Trackins (Trk-Targeting Drugs): A Novel Therapy for Different Diseases
Abstract
1. Introduction
Thus, the task is not so much to see what no one has yet seen but to think what nobody has yet thought about that which everybody sees.Arthur Schopenhauer
2. Neurotrophins and Their Receptors
3. NGF, BDNF, and Their Trk Receptors: Druggable Targets for Disease Therapies
4. Conclusions and Perspectives
In science, the Apollonian tends to develop established lines to perfection, while the Dionysian rather relies on intuition and is more likely to open new, unexpected alleys for research. The future of mankind depends on the progress of science, and the progress of science depends on the support it can find. Support mostly takes the form of grants, and the present methods of distributing grants unduly favor the Apollonian.
Albert Szent-Gyorgyi (1972), Nobel Prize winner 1937 in Physiology or Medicine
5. Addendum
- A metabolic process, whereby animals take in matter, change its qualities, and distribute these to use to grow, live, and reproduce.
- Temperature regulation, whereby animals maintain a steady state, which progressively fails in old age.
- An information-processing model, whereby animals receive sensory information and use it to drive movements of the limbs.
- The process of inheritance.
- The processes of embryonic development and spontaneous generation
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Acknowledgments
Conflicts of Interest
References
- Levi-Montalcini, R. The nerve growth factor 35 years later. Science 1987, 237, 1154–1162. [Google Scholar] [CrossRef] [PubMed]
- Cohen, S.; Levi-Montalcini, R.; Hamburger, V. A Nerve Growth-Stimulating Factor Isolated from Sarcomas 37 and 180. Proc. Natl. Acad. Sci. USA 1954, 40, 1014–1018. [Google Scholar] [CrossRef] [PubMed]
- Yanev, S.; Aloe, L.; Fiore, M.; Chaldakov, G.N. Neurotrophic and metabotrophic potential of nerve growth factor and brain-derived neurotrophic factor: Linking cardiometabolic and neuropsychiatric diseases. World J. Pharmacol. 2013, 2, 92. [Google Scholar] [CrossRef]
- Yanev, S.; Fiore, M.; Hinev, A.; Ghenev, P.I.; Hristova, M.G.; Panayotov, P.; Tonchev, A.; Evtimov, N.; Aloe, L.; Chaldakov, G.N. From antitubulins to trackins. Biomed. Rev. 2016, 27, 59–67. [Google Scholar] [CrossRef]
- Chaldakov, G.; Fiore, M.; Tonchev, A.; Aloe, L. Adipopharmacology, a Novel Drug Discovery Approach: A Metabotrophic Perspective. Lett. Drug Des. Discov. 2008, 3, 503–505. [Google Scholar] [CrossRef]
- Frohlich, J.; Chaldakov, G.N.; Vinciguerra, M. Cardio- and Neurometabolic Adipobiology: Consequences and Implications for Therapy. Int. J. Mol. Sci. 2021, 22, 4137. [Google Scholar] [CrossRef] [PubMed]
- Chaldakov, G.N.; Fiore, M.; Stankulov, I.S.; Manni, L.; Hristova, M.G.; Antonelli, A.; Ghenev, P.I.; Aloe, L. Neurotrophin presence in human coronary atherosclerosis and metabolic syndrome: A role for NGF and BDNF in cardiovascular disease? Prog. Brain Res. 2004, 146, 279–289. [Google Scholar] [CrossRef] [PubMed]
- Aloe, L.; Tirassa, P.; Lambiase, A. The topical application of nerve growth factor as a pharmacological tool for human corneal and skin ulcers. Pharmacol. Res. 2008, 57, 253–258. [Google Scholar] [CrossRef] [PubMed]
- Chaldakov, G.N.; Stankulov, I.S.; Fiore, M.; Ghenev, P.I.; Aloe, L. Nerve growth factor levels and mast cell distribution in human coronary atherosclerosis. Atherosclerosis 2001, 159, 57–66. [Google Scholar] [CrossRef]
- Manni, L.; Nikolova, V.; Vyagova, D.; Chaldakov, G.N.; Aloe, L. Reduced plasma levels of NGF and BDNF in patients with acute coronary syndromes. Int. J. Cardiol. 2005, 102, 169–171. [Google Scholar] [CrossRef]
- Gentry, J.J.; Barker, P.A.; Carter, B.D. The p75 neurotrophin receptor: Multiple interactors and numerous functions. Prog. Brain Res. 2004, 146, 25–39. [Google Scholar] [CrossRef]
- Jeanneteau, F.; Chao, M.V. Promoting neurotrophic effects by GPCR ligands. Novartis Found Symp. 2006, 276, 181–192, 233–237, 275–281. [Google Scholar]
- Sahay, A.; Kale, A.; Joshi, S. Role of neurotrophins in pregnancy and offspring brain development. Neuropeptides 2020, 83, 102075. [Google Scholar] [CrossRef]
- Galvez-Contreras, A.Y.; Campos-Ordonez, T.; Lopez-Virgen, V.; Gomez-Plascencia, J.; Ramos-Zuniga, R.; Gonzalez-Perez, O. Growth factors as clinical biomarkers of prognosis and diagnosis in psychiatric disorders. Cytokine Growth Factor Rev. 2016, 32, 85–96. [Google Scholar] [CrossRef]
- Lamballe, F.; Klein, R.; Barbacid, M. The trk family of oncogenes and neurotrophin receptors. Princess Takamatsu Symp. 1991, 22, 153–170. [Google Scholar]
- French, S.J.; Humby, T.; Horner, C.H.; Sofroniew, M.V.; Rattray, M. Hippocampal neurotrophin and trk receptor mRNA levels are altered by local administration of nicotine, carbachol and pilocarpine. Mol. Brain Res. 1999, 67, 124–136. [Google Scholar] [CrossRef]
- Sinkevicius, K.W.; Kriegel, C.; Bellaria, K.J.; Lee, J.; Lau, A.N.; Leeman, K.T.; Zhou, P.; Beede, A.M.; Fillmore, C.M.; Caswell, D.; et al. Neurotrophin receptor TrkB promotes lung adenocarcinoma metastasis. Proc. Natl. Acad. Sci. USA 2014, 111, 10299–10304. [Google Scholar] [CrossRef]
- Aloe, L.; Rocco, M.L.; Balzamino, B.O.; Micera, A. Nerve growth factor: Role in growth, differentiation and controlling cancer cell development. J. Exp. Clin. Cancer Res. 2016, 35, 1–7. [Google Scholar] [CrossRef]
- Esteban-Villarrubia, J.; Soto-Castillo, J.J.; Pozas, J.; San Román-Gil, M.; Orejana-Martín, I.; Torres-Jiménez, J.; Carrato, A.; Alonso-Gordoa, T.; Molina-Cerrillo, J. Tyrosine kinase receptors in oncology. Int. J. Mol. Sci. 2020, 21, 1–48. [Google Scholar] [CrossRef]
- Zhang, Q.; Descamps, O.; Hart, M.J.; Poksay, K.S.; Spilman, P.; Kane, D.J.; Gorostiza, O.; John, V.; Bredesen, D.E. Paradoxical effect of TrkA inhibition in alzheimer’s disease models. J. Alzheimer’s Dis. 2014, 40, 605–617. [Google Scholar] [CrossRef]
- Ciafrè, S.; Ferraguti, G.; Tirassa, P.; Iannitelli, A.; Ralli, M.; Greco, A.; Chaldakov, G.N.; Rosso, P.; Fico, E.; Messina, M.P.; et al. Nerve growth factor in the psychiatric brain. Riv. Psichiatr. 2020, 55, 4–15. [Google Scholar] [CrossRef]
- Chaldakov, G.N. The metabotrophic NGF and BDNF: An emerging concept. Arch. Ital. Biol. 2011, 149, 257–263. [Google Scholar]
- Hirose, M.; Kuroda, Y.; Murata, E. NGF/TrkA Signaling as a Therapeutic Target for Pain. Pain Pract. 2016, 16, 175–182. [Google Scholar] [CrossRef]
- Ghenev, P.; Kitanova, M.; Popov, H.; Evtimov, N.; Stoev, S.; Tonchev, A.; Chaldakov, G. Neuroadipobiology of arrhythmogenic right ventricular dysplasia. An immunohistochemical study of neurotrophins. Adipobiology 2017, 8, 55. [Google Scholar] [CrossRef]
- Voronin, M.V.; Vakhitova, Y.V.; Seredenin, S.B. Chaperone Sigma1R and antidepressant effect. Int. J. Mol. Sci. 2020, 21, 1–33. [Google Scholar] [CrossRef]
- Alizadeh Pahlavani, H. Possible role of exercise therapy on depression: Effector neurotransmitters as key players. Behav. Brain Res. 2024, 459, 114791. [Google Scholar] [CrossRef]
- Hochstrasser, T.; Ehrlich, D.; Sperner-Unterweger, B.; Humpel, C. Antidepressants and anti-inflammatory drugs differentially reduce the release of NGF and BDNF from rat platelets. Pharmacopsychiatry 2013, 46, 29–34. [Google Scholar] [CrossRef]
- Angelucci, F.; Mathé, A.A.; Aloe, L. Neurotrophic factors and CNS disorders: Findings in rodent models of depression and schizophrenia. Prog. Brain Res. 2004, 146, 151–165. [Google Scholar] [CrossRef]
- Kozisek, M.E.; Middlemas, D.; Bylund, D.B. Brain-derived neurotrophic factor and its receptor tropomyosin-related kinase B in the mechanism of action of antidepressant therapies. Pharmacol. Ther. 2008, 117, 30–51. [Google Scholar] [CrossRef]
- Jiang, C.; Salton, S.R. The role of neurotrophins in major depressive disorder. Transl. Neurosci. 2013, 4, 46–58. [Google Scholar] [CrossRef]
- Raap, U.; Ständer, S.; Metz, M. Pathophysiology of itch and new treatments. Curr. Opin Allergy Clin. Immunol. 2011, 11, 420–427. [Google Scholar] [CrossRef]
- Raap, U.; Papakonstantinou, E.; Metz, M.; Lippert, U.; Schmelz, M. Update on the cutaneous neurobiology of pruritus. Hautarzt 2016, 67, 595–600. [Google Scholar] [CrossRef]
- Zisiadis, G.A.; Alevyzaki, A.; Nicola, E.; Rodrigues, C.F.D.; Blomgren, K.; Osman, A.M. Memantine increases the dendritic complexity of hippocampal young neurons in the juvenile brain after cranial irradiation. Front. Oncol. 2023, 13, 1202200. [Google Scholar] [CrossRef]
- Minoretti, P.; Santiago Sáez, A.S.; García Martín, Á.F.; Riera, M.; Gómez Serrano, M.; Lahmar, A.; Emanuele, E. Impact of Job Types on Plasma Neurotrophins Levels: A Preliminary Study in Airline Pilots, Construction Workers, and Fitness Instructors. Neuro Endocrinol. Lett. 2023, 44, 439–443. [Google Scholar]
- Khodabakhsh, P.; Asgari Taei, A.; Shafaroodi, H.; Pournajaf, S.; Dargahi, L. Effect of Metformin on Epidermal Neural Crest Stem Cells and Their Potential Application in Ameliorating Paclitaxel-induced Neurotoxicity Phenotype. Stem Cell Rev. Rep. 2024, 20, 394–412. [Google Scholar] [CrossRef]
- Chen, W.; Ren, Q.; Zhou, J.; Liu, W. Mesenchymal Stem Cell-Induced Neuroprotection in Pediatric Neurological Diseases: Recent Update of Underlying Mechanisms and Clinical Utility. Appl. Biochem. Biotechnol. 2024. [Google Scholar] [CrossRef]
- Moghadasi, M.; Akbari, F.; Najafi, P. Interaction of aerobic exercise and crocin improves memory, learning and hypocampic tau and neurotrophins gene expression in rats treated with trimethytin as a model of Alzheimer’s disease. Mol. Biol. Rep. 2024, 51, 111. [Google Scholar] [CrossRef]
- Shafiee, A.; Rafiei, M.A.; Jafarabady, K.; Eskandari, A.; Abhari, F.S.; Sattari MAAmini, M.J.; Bakhtiyari, M. Effect of cannabis use on blood levels of brain-derived neurotrophic factor (BDNF) and nerve growth factor (NGF): A systematic review and meta-analysis. Brain Behav. 2024, 14, e3340. [Google Scholar] [CrossRef]
- Tu, Y.; Han, D.; Liu, Y.; Hong, D.; Chen, R. Nicorandil attenuates cognitive impairment after traumatic brain injury via inhibiting oxidative stress and inflammation: Involvement of BDNF and NGF. Brain Behav. 2024, 14, e3356. [Google Scholar] [CrossRef]
- Liu, J.; Guan, J.; Xiong, J.; Wang, F. Effects of Transcranial Magnetic Stimulation Combined with Sertraline on Cognitive Level, Inflammatory Response and Neurological Function in Depressive Disorder Patients with Non-suicidal Self-injury Behavior. Actas Esp. Psiquiatr. 2024, 52, 28–36. [Google Scholar]
- Crews, F.T.; Macht, V.; Vetreno, R.P. Epigenetic regulation of microglia and neurons by proinflammatory signaling following adolescent intermittent ethanol (AIE) exposure and in human AUD. Adv. Drug Alcohol. Res. 2024, 4, 12094. [Google Scholar] [CrossRef]
- Sun, L.; Xiao, K.; Shen, X.-Y.; Wang, S. Impact of transcranial electrical stimulation on serum neurotrophic factors and language function in patients with speech disorders. World J. Clin. Cases 2024, 12, 1742–1749. [Google Scholar] [CrossRef]
- Yu, Z.; Joy, S.; Mi, T.; Yazdanpanah, G.; Burgess, K.; de Paiva, C.S. New, potent, small molecule agonists of tyrosine kinase receptors attenuate dry eye disease. Front. Med. 2022, 9, 937142. [Google Scholar] [CrossRef]
- Ricci, A.; Salvucci, C.; Castelli, S.; Carraturo, A.; de Vitis, C.; D’Ascanio, M. Adenocarcinomas of the Lung and Neurotrophin System: A Review. Biomedicines 2022, 10, 2531. [Google Scholar] [CrossRef]
- Sullivan, I.; Kc, R.; Singh, G.; Das, V.; Ma, K.; Li, X.; Mwale, F.; Votta-Velis, G.; Bruce, B.; Natarajan Anbazhagan, A.; et al. Sensory Neuron-Specific Deletion of Tropomyosin Receptor Kinase A (TrkA) in Mice Abolishes Osteoarthritis (OA) Pain via NGF/TrkA Intervention of Peripheral Sensitization. Int. J. Mol. Sci. 2022, 23, 12076. [Google Scholar] [CrossRef]
- Qin, S.; Zhang, Z.; Zhao, Y.; Liu, J.; Qiu, J.; Gong, Y.; Fan, W.; Guo, Y.; Guo, Y.; Xu, Z.; et al. The impact of acupuncture on neuroplasticity after ischemic stroke: A literature review and perspectives. Front. Cell Neurosci. 2022, 16, 817732. [Google Scholar] [CrossRef]
- Arutjunyan, A.V.; Kerkeshko, G.O.; Milyutina, Y.P.; Shcherbitskaia, A.D.; Zalozniaia, I.V.; Mikhel, A.V.; Inozemtseva, D.B.; Vasilev, D.S.; Kovalenko, A.A.; Kogan, I.Y. Imbalance of Angiogenic and Growth Factors in Placenta in Maternal Hyperhomocysteinemia. Biochemistry 2023, 88, 262–279. [Google Scholar] [CrossRef]
- Lutfi Ismaeel, G.; Makki AlHassani, O.J.; Alazragi, R.S.; Hussein Ahmed, A.; Mohamed, A.H.; Yasir Jasim, N.; Hassan Shari, F.; Almashhadani, H.A. Genetically engineered neural stem cells (NSCs) therapy for neurological diseases; state-of-the-art. Biotechnol. Prog. 2023, 39, e3363. [Google Scholar] [CrossRef]
- Redigolo, L.; Sanfilippo, V.; La Mendola, D.; Forte, G.; Satriano, C. Bioinspired Nanoplatforms Based on Graphene Oxide and Neurotrophin-Mimicking Peptides. Membranes 2023, 13, 50489. [Google Scholar] [CrossRef]
- Jashire Nezhad, N.; Safari, A.; Namavar, M.R.; Nami, M.; Karimi-Haghighi, S.; Pandamooz, S.; Dianatpour, M.; Azarpira, N.; Khodabandeh, Z.; Zare, S.; et al. Short-term beneficial effects of human dental pulp stem cells and their secretome in a rat model of mild ischemic stroke. J. Stroke Cerebrovasc. Dis. 2023, 32, 107202. [Google Scholar] [CrossRef]
- Pahlavani, H.A. Exercise therapy to prevent and treat Alzheimer’s disease. Front. Aging Neurosci. 2023, 15, 1243869. [Google Scholar] [CrossRef]
- Wan, T.; Zhang, F.S.; Qin, M.Y.; Jiang, H.R.; Zhang, M.; Qu, Y.; Wang, Y.L.; Zhang, P.X. Growth factors: Bioactive macromolecular drugs for peripheral nerve injury treatment—Molecular mechanisms and delivery platforms. Biomed. Pharmacother. 2024, 170, 116024. [Google Scholar] [CrossRef] [PubMed]
- Giri, S.S.; Tripathi, A.S.; Erkekoğlu, P.; Zaki, M.E.A. Molecular pathway of pancreatic cancer-associated neuropathic pain. J. Biochem. Mol. Toxicol. 2024, 38, e23638. [Google Scholar] [CrossRef] [PubMed]
- Stabile, A.M.; Pistilli, A.; Moretti, E.; Bartolini, D.; Ruggirello, M.; Rende, M.; Castellini, C.; Mattioli, S.; Ponchia, R.; Tripodi, S.A.; et al. A Possible Role for Nerve Growth Factor and Its Receptors in Human Sperm Pathology. Biomedicines 2023, 11, 3345. [Google Scholar] [CrossRef]
- Rosso, P.; Fico, E.; Mesentier-Louro, L.A.; Triaca, V.; Lambiase, A.; Rama, P.; Tirassa, P. NGF eye administration recovers the trkb and glutamate/GABA marker deficit in the adult visual cortex following optic nerve crush. Int. J. Mol. Sci. 2021, 22, 10014. [Google Scholar] [CrossRef]
- D’Souza, S.; Vaidya, T.; Nair, A.P.; Shetty, R.; Kumar, N.R.; Bisht, A.; Panigrahi, T.; J, T.S.; Khamar, P.; Dickman, M.M.; et al. Altered Ocular Surface Health Status and Tear Film Immune Profile Due to Prolonged Daily Mask Wear in Health Care Workers. Biomedicines 2022, 10, 1160. [Google Scholar] [CrossRef]
- Shu, J.; He, X.; Li, H.; Liu, X.; Qiu, X.; Zhou, T.; Wang, P.; Huang, X. The beneficial effect of human amnion mesenchymal cells in inhibition of inflammation and induction of neuronal repair in EAE mice. J. Immunol. Res. 2018, 2018, 5083797. [Google Scholar] [CrossRef] [PubMed]
- Sun, S.; Diggins, N.H.; Gunderson, Z.J.; Fehrenbacher, J.C.; White, F.A.; Kacena, M.A. No pain, no gain? The effects of pain-promoting neuropeptides and neurotrophins on fracture healing. Bone 2020, 131, 115109. [Google Scholar] [CrossRef]
- Valente, S.; Curti, N.; Giampieri, E.; Randi, V.; Donadei, C.; Buzzi, M.; Versura, P. Impact of blood source and component manufacturing on neurotrophin content and in vitro cell wound healing. Blood Transfus. 2022, 20, 213–222. [Google Scholar] [CrossRef]
- Sipione, R.; Liaudet, N.; Rousset, F.; Landis, B.N.; Hsieh, J.W.; Senn, P. Axonal Regrowth of Olfactory Sensory Neurons In Vitro. Int. J. Mol. Sci. 2023, 24, 12863. [Google Scholar] [CrossRef]
- Zhang, Y.; Zhao, X.; Ge, D.; Huang, Y.; Yao, Q. The impact and mechanism of nerve injury on bone metabolism. Biochem. Biophys. Res. Commun. 2024, 704, 149699. [Google Scholar] [CrossRef] [PubMed]
- Lambiase, A.; Rama, P.; Bonini, S.; Caprioglio, G.; Aloe, L. Topical Treatment with Nerve Growth Factor for Corneal Neurotrophic Ulcers. N. Engl. J. Med. 1998, 338, 1174–1180. [Google Scholar] [CrossRef] [PubMed]
- Aloe, L. Nerve growth factor, human skin ulcers and vascularization. Our experience. Prog. Brain Res. 2004, 146, 515–522. [Google Scholar] [CrossRef]
- Raap, U.; Kapp, A. Neurotrophins in healthy and diseased skin. G. Ital. Dermatol. Venereol. Organo Uff. Soc. Ital. Dermatol. Sifilogr. 2010, 145, 205–211. [Google Scholar]
- Scuri, M.; Samsell, L.; Piedimonte, G. The role of neurotrophins in inflammation and allergy. Inflamm. Allergy Drug Targets 2010, 9, 173–180. [Google Scholar] [CrossRef]
- D’Amico, F.; Lugarà, C.; Luppino, G.; Giuffrida, C.; Giorgianni, Y.; Patanè, E.M.; Manti, S.; Gambadauro, A.; La Rocca, M.; Abbate, T. The Influence of Neurotrophins on the Brain-Lung Axis: Conception, Pregnancy, and Neonatal Period. Curr. Issues Mol. Biol. 2024, 46, 2528–2543. [Google Scholar] [CrossRef]
- Pham, T.L.; He, J.; Kakazu, A.H.; Jun, B.; Bazan, N.G.; Bazan, H.E.P. Defining a mechanistic link between pigment epithelium–derived factor, docosahexaenoic acid, and corneal nerve regeneration. J. Biol. Chem. 2017, 292, 18486–18499. [Google Scholar] [CrossRef] [PubMed]
- Ghosh, T.; Maity, N.; Sur, V.P.; Konar, A.; Hazra, S. Mitigating fibrosis-An impediment to corneal re-innervation following lamellar flap surgery. Exp. Eye Res. 2020, 194, 108009. [Google Scholar] [CrossRef]
- Micera, A.; Jirsova, K.; Esposito, G.; Balzamino, B.O.; Zazzo ADi Bonini, S. Mast cells populate the corneoscleral limbus: New insights for our understanding of limbal microenvironment. Investig. Ophthalmol. Vis. Sci. 2020, 61, 43. [Google Scholar] [CrossRef]
- Moramarco, A.; Sacchetti, M.; Franzone, F.; Segatto, M.; Cecchetti, D.; Miraglia, E.; Roberti, V.; Iacovino, C.; Giustini, S. Ocular surface involvement in patients with neurofibromatosis type 1 syndrome. Graefe’s Arch. Clin. Exp. Ophthalmol. 2020, 258, 1757–1762. [Google Scholar] [CrossRef]
- Owens, J. Determining druggability. Nat. Rev. Drug Discov. 2007, 6, 187. [Google Scholar] [CrossRef]
- Dixon, S.J.; Stockwell, B.R. Identifying druggable disease-modifying gene products. Curr. Opin. Chem. Biol. 2009, 13, 549–555. [Google Scholar] [CrossRef]
- Carito, V.; Ceccanti, M.; Cestari, V.; Natella, F.; Bello, C.; Coccurello, R.; Mancinelli, R.; Fiore, M. Olive polyphenol effects in a mouse model of chronic ethanol addiction. Nutrition 2017, 33, 65–69. [Google Scholar] [CrossRef] [PubMed]
- Fiore, M.; Messina, M.P.; Petrella, C.; D’Angelo, A.; Greco, A.; Ralli, M.; Ferraguti, G.; Tarani, L.; Vitali, M.; Ceccanti, M. Antioxidant properties of plant polyphenols in the counteraction of alcohol-abuse induced damage: Impact on the Mediterranean diet. J. Funct. Foods 2020, 71, 104012. [Google Scholar] [CrossRef]
- Abe, T.; Morgan, D.A.; Gutterman, D.D. Protective role of nerve growth factor against postischemic dysfunction of sympathetic coronary innervation. Circulation 1997, 95, 213–220. [Google Scholar] [CrossRef] [PubMed]
- Aloe, L.; Rocco, M.L.; Bianchi, P.; Manni, L. Nerve growth factor: From the early discoveries to the potential clinical use. J. Transl. Med. 2012, 10, 239. [Google Scholar] [CrossRef] [PubMed]
- Chiaretti, A.; Piastra, M.; Caresta, E.; Nanni, L.; Aloe, L. Improving ischaemic skin revascularisation by nerve growth factor in a child with crush syndrome. Arch. Dis. Child 2002, 87, 446–448. [Google Scholar] [CrossRef] [PubMed][Green Version]
- Watanabe, T.; Inoue, M.; Sasaki, K.; Araki, M.; Uehara, S.; Monden, K.; Saika, T.; Nasu, Y.; Kumon, H.; Chancellor, M.B. Nerve growth factor level in the prostatic fluid of patients with chronic prostatitis/chronic pelvic pain syndrome is correlated with symptom severity and response to treatment. BJU Int. 2011, 108, 248–251. [Google Scholar] [CrossRef]
- Warrington, R.J.; Lewis, K.E. Natural antibodies against nerve growth factor inhibit in vitro prostate cancer cell metastasis. Cancer Immunol. Immunother. 2011, 60, 187–195. [Google Scholar] [CrossRef]
- Festuccia, C.; Muzi, P.; Gravina, G.L.; Millimaggi, D.; Speca, S.; Dolo, V.; Ricevuto, E.; Vicentini, C.; Bologna, M. Tyrosine kinase inhibitor CEP-701 blocks the NTRK1/NGF receptor and limits the invasive capability of prostate cancer cells in vitro. Int. J. Oncol. 2007, 30, 193–200. [Google Scholar] [CrossRef]
- Thiele, C.J.; Li, Z.; McKee, A.E. On Trk—The TrkB signal transduction pathway is an increasingly important target in cancer biology. Clin. Cancer Res. 2009, 15, 5962–5967. [Google Scholar] [CrossRef]
- Chiarenza, A.; Lazarovici, P.; Lempereur, L.; Cantarella, G.; Bianchi, A.; Bernardini, R. Tamoxifen inhibits nerve growth factor-induced proliferation of the human breast cancerous cell line MCF-7. Cancer Res. 2001, 61, 3002–3008. [Google Scholar]
- Chen, P.S.; Chen, L.S.; Cao, J.M.; Sharifi, B.; Karagueuzian, H.S.; Fishbein, M.C. Sympathetic nerve sprouting, electrical remodeling and the mechanisms of sudden cardiac death. Cardiovasc. Res. 2001, 50, 409–416. [Google Scholar] [CrossRef] [PubMed]
- Salvinelli, F.; Frari, V.; Rocco, M.L.; Rosso, P.; Aloe, L. Enhanced presence of NGF and mast cells number in nasal cavity after autologous stimulation: Relation with sensorineural hearing deficit. Eur. Rev. Med. Pharmacol. Sci. 2015, 19, 381–391. [Google Scholar]
- Povarnina, P.Y.; Vorontsova, O.N.; Gudasheva, T.A.; Ostrovskaya, R.U.; Seredenin, S.B. Original nerve growth factor mimetic dipeptide GK-2 restores impaired cognitive functions in rat models of Alzheimer’s disease. Acta Naturae 2013, 5, 84–91. [Google Scholar] [CrossRef]
- Head, B.P.; Patel, H.H.; Insel, P.A. Interaction of membrane/lipid rafts with the cytoskeleton: Impact on signaling and function: Membrane/lipid rafts, mediators of cytoskeletal arrangement and cell signaling. Biochim. Biophys. Acta Biomembr. 2014, 1838, 532–545. [Google Scholar] [CrossRef] [PubMed]
- Pryor, S.; McCaffrey, G.; Young, L.R.; Grimes, M.L. NGF causes TrKA to specifically attract microtubules to lipid rafts. PLoS ONE 2012, 7, e35163. [Google Scholar] [CrossRef]
- Kropf, E.; Fahnestock, M. Effects of reactive oxygen and nitrogen species on trka expression and signalling: Implications for prongf in aging and alzheimer’s disease. Cells 2021, 10, 1983. [Google Scholar] [CrossRef]
- Manoj, K.M. Murburn concept: Murzyme roles of redox proteins in xenobiotic metabolism and ATP-synthesis. Biomed. Rev. 2023, 34, 27. [Google Scholar] [CrossRef]
- Manoj, K.M.; Jaeken, L. Synthesis of theories on cellular powering, coherence, homeostasis and electro-mechanics: Murburn concept and evolutionary perspectives. J. Cell Physiol. 2023, 238, 931–953. [Google Scholar] [CrossRef]
- Francati, S.; Fiore, M.; Ferraguti, G. The janus face of oxidative stress in health and disease: The cause or the cure? Biomed. Rev. 2023, 34, 13. [Google Scholar] [CrossRef]
- Lurz, J.; Ladwig, K.H. Mind and body interventions in cardiology: The importance of the brain–heart connection. Herz 2022, 47, 103–109. [Google Scholar] [CrossRef] [PubMed]
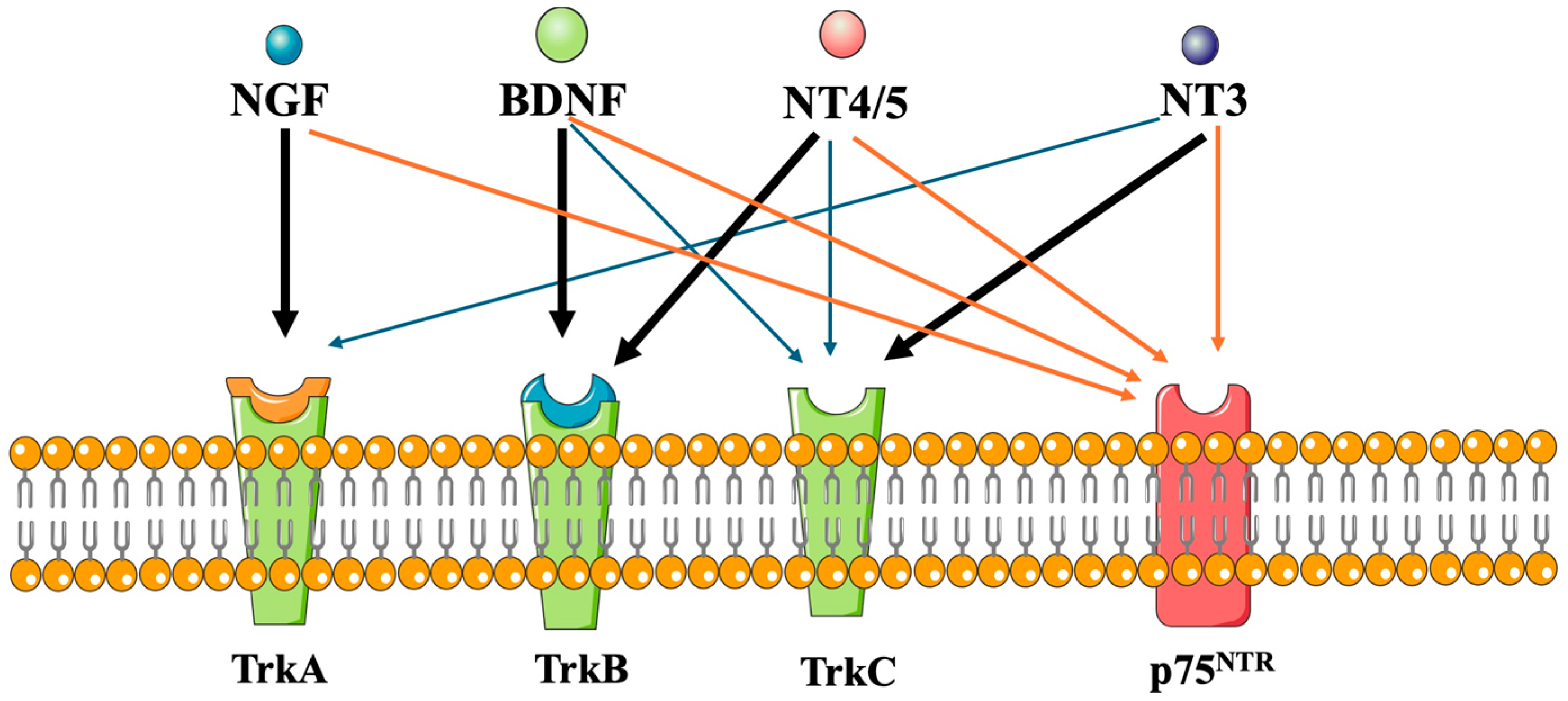
| Receptors * | Neurotrophins |
|---|---|
| p75NTR | NGF, BDNF, NT-3. NT-4/5 |
| TrkA | NGF, pro-NGF |
| TrkB | BDNF, pro-BDNF, NT-4/5 |
| TrkC | NT-3 |
| Physiotherapeutic | Pathogenic |
|---|---|
| Neurotrophic [13,14,15,16] | Oncotrophic (cancerogenic) [17,18,19,20] |
| Immunotrophic [21,22] | Nociceptogenic [23] |
| Меtabotrophic [5,6,22] | Arrhythmogenic [24] * |
| Psychotrophic [20,25,26,27,28,29,30] | Pruritus [31,32] |
| Cognitogenic [33,34,35,36,37,38,39,40,41,42] | Dry-eye disease [43] |
| Angiogenic [44,45,46,47,48,49,50,51,52,53] | |
| Sperm vitality, mobility, fertility [54] | |
| Skin, cornea, axon and bone wound/fracture healing [31,32,43,55,56,57,58,59,60,61,62,63,64,65,66,67,68,69,70] | |
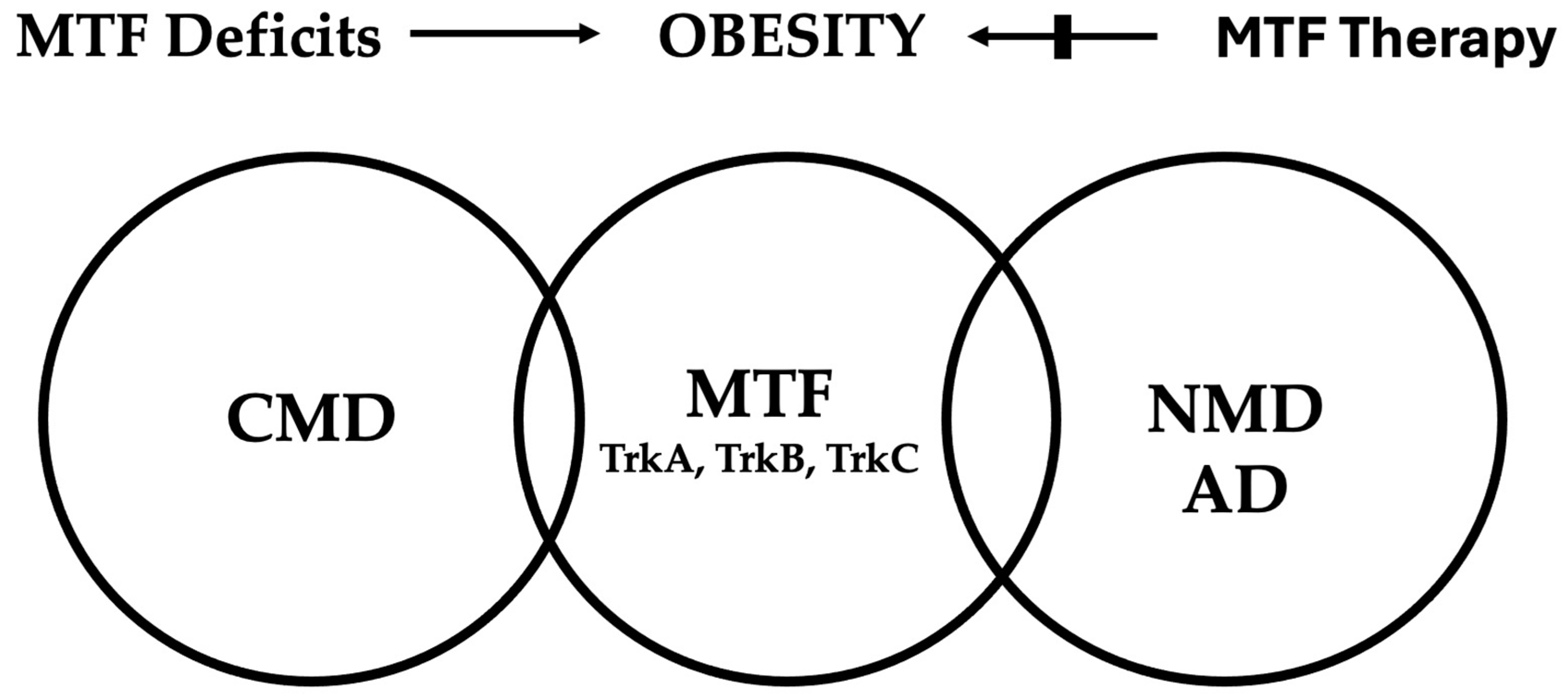
| NGF and BDNF are released by pancreatic beta cells and have an insulinotropic effect |
| NGF has homology with proinsulin |
| BDNF-deficient mice may develop metabolic syndrome-like abnormalities |
| NGF up-regulates the expression of PPAR-gamma |
| NGF and BDNF are trophic factors for pancreatic beta cells |
| BDNF improves cognition |
| NGF up-regulates the expression of LDL receptor-related proteins |
| NGF increases skin and corneal wound healing |
| NGF inhibits glucose-induced down-regulation of caveolin-1 |
| NGF increases diabetic erectile dysfunction |
| NGF may rescue silent myocardial ischemia in diabetes mellitus |
| A healthy lifestyle potentiates brain and/or circulating BDNF and NGF |
| An atherogenic diet reduces brain BDNF |
| BDNF potentiates cognitive processes |
| BDNF-deficient mice may develop abnormalities similar to the metabolic syndrome |
| Agonists | Antagonists |
|---|---|
| TrkANGF, TrkApro-NGF, TrkBBDNF, TrkCNT−3 | TrkANGF |
| Cardiometabolic diseases | Cancers |
| Atherosclerosis, hypertension | Prostate, Breast |
| Obesity, T2DM *, metabolic syndrome | Brain, Pancreas, Lung |
| Atrial fibrillation | |
| Diabetic erectile dysfunction | |
| Cardiovascular diseases | |
| Arrhythmogenic right ventricular dysplasia | |
| Sudden cardiac death | |
| Neurometabolic diseases | |
| Alzheimer’s disease (T3DM) * | Pain |
| Parkinson’s disease | Pruritus |
| Multiple sclerosis | |
| Wounds | |
| Skin, cornea, bone, axon |
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2024 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Chaldakov, G.N.; Aloe, L.; Yanev, S.G.; Fiore, M.; Tonchev, A.B.; Vinciguerra, M.; Evtimov, N.T.; Ghenev, P.; Dikranian, K. Trackins (Trk-Targeting Drugs): A Novel Therapy for Different Diseases. Pharmaceuticals 2024, 17, 961. https://doi.org/10.3390/ph17070961
Chaldakov GN, Aloe L, Yanev SG, Fiore M, Tonchev AB, Vinciguerra M, Evtimov NT, Ghenev P, Dikranian K. Trackins (Trk-Targeting Drugs): A Novel Therapy for Different Diseases. Pharmaceuticals. 2024; 17(7):961. https://doi.org/10.3390/ph17070961
Chicago/Turabian StyleChaldakov, George N., Luigi Aloe, Stanislav G. Yanev, Marco Fiore, Anton B. Tonchev, Manlio Vinciguerra, Nikolai T. Evtimov, Peter Ghenev, and Krikor Dikranian. 2024. "Trackins (Trk-Targeting Drugs): A Novel Therapy for Different Diseases" Pharmaceuticals 17, no. 7: 961. https://doi.org/10.3390/ph17070961
APA StyleChaldakov, G. N., Aloe, L., Yanev, S. G., Fiore, M., Tonchev, A. B., Vinciguerra, M., Evtimov, N. T., Ghenev, P., & Dikranian, K. (2024). Trackins (Trk-Targeting Drugs): A Novel Therapy for Different Diseases. Pharmaceuticals, 17(7), 961. https://doi.org/10.3390/ph17070961








