Age-Specific Differences in Foreign Bodies Ingested by Children: A Cohort Study of 252 Japanese Cases
Abstract
1. Introduction
2. Materials and Methods
2.1. Setting
2.2. Study Design and Methods
2.3. Definition
2.4. Classification
2.5. Statistical Analysis
3. Results
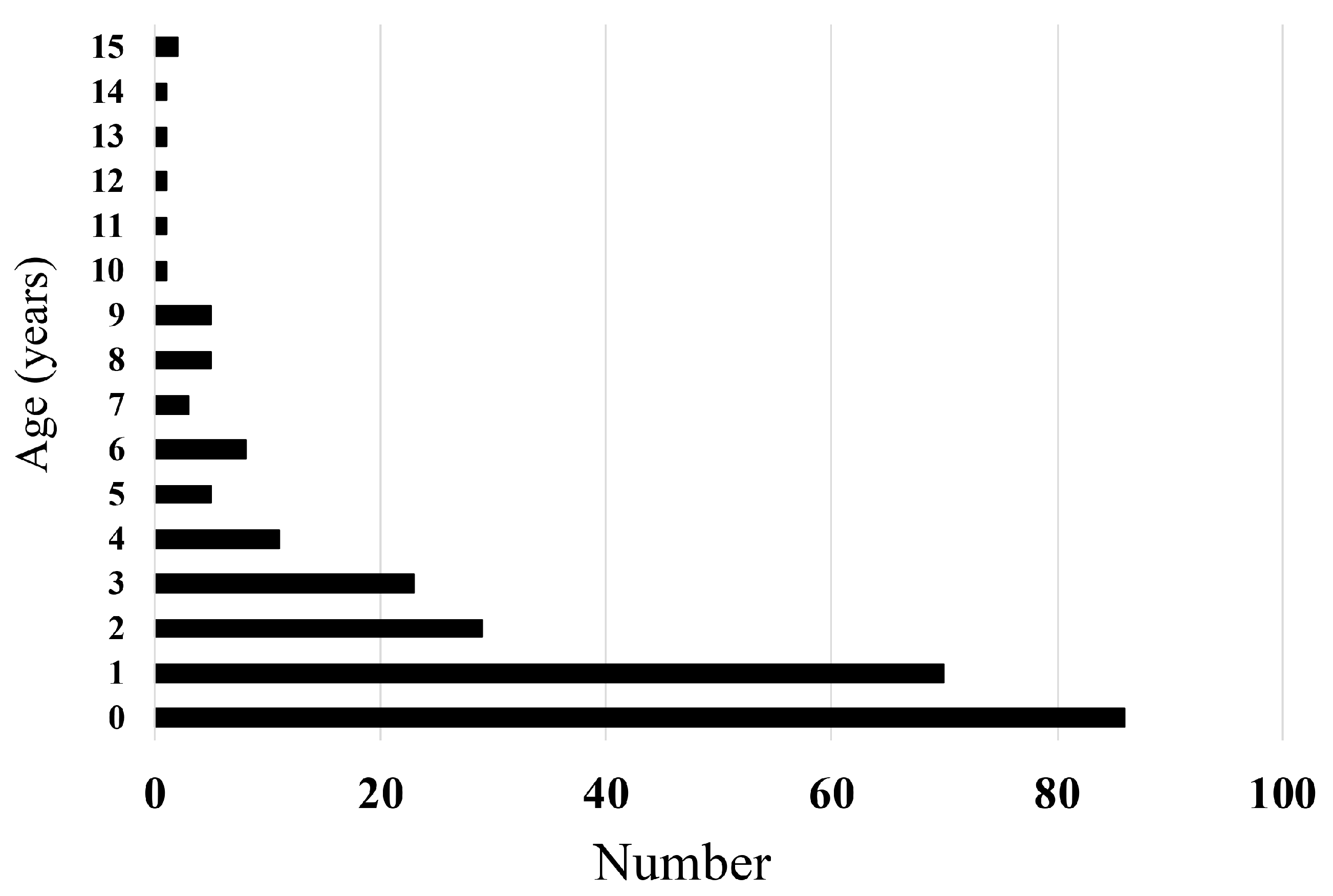
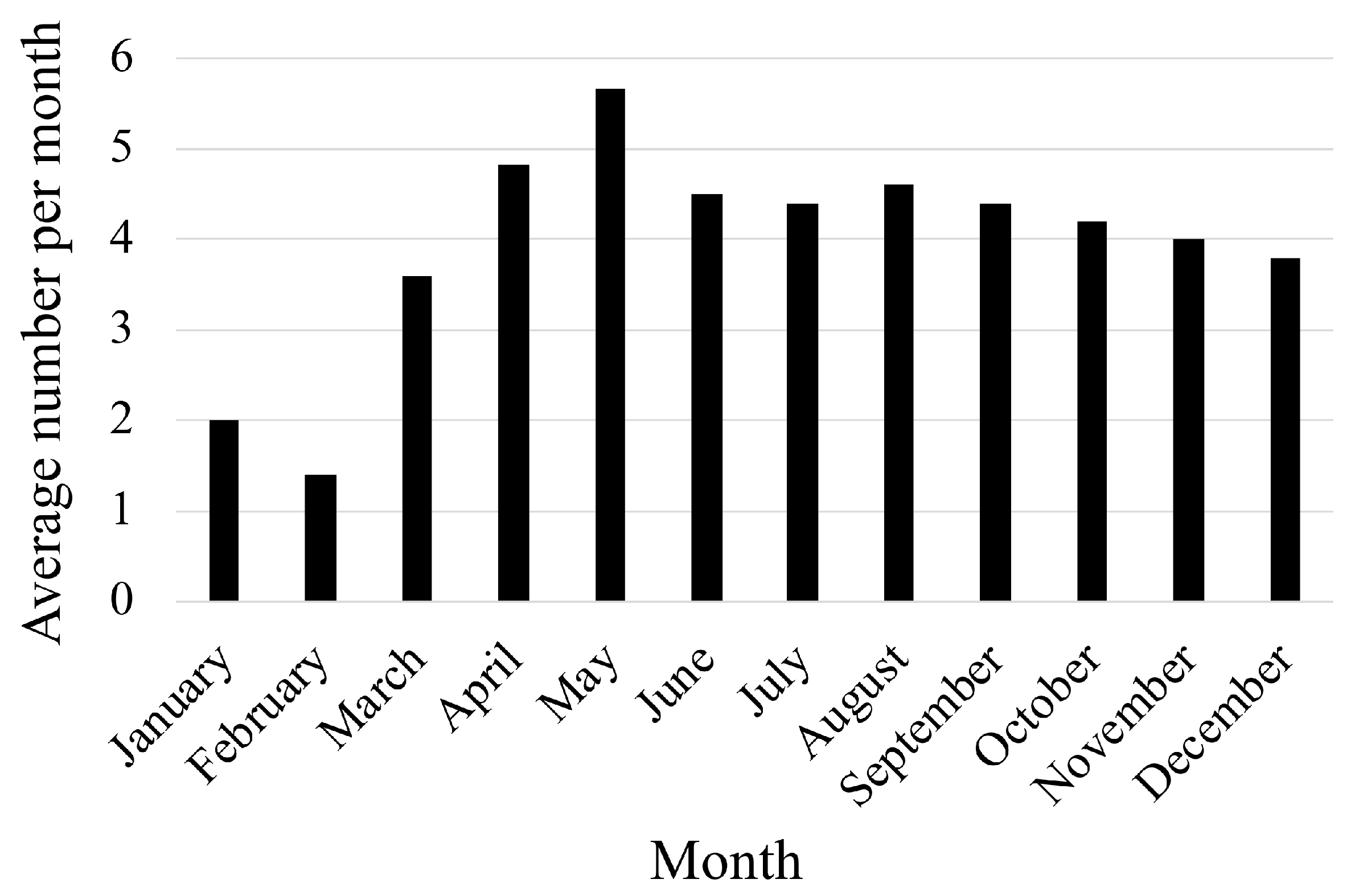
3.1. Patient Characteristics
3.2. Causes
3.3. Age-Specific Characteristics and Types of Foreign Bodies
4. Discussion
5. Conclusions
Author Contributions
Funding
Conflicts of Interest
References
- Kim, S.Y.; Park, B.; Kong, I.G.; Choi, H.G. Analysis of ingested foreign bodies according to age, type and location: A retrospective observational study. Clin. Otolaryngol. 2016, 41, 640–645. [Google Scholar] [CrossRef] [PubMed]
- Gummin, D.D.; Mowry, J.B.; Spyker, D.A.; Brooks, D.E.; Fraser, M.O.; Banner, W. 2016 Annual Report of the American Association of Poison Control Centers’ National Poison Data System (NPDS): 34th Annual Report. Clin. Toxicol. 2017, 55, 1072–1252. [Google Scholar] [CrossRef] [PubMed]
- Uyemura, M.C. Foreign body ingestion in children. Am. Fam. Physician 2005, 72, 287–291. [Google Scholar] [PubMed]
- Simic, M.A.; Budakov, B.M. Fatal upper esophageal hemorrhage caused by a previously ingested chicken bone: Case report. Am. J. Forensic Med. Pathol. 1998, 19, 166–168. [Google Scholar] [CrossRef] [PubMed]
- Yardeni, D.; Yardeni, H.; Coran, A.G.; Golladay, E.S. Severe esophageal damage due to button battery ingestion: Can it be prevented? Pediatr. Surg. Int. 2004, 20, 496–501. [Google Scholar] [CrossRef] [PubMed]
- Wyllie, R. Foreign bodies in the gastrointestinal tract. Curr. Opin. Pediatr. 2006, 18, 563–564. [Google Scholar] [CrossRef] [PubMed]
- Waltzman, M.L.; Baskin, M.; Wypij, D.; Mooney, D.; Jones, D.; Fleisher, G. A randomized clinical trial of the management of esophageal coins in children. Pediatrics 2005, 116, 614–619. [Google Scholar] [CrossRef] [PubMed]
- Kramer, R.E.; Lerner, D.G.; Lin, T.; Manfredi, M.; Shah, M.; Stephen, T.C.; Gibbons, T.E.; Pall, H.; Sahn, B.; McOmber, M.; et al. Management of ingested foreign bodies in children: A clinical report of the NASPGHAN Endoscopy Committee. J. Pediatr. Gastroenterol. Nutr. 2015, 60, 562–574. [Google Scholar] [CrossRef] [PubMed]
- Little, D.C.; Shah, S.R.; St Peter, S.D.; Calkins, C.M.; Morrow, S.E.; Murphy, J.P.; Sharp, R.J.; Andrews, W.S.; Holcomb, G.W., 3rd; Ostlie, D.J.; et al. Esophageal foreign bodies in the pediatric population: Our first 500 cases. J. Pediatr. Surg. 2006, 41, 914–918. [Google Scholar] [CrossRef] [PubMed]
- Banerjee, R.; Rao, G.V.; Sriram, P.V.; Reddy, K.S.; Nageshwar Reddy, D. Button battery ingestion. Indian J. Pediatr. 2005, 72, 173–174. [Google Scholar] [CrossRef] [PubMed]
- Ginsberg, G.G. Management of ingested foreign objects and food bolus impactions. Gastrointest. Endosc. 1995, 41, 33–38. [Google Scholar] [CrossRef]
- Webb, W.A. Management of foreign bodies of the upper gastrointestinal tract: Update. Gastrointest. Endosc. 1995, 41, 39–51. [Google Scholar] [CrossRef]
- Kurowski, J.A.; Kay, M. Caustic Ingestions and Foreign Bodies Ingestions in Pediatric Patients. Pediatr. Clin. N. Am. 2017, 64, 507–524. [Google Scholar] [CrossRef]
- Palta, R.; Sahota, A.; Bemarki, A.; Salama, P.; Simpson, N.; Laine, L. Foreign-body ingestion: Characteristics and outcomes in a lower socioeconomic population with predominantly intentional ingestion. Gastrointest. Endosc. 2009, 69 Pt 1, 426–433. [Google Scholar] [CrossRef]
- Kay, M.; Wyllie, R. Foreign body ingestions in the pediatric population and techniques of endoscopic removal. Tech. Gastrointest. Endosc. 2013, 15, 9–17. [Google Scholar] [CrossRef]
- Wai Pak, M.; Chung Lee, W.; Kwok Fung, H.; van Hasselt, C.A. A prospective study of foreign-body ingestion in 311 children. Int. J. Pediatr. Otorhinolaryngol. 2001, 58, 37–45. [Google Scholar] [CrossRef]
- Ministry of Health, Labour and Welfare, Smoking Status. The National Health and Nutrition Survey in Japan. 2017. 2018; pp. 54–56. Available online: https://www.mhlw.go.jp/content/000451755.pdf (accessed on 10 January 2020). (In Japanese)
- Arana, A.; Hauser, B.; Hachimi-Idrissi, S.; Vandenplas, Y. Management of ingested foreign bodies in childhood and review of the literature. Eur. J. Pediatr. 2001, 160, 468–472. [Google Scholar] [CrossRef]
- Schuldta, T.; Großmanna, W.; Weissa, N.M.; Ovarib, A.; Mlynskia, R.; Schravena, S.P. Aural and nasal foreign bodies in children—Epidemiology and correlation with hyperkinetic disorders, developmental disorders and congenital malformations. Int. J. Pediatr. Otorhinolaryngol. 2019, 118, 165–169. [Google Scholar] [CrossRef] [PubMed]
- Ministry of Health, Labour and Welfare. A Report on Accidental Ingestion Related to Household Items in Children. Health Hazard Monitoring Related to Household Items in Japan. 2017. 2018; pp. 15–34. Available online: https://www.mhlw.go.jp/content/11124000/000451980.pdf (accessed on 10 January 2019). (In Japanese)


| Background | N = 252 |
|---|---|
| Age (years) | 1 (0–15) |
| Male/Female | 140 (55%)/112 (44%) |
| Recurrence | 6 (2%) |
| Place of occurrence | |
| House | 170 (67%) |
| Public accommodation | 11 (4%) |
| Others | 71 (28%) |
| First aid by bystanders | 67 (27%) |
| Symptoms at the time of ingestion | |
| Absent | 151 (60%) |
| Present | 101 (40%) |
| Nausea and vomiting | 39 (15%) |
| Cough | 18 (7%) |
| Disturbance of consciousness | 14 (5%) |
| Pharyngeal pain | 9 (4%) |
| Displeasure | 7 (3%) |
| Crying | 6 (2%) |
| Abdominal pain and diarrhea | 5 (2%) |
| Pale | 2 (1%) |
| Respiratory distress | 2 (1%) |
| Age | <12 Months n = 86 | 1 to 6 Years n = 146 | ≥7 Years n = 20 | p-Value |
|---|---|---|---|---|
| Male/Female | 48 (56%)/38 (44%) | 82 (56%)/64 (44%) | 10 (50%)/10 (50%) | 0.872 |
| Symptoms | 38 (44%) | 55 (38%) | 8 (40%) | 0.620 |
| Occurrence at home | 60 (70%) | 101 (69%) | 9 (45%) | 0.082 |
| First aid provided | 30 (35%) | 34 (23%) | 3 (15%) | 0.073 |
| Major types | ||||
| Cigarettes | 20 (23%) | 23 (16%) | 1 (5%) | <0.01 |
| Plastics | 27 (31%) | 14 (10%) | 2 (10%) | |
| Chemicals | 8 (19%) | 19 (13%) | 0 (0%) | |
| Internal medicines | 0 (0%) | 20 (13%) | 6 (30%) | |
| Metals | 5 (6%) | 18 (12%) | 3 (15%) | |
| Others | 26 (30%) | 52 (36%) | 8 (40%) |
© 2020 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (http://creativecommons.org/licenses/by/4.0/).
Share and Cite
Fujisawa, J.; Mutoh, T.; Kawamura, K.; Yonezawa, R.; Hirai, M.; Morioka, I. Age-Specific Differences in Foreign Bodies Ingested by Children: A Cohort Study of 252 Japanese Cases. Medicina 2020, 56, 39. https://doi.org/10.3390/medicina56010039
Fujisawa J, Mutoh T, Kawamura K, Yonezawa R, Hirai M, Morioka I. Age-Specific Differences in Foreign Bodies Ingested by Children: A Cohort Study of 252 Japanese Cases. Medicina. 2020; 56(1):39. https://doi.org/10.3390/medicina56010039
Chicago/Turabian StyleFujisawa, Jumpei, Tomokazu Mutoh, Kengo Kawamura, Ryuta Yonezawa, Maiko Hirai, and Ichiro Morioka. 2020. "Age-Specific Differences in Foreign Bodies Ingested by Children: A Cohort Study of 252 Japanese Cases" Medicina 56, no. 1: 39. https://doi.org/10.3390/medicina56010039
APA StyleFujisawa, J., Mutoh, T., Kawamura, K., Yonezawa, R., Hirai, M., & Morioka, I. (2020). Age-Specific Differences in Foreign Bodies Ingested by Children: A Cohort Study of 252 Japanese Cases. Medicina, 56(1), 39. https://doi.org/10.3390/medicina56010039





