Effects of 12 Weeks of Resistance Training on Cardiovascular Risk Factors in School Adolescents
Abstract
1. Introduction
2. Materials and Methods
2.1. Ethics Statement
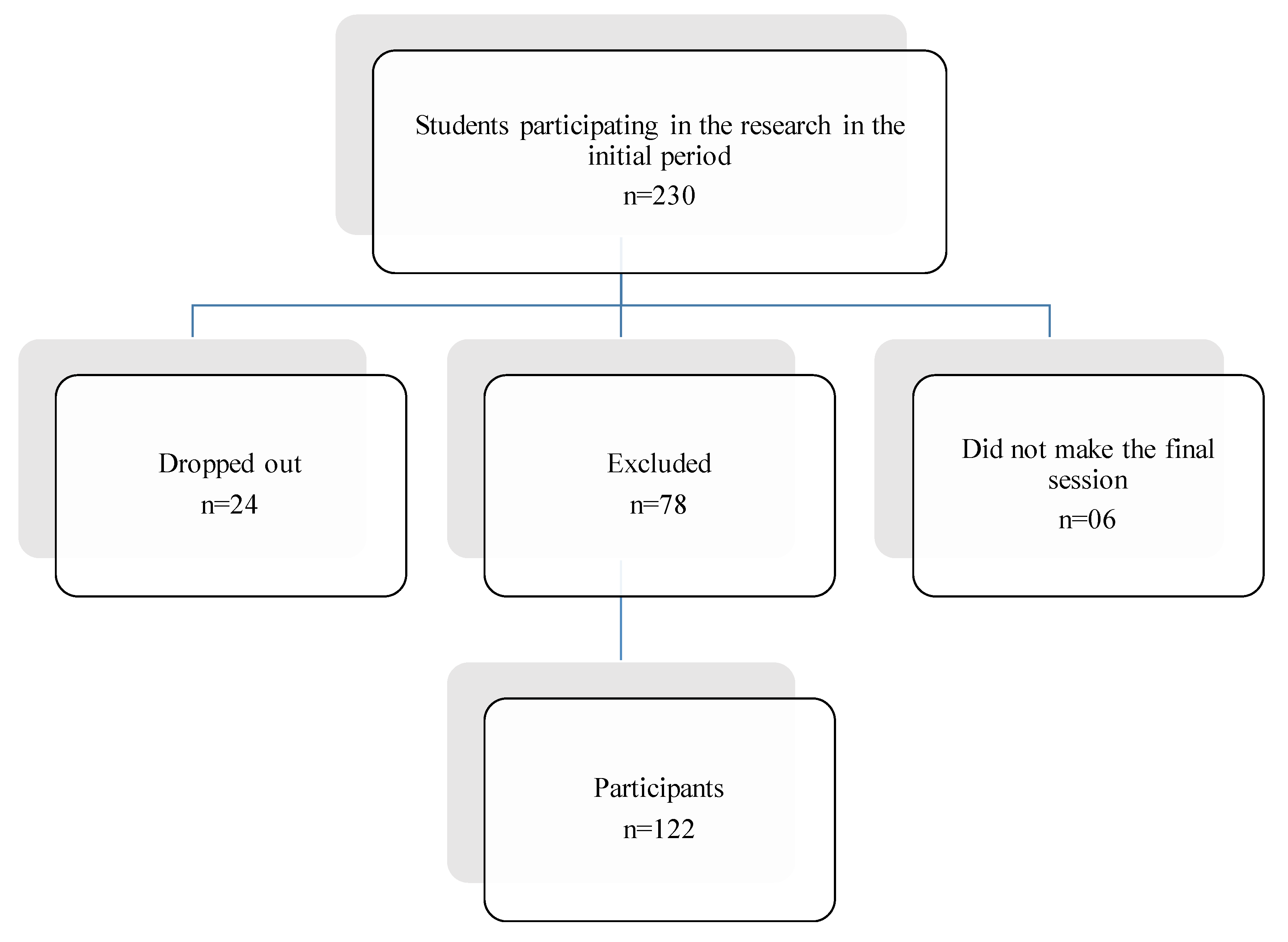
2.2. Participants
2.3. Study Design
- The first stage: the selection of students participating in the study, separation of both groups and obtaining authorization from their parents (signing of the Informed Consent Form) to participate in the research;
- The second stage: anamnesis through a questionnaire containing personal socioeconomic data, blood collection and anthropometric assessment (Table 1). For anthropometric analysis, we used the Pollock protocol and a suitable tape measure for body measurements of 1.5 m [19]. Body weight values were verified using an Omron HBF 514 (0–150 Kg) digital scale, height was assessed by means of a fixed Wiso E210 medical stadiometer (0–210 cm). These results were recorded in the anamnesis form of each participant, in order to serve as a basis for the calculation of the students’ Body Mass Index (BMI). Blood pressure data (SBP and DBP) were also collected by an aneroid sphygmomanometer (Ea1000 black Incoterm, Type: ACMNP-1), together with a stethoscope (Littman Classic II, 28 inches, 2114R). Both measurements were performed pre and post intervention by the same evaluators, in order to avoid any complications in the data collection. Three initial blood pressure (BP) measurements were performed in order to avoid any kind of variations that may interfere with the study, considering for the research records the average between the obtained values. Blood collection (10 mL) was performed by a competent health professional (two nursing technicians), and the student was fasting in the last 12 h prior to the collection. The samples were placed in vacuum blood collection tubes and directed to the Laboclínica Clinic Laboratory (Lagarto, SE), where the biochemical analyses were performed by a competent biochemist from the laboratory. The variables evaluated were Triglycerides (TG) Low-Density Lipoprotein (LDL) and High-Density Lipoprotein (HDL), Total Cholesterol, Non-HDL, Very Low-Density Lipoprotein (VLDL) and Blood Glucose;
- The third stage: the induction of the RTP, which consisted of a set of 10 free exercises (Table 1) that do not exceed the maximum effort limit of each individual, so as not to impair the process of maturation, growth and development of students [12]. The exercises were performed following the order of alternation of body segments (one exercise for lower limbs, another for upper limbs and so on) [18]. The RTP carried out two days a week (Wednesday and Friday) over a period of 12 weeks [18]. The overload variable changed during the research due to the students’ physical development. In this sense, a progressive advancement of external load beyond the body weight of the individuals themselves was performed from the third week. The loads were added based on the responses obtained in the intensity evaluation performed using the Borg scale as an instrument [20], which was based on the intensity of the evaluations whose answers continued to be “Strong”. Therefore, responses with intensities lower than those previously mentioned were considered as indicative of overload. For this purpose, 2 kg, 3 kg, 4 kg and 5 kg dumbbells were used in pairs to perform the proposed exercises;
- The fourth stage: this consisted of a post-intervention evaluation, which verified the effects and morphofunctional changes caused by the training in the students, performing a new data collection as well as previously performed Low Density Lipoprotein (LDL) and High-Density Lipoprotein (ncHDL), Total Cholesterol, Non-HDL, VLDL and Blood Glucose measurements. After the last stage of the research, the collected data will be compared in order to obtain the inferences and possible results found throughout the investigation about such a program and its influences on the reduction in adolescents’ CRFs.
2.4. Statistical Analysis
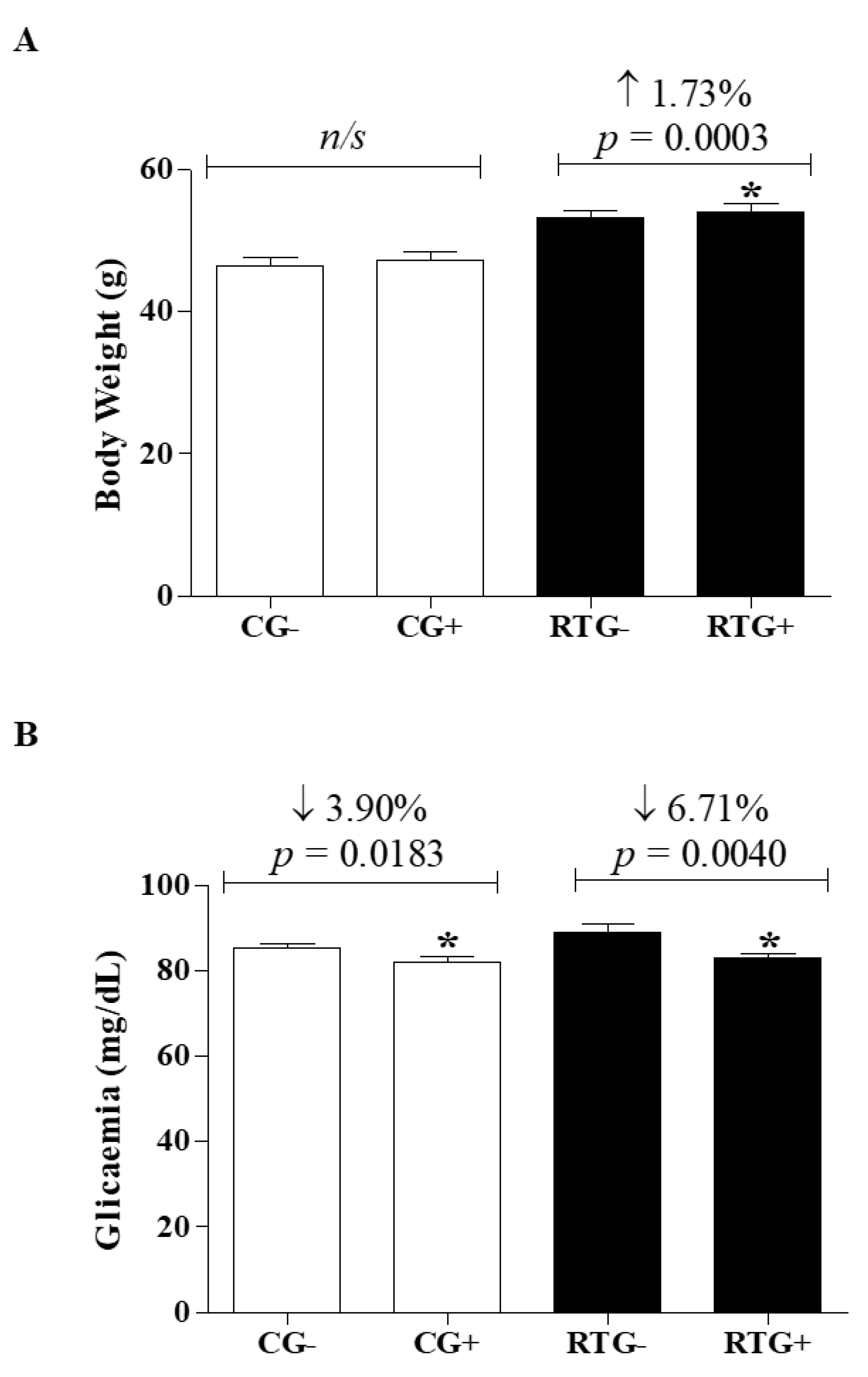
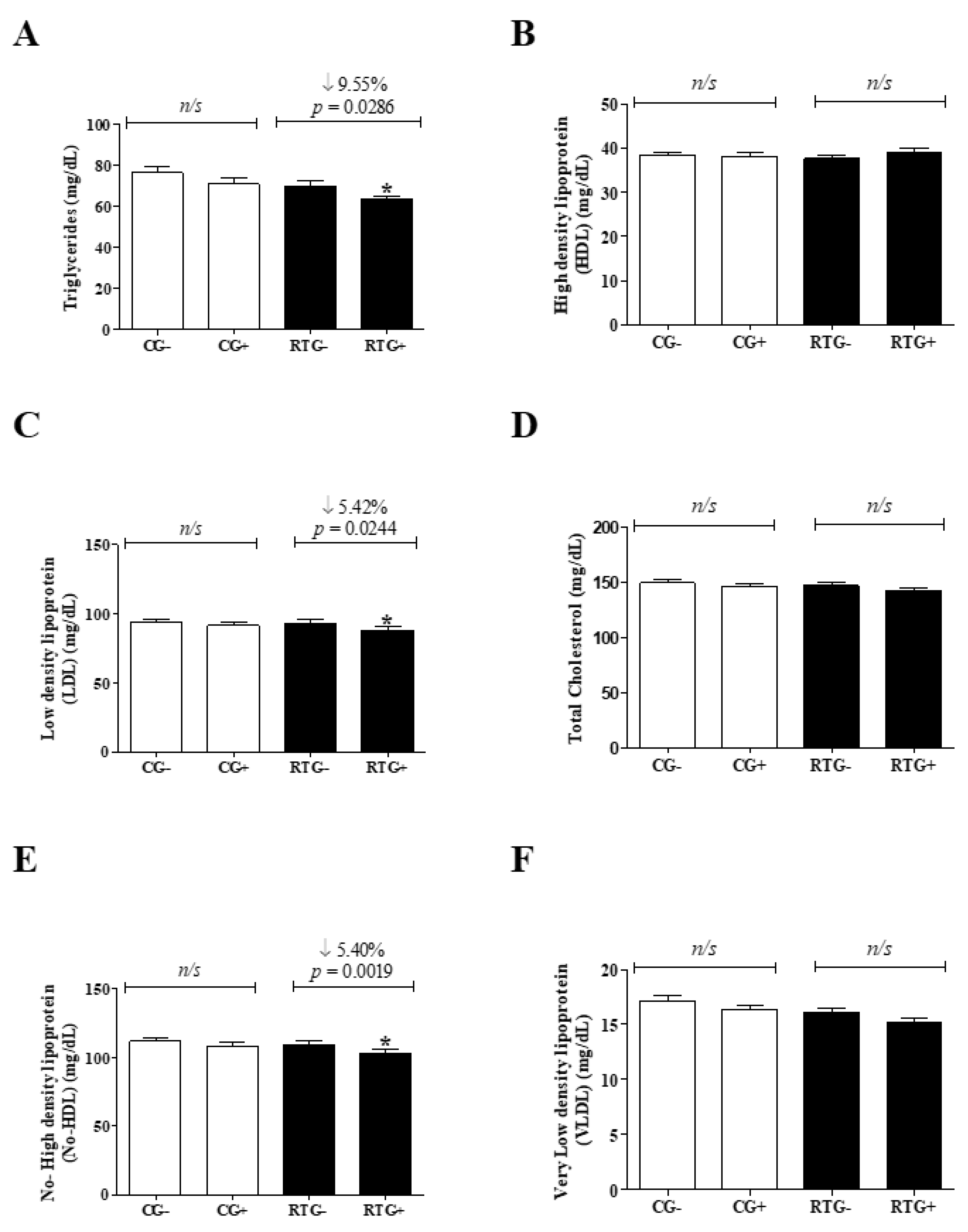
3. Results
4. Discussion
5. Conclusions
6. Patents
Author Contributions
Funding
Acknowledgments
Conflicts of Interest
References
- Biglu, M.H.; Ghavami, M.; Biglu, S. Cardiovascular diseases in the mirror of science. J. Cardiovasc. Thorac. Res. 2016, 8, 158–163. [Google Scholar] [CrossRef] [PubMed]
- Pagidipati, N.J.; Gaziano, T.A. Estimating deaths from cardiovascular disease: A review of global methodologies of mortality measurement. Circulation 2013, 127, 749–756. [Google Scholar] [CrossRef] [PubMed]
- Brant, L.C.C.; Nascimento, B.R.; Passos, V.M.A.; Duncan, B.B.; Bensenõr, I.J.M.; Malta, D.C.; Souza, M.F.M.; Ishitani, L.H.; França, E.; Oliveira, M.S.; et al. Variations and particularities in cardiovascular disease mortality in Brazil and Brazilian states in 1990 and 2015: Estimates from the Global Burden of Disease. Rev. Bras. Epidemiol. 2017, 20, 116–128. [Google Scholar] [CrossRef] [PubMed]
- Angelini, P.; Cheong, B.Y.; Lenge de Rosen, V.V.; Lopez, A.; Uribe, C.; Masso, A.H.; Ali, S.W.; Davis, B.R.; Muthupilai, R.; Willerson, J.T. High-risk cardiovascular conditions in sports-related sudden death: Prevalence in 5169 schoolchildren screened via cardiac magnetic resonance. Tex. Hearth Inst. J. 2018, 45, 205–213. [Google Scholar] [CrossRef] [PubMed]
- Farias Júnior, J.C.; Mendes, J.K.F.; Barbosa, D.B.M.; Lopes, A.S. Fatores de risco cardiovascular em adolescents: Prevalência e associação com fatores sociodemográficos. Rev. Bras. Epidemiol. 2011, 14, 50–62. [Google Scholar] [CrossRef]
- Davel, A.P.; Wenceslau, C.F.; Akamine, E.H.; Xavier, F.E.; Couto, G.K.; Oliveira, H.T.; Rossoni, L.V. Endothelial dysfunction in cardiovascular and endocrine-metabolic diseases: An update. Braz. J. Med. Biol. Res. 2011, 44, 920–932. [Google Scholar] [CrossRef]
- Oliveira, C.M.; Ulbrich, A.Z.; Neves, F.S.; Dias, F.A.L.; Horimoto, A.R.V.R.; Krieger, J.E.; Alvim, R.O.; Pereira, A.D.C. Association between anthropometric indicators of adiposity and hypertension in a Brazilian population: Baependi Heart Study. PLoS ONE 2017, 12, e0185225. [Google Scholar] [CrossRef]
- Skilton, M.R.; Celermajer, D.S.; Cosmi, E.; Crispi, F.; Gidding, S.S.; Raitakari, O.T.; Urbina, E.M. Natural history of atherosclerosis and abdominal aortic intima-media thickness: Rationale, evidence, and best practice for detection of atherosclerosis in the young. J. Clin. Med. 2019, 8, E1201. [Google Scholar] [CrossRef]
- Couto, G.K.; Paula, S.M.; Gomes-Santos, I.L.; Negrão, C.E.; Rossoni, L.V. Exercise training induces eNOS coupling and restores relaxation in coronary arteries of heart failure rats. Am. J. Physiol. Heart Circ. Physiol. 2018, 314, H878–H887. [Google Scholar] [CrossRef]
- Fernandes, T.; Baraúna, V.G.; Negrão, C.E.; Phillips, M.I.; Oliveira, E.M. Aerobic exercise training promotes physiological cardiac remodeling involving a set of microRNAs. Am. J. Physiol. Heart Circ. Physiol. 2015, 309, H543–H552. [Google Scholar] [CrossRef]
- Faigenbaum, A.D.; Kraemer, W.J.; Cahill, B.; Chandler, J.; Dziados, J.; Elfrink, L.D.; Forman, E.; Gaudiose, M.; Micheli, L.; Nitka, M.; et al. Youth resistance training: Position Statement paper and literature review. Strength Cond. J. 2009, 23 (Suppl. 5), S60–S79. [Google Scholar] [CrossRef]
- Damas, F.; Libardi, C.A.; Ugrinowitsch, C.; Vechin, F.C.; Lixandrão, M.E.; Sniiders, T.; Nederveen, J.P.; Bacurau, A.V.; Brum, P.; Tricoli, V.; et al. Early- and later-phases satellite cell responses and myonuclear content with resistance training in young men. PLoS ONE 2018, 13, e0191039. [Google Scholar] [CrossRef] [PubMed]
- Cichocki, M.; Fernandes, K.P.; Castro-Alves, D.C.; Gomes, M.V.M. Atividade física e modulação do risco cardiovascular. Rev. Bras. Med. Esporte 2017, 23, 21–25. [Google Scholar] [CrossRef]
- Tomeleri, C.M.; Ronque, E.R.; Silva, D.R.; Cardoso Júnior, C.G.; Fernandes, R.A.; Teixeira, D.C.; Barbosa, D.S.; Venturini, D.; Okino, A.M.; Oliveira, J.A.; et al. Prevalence of dyslipidemia in adolescents: Comparision between definitions. Rev. Port. Cardiol. 2015, 34, 103–109. [Google Scholar] [CrossRef] [PubMed]
- Arazi, H.; Ghiasi, A.; Asgharpoor, S. A comparative study of cardiovascular responses to two rest intervals between circuit resistance exercises in normotensive woman. Rev. Bras. Med. Esporte 2013, 19, 176–180. [Google Scholar] [CrossRef]
- Sigal, R.J.; Alberga, A.S.; Goldfield, G.S.; Prud’homme, D.; Hadjiyannakis, S.; Gougeon, R.; Phillips, P.; Tulloch, H.; Malcolm, J.; Doucette, S.; et al. Effects of aerobic training, resistance training, or both on percentage body fat and cardiometabolic risk markers in obese adolescents: The healthy eating aerobic and resistance training in youth randomized clinical trial. JAMA Pediatr. 2014, 168, 1006–1014. [Google Scholar] [CrossRef]
- Chulani, V.L.; Gordon, L.P. Adolescent growth and development. Prim. Care 2014, 41, 465–487. [Google Scholar] [CrossRef]
- Lima, F.C.; Costa, S.P.; Minelli, B.; Matos, D.G.; Venturini, G.; Mazini Filho, M.L.; Aidar, F.J. Treinamento resistido na educação física escolar: Uma proposta de Ensino. Cinergis 2014, 15, 207–217. [Google Scholar] [CrossRef]
- Pollock, M.L.; Franklin, B.A.; Balady, G.J.; Chaitman, B.L.; Fleg, J.L.; Fletcher, B.; Limacher, M.; Piña, I.L.; Stein, R.A.; Williams, M.; et al. Resistance exercise in individuals with and without cardiovascular disease. Circulation 2000, 101, 828–833. [Google Scholar] [CrossRef]
- Pinheiro, F.A.; Viana, B.; Pires, F.O. Ratings of perceived exertion as an indicator of the tolerable exercise duration. Motri 2014, 10, 100–106. [Google Scholar] [CrossRef]
- Barbetta, P.A. Estatística Aplicada às Ciências Sociais, 1st ed.; UFSC: Florianópolis, Brazil, 1994. [Google Scholar]
- Fay, D.S.; Gerow, K. A Biologist’s Guide to Statistical Thinking and Analysis, WormBook, ed. The C. elegans Research Community, WormBook. 9 July 2013. Available online: http://www.wormbook.org (accessed on 6 May 2020). [CrossRef]
- Barbosa Filho, V.C.; Quadros, T.M.B.D.; Souza, E.A.D.; Gordia, A.P.; Campos, W.D. A utilização do critério da Organização Mundial de Saúde para classificação do estado nutricional em crianças. Motriz: Revista Educação Física 2010, 16, 811–819. [Google Scholar] [CrossRef]
- De Onis, M.; Onyango, A.W.; Borghi, E.; Siyam, A.; Nishida, C.; Siekmann, J. Development of a WHO growth reference for school-aged children and adolescents. Bull World Health Organ. 2007, 85, 660–667. [Google Scholar] [CrossRef] [PubMed]
- Rodríguez, J.H.; Domínguez, Y.A.; Choqueticlla, J.M. Efectos benéficos del ejercicio físico en las personas con diabetes mellitus tipo 2. Rev. Cubana Endocrinol. 2018, 29, 1–18. [Google Scholar]
- Lee, E.Y.; Yoon, K.H. Epidemic obesity in children and adolescents: Risk factors and prevention. Front. Med. 2018, 12, 658–666. [Google Scholar] [CrossRef]
- Piñeros-Garzón, F.S.; Rodríguez-Hernández, J.M. Factores de riesgo asociados al control glucémico y syndrome metabólico en pacientes con diabetes mellitus tipo 2. Univ. Salud 2018, 21, 61–71. [Google Scholar] [CrossRef]
- Andreis, N.G.; Balbé, G.P. A influência do treinamento de força em indivíduos com síndrome metabólica. Rev. Biomotriz 2018, 12, 137–149. [Google Scholar] [CrossRef]
- Mota, G.R.; Orsatti, F.L.; Delbin, M.A.; Zanesco, A. Resistance exercise improves metabolic parameters and changes adipocyte-derived leptin: A comparison between genders in untrained adults. Motriz: Rev. Educ. Fis. 2016, 22, 217–222. [Google Scholar] [CrossRef][Green Version]
- Silva, D.A.S.; Martins, P.C. Impact of physical growth, body adiposity and lifestyle on muscular strength and cardiorespiratory fitness of adolescents. J. Bodyw. Mov. Ther. 2017, 21, 896–901. [Google Scholar] [CrossRef]
- Kraus, W.E.; Slentz, C.A. Exercise training, lipid regulation, and insulin action: A tangled web of cause and effect. Obesity 2009, 17, S21–S26. [Google Scholar] [CrossRef]
- Albarello, R.A.; Farinha, J.B.; Azambuja, C.R.; Santos, D.L. Efeitos do treinamento resistido sobre o perfil lipídico de indivíduos com síndrome metabólica. Rev. Andal. Med. Deporte 2017, 10, 142–146. [Google Scholar] [CrossRef][Green Version]
- Giordano, P.; Muggeo, P.; Delvecchio, M.; Carbonara, S.; Romano, A.; Altomare, M.; Ricci, G.; Valente, F.; Zito, A.; Scicchitano, P.; et al. Endothelial dysfunction and cardiovascular risk factors in childhood acute lymphoblastic leukemia survivors. Int. J. Cardiol. 2017, 228, 621–627. [Google Scholar] [CrossRef] [PubMed]
- O’donovan, G.; McEneny, J.; Kearney, E.M.; Owen, A.; Nevill, A.M.; Woolf-May, K.; Bird, S.R. LDL particle size in habitual exercisers, lean sedentary men and abdominally obese sedentary men. Int. J. Sports Med. 2007, 28, 644–649. [Google Scholar] [CrossRef] [PubMed]
- Waloszek, J.M.; Woods, M.J.; Byrne, M.L.; Nicholas, C.L.; Bei, B.; Murray, G.; Raniti, M.; Allen, N.B.; Trinder, J. Nocturnal indicators of increased cardiovascular risk in depressed adolescent girls. J. Sleep Resp. 2016, 25, 216–224. [Google Scholar] [CrossRef] [PubMed]
- Kelishadi, R.; Haghdoost, A.A.; Sadeghirad, B.; Khajehkazemi, R. Trend in the prevalence of obesity and overweight among Iranian children and adolescents: A systematic review and meta-analysis. Nutrition 2014, 30, 393–400. [Google Scholar] [CrossRef]
- Tibana, R.A.; Prestes, J.; Nascimento, D.C.; Martins, O.V.; Santana, F.S.; Balsamo, S. Higher muscle performance in adolescents compared with adults after a resistance training session with different rest intervals. J. Strength Cond. Res. 2012, 26, 1027–1032. [Google Scholar] [CrossRef]
- Nascimento, D.D.C.; Silva, C.R.; Valduga, R.; Saraiva, B.; Sousa Neto, I.V.; Vieira, A.; Funghetto, S.S.; Silva, A.O.; Oliveira, S.D.C.; Pereira, G.B.; et al. Blood pressure response to resistance training in hypertensive and normotensive older women. Clin. Interv. Aging 2018, 13, 541–553. [Google Scholar] [CrossRef]
- Cornelissen, V.A.; Fagard, R.H.; Coeckelberghs, E.; Vanhees, L. Impact of resistance training on blood pressure and other cardiovascular risk factors: A meta-analysis of randomized, controlled trials. Hypertension 2011, 58, 950–958. [Google Scholar] [CrossRef]
- Umpierre, D.; Stein, R. Efeitos hemodinâmicos e vasculares do treinamento resistido: Implicações na doença cardiovascular. Arq. Bras. Cardiol. 2007, 89, 256–262. [Google Scholar] [CrossRef]
- Saldanha, M.A.; Vilaça-Alves, J.; Rodrigues Neto, G.; Novaes, J.S.; Saavedra, F.; Reis, V.M.; Rabelo, H.T. Acute effect of resistance exercise performed at different intensities on the hemodynamics of normotensive men. Motricidade 2016, 12, 60–68. [Google Scholar] [CrossRef]
- Lemes, Í.R.; Ferreira, P.H.; Linares, S.N.; Machado, A.F.; Pastre, C.M.; Netto, J.J. Resistance training reduces systolic blood pressure in metabolic syndrome: A systematic review and meta-analysis of randomized controlled trials. Br. J. Sports Med. 2016, 50, 1438–1442. [Google Scholar] [CrossRef]
- Trevizani, G.A.; Seixas, M.B.; Benchimol-Barbosa, P.R.; Vianna, J.M.; Silva, L.P.; Nadal, J. Effect of resistance training on blood pressure and autonomic responses in treated hypertensives. J. Strength Cond. Res. 2018, 32, 1462–1470. [Google Scholar] [CrossRef] [PubMed]

| Exercises | Sets | Repetitions | Overload | Rest |
|---|---|---|---|---|
| Free squat | 3 | 20 | Body weight | 1 min |
| Lunge | 3 | 20 | Body weight | 1 min |
| Standing calf rise | 3 | 20 | Body weight | 1 min |
| Push ups | 3 | 20 | Body weight | 1 min |
| Bench triceps dips | 3 | 15 | Body weight | 1 min |
| TRX pull ups | 3 | 10 | Body weight | 1 min |
| Biceps curl (elastic band) | 3 | 15 | Body weight and band tension | 1 min |
| Upright row (elastic band) | 3 | 20 | Body weight and band tension | 1 min |
| Lateral raise (elastic band) | 3 | 15 | Body weight and band tension | 1 min |
| Plank stabilization | 3 | 30 sec 1 | Body weight | 1 min |
| Variables | CG- | RTG- | p Value |
|---|---|---|---|
| Age (years) | 1300 ± 1.049 | 13.39 ± 0.9709 * | 0.0336 |
| Body weight (grams) | 46.54 ± 8.977 | 53.23 ± 8.271 * | <0.0001 |
| Height (cm) | 158.3 ± 8.358 | 162.0 ± 6.802 * | 0.0080 |
| Body mass index (BMI) (kg/m2) | 18.39 ± 2.765 | 20.30 ± 2.991 * | 0.0004 |
| Glicaemia (mg/dL) | 85.38 ± 0.9389 | 89.00 ± 1.792 | 0.0759 |
| Triglycerides (mg/dL) | 76.38 ± 23.27 | 69.85 ± 19.26 | 0.0943 |
| High density lipoprotein (HDL) (mg/dL) | 38.38 ± 5.352 | 37.64 ± 5.456 | 0.4524 |
| Low density lipoprotein (LDL) (mg/dL) | 93.85 ± 19.33 | 93.07 ± 23.59 | 0.8406 |
| Total Cholesterol (mg/dL) | 149.3 ± 22.50 | 146.9 ± 26.48 | 0.5789 |
| No-High density lipoprotein (No-HDL) (mg/dL) | 111.9 ± 20.83 | 109.2 ± 24.14 | 0.5218 |
| Very Low-density lipoprotein (VLDL) (mg/dL) | 17.15 ± 3.301 | 16.15 ± 2.982 | 0.0817 |
| Systolic blood pressure―SBP (mmHg) | 95.46 ± 15.47 | 103.20 ± 14.31 * | 0.0048 |
| Diastolic blood pressure―DBP (mmHg) | 59.33 ± 8.300 | 59.67 ± 7.600 | 0.8139 |
© 2020 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (http://creativecommons.org/licenses/by/4.0/).
Share and Cite
Rosa Santos, L.d.; Araujo, S.S.d.; Vieira, E.F.d.S.; Estevam, C.d.S.; Santos, J.L.d.; Wichi, R.B.; Lima, F.B.; Carvalho, C.R.O.; Aidar, F.J.; Marçal, A.C. Effects of 12 Weeks of Resistance Training on Cardiovascular Risk Factors in School Adolescents. Medicina 2020, 56, 220. https://doi.org/10.3390/medicina56050220
Rosa Santos Ld, Araujo SSd, Vieira EFdS, Estevam CdS, Santos JLd, Wichi RB, Lima FB, Carvalho CRO, Aidar FJ, Marçal AC. Effects of 12 Weeks of Resistance Training on Cardiovascular Risk Factors in School Adolescents. Medicina. 2020; 56(5):220. https://doi.org/10.3390/medicina56050220
Chicago/Turabian StyleRosa Santos, Lorrany da, Silvan Silva de Araujo, Erlânyo Francisco dos Santos Vieira, Charles dos Santos Estevam, Jymmys Lopes dos Santos, Rogério Brandão Wichi, Fábio Bessa Lima, Carla Roberta Oliveira Carvalho, Felipe José Aidar, and Anderson Carlos Marçal. 2020. "Effects of 12 Weeks of Resistance Training on Cardiovascular Risk Factors in School Adolescents" Medicina 56, no. 5: 220. https://doi.org/10.3390/medicina56050220
APA StyleRosa Santos, L. d., Araujo, S. S. d., Vieira, E. F. d. S., Estevam, C. d. S., Santos, J. L. d., Wichi, R. B., Lima, F. B., Carvalho, C. R. O., Aidar, F. J., & Marçal, A. C. (2020). Effects of 12 Weeks of Resistance Training on Cardiovascular Risk Factors in School Adolescents. Medicina, 56(5), 220. https://doi.org/10.3390/medicina56050220






