Ultrasonographic Diagnosis of Fetal Hypospadias
Abstract
:1. Introduction
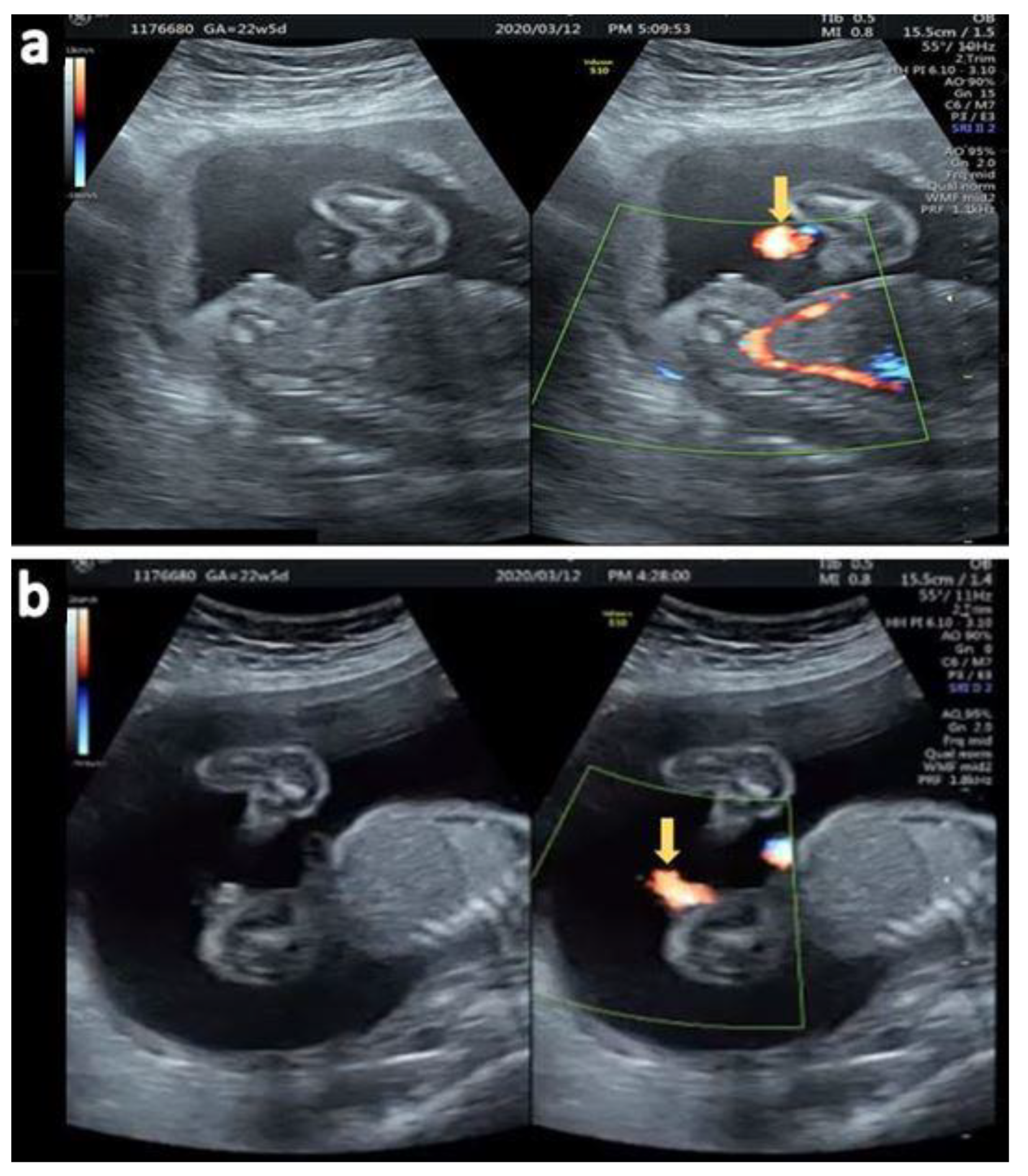
2. Case Reports
2.1. Case 1
2.2. Case 2
2.3. Case 3
2.4. Case 4
3. Discussion
Funding
Institutional Review Board Statement
Informed Consent Statement
Conflicts of Interest
References
- CDC Birth Defects Surveillance Toolkit 4.8 Congenital Malformations of Genital Organs. Available online: https://www.cdc.gov/ncbddd/birthdefects/surveillancemanual/chapters/chapter-4/chapter4-8.html (accessed on 11 February 2022).
- Baskin, L.S.; Erol, A.; Li, Y.W.; Cunha, G.R. Anatomical studies of hypospadias. J. Urol. 1998, 160, 1108. [Google Scholar] [CrossRef]
- van der Horst, H.J.; de Wall, L.L. Hypospadias, all there is to know. Eur. J. Pediatr. 2017, 176, 435–441. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Gürel, S.A. Prenatal Diagnosis of Isolated Hypospadias by Using “Tulip Sign” with Two and Three-Dimensional Ultrasonography. Gynecol. Obstet. Reprod. Med. 2016, 22, 54–56. [Google Scholar] [CrossRef] [Green Version]
- Sparks, T.N. Hypospadias. Am. J. Obstet. Gynecol. 2021, 225, B18–B20. [Google Scholar] [CrossRef] [PubMed]
- Brouwers, M.M.; Feitz, W.F.; Roelofs, L.A.; Kiemeney, L.A.; De Gier, R.P.; Roeleveld, N. Risk factors for hypospadias. Eur. J. Pediatr. 2007, 166, 671. [Google Scholar] [CrossRef] [PubMed]
- Utsch, B.; Albers, N.; Ludwig, M. Genetic and molecular aspects of hypospadias. Eur. J. Pediatr. Surg. 2004, 14, 297. [Google Scholar] [CrossRef] [PubMed]
- Epelboym, Y.; Estrada, C.; Estroff, J. Ultrasound diagnosis of fetal hypospadias: Accuracy and outcomes. J. Pediatr. Urol. 2017, 13, 484.e1–484.e4. [Google Scholar] [CrossRef] [PubMed]











Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2022 by the author. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Law, K.-S. Ultrasonographic Diagnosis of Fetal Hypospadias. Diagnostics 2022, 12, 774. https://doi.org/10.3390/diagnostics12040774
Law K-S. Ultrasonographic Diagnosis of Fetal Hypospadias. Diagnostics. 2022; 12(4):774. https://doi.org/10.3390/diagnostics12040774
Chicago/Turabian StyleLaw, Kim-Seng. 2022. "Ultrasonographic Diagnosis of Fetal Hypospadias" Diagnostics 12, no. 4: 774. https://doi.org/10.3390/diagnostics12040774
APA StyleLaw, K.-S. (2022). Ultrasonographic Diagnosis of Fetal Hypospadias. Diagnostics, 12(4), 774. https://doi.org/10.3390/diagnostics12040774





