Lactamase Inhibitor ETX2514 in Clinical Isolates of Acinetobacter Baumannii. Antimicrob. Agents Chemother. 2018, 62, e01576-17. [Google Scholar] [CrossRef] [PubMed]
- Sagan, O.; Yakubsevitch, R.; Yanev, K.; Fomkin, R.; Stone, E.; Hines, D.; O’Donnell, J.; Miller, A.; Isaacs, R.; Srinivasan, S. Pharmacokinetics and Tolerability of Intravenous Sulbactam-Durlobactam with Imipenem-Cilastatin in Hospitalized Adults with Complicated Urinary Tract Infections, Including Acute Pyelonephritis. Antimicrob. Agents Chemother. 2020, 64, e01506-19. [Google Scholar] [CrossRef] [PubMed]
- Drug Banck Online. Nacubactam: Uses, Interactions, Mechanism of Action. Available online: https://go.drugbank.com/drugs/DB15353 (accessed on 10 February 2022).
- Mushtaq, S.; Vickers, A.; Woodford, N.; Haldimann, A.; Livermore, D.M. Activity of Nacubactam (RG6080/OP0595) Combinations against MBL-Producing Enterobacteriaceae. J. Antimicrob. Chemother. 2018, 74, 953–960. [Google Scholar] [CrossRef]
- Okujava, R.; Garcia-Alcalde, F.; Haldimann, A.; Zampaloni, C.; Morrissey, I.; Magnet, S.; Kothari, N.; Harding, I.; Bradley, K. 1359. Activity of Meropenem/Nacubactam Combination against Gram-Negative Clinical Isolates: ROSCO Global Surveillance 2017. Open Forum Infect. Dis. 2018, 5, S416. [Google Scholar] [CrossRef]
- Asempa, T.E.; Motos, A.; Abdelraouf, K.; Bissantz, C.; Zampaloni, C.; Nicolau, D.P. Meropenem–Nacubactam Activity against AmpC-Overproducing and KPC-Expressing Pseudomonas Aeruginosa in a Neutropenic Murine Lung Infection Model. Int. J. Antimicrob. Agents 2020, 55, 105838. [Google Scholar] [CrossRef]
- Mallalieu, N.L.; Winter, E.; Fettner, S.; Patel, K.; Zwanziger, E.; Attley, G.; Rodriguez, I.; Kano, A.; Salama, S.M.; Mallalieu, N.L.; et al. Safety and Pharmacokinetic Characterization of Nacubactam, a Novel β-Lactamase Inhibitor, Alone and in Combination with Meropenem, in Healthy Volunteers. Antimicrob. Agents Chemother. 2020, 64, e02229-19. [Google Scholar] [CrossRef]
- MedKoo Bioscience Inc. EDX1317 Sodium. Available online: https://medkoo.com/products/30175 (accessed on 10 February 2022).
- MedKoo Bioscience Inc. EDX0282. Available online: https://www.medkoo.com/products/30174 (accessed on 10 February 2022).
- Durand-Réville, T.F.; Comita-Prevoir, J.; Zhang, J.; Wu, X.; May-Dracka, T.L.; Romero, J.A.C.; Wu, F.; Chen, A.; Shapiro, A.B.; Carter, N.M.; et al. Discovery of an Orally Available Diazabicyclooctane Inhibitor (ETX0282) of Class A, C, and D Serine β-Lactamases. J. Med. Chem. 2020, 63, 12511–12525. [Google Scholar] [CrossRef]
- Miller, A.A.; Shapiro, A.B.; McLeod, S.M.; Carter, N.M.; Moussa, S.H.; Tommasi, R.; Mueller, J.P. In Vitro Characterization of ETX1317, a Broad-Spectrum β-Lactamase Inhibitor That Restores and Enhances β-Lactam Activity against Multi-Drug-Resistant Enterobacteriales, Including Carbapenem-Resistant Strains. ACS Infect. Dis. 2020, 6, 1389–1397. [Google Scholar] [CrossRef]
- Thomas Durand-Réville. Entasis Therapeutic. ETX0282, a Novel Oral Agent against Multidrug-Resistant Enterobacteriaceae. Available online: https://www.entasistx.com/application/files/9815/1846/7744/ETX0282-ASM-Microbe-2017.pdf (accessed on 10 February 2022).
- MedKoo Bioscience Inc. WCK-5153. Available online: https://www.medkoo.com/products/18787 (accessed on 10 February 2022).
- Papp-Wallace, K.M.; Nguyen, N.Q.; Jacobs, M.R.; Bethel, C.R.; Barnes, M.D.; Kumar, V.; Bajaksouzian, S.; Rudin, S.D.; Rather, P.N.; Bhavsar, S.; et al. Strategic Approaches to Overcome Resistance against Gram-Negative Pathogens Using β-Lactamase Inhibitors and β-Lactam Enhancers: Activity of Three Novel Diazabicyclooctanes WCK 5153, Zidebactam (WCK 5107), and WCK 4234. J. Med. Chem. 2018, 61, 4067–4086. [Google Scholar] [CrossRef]
- MedKoo Bioscience Inc. WCK-4232 Sodium. Available online: https://www.medkoo.com/products/18790 (accessed on 10 February 2022).
- Mushtaq, S.; Vickers, A.; Woodford, N.; Livermore, D.M. WCK 4234, a Novel Diazabicyclooctane Potentiating Carbapenems against Enterobacteriaceae, Pseudomonas and Acinetobacter with Class A, C and D β-Lactamases. J. Antimicrob. Chemother. 2017, 72, 1688–1695. [Google Scholar] [CrossRef][Green Version]
- MedKoo Bioscience Inc. ANT3310. Available online: https://www.medkoo.com/products/42472 (accessed on 10 February 2022).
- Antabio Receives FDA Qualified Infectious Disease Product (QIDP) Designation for MEM-ANT3310, a Novel Broad-Spectrum Combination Therapy Targeting WHO’s Priority Pathogens. Available online: https://antabio.com/2020/05/06/antabio-receives-fda-qualified-infectious-disease-product-qidp-designation-for-mem-ant3310-a-novel-broad-spectrum-combination-therapy-targeting-whos-priority-pathogens/ (accessed on 10 February 2022).
- MedChemExpress. GT-055 (LCB18-055). Available online: https://www.medchemexpress.com/gt-055.html (accessed on 10 February 2022).
- Nguyen, L.P.; Pinto, N.A.; Vu, T.N.; Lee, H.; Cho, Y.L.; Byun, J.-H.; D’Souza, R.; Yong, D. In Vitro Activity of a Novel Siderophore-Cephalosporin, GT-1 and Serine-Type β-Lactamase Inhibitor, GT-055, against Escherichia Coli, Klebsiella Pneumoniae and Acinetobacter Spp. Panel Strains. Antibiotics 2020, 9, 267. [Google Scholar] [CrossRef] [PubMed]
- Halasohoris, S.A.; Scarff, J.M.; Pysz, L.M.; Lembirik, S.; Lemmon, M.M.; Biek, D.; Hannah, B.; Zumbrun, S.D.; Panchal, R.G. In Vitro and in Vivo Activity of GT-1, a Novel Siderophore Cephalosporin, and GT-055, a Broad-Spectrum β-Lactamase Inhibitor, against Biothreat and ESKAPE Pathogens. J. Antibiot. 2021, 74, 884–892. [Google Scholar] [CrossRef]
- Drug Banck Online. Vaborbactam: Uses, Interactions, Mechanism of Action. Available online: https://go.drugbank.com/drugs/DB12107 (accessed on 10 February 2022).
- Hecker, S.J.; Reddy, K.R.; Totrov, M.; Hirst, G.C.; Lomovskaya, O.; Griffith, D.C.; King, P.; Tsivkovski, R.; Sun, D.; Sabet, M.; et al. Discovery of a Cyclic Boronic Acid β-Lactamase Inhibitor (RPX7009) with Utility vs. Class A Serine Carbapenemases. J. Med. Chem. 2015, 58, 3682–3692. [Google Scholar] [CrossRef] [PubMed]
- Griffith, D.C.; Loutit, J.S.; Morgan, E.E.; Durso, S.; Dudley, M.N. Phase 1 Study of the Safety, Tolerability, and Pharmacokinetics of the β-Lactamase Inhibitor Vaborbactam (RPX7009) in Healthy Adult Subjects. Antimicrob. Agents Chemother. 2016, 60, 6326–6332. [Google Scholar] [CrossRef]
- Griffith, D.C.; Rubino, C.M.; Loutit, J.S.; Morgan, E.E.; White, D.; Dudley, M.N. Single-Dose Pharmacokinetics and Safety of Meropenem-Vaborbactam in Subjects with Chronic Renal Impairment. Antimicrob. Agents Chemother. 2018, 62, e02103-17. [Google Scholar]
- Kaye, K.S.; Bhowmick, T.; Metallidis, S.; Bleasdale, S.C.; Sagan, O.S.; Stus, V.; Vazquez, J.; Zaitsev, V.; Bidair, M.; Chorvat, E.; et al. Effect of Meropenem-Vaborbactam vs. Piperacillin-Tazobactam on Clinical Cure or Improvement and Microbial Eradication in Complicated Urinary Tract Infection: The TANGO I Randomized Clinical Trial. J. Am. Med. Assoc. 2018, 319, 788–799. [Google Scholar] [CrossRef] [PubMed]
- Wunderink, R.G.; Giamarellos-Bourboulis, E.J.; Rahav, G.; Mathers, A.J.; Bassetti, M.; Vazquez, J.; Cornely, O.A.; Solomkin, J.; Bhowmick, T.; Bishara, J.; et al. Effect and Safety of Meropenem–Vaborbactam versus Best-Available Therapy in Patients with Carbapenem-Resistant Enterobacteriaceae Infections: The TANGO II Randomized Clinical Trial. Infect. Dis. Ther. 2018, 7, 439–455. [Google Scholar] [CrossRef]
- Drug Banck Online. Taniborbactam: Uses, Interactions, Mechanism of Action. Available online: https://go.drugbank.com/drugs/DB16338 (accessed on 10 February 2022).
- Hamrick, J.C.; Docquier, J.-D.; Uehara, T.; Myers, C.L.; Six, D.A.; Chatwin, C.L.; John, K.J.; Vernacchio, S.F.; Cusick, S.M.; Trout, R.E.L.; et al. VNRX-5133 (Taniborbactam), a Broad-Spectrum Inhibitor of Serine- and Metallo-β-Lactamases, Restores Activity of Cefepime in Enterobacterales and Pseudomonas aeruginosa. Antimicrob. Agents Chemother. 2020, 64, e01963-19. [Google Scholar] [CrossRef]
- Dowell, J.A.; Dickerson, D.; Henkel, T. Safety and Pharmacokinetics in Human Volunteers of Taniborbactam (VNRX-5133), a Novel Intravenous β-Lactamase Inhibitor. Antimicrob. Agents Chemother. 2021, 65, e01053-21. [Google Scholar] [CrossRef]
- Venatorx Pharmaceuticals. Cefepime-taniborbactam. Available online: https://www.venatorx.com/cefepime-taniborbactam/ (accessed on 10 February 2022).
- Castro, A.M. Drugs Approval International. VNRX-7145. Available online: http://drugapprovalsint.com/vnrx-7145/ (accessed on 10 February 2022).
- Trout, R.E.; Zulli, A.; Mesaros, E.; Jackson, R.W.; Boyd, S.; Liu, B.; Hamrick, J.; Daigle, D.; Chatwin, C.L.; John, K.; et al. Discovery of VNRX-7145 (VNRX-5236 Etzadroxil): An Orally Bioavailable β-Lactamase Inhibitor for Enterobacterales Expressing Ambler Class A, C, and D Enzymes. J. Med. Chem. 2021, 64, 10155–10166. [Google Scholar] [CrossRef]
- Venatorx Pharmaceuticals. Ceftibuten/VNRX-7145. Available online: https://www.venatorx.com/ceftibuten-vnrx-7145 (accessed on 10 February 2022).
- MedKoo Bioscience Inc. QPX7728. Available online: https://www.medkoo.com/products/37690 (accessed on 10 February 2022).
- Nelson, K.; Rubio-Aparicio, D.; Sun, D.; Dudley, M.; Lomovskaya, O. In Vitro Activity of the Ultrabroad-Spectrum-Beta-Lactamase Inhibitor QPX7728 against Carbapenem-Resistant Enterobacterales with Varying Intrinsic and Acquired Resistance Mechanisms. Antimicrob. Agents Chemother. 2020, 64, e00757-20. [Google Scholar] [CrossRef] [PubMed]
- Lomovskaya, O.; Nelson, K.J.; Rubio-Aparicio, D.; Tsivkovski, R.; Sun, D.; Dudley, M.N. Impact of Intrinsic Resistance Mechanisms on Potency of QPX7728, a New Ultrabroad-Spectrum Beta-Lactamase Inhibitor of Serine and Metallo-Beta-Lactamases in Enterobacteriaceae, Pseudomonas Aeruginosa, and Acinetobacter Baumannii. Antimicrob. Agents Chemother. 2020, 64, e00552-20. [Google Scholar] [CrossRef] [PubMed]
- Qpex Biopharma Initiates Phase 1 Clinical Trial of QPX7728 for Drug-Resistant Bacterial Infections. Available online: https://pipelinereview.com/index.php/2020120476731/Small-Molecules/Qpex-Biopharma-Initiates-Phase-1-Clinical-Trial-of-QPX7728-for-Drug-Resistant-Bacterial-Infections.html (accessed on 10 February 2022).
- Sabet, M.; Tarazi, Z.; Griffith, D.C. In Vivo Activity of QPX7728, an Ultrabroad-Spectrum Beta-Lactamase Inhibitor, in Combination with Beta-Lactams against Carbapenem-Resistant Klebsiella Pneumoniae. Antimicrob. Agents Chemother. 2020, 64, e01267-20. [Google Scholar] [CrossRef] [PubMed]
- Davies, D.T.; Leiris, S.; Zalacain, M.; Sprynski, N.; Castandet, J.; Bousquet, J.; Lozano, C.; Llanos, A.; Alibaud, L.; Vasa, S.; et al. Discovery of ANT3310, a Novel Broad-Spectrum Serine β-Lactamase Inhibitor of the Diazabicyclooctane Class, Which Strongly Potentiates Meropenem Activity against Carbapenem-Resistant Enterobacterales and Acinetobacter Baumannii. J. Med. Chem. 2020, 63, 15802–15820. [Google Scholar] [CrossRef]
- Adis Insights. ANT 2681. Available online: https://adisinsight.springer.com/drugs/800038680 (accessed on 10 February 2022).
- Das, S.; Johnson, A.; McEntee, L.; Farrington, N.; Kirby, A.; Unsworth, J.; Jimenez-Valverde, A.; Kolamunnage-Dona, R.; Bousquet, J.; Alibaud, L.; et al. Pharmacodynamics of the Novel Metallo-c-Lactamase Inhibitor ANT2681 in Combination with Meropenem for the Treatment of Infections Caused by NDM-Producing Enterobacteriaceae. Antimicrob. Agents Chemother. 2020, 64, e01076-20. [Google Scholar] [CrossRef]
- Zalacain, M.; Lozano, C.; Llanos, A.; Sprynski, N.; Valmont, T.; Piano, C.D.; Davies, D.; Leiris, S.; Sable, C.; Ledoux, A.; et al. Novel Specific Metallo-β-Lactamase Inhibitor ANT2681 Restores Meropenem Activity to Clinically Effective Levels against NDM-Positive Enterobacterales. Antimicrob. Agents Chemother. 2021, 65, e00203-21. [Google Scholar] [CrossRef]
- Augmentin®. Available online: https://www.bing.com/search?q=Augmentin%C2%AE&pc=0ADS&ptag=C7N3516A308CE7CCFF&form=CONBNT&conlogo=CT3210127 (accessed on 10 February 2022).
- Timentin®. Available online: https://www.torrinomedica.it/schede-farmaci/timentin_3000_mg___200_mg/ (accessed on 10 February 2022).
- Clavucar®. Available online: https://www.torrinomedica.it/schede-farmaci/clavucar/ (accessed on 10 February 2022).
- Zosyn®. Available online: https://www.pfizermedicalinformation.com/en-us/zosyn/dosage-admin (accessed on 10 February 2022).
- Zerbaxa®. Available online: https://www.torrinomedica.it/schede-farmaci/Zerbaxa/ (accessed on 10 February 2022).
- Unasyn®. Available online: https://www.my-personaltrainer.it/Foglietti-illustrativi/Unasyn.html (accessed on 10 February 2022).
- Sultamicillin®. Available online: https://www.mims.com/philippines/drug/info/sultamicillin (accessed on 10 February 2022).
- Sulperazon®. Available online: https://omedicine.info/it/sulperazon.html (accessed on 10 February 2022).
- Recarbrio®. Available online: https://www.torrinomedica.it/schede-farmaci/recarbrio/ (accessed on 10 February 2022).
- Avycaz®. Available online: https://www.avycaz.com/ (accessed on 10 February 2022).
- Zavicefta®. Available online: https://www.torrinomedica.it/schede-farmaci/zavicefta/ (accessed on 10 February 2022).
- Vaborem®. Available online: https://www.torrinomedica.it/schede-farmaci/vaborem/ (accessed on 10 February 2022).
- Song, J.Y.; Jensen, S.E.; Lee, K.J. Clavulanic Acid Biosynthesis and Genetic Manipulation for Its Overproduction. Appl. Microbiol. Biotechnol. 2010, 88, 659–669. [Google Scholar] [CrossRef]
- Chen, J.; Zhang, X. Method for Preparing Sulbactam Acid. Faming Zhuanli Shenqing CN 109705142, 3 May 2019. [Google Scholar]
- Qin, S. Method for Synthesizing Tazobactam. Faming Zhuanli Shenqing CN 110357903, 4 September 2020. [Google Scholar]
- Zhou, S.; Xin, Y.; Wang, J.; Wu, C.; Sun, T. Application of Continuous Flow in Tazobactam Synthesis. Org. Process Res. Dev. 2021, 25, 1648–1657. [Google Scholar] [CrossRef]
- Peng, D.-M.; Li, Y.-X.; Liu, Y.-F.; Lu, M.-F.; Wang, F.-D. Synthesis of tebipenem pivoxil. Zhongguo Kangshengsu Zazhi 2013, 38, 41–43. [Google Scholar]
- Udayampalayam Palanisamy, S.; Gnanaprakasam, A.; Ganapathy, P.; Gohain, M.; Hariharan, V.; Rajagopal, S.; Paul-Satyaseela, M.; Solanki, S.S.; Devarajan, S. Preparation of 2-Substituted Methyl Penam Derivatives for the Treatment of Bacterial Infections. U.S. Patent Applications Publication No. US 20080015156 A1, 17 January 2008. [Google Scholar]
- Udayampalayam Palanisamy, S.; Paul-Satyaseela, M.; Shridhar, N.; Gopalan, B.; Aravind, A.; Senthilnathan, M.; Hariharan, P. β-Lactamase Inhibitors and Their Use as Antimicrobial Agents. PCT International Applications No. WO 2012070071 A1, 31 May 2012. [Google Scholar]
- Faini, A.; Forzatti, M.; Fogliato, G.; Biondi, S. Method of Forming Methylpenam Triazolyl Derivatives as β-Lactamase Inhibitors. PCT International Applications No. WO 2015173378 A2, 19 November 2015. [Google Scholar]
- Venkatesan, A.M.; Agarwal, A.; Abe, T.; Ushirogochi, H.; Yamamura, I.; Kumagai, T.; Petersen, P.J.; Weiss, W.J.; Lenoy, E.; Yang, Y.; et al. Novel Imidazole Substituted 6-Methylidene-Penems as Broad-Spectrum β-Lactamase Inhibitors. Bioorganic Med. Chem. 2004, 12, 5807–5817. [Google Scholar] [CrossRef]
- Osborne, N.F.; Broom, N.J.P.; Coulton, S.; Harbridge, J.B.; Harris, M.A.; Stirling-François, I.; Walker, G. A Novel and Stereocontrolled Synthesis of (5R)-(Z)-6-(1-Methyl-1,2,3-Triazol-4-Ylmethylene)Penem-3-Carboxylic Acid, a Potent Broad Spectrum β-Lactamase Inhibitor. J. Chem. Soc. Chem. Commun. 1989, 6, 371–373. [Google Scholar] [CrossRef]
- Buynak, J.D.; Rao, A.S.; Doppalapudi, V.R.; Adam, G.; Petersen, P.J.; Nidamarthy, S.D. The Synthesis and Evaluation of 6-Alkylidene-2′β-Substituted Penam Sulfones as β-Lactamase Inhibitors. Bioorganic Med. Chem. Lett. 1999, 9, 1997–2002. [Google Scholar] [CrossRef]
- Edoo, Z.; Iannazzo, L.; Compain, F.; Li de la Sierra Gallay, I.; van Tilbeurgh, H.; Fonvielle, M.; Bouchet, F.; Le Run, E.; Mainardi, J.-L.; Arthur, M.; et al. Synthesis of Avibactam Derivatives and Activity on β-Lactamases and Peptidoglycan Biosynthesis Enzymes of Mycobacteria. Chem. A Eur. J. 2018, 24, 8081–8086. [Google Scholar] [CrossRef] [PubMed]
- Peilleron, L.; Cariou, K. Synthetic Approaches towards Avibactam and Other Diazabicyclooctane β-Lactamase Inhibitors. Org. Biomol. Chem. 2020, 18, 830–844. [Google Scholar] [CrossRef] [PubMed]
- Miller, S.P.; Limanto, J.; Zhong, Y.-L.; Yasuda, N.; Liu, Z. Preparation of Tert-Butyl-4-((1R,2S,5R)-6-(benzyloxy)-7-oxo-1,6-diazabicyclo[3.2.1]octane-2-Carboxamido Piperidine-1-Carboxylate. Application No. AU 2014278556 B2. WO20142007, 19 July 2018. [Google Scholar]
- Maiti, S.N.; Nguyen, D.; Khan, J.; Ling, R. Preparation of 1,6-diazabicyclo[3.2.1]octane-2-carboxamide Compounds and Their Use as Antibacterial ageNts and Beta-Lactamase Inhibitors. PCT International Applications No. WO 2014091268 A1, 19 June 2014. [Google Scholar]
- Liu, B.; Trout, R.E.L.; Chu, G.-H.; McGarry, D.; Jackson, R.W.; Hamrick, J.C.; Daigle, D.M.; Cusick, S.M.; Pozzi, C.; De Luca, F.; et al. Discovery of Taniborbactam (VNRX-5133): A Broad-Spectrum Serine- and Metallo-β-Lactamase Inhibitor for Carbapenem-Resistant Bacterial Infections. Antimicrob. Agents Chemother. 2020, 63, 2789–2801. [Google Scholar] [CrossRef] [PubMed]
- Hecker, S.J.; Reddy, K.R.; Lomovskaya, O.; Griffith, D.C.; Rubio-Aparicio, D.; Nelson, K.; Tsivkovski, R.; Sun, D.; Sabet, M.; Tarazi, Z.; et al. Discovery of Cyclic Boronic Acid QPX7728, an Ultrabroad-Spectrum Inhibitor of Serine and Metallo-β-Lactamases. Antimicrob. Agents Chemother. 2020, 63, 7491–7507. [Google Scholar] [CrossRef]
- Davies, D.T.; Leiris, S.; Sprynski, N.; Castandet, J.; Lozano, C.; Bousquet, J.; Zalacain, M.; Vasa, S.; Dasari, P.K.; Pattipati, R.; et al. ANT2681: SAR Studies Leading to the Identification of a Metallo-β-Lactamase Inhibitor with Potential for Clinical Use in Combination with Meropenem for the Treatment of Infections Caused by NDM-Producing Enterobacteriaceae. ACS Infect. Dis. 2020, 6, 2419–2430. [Google Scholar] [CrossRef] [PubMed]











| (BLAs) * | Penicillins | Narrow spectrum | β-lactamase sensitive (1st generation) | benzylpenicillin (G) # benzathine benzylpenicillin # procaine benzylpenicillin # phenoxymethylpenicillin (V) # propicillin ‡, pheneticillin ‡ azidocillin ‡, clometocillin ‡ penamecillin ‡ |
| β-lactamase resistant (2nd generation) | cloxacillin #, dicloxacillin flucloxacillin; oxacillin; nafcillin methicillin ‡ | |||
| Extended spectrum | aminopenicillins (3rd generation) | amoxicillin # ampicillin #; pivampicillin hetacillin ‡; bacampicillin ‡ metampicillin ‡; talampicillin ‡ epicillin ‡ | ||
| carboxypenicillins (4th generation) | ticarcillin carbenicillin ‡;carindacillin ‡ temocillin ‡ | |||
| ureidopenicillins (4th generation) | piperacillin; azlocillin ‡; mezlocillin ‡ | |||
| Others | mecillinam; pivmecillinam, sulbenicillin ‡ | |||
| carbapenems | ertapenem 1; doripenem 2; imipenem 2; meropenem 2; biapenem ‡; panipenem faropenem 3; ritipenem 3,§ | |||
| cephems cephalosporins cephamycins carbacephems | 1st generation | cefazolin #; cefalexin #; cefadroxil; cefapirin; cefazedone ‡ cefazaflur; cefradine ‡; cefroxadine ‡; ceftezole ‡; cefaloglycin ‡ cefacetrile ‡; cefalonium ‡; cefaloridine ‡; cefalotin; cefatrizine ‡ | ||
| 2nd generation | cefaclor, cefprozil, cefuroxime, cefuroxime axetil, cefamandole ‡, cefonicid ‡;, ceforanide ‡;, cefuzonam ‡;, cefoxitin, cefotetan cefminox ‡; cefbuperazone ‡; cefmetazole ‡; loracarbef ‡ | |||
| 3rd generation | cefixime #; ceftriaxone #; cefotaxime #; ceftazidime #,2; cefoperazone ‡,2 cefdinir; cefcapene; cefdaloxime; ceftizoxime; cefmenoxime cefpiramide; cefpodoxime; ceftibuten; cefditoren; cefotiam ‡ cefetamet ‡; cefodizime ‡; cefpimizole ‡; cefsulodin ‡; cefteram ‡ ceftiolene ‡; flomoxef ‡; latamoxef ‡ | |||
| 4th generation | cefepime; cefozopran ‡; cefpirome; cefquinome ‡ | |||
| 5th generation | ceftaroline fosamil; ceftolozane; ceftobiprole | |||
| siderophore | cefiderocol # | |||
| veterinary | ceftiofur; cefquinome; cefovecin | |||
| monobactams | aztreonam, tigemonam ‡; carumonam ‡; nocardicin A ‡ | |||
| BLEs | Ambler Class | Subclass | Producer Bacteria | Susceptible BLAs | Not Susceptible BLAs |
|---|---|---|---|---|---|
| SBLEs ESSBLEs | A | KPCs * [34] | K. pneumoniae Enterobacter spp., Salmonella spp. P. aeruginosa A. baumannii | carbapenems | N.R. |
| GESs [35,36,37] | P. aeruginosa | N.R | N.R. | ||
| CTX-Ms ** [35,36,37,38] | S. entericaserovar typhimurium E. coli Enterobacteriaceae. | cefotaxime ceftazidime ceftriaxone cefepime | N.R | ||
| SHVs [35,36,37] | Enterobacteriaceae P. aeruginosa | aztreonam 3rd cefotaxime 3rd ceftazidime | cefozitin imipenem | ||
| TEMs [35,36,37] | Enterobacteriaceae P. aeruginosa H. influenzae N. gonorrhoeae | penicillin 1st cephalosporins 2nd cephalosporins | 3rd cefotaxime 3rd ceftazidime 3rd ceftriaxone 4th cefepime. | ||
| D (CHDLs §) | OXAs * [39,40] | Enterobacteriaceae P. aeruginosa Acinetobacter supp. | ampicillin cephalothin oxacillin cloxacillin carbapenems cefotaxime cefepime | N.R. | |
| C [35,36,37,41] | ACTs a | Enterobacteriaceae | cephalothin cefazolin cefoxitin penicillin derivatives cefotaxime ceftazidime ceftriaxone | N.R. | |
| DHAs a | |||||
| CMYs a | |||||
| ADCs a | |||||
| MBLEs 1 | B [42,43,44,45,46,47] | B1 *,2 | P. aeruginosa A. baumannii Enterobacteriaceae, | penicillin cephalosporins carbapenems | |
| B2 *,3 | carbapenems | penicillin cephalosporins | |||
| B3 *,2 | penicillin cephalosporins carbapenems |
| BLEsIs | Chemical Structure | Not Carbapanemases SBLEs | Carbapanemases SBLEs | MBLEs | ||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|
| Class A | Class C | Class D | Class A | Class D | Class C | Class B | ||||||
| GES CTX-M SHV TEM | AmpC | N.R. | KPC | OXA23 | OXA 24/40 | OXA-48 | N.R. | NDM | VIM | IMP | ||
| Clavulanic Acid (CA) *,1 [55,56] | 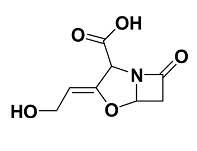 |  |  |  |  |  |  |  |  |  |  |  |
| Sulbactam *,1 [57,58,59] |  |  |  |  |  |  |  |  |  |  |  |  |
| Tazobactam *,1 [60,61,62] |  |  |  |  |  |  |  |  |  |  |  |  |
| Tebipenem pivoxil *,1,2 [63] | 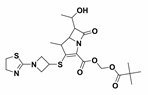 |  |  |  |  |  |  |  | N.R. |  |  |  |
| Enmetazobactam *,$ [64,65,66,67] | 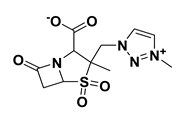 |  |  |  |  |  |  |  |  |  |  |  |
| 6-methylidene penems *,1,$ [68] |  |  |  |  |  |  |  |  |  |  |  |  |
| LN-1-255 *,$ [30,69,70,71] |  |  |  |  |  |  |  |  | N.R. |  |  |  |
| Avibactam §,** [1,16,62,72,73,74,75,76,77,78] | 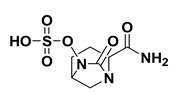 |  |  |  |  |  |  |  | N.R. |  |  |  |
| Relebactam §,** [15,62,79,80,81] | 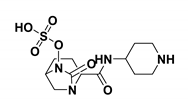 |  |  |  |  |  |  |  | N.R. |  |  |  |
| Zidebactam §,§§,3,$ [22,62,82,83,84,85] | 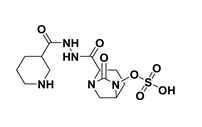 |  |  |  |  |  |  |  | N.R. |  |  |  |
| Durlobactam §,3,4,$ [62,86,87,88,89] | 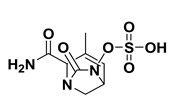 |  |  |  |  |  |  |  | N.R. |  |  |  |
| Nacubactam §,3,$ [62,90,91,92,93,94] | 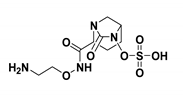 |  |  |  |  |  |  | N.R. | N.R. |  |  |  |
| ETX-1317 §,3,$ [62,95,96,97,98,99] | 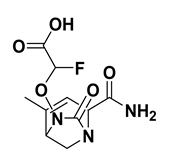 |  |  |  |  | N.R. | N.R. |  | N.R. |  |  |  |
| WCK-5153 §,3,$ [100,101] |  |  |  |  |  |  |  |  |  |  |  |  |
| WCK-4234 §,3,$ [101,102,103] | 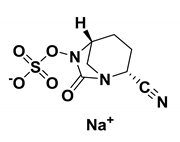 |  |  |  |  |  |  |  | N.R. |  |  |  |
| ANT-3310 §,3,$ [104,105] | 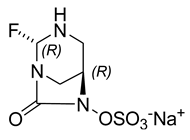 |  |  |  |  |  |  |  | N.R. |  |  |  |
| GT-055 §,3,$ [62,106,107,108] | 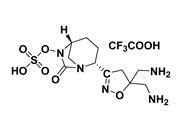 |  |  |  |  | N.R | N.R | N.R | N.R. |  |  |  |
| Vaborbactam #,** [62,109,110,111,112,113,114] | 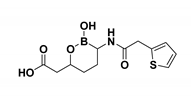 |  |  |  |  |  |  |  | N.R. |  |  |  |
| Taniborbactam #,3,$,## [115,116,117,118] | 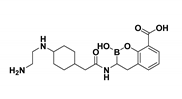 |  |  |  |  | N.R. | N.R. |  | N.R. |  |  |  |
| Ledaborbactam etzadroxil (VNRX-7145 #,3,$,##) (Prodrug of VNRX-5236, blue structure) [62,119,120,121] | 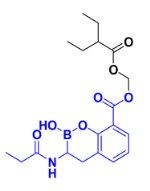 |  |  |  |  |  |  |  | N.R. |  |  |  |
| Xeruborbactam(QPX-7728) #,3,$,## [62,122,123,124,125,126] | 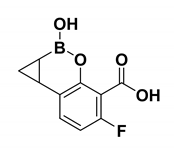 |  |  |  |  |  | N.R. |  | N.R. |  |  |  |
| ANT-2681 ***,3,$,## [62,127,128,129,130] |  |  |  |  |  |  |  |  |  |  |  |  |
| Brand Name | Composition § | Dosage Form | Type of Infection | Posology |
|---|---|---|---|---|
| Augmentin® [131] | Amoxacillin/K clavulanate 7/1 875 mg/125 mg | Film Coated Tablets (adults) | Diabetic foot cIAIs, cUTIs, LRTIs Pulmonary infections Brain abscesses Prophylaxis after surgery Acute otitis Sinusitis Skin infections Gynecologic infections Septicemia Bone and joint infections Endometritis Peritonitis | 1 tablet 2/3 a day |
| Amoxacillin/K clavulanate 7/1 875 mg/125 mg | Powder for oral suspension in sachets (adults/children ≥ 40 kg) | 1 sachet 2/3 times a day | ||
| Amoxacillin/K clavulanate 7/1 400 mg/57 mg | Powder for oral suspension in sachets (children) | 25/3.6 mg to 45/6.4 mg/Kg day given in two doses. | ||
| Amoxacillin/K clavulanate 7/1 400 mg/57 mg/5mL | Powder for oral suspension in sachets (children) | 25/3.6 mg to 45/6.4 mg/Kg day given in two doses with measuring spoon or syringe | ||
| Amoxacillin/K clavulanate 5/1 1000 mg/200 mg | Powder for solution for injection/infusion (adults/children ≥ 40 kg) | 1000 mg/200 mg every 8 h | ||
| Powder for solution for injection/infusion (children < 40 kg) | Children ≥ 3 months 25 mg/5 mg/kg every 8 h | |||
| Children < 3 months or < 4 kg 25 mg/5 mg/kg every 12 h | ||||
| Amoxacillin/K clavulanate 10/1 2000 mg/200 mg | Powder for solution for infusion (adults/children ≥ 40 kg) | 1000 mg/100 mg every 8/12 h | ||
| Powder for solution for injection/infusion (children < 40 kg) | Children ≥ 3 months50 mg/5 mg/kg every 8 h | |||
| Children < 3 months or < 4 kg 50 mg/5 mg/kg every 12 h | ||||
| Timentin® [132] | (Na)2 Ticarcillin/K clavulanate 30/1 30 mg/mL/1 mg/mL | Injection Powder for solution (adults ≥ 60 kg) | Systemic infections, cUTIs | 3.1 g Timentin every 4/6 h |
| gynecologic infections * | Moderate infections 200 mg/kg/day every 6 h | |||
| Severe infections 300 mg/kg/day in divided doses every 4 h. | ||||
| Injection Powder for solution (children ≥ 3 month) | Aspiration Pneumonia Bacteremia cUTIs, cIAIs, VAP, HAP Appendicitis Bone infection | Mild/moderate infections 200 mg/kg/day divided doses every 6 h | ||
| Severe infections 300 mg/kg/day divided doses every 4 h | ||||
| Clavucar [133] | (Na)2 Ticarcillin/K clavulanate 5/1 1000 mg/200 mg | Intramuscolar Injection (IMI) (adults) | Aspiration Pneumonia Bacteremia cUTIs, cIAIs, VAP, HAP Appendicitis Bone infection Gynecologic infections | 1 bottle (1.2 g) 2–3 times a day. |
| (Na)2 Ticarcillin/K clavulanate 15/1 3000 mg/200 mg | Intravenous Infusion (IVI) (adults) | 1 bottle (3.2 g) every 8 h | ||
| Zosyn® [134] | Piperacillin/Na tazobactam 8/1 Zosyn 2.25 g/50 mL, 3.375 g/50 mL, 4.5 g/100 mL | Frozen iso-osmotic sterile non-pyrogenic premixed solution for IVI | Cellulitis Diabetic foot LRTIs cIAIs, cUTIs, HAP, VAP Gynaecologic Skin infections Appendicitis Postpartum endometritis Stomach infections Severe uterine infections | Adults 3.375 g Zosyn every six hours totaling 13.5 g a day 12.0 g piperacillin 1.5 g tazobactam |
| Piperacillin/Na tazobactam 8/1 Zosyn 2.25, 3.375, 4.5 g single dose vials | Powder/lyophilized for solution for IVI | Pediatric patients ≥ 9 months < 40 kg 112.5 mg/Kg Zosyn every 8 h | ||
| Pediatric patients 2–9 months 90 mg/Kg Zosyn every 8 h | ||||
| Zerbaxa [135] | Ceftalozane sulfate 1000 g Na tazobactam 500 g 2/1 | Powder for concentrate for solution for IVI | HAP, VAP, cIAIs Acute pyelonephritis | 1 bottle (1.5 g) every 8 h Not for individuasl < 18 years |
| Unasyn® [136] | Na Ampicillin/Na Sulbactam (2/1)/1.6 mL 500 mg/250 mg | Powder and solvent for solution for injection | VAP, HAP, cUTIs, cIAIs Lower respiratory tract Gynecological Obstetric Acute epiglottitis Periorbital cellulitis Diabetic foot Skin and soft tissue Gonorrhoea Otitis media | Adults 3–12 g Unasyn/a day Every 6, 8, 12 h |
| Na Ampicillin/Na Sulbactam (2/1)/3.2 mL 1000 mg/500 mg | Powder and solvent for solution for IMI | |||
| Na Ampicillin/Na Sulbactam (2/1)/3.2 mL 1000 mg/500 mg | Powder and solvent for solution for IVI | Children 150 mg/kg/die every 6–8 h | ||
| Na Ampicillin/Na Sulbactam (2/1) 1000 mg/500 mg | Powder for solution for IMI | Neonates 75 mg/kg/die every 12 h | ||
| Sultamicillin®,1 [137] | Bounded ampicillin and sulbactam | Tablets (375, 750 mg) | Adults 375–750 mg/day | |
| Children < 30 Kg 25–50 mg/kg/day in 2 doses | ||||
| Sulperazon® [138] | Na cefoperazone/Na Sulbactam 1/1 1000 mg/1000 mg | Injection Powder for injection | Upper/LRTIs cUTIs, cIAIs Sepsis Meningitis Skin infections Bone and joint infections Endometritis Gonorrhoea | Adults 2–4 mg Sulperazon/day divided into 2 doses |
| Children 40–80 mg/kg/day in 2–4 doses | ||||
| New-borns Max 80 mg/kg/day in 2 doses | ||||
| Recarbrio™ [139] | Imipenem/Na cilastatin/relebactam 2/2/1 500 mg/500 mg/250 mg | Power for solution IVI | cUTIs, cIAIs, HAP, VAP | 1.25 g Recarbrio every 6 h Not for individuasl < 18 years |
| Avycaz® [140] | Ceftazidime/avibactam 4/1 2000 mg/500 mg | Vials for IVI (2.5 g) | cIAIs, HAP, VAP cUTIs (pyelonephritis) | >18 years old 2.5 g Avycaz every 8 h |
| Zavicefta® [141] | Power for solution for IVI (2.5 g) | 3–6 months 50 mg/Kg Avycaz every 8 h | ||
| 3 months–2 years old 62.5 mg/Kg Avycaz every 8 h | ||||
| 2–18 years old 62.5 mg/Kg Avycaz every 8 h | ||||
| Vabomere® [142] | Meropenem/vaborbactam 1/1 1000 mg/1000 mg | Power for solution for IVI (2.0 g) | cUTIs, cIAIs, HAP, VAP Acute pyelonephritis | >18 years old 4g Vabomere every 8 h |
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2022 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Alfei, S.; Zuccari, G. Recommendations to Synthetize Old and New β-Lactamases Inhibitors: A Review to Encourage Further Production. Pharmaceuticals 2022, 15, 384. https://doi.org/10.3390/ph15030384
Alfei S, Zuccari G. Recommendations to Synthetize Old and New β-Lactamases Inhibitors: A Review to Encourage Further Production. Pharmaceuticals. 2022; 15(3):384. https://doi.org/10.3390/ph15030384
Chicago/Turabian StyleAlfei, Silvana, and Guendalina Zuccari. 2022. "Recommendations to Synthetize Old and New β-Lactamases Inhibitors: A Review to Encourage Further Production" Pharmaceuticals 15, no. 3: 384. https://doi.org/10.3390/ph15030384
APA StyleAlfei, S., & Zuccari, G. (2022). Recommendations to Synthetize Old and New β-Lactamases Inhibitors: A Review to Encourage Further Production. Pharmaceuticals, 15(3), 384. https://doi.org/10.3390/ph15030384