Relevance of HLA-DQB1*02 Allele in the Genetic Predisposition of Children with Celiac Disease: Additional Cues from a Meta-Analysis
Abstract
1. Introduction
2. Materials and Methods
2.1. Protocol
2.2. Search Strategy
2.3. Data Extraction
2.4. Data Synthesis and Meta-Analysis
3. Results
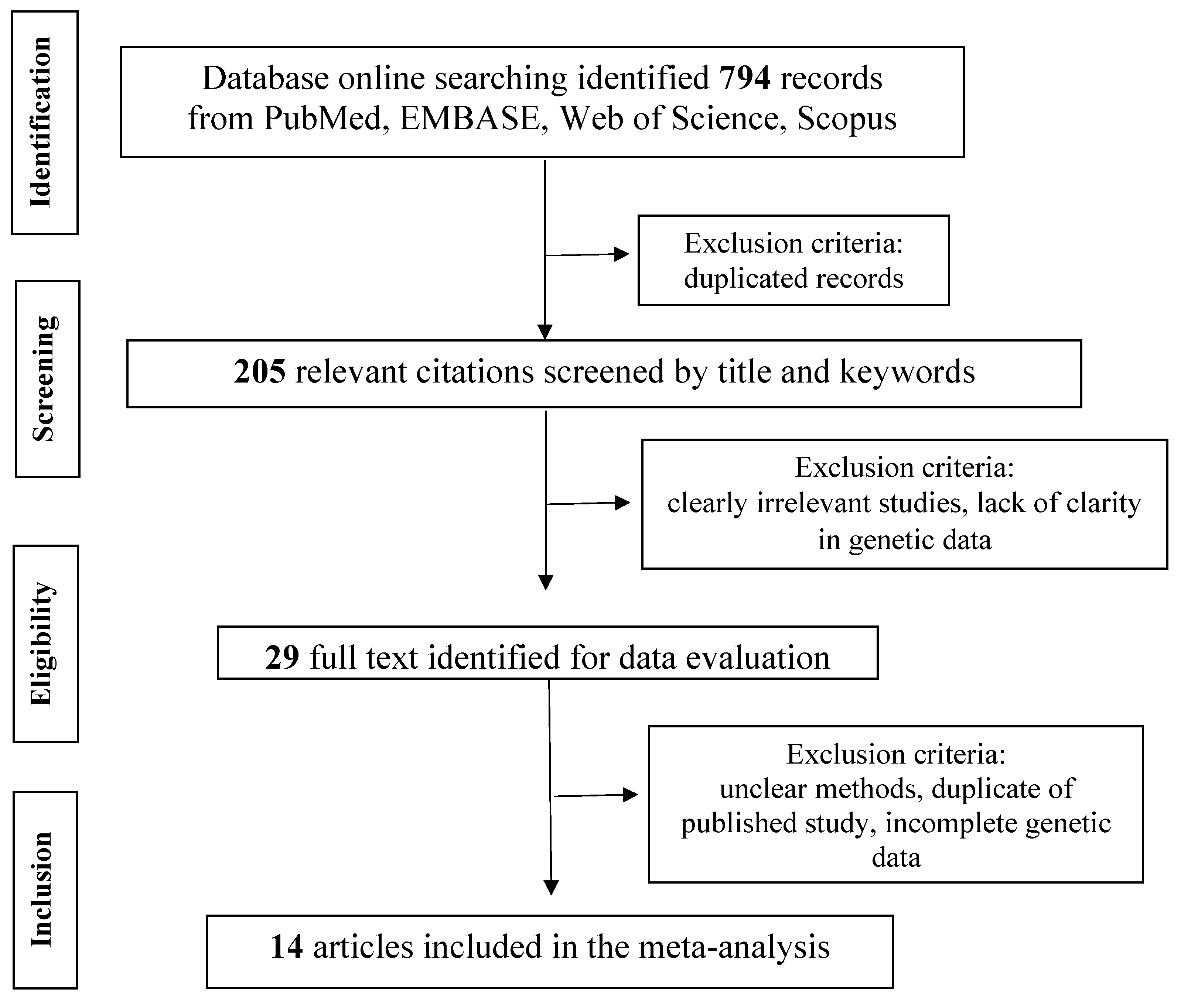
3.1. Study Selection
3.2. Study Quality
3.3. Meta-Analysis According to the Complete MHC-DQ2 and/or DQ8 Genotype
3.4. Meta-Analysis According to the Isolated Presence of HLA-DQB1*02 Allele
4. Discussion
5. Conclusions
Author Contributions
Funding
Conflicts of Interest
References
- Lindfors, K.; Ciacci, C.; Kurppa, K.; Lundin, K.E.A.; Makharia, G.K.; Mearin, M.L.; Murray, J.A.; Verdu, E.F.; Kaukinen, K. Coeliac disease. Nat. Rev. Dis. Primers 2019, 5, 3. [Google Scholar] [CrossRef] [PubMed]
- Lebwohl, B.; Sanders, D.S.; Green, P.H.R. Coeliac disease. Lancet 2018, 391, 70–81. [Google Scholar] [CrossRef]
- Ludvigsson, J.F. Mortality and malignancy in celiac disease. Gastrointest. Endosc. Clin. N. Am. 2012, 22, 705–722. [Google Scholar] [CrossRef]
- Abdul Sultan, A.; Crooks, C.J.; Card, T.; Tata, L.J.; Fleming, K.M.; West, J. Causes of death in people with coeliac disease in England compared with the general population: A competing risk analysis. Gut 2015, 64, 1220–1226. [Google Scholar] [CrossRef] [PubMed]
- Paarlahti, P.; Kurppa, K.; Ukkola, A.; Collin, P.; Huhtala, H.; Mäki, M.; Kaukinen, K. Predictors of persistent symptoms and reduced quality of life in treated coeliac disease patients: A large cross-sectional study. BMC Gastroenterol. 2013, 13, 75. [Google Scholar] [CrossRef]
- Stordal, K.; Bakken, I.J.; Suren, P. Epidemiology of coeliac disease and comorbidity in Norwegian children. J. Pediatr. Gastroenterol. Nutr. 2013, 57, 467–471. [Google Scholar] [CrossRef] [PubMed]
- Bjorck, S.; Brundin, C.; Lorinc, E.; Lynch, K.F.; Agardh, D. Screening detects a high proportion of celiac disease in young HLA-genotyped children. J. Pediatr. Gastroenterol. Nutr. 2010, 50, 49–53. [Google Scholar] [CrossRef]
- De Silvestri, A.; Capittini, C.; Poddighe, D.; Valsecchi, C.; Marseglia, G.; Tagliacarne, S.C.; Scotti, V.; Rebuffi, C.; Pasi, A.; Martinetti, M.; Tinelli, C. HLA-DQ genetics in children with celiac disease: A meta-analysis suggesting a two-step genetic screening procedure starting with HLA-DQ β chains. Pediatr. Res. 2018, 83, 564–572. [Google Scholar] [CrossRef]
- Husby, S.; Koletzko, S.; Korponay-Szabó, I.R.; Mearin, M.L.; Phillips, A.; Shamir, R.; Troncone, R.; Giersiepen, K.; Branski, D.; Catassi, C.; et al. ESPGHAN Working Group on Coeliac Disease Diagnosis; ESPGHAN Gastroenterology Committee; European Society for Pediatric Gastroenterology, Hepatology, and Nutrition. European Society for Pediatric Gastroenterology, Hepatology, and Nutrition guidelines for the diagnosis of coeliac disease. J. Pediatr. Gastroenterol. Nutr. 2012, 54, 136–160. [Google Scholar] [PubMed]
- Poddighe, D. Individual screening strategy for pediatric celiac disease. Eur. J. Pediatr. 2018, 177, 1871. [Google Scholar] [CrossRef] [PubMed]
- Verma, A.K.; Singh, A.; Gatti, S.; Lionetti, E.; Galeazzi, T.; Monachesi, C.; Franceschini, E.; Ahuja, V.; Catassi, C.; Makharia, G.K. Validation of a novel single-drop rapid human leukocyte antigen-DQ2/-DQ8 typing method to identify subjects susceptible to celiac disease. JGH Open 2018, 2, 311–316. [Google Scholar] [CrossRef]
- Poddighe, D. Relevance of HLA-DQB1*02 allele in predisposing to Coeliac Disease. Int. J. Immunogenet. 2019, in press. [Google Scholar] [CrossRef]
- Moher, D.; Liberati, A.; Tetzlaff, J.; Altman, D.G.; PRISMA Group. Preferred reporting items for systematic reviews and meta-analyses: The PRISMA statement. J. Clin. Epidemiol. 2009, 62, 1006–1012. [Google Scholar] [CrossRef]
- Meeuwisse, G.W. Round table discussion. Diagnostic criteria in coeliac disease. Acta Paediatr. Scand. 1970, 59, 461–463. [Google Scholar]
- Walker-Smith, J.A.; Guandalini, S.; Schmitz, J. Revised criteria for diagnosis of coeliac disease. Arch. Dis. Child. 1990, 65, 909–911. [Google Scholar]
- Zamora, J.; Abraira, V.; Muriel, A.; Khan, K.; Coomarasamy, A. Meta-DiSc: A software for metaanalysis of test accuracy data. BMC Med. Res. Methodol. 2006, 6, 31. [Google Scholar] [CrossRef] [PubMed]
- Higgins, J.P.; Thompson, S.G. Quantifying heterogeneity in a meta-analysis. Stat. Med. 2002, 21, 1539–1558. [Google Scholar] [CrossRef] [PubMed]
- Der Simonian, R.; Laird, N. Meta-analysis in clinical trials. Control. Clin. Trials 1986, 7, 177–188. [Google Scholar] [CrossRef]
- Higgins, J.P.T.; Green, S. Cochrane Handbook for Systematic Reviews of Interventions, Version 5.1.0 (updated March 2011). The Cochrane Collaboration. Available online: http:// www.cochrane-handbook.org (accessed on 1 March 2015).
- Araya, M.; Oyarzun, A.; Lucero, Y.; Espinosa, N.; Pérez-Bravo, F. DQ2, DQ7 and DQ8 Distribution and Clinical Manifestations in Celiac Cases and Their First-Degree Relatives. Nutrients 2015, 7, 4955–4965. [Google Scholar] [CrossRef] [PubMed]
- Araya, M.; Mondragón, A.; Pérez-Bravo, F.; Roessler, J.L.; Alarcón, T.; Rios, G.; Bergenfreid, C. Celiac disease in a Chilean population carrying Amerindian traits. J. Pediatr. Gastroenterol. Nutr. 2000, 31, 381–386. [Google Scholar] [CrossRef]
- Bonamico, M.; Ferri, M.; Mariani, P.; Nenna, R.; Thanasi, E.; Luparia, R.P.; Picarelli, A.; Magliocca, F.M.; Mora, B.; Bardella, M.T.; Verrienti, A.; et al. Serologic and genetic markers of celiac disease: A sequential study in the screening of first degree relatives. J. Pediatr. Gastroenterol. Nutr. 2006, 42, 150–154. [Google Scholar] [CrossRef]
- Cintado, A.; Sorell, L.; Galván, J.A.; Martínez, L.; Castañeda, C.; Fragoso, T.; Camacho, H.; Ferrer, A.; Companioni, O.; Benitez, J.; et al. HLA DQA1*0501 and DQB1*02 in Cuban celiac patients. Hum. Immunol. 2006, 67, 639–642. [Google Scholar] [CrossRef]
- El-Akawi, Z.J.; Al-Hattab, D.M.; Migdady, M.A. Frequency of HLA-DQA1*0501 and DQB1*0201 alleles in patients with coeliac disease, their first-degree relatives and controls in Jordan. Ann. Trop. Paediatr. 2010, 30, 305–309. [Google Scholar] [CrossRef] [PubMed]
- Farré, C.; Humbert, P.; Vilar, P.; Varea, V.; Aldeguer, X.; Carnicer, J.; Carballo, M.; Gassull, M.A. Serological markers and HLA-DQ2 haplotype among first-degree relatives of celiac patients. Dig. Dis. Sci. 1999, 44, 2344–2349. [Google Scholar] [CrossRef] [PubMed]
- Karinen, H.; Kärkkäinen, P.; Pihlajamäki, J.; Janatuinen, E.; Heikkinen, M.; Julkunen, R.; Kosma, V.M.; Naukkarinen, A.; Laakso, M. HLA genotyping is useful in the evaluation of the risk for coeliac disease in the 1st-degree relatives of patients with coeliac disease. Scand. J. Gastroenterol. 2006, 41, 1299–1304. [Google Scholar] [CrossRef]
- Martins, R.C.; Gandolfi, L.; Modelli, I.C.; Almeida, R.C.; Castro, L.C.; Pratesi, R. Serologic screening and genetic testing among brazilian patients with celiac disease and their first degree relatives. Arq. Gastroenterol. 2010, 47, 257–262. [Google Scholar] [CrossRef]
- Megiorni, F.; Mora, B.; Bonamico, M.; Barbato, M.; Nenna, R.; Maiella, G.; Lulli, P.; Mazzilli, MC. HLA-DQ and risk gradient for celiac disease. Hum. Immunol. 2009, 70, 55–59. [Google Scholar] [CrossRef]
- Mishra, A.; Prakash, S.; Kaur, G.; Sreenivas, V.; Ahuja, V.; Gupta, S.D.; Makharia, G.K. Prevalence of celiac disease among first-degree relatives of Indian celiac disease patients. Dig. Liver Dis. 2016, 48, 255–259. [Google Scholar] [CrossRef]
- Rubio-Tapia, A.; Van Dyke, C.T.; Lahr, B.D.; Zinsmeister, A.R.; El-Youssef, M.; Moore, S.B.; Bowman, M.; Burgart, L.J.; Melton III, L.J.; Murray, J.A. Predictors of family risk for celiac disease: A population-based study. Clin. Gastroenterol. Hepatol. 2008, 6, 983–987. [Google Scholar] [CrossRef]
- Singla, S.; Kumar, P.; Singh, P.; Kaur, G.; Rohtagi, A.; Choudhury, M. HLA Profile of Celiac Disease among First-Degree Relatives from a Tertiary Care Center in North India. Ind. J. Pediatr. 2016, 83, 1248–1252. [Google Scholar] [CrossRef]
- Srivastava, A.; Yachha, S.K.; Mathias, A.; Parveen, F.; Poddar, U.; Agrawal, S. Prevalence, human leukocyte antigen typing and strategy for screening among Asian first-degree relatives of children with celiac disease. J. Gastroenterol. Hepatol. 2010, 25, 319–324. [Google Scholar] [CrossRef]
- Vaquero, L.; Caminero, A.; Nuñez, A.; Hernando, M.; Iglesias, C.; Casqueiro, J.; Vivas, S. Coeliac disease screening in first-degree relatives on the basis of biopsy and genetic risk. Eur. J. Gastroenterol. Hepatol. 2014, 26, 263–267. [Google Scholar] [CrossRef]
- Dorn, S.D.; Matchar, D.B. Cost-effectiveness analysis of strategies for diagnosing celiac disease. Dig. Dis. Sci. 2008, 53, 680–688. [Google Scholar] [CrossRef] [PubMed]
- Megiorni, F.; Pizzuti, A. HLA-DQA1 and HLA-DQB1 in Celiac disease predisposition: Practical implications of the HLA molecular typing. J. Biomed. Sci. 2012, 19, 88. [Google Scholar] [CrossRef]
- Vader, W.; Stepniak, D.; Kooy, Y.; Mearin, L.; Thompson, A.; van Rood, J.J.; Spaenij, L.; Koning, F. The HLA-DQ2 gene dose effect in celiac disease is directly related to the magnitude and breadth of gluten specific T cell responses. Proc. Natl. Acad. Sci. USA 2003, 100, 12390–12395. [Google Scholar] [CrossRef]
- Sollid, L.M. Coeliac disease: Dissecting a complex inflammatory disorder. Nat. Rev. Immunol. 2002, 2, 647–655. [Google Scholar] [CrossRef]
- Poddighe, D.; Capittini, C.; Gaviglio, I.; Brambilla, I.; Marseglia, G.L. HLA-DQB1*02 allele in children with Celiac Disease: Potential usefulness for screening strategies. Int. J. Immunogenet. 2019, in press. [Google Scholar] [CrossRef]
- Fernández-Fernández, S.; Borrell, B.; Cilleruelo, M.L.; Tabares, A.; Jiménez-Jiménez, J.; Rayo, A.I.; Perucho, T.; García-García, M.L. Prevalence of Celiac Disease in a Long-Term Study of a Spanish At-Genetic-Risk Cohort from the General Population. J. Pediatr. Gastroenterol. Nutr. 2019, 68, 364–370. [Google Scholar] [CrossRef]
- Cilleruelo, M.L.; Fernández-Fernández, S.; Jiménez-Jiménez, J.; Rayo, A.I.; de Larramendi, C.H. Prevalence and Natural History of Celiac Disease in a Cohort of At-risk Children. J. Pediatr. Gastroenterol. Nutr. 2016, 62, 739–745. [Google Scholar] [CrossRef] [PubMed]
- Wessels, M.M.S.; de Rooij, N.; Roovers, L.; Verhage, J.; de Vries, W.; Mearin, M.L. Towards an individual screening strategy for first-degree relatives of celiac patients. Eur. J. Pediatr. 2018, 177, 1585–1592. [Google Scholar] [CrossRef]
- Makharia, G.K.; Catassi, C. Celiac Disease in Asia. Gastroenterol. Clin. N. Am. 2019, 48, 101–113. [Google Scholar]
- Poddighe, D.; Rakhimzhanova, M.; Marchenko, Y.; Catassi, C. Pediatric Celiac Disease in Central and East Asia: Current Knowledge and Prevalence. Medicina 2019, 55, 11. [Google Scholar] [CrossRef]
- Singh, P.; Arora, A.; Strand, T.A.; Leffler, DA.; Catassi, C.; Green, P.H.; Kelly, C.P.; Ahuja, V.; Makharia, G.K. Global Prevalence of Celiac Disease: Systematic Review and Meta-analysis. Clin. Gastroenterol. Hepatol. 2018, 16, 823–836. [Google Scholar] [CrossRef]

| Summary—Positive Likelihood Ratio (Random Effects Model) | ||||
|---|---|---|---|---|
| Study (Year) | Country | LR+ | 95% Conf. Interval | % Weight |
| Araya et al. (2015) | Chile | 1.008 | 0.749–1.357 | 5.92 |
| Araya et al. (2000) | Chile | 7.557 | 4.475–12.762 | 3.47 |
| Bonamico et al. (2006) | Italy | 1.779 | 1.572–2.014 | 8.20 |
| Cintado et al. (2006) | Cuba | 1.054 | 0.809–1.372 | 6.38 |
| Elakawi et al. (2010) | Jordan | 1.487 | 1.061–2.084 | 5.40 |
| Farre et al. (1999) | Spain | 1.563 | 1.317–1.854 | 7.64 |
| Karinen et al. (2006) | Finland | 1.008–1.255 | 8.35 | |
| Martins et al. (2010) | Brazil | 1.691 | 1.393–2.052 | 7.35 |
| Megiorni et al. (2009) | Italy | 1.707 | 1.590–1.832 | 8.67 |
| Mishra et al. (2016) | India | 1.304 | 1.126–1.511 | 7.94 |
| Rubio-Tapia et al. (2010) | USA | 1.413 | 1.302–1.533 | 8.59 |
| Singla et al. (2016) | India | 1.148 | 1.040–1.268 | 8.45 |
| Srivastava et al. (2010) | India | 1.063 | 0.783–1.443 | 5.82 |
| Vaquero et al. (2014) | Spain | 1.530 | 1.309–1.789 | 7.83 |
| (REM) pooled LR+ | 1.449 | 1.279–1.642 | ||
| Summary—Negative Likelihood Ratio (Random Effects Model) | ||||
|---|---|---|---|---|
| Study (Year) | Country | LR− | 95% Conf. Interval | % Weight |
| Araya et al. (2015) | Chile | 0.933 | 0.065–13.461 | 4.86 |
| Araya et al. (2000) | Chile | 0.081 | 0.006–1.178 | 4.86 |
| Bonamico et al. (2006) | Italy | 0.107 | 0.028–0.416 | 11.74 |
| Cintado et al. (2006) | Cuba | 0.641 | 0.041–10.017 | 4.64 |
| Elakawi et al. (2010) | Jordan | 0.217 | 0.015–3.170 | 4.83 |
| Farre et al. (1999) | Spain | 0.108 | 0.007–1.636 | 4.72 |
| Karinen et al. (2006) | Finland | 0.526 | 0.265–1.044 | 18.52 |
| Martins et al. (2010) | Brazil | 0.158 | 0.024–1.054 | 7.99 |
| Megiorni et al. (2009) | Italy | 0.044 | 0.006–0.310 | 7.73 |
| Mishra et al. (2016) | India | 0.188 | 0.047–0.757 | 11.43 |
| Rubio-Tapia et al. (2010) | USA | 0.042 | 0.003–0.656 | 4.61 |
| Singla et al. (2016) | India | 0.173 | 0.011–2.730 | 4.61 |
| Srivastava et al. (2010) | India | 0.652 | 0.045–9.460 | 4.85 |
| Vaquero et al. (2014) | Spain | 0.043 | 0.003–0.674 | 4.60 |
| (REM) pooled LR− | 0.187 | 0.096–0.362 | ||
| Summary—Positive Likelihood Ratio (Random Effects Model) | |||
|---|---|---|---|
| Study (Year) | LR+ | 95% Conf. Interval | % Weight |
| Araya et al. (2015) | 7.557 | 4.475–12.762 | 9.44 |
| Cintado et al. (2006) | 1.054 | 0.809–1.372 | 14.07 |
| Elakawi et al. (2010) | 1.487 | 1.061–2.084 | 12.72 |
| Farre et al. (1999) | 1.563 | 1.317–1.854 | 15.58 |
| Karinen et al. (2006) | 1.125 | 1.008–1.255 | 16.32 |
| Martins et al. (2010) | 1.691 | 1.393–2.052 | 15.24 |
| Megiorni et al. (2009) | 1.707 | 1.590–1.832 | 16.64 |
| (REM) pooled LR+ | 1.659 | 1.302–2.115 | |
| Summary—Negative Likelihood Ratio (Random Effects Model) | |||
|---|---|---|---|
| Study (year) | LR− | 95% Conf. Interval | % Weight |
| Araya et al. (2015) | 0.081 | 0.006–1.178 | 10.43 |
| Cintado et al. (2006) | 0.641 | 0.041–10.017 | 10.03 |
| Elakawi et al. (2010) | 0.217 | 0.015–3.170 | 10.38 |
| Farre et al. (1999) | 0.108 | 0.007–1.636 | 10.18 |
| Karinen et al. (2006) | 0.526 | 0.265–1.044 | 28.05 |
| Martins et al. (2010) | 0.158 | 0.024–1.054 | 15.66 |
| Megiorni et al. (2009) | 0.044 | 0.006–0.310 | 15.26 |
| (REM) pooled LR− | 0.195 | 0.068–0.558 | |
© 2019 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (http://creativecommons.org/licenses/by/4.0/).
Share and Cite
Capittini, C.; De Silvestri, A.; Rebuffi, C.; Tinelli, C.; Poddighe, D. Relevance of HLA-DQB1*02 Allele in the Genetic Predisposition of Children with Celiac Disease: Additional Cues from a Meta-Analysis. Medicina 2019, 55, 190. https://doi.org/10.3390/medicina55050190
Capittini C, De Silvestri A, Rebuffi C, Tinelli C, Poddighe D. Relevance of HLA-DQB1*02 Allele in the Genetic Predisposition of Children with Celiac Disease: Additional Cues from a Meta-Analysis. Medicina. 2019; 55(5):190. https://doi.org/10.3390/medicina55050190
Chicago/Turabian StyleCapittini, Cristina, Annalisa De Silvestri, Chiara Rebuffi, Carmine Tinelli, and Dimitri Poddighe. 2019. "Relevance of HLA-DQB1*02 Allele in the Genetic Predisposition of Children with Celiac Disease: Additional Cues from a Meta-Analysis" Medicina 55, no. 5: 190. https://doi.org/10.3390/medicina55050190
APA StyleCapittini, C., De Silvestri, A., Rebuffi, C., Tinelli, C., & Poddighe, D. (2019). Relevance of HLA-DQB1*02 Allele in the Genetic Predisposition of Children with Celiac Disease: Additional Cues from a Meta-Analysis. Medicina, 55(5), 190. https://doi.org/10.3390/medicina55050190





