Eating Disorders in Pregnant and Breastfeeding Women: A Systematic Review
Abstract
1. Introduction
2. Materials and Methods
2.1. Design
2.2. Eligibility Criteria
2.3. Search Strategy
2.4. Data Collection
2.5. Data Synthesis
2.6. Methodological Quality
3. Results
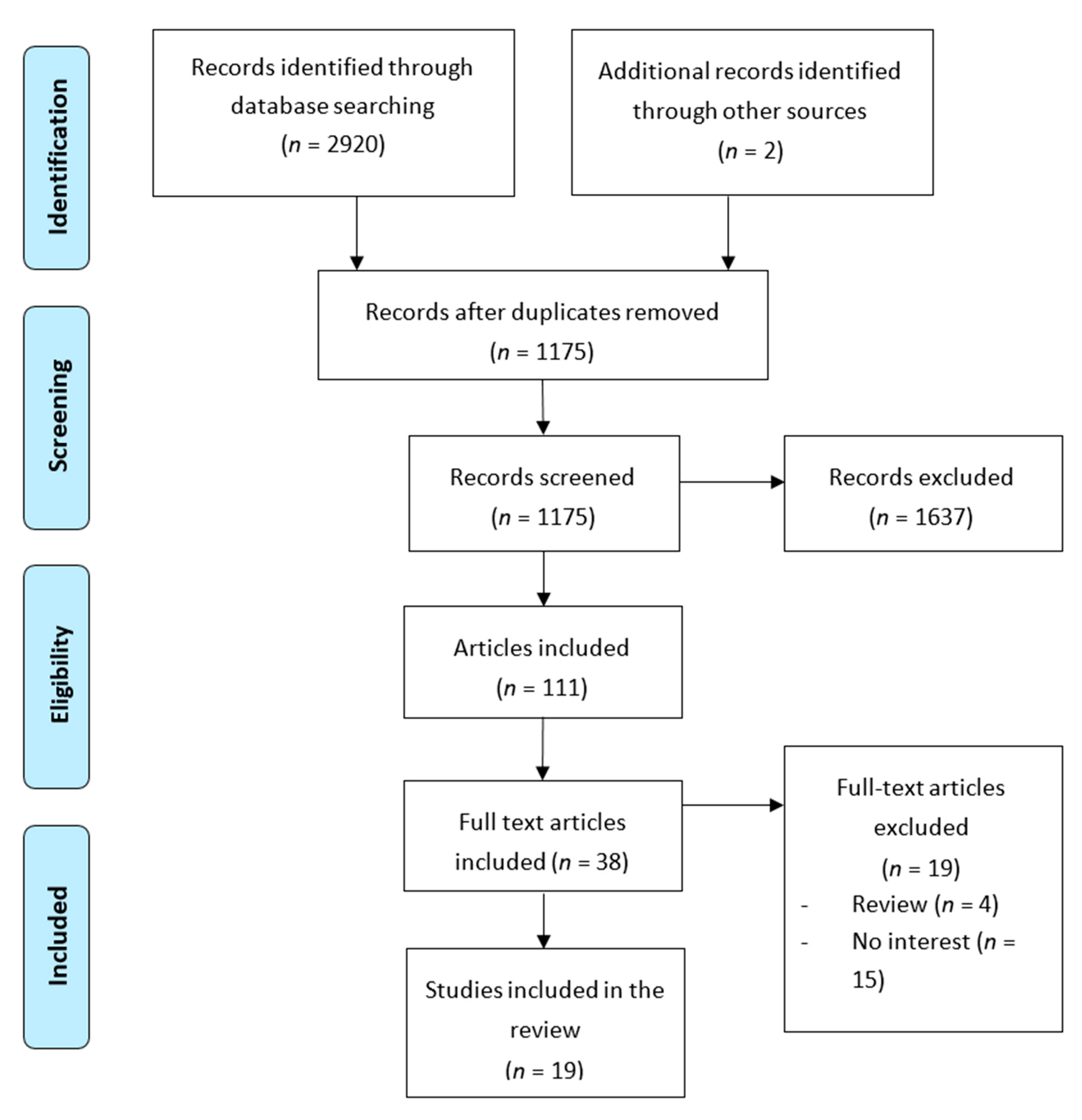
3.1. Study Selection
3.2. Study Description
3.3. Synthesis of Findings
3.3.1. Concern about Weight and Other Symptoms
3.3.2. Effects and Complications of EDs during Pregnancy
3.3.3. Feeding during Pregnancy and Cessation of Breastfeeding
4. Discussion
5. Conclusions
Supplementary Materials
Author Contributions
Funding
Conflicts of Interest
References
- Purizaca, M. Modificaciones fisiológicas en el embarazo. Rev. Peru. Ginecol. Obstet. 2010, 56, 57–69. [Google Scholar]
- Paskulin, J.T.A.; Drehmer, M.; Olinto, M.T.; Hoffmann, J.F.; Pinheiro, A.P.; Schmidt, M.I.; Nunes, M.A. Association between dietary patterns and mental disorders in pregnant women in Southern Brazil. Rev. Bras. Psiquiatr. 2017, 39, 208–215. [Google Scholar] [CrossRef] [PubMed]
- Lewis, A.J.; Austin, E.; Knapp, R.; Vaiano, T.; Galbally, M. Perinatal Maternal Mental Health, Fetal Programming and Child Development. Healthcare 2015, 3, 1212–1227. [Google Scholar] [CrossRef] [PubMed]
- Singh, S.; Sethi, N. Neuroanesthesia and pregnancy: Uncharted waters. Med. J. Armed Forces India 2019, 75, 125–129. [Google Scholar] [CrossRef] [PubMed]
- Vela, B.L.; Alarcón, S.H.; Rodríguez, A.M. Revisión de las herramientas en español para la detección de los trastornos del comportamiento alimentario en adultos. Rev. Esp. Nutr. Comunitaria 2014, 20, 109–117. [Google Scholar]
- Raevuori, A.; Linna, M.S.; Keski-Rahkonen, A. Prenatal and perinatal factors in eating disorders: A descriptive review. Int. J. Eat. Disord. 2014, 47, 676–685. [Google Scholar] [CrossRef]
- Ortega, L.; Lartigue, T.; Figueroa, M.E. Prevalencia de depresión, a través de la Escala de Depresión Perinatal de Edinburgh (EPDS), en una muestra de mujeres mexicanas embarazadas. Perinatología Reproducción Humana 2001, 15, 11–20. [Google Scholar]
- Alder, J.; Fink, N.; Bitzer, J.; Hösli, I.; Holzgreve, W. Depression and Anxiety During Pregnancy: A Risk Factor for Obstetric, Fetal and Neonatal Outcome? A Critical Review of the Literature. J. Matern. Fetal. Neonatal Med. 2007, 20, 189–209. [Google Scholar] [CrossRef]
- Riemann, D. Primary insomnia: A risk factor to develop depression? J. Affect. Disord. 2003, 76, 255–259. [Google Scholar] [CrossRef]
- Wołyńczyk-Gmaj, D.; Różańska-Walędziak, A.; Ziemka, S.; Ufnal, M.; Brzezicka, A.; Gmaj, B.; Januszko, P.; Fudalej, S.; Czajkowski, K.; Wojnar, M. Insomnia in Pregnancy Is Associated with Depressive Symptoms and Eating at Night. J. Clin. Sleep Med. 2017, 13, 1171–1176. [Google Scholar] [CrossRef]
- Kızılırmak, A.; Timur, S.; Kartal, B. Insomnia in Pregnancy and Factors Related to Insomnia. Sci. World J. 2012, 2012, 197093. [Google Scholar] [CrossRef] [PubMed]
- Zerwas, S.C.; Claydon, E.A. Eating Disorders Across the Life-Span: From Menstruation to Menopause. In Women’s Reproductive Mental Health across the Lifespan; Springer International Publishing AG: Cham, Switzerland, 2014; pp. 237–261. [Google Scholar]
- Kudielka, B.M.; Kirschbaum, C. Sex differences in HPA axis responses to stress: A review. Boil. Psychol. 2005, 69, 113–132. [Google Scholar] [CrossRef] [PubMed]
- Easter, A.; Bye, A.; Taborelli, E.; Corfield, F.; Schmidt, U.; Treasure, J.; Micali, N. Recognising the Symptoms: How Common Are Eating Disorders in Pregnancy? Eur. Eat. Disord. Rev. 2013, 21, 340–344. [Google Scholar] [CrossRef] [PubMed]
- Schmidt, U.; Adan, R.; Böhm, I.; Campbell, I.C.; Dingemans, A.; Ehrlich, S.; Elzakkers, I.; Favaro, A.; Giel, K.; Harrison, A.; et al. Eating disorders: The big issue. Lancet Psychiatry 2016, 3, 313–315. [Google Scholar] [CrossRef]
- Martínez-González, L.; Fernández Villa, T.; Molina de la Torre, A.J.; Ayán Pérez, C.; Bueno Cavanillas, A.; Capelo Álvarez, R.; Mateos Campos, R.; Martín Sánchez, V. Prevalencia de trastornos de la conducta alimentaria en universitarios españoles y factores asociados: Proyecto uniHcos. Nutr. Hosp. 2014, 30, 927–934. [Google Scholar]
- Dunker, K.L.; Alvarenga, M.D.; Alves, V.P. Eating disorders and pregnancy—A review [Transtornos alimentares e gestação - Uma revisão]. J. Brasileiro Psiquiatria 2009, 58, 60–68. [Google Scholar] [CrossRef][Green Version]
- Sandín, B. DSM-5 Nueva Clasificación de Los Trastornos Mentales. Revista Psicopatología Psicología Clínica 2013, 18, 255–286. [Google Scholar] [CrossRef]
- Pichot, P.; López-Ibor Aliño, J.J.; Valdés Miyar, M. DSM-IV Manual Diagnóstico Y Estadístico De Los Trastornos Mentales; Masson, S.A.: Barcelona, Spain, 1995. [Google Scholar]
- Johnson, J.L.; Stewart, D.E. DSM-V: Toward a gender sensitive approach to psychiatric diagnosis. Arch. Women’s Ment. Health 2010, 13, 17–19. [Google Scholar] [CrossRef]
- Rosa Behar, A. Fifteen years researching on eating disorders [Quince años de investigación en trastornos de la conducta alimentaria]. Rev. Chil. Neuropsiquiatr. 2010, 48, 135–146. [Google Scholar]
- Li, K.; Wahlqvist, M.L.; Li, K. Nutrition, One-Carbon Metabolism and Neural Tube Defects: A Review. Nutrients 2016, 8, 741. [Google Scholar] [CrossRef]
- Rizzo, G.; Garzon, S.; Fichera, M.; Panella, M.M.; Catena, U.; Schiattarella, A.; de Franciscis, P.; Vilos, G.; Tesarik, J.; Török, P.; et al. Vitamin D and Gestational Diabetes Mellitus: Is There a Link? Antioxidants 2019, 8, 511. [Google Scholar] [CrossRef] [PubMed]
- Dörsam, A.F.; Preißl, H.; Micali, N.; Lörcher, S.B.; Zipfel, S.; Giel, K.E. The Impact of Maternal Eating Disorders on Dietary Intake and Eating Patterns during Pregnancy: A Systematic Review. Nutrients 2019, 11, 840. [Google Scholar] [CrossRef]
- Harrison, M.E.; Obeid, N.; Haslett, K.; McLean, N.; Clarkin, C. Embodied Motherhood: Exploring Body Image in Pregnant and Parenting Youth. J. Pediatr. Adolesc. Gynecol. 2019, 32, 44–50. [Google Scholar] [CrossRef] [PubMed]
- Perestola-Pérez, L. Standards on how to develop and report systematic reviews in Psychology and Health. Int. J. Clin. Health Psychol. 2013, 13, 49–57. [Google Scholar] [CrossRef]
- Moher, D.; Liberati, A.; Tetzlaff, J.; Altman, D.G.; PRISMA Group. Preferred Reporting Items for Systematic Reviews and Meta-Analyses: The PRISMA Statement. PLoS Med. 2009, 6, e1000097. [Google Scholar] [CrossRef] [PubMed]
- Zeng, X.-T.; Zhang, Y.; Kwong, J.S.W.; Zhang, C.; Li, S.; Sun, F.; Niu, Y.; Du, L. The methodological quality assessment tools for preclinical and clinical studies, systematic review and meta-analysis, and clinical practice guideline: A systematic review. J. Evid.-Based Med. 2015, 8, 2–10. [Google Scholar] [CrossRef]
- Bulik, C.M.; Torgersen, L.; Reichborn-Kjennerud, T.; Gendall, K.; Holle, A.V.; James, W.H. Maternal eating disorders and offspring sex ratios at birth. Acta Obstet. Gynecol. Scand. 2009, 88, 489. [Google Scholar] [CrossRef]
- Torgersen, L.; Ystrom, E.; Haugen, M.; Meltzer, H.M.; Von Holle, A.; Berg, C.K.; Reichborn-Kjennerud, T.; Bulik, C. Breastfeeding practice in mothers with eating disorders. Matern. Child Nutr. 2009, 6, 243–252. [Google Scholar] [CrossRef]
- Siega-Riz, A.M.; Von Holle, A.; Haugen, M.; Meltzer, H.M.; Hamer, R.; Torgersen, L.; Berg, C.K.; Reichborn-Kjennerud, T.; Bulik, C.M. Gestational weight gain of women with eating disorders in the Norwegian pregnancy cohort. Int. J. Eat. Disord. 2010, 44, 428–434. [Google Scholar] [CrossRef]
- Knoph, C.; Von Holle, A.; Zerwas, S.; Torgersen, L.; Tambs, K.; Stoltenberg, C.; Bulik, C.M.; Reichborn-Kjennerud, T. Course and predictors of maternal eating disorders in the postpartum period. Int. J. Eat. Disord. 2013, 46, 355–368. [Google Scholar] [CrossRef]
- Watson, H.J.; Zerwas, S.; Torgersen, L.; Gustavson, K.; Diemer, E.W.; Knudsen, G.P.; Reichborn-Kjennerud, T.; Bulik, C.M. Maternal eating disorders and perinatal outcomes: A three-generation study in the Norwegian Mother and Child Cohort Study. J. Abnorm. Psychol. 2017, 126, 552–564. [Google Scholar] [CrossRef] [PubMed]
- Swann, R.A.; Von Holle, A.; Torgersen, L.; Gendall, K.; Reichborn-Kjennerud, T.; Bulik, C.M. Attitudes toward weight gain during pregnancy: Results from the Norwegian mother and child cohort study (MoBa). Int. J. Eat. Disord. 2009, 42, 394–401. [Google Scholar] [CrossRef] [PubMed]
- Easter, A.; Treasure, J.; Micali, N. Fertility and prenatal attitudes towards pregnancy in women with eating disorders: Results from the Avon Longitudinal Study of Parents and Children. BJOG: Int. J. Obstet. Gynaecol. 2011, 118, 1491–1498. [Google Scholar] [CrossRef] [PubMed]
- Micali, N.; De Stavola, B.; Dos-Santos-Silva, I.; Graaff, J.S.-D.; Jansen, P.; Jaddoe, V.; Hofman, A.; Verhulst, F.; Steegers, E.; Tiemeier, H. Perinatal outcomes and gestational weight gain in women with eating disorders: A population-based cohort study. BJOG Int. J. Obstet. Gynaecol. 2012, 119, 1493–1502. [Google Scholar] [CrossRef] [PubMed]
- Soares, R.M.; Nunes, M.A.; Schmidt, M.I.; Giacomello, A.; Manzolli, P.; Camey, S.; Buss, C.; Drehmer, M.; Melere, C.; Hoffman, J.; et al. Inappropriate eating behaviors during pregnancy: Prevalence and associated factors among pregnant women attending primary care in southern Brazil. Int. J. Eat. Disord. 2009, 42, 387–393. [Google Scholar] [CrossRef] [PubMed]
- Nunes, M.A.A.; Pinheiro, A.P.; Camey, S.A.; Schmidt, M.I.; Antunes Nunes, M.A.; Pinheiro, A.P.; Camey, S.A.; Schmidt, M.I. Binge eating during pregnancy and birth outcomes: A cohort study in a disadvantaged population in Brazil. Int. J. Eat. Disord. 2012, 45, 827–831. [Google Scholar] [CrossRef]
- Angélica Nunes, M.; Poyastro Pinheiro, A.; Feliciati Hoffmann, J.; Inês Schmidt, M.; Nunes, M.A.; Pinheiro, A.P.; Hoffmann, J.F.; Schmidt, M.I. Eating disorders symptoms in pregnancy and postpartum: A prospective study in a disadvantaged population in Brazil. Int. J. Eat. Disord. 2014, 47, 426–430. [Google Scholar] [CrossRef]
- Easter, A.; Taborelli, E.; Bye, A.; Zunszain, P.; Pariante, C.; Treasure, J.; Schmidt, U.; Micali, N. Perinatal hypothalamic-pituitary-adrenal axis regulation among women with eating disorders and their infants. Psychoneuroendocrinology 2017, 76, 127–134. [Google Scholar] [CrossRef]
- Martini, M.G.; Taborelli, E.; Schmidt, U.; Treasure, J.; Micali, N. Infant feeding behaviours and attitudes to feeding amongst mothers with eating disorders: A longitudinal study. Eur. Eat. Disord. Rev. 2018, 27, 137–146. [Google Scholar] [CrossRef]
- Nguyen, A.N.; De Barse, L.M.; Tiemeier, H.; Jaddoe, V.W.; Franco, O.H.; Jansen, P.W.; Voortman, T. Maternal history of eating disorders: Diet quality during pregnancy and infant feeding. Appetite 2017, 109, 108–114. [Google Scholar] [CrossRef]
- Pettersson, C.B.; Zandian, M.; Clinton, D. Eating disorder symptoms pre- and postpartum. Arch. Women’s Ment. Health 2016, 19, 675–680. [Google Scholar] [CrossRef] [PubMed]
- Nunes, M.A.; Ferri, C.P.; Manzolli, P.; Soares, R.M.; Drehmer, M.; Buss, C.; Giacomello, A.; Hoffmann, J.F.; Ozcariz, S.; Melere, C.; et al. Nutrition, mental health and violence: From pregnancy to postpartum Cohort of women attending primary care units in Southern Brazil-ECCAGE study. BMC Psychiatry 2010, 10, 66. [Google Scholar] [CrossRef] [PubMed]
- Buss, C.; Nunes, M.A.; Camey, S.; Manzolli, P.; Soares, R.M.; Drehmer, M.; Giacomello, A.; Duncan, B.B.; Schmidt, M.I. Dietary fibre intake of pregnant women attending general practices in southern Brazil—The ECCAGE Study. Public Health Nutr. 2009, 12, 1392–1398. [Google Scholar] [CrossRef] [PubMed][Green Version]
- Hoffmann, J.F.; Nunes, M.A.A.; Schmidt, M.I.; Olinto, M.T.A.; Melere, C.; Ozcariz, S.G.I.; Buss, C.; Drhemer, M.; Manzolli, P.; Soares, R.M.; et al. Dietary patterns during pregnancy and the association with sociodemographic characteristics among women attending general practices in southern Brazil: The ECCAGe Study. Cad. Saude Publica 2013, 29, 970–980. [Google Scholar] [CrossRef] [PubMed]
- Fairburn, C.G.; Beglin, S.J. Assessment of eating disorders: Interview or self-report questionnaire? Int. J. Eat. Disord. 1994, 16, 363–370. [Google Scholar] [PubMed]
- Sichieri, R.; Everhart, J.E. Validity of a Brazilian food frequency questionnaire against dietary recalls and estimated energy intake. Nutr. Res. 1998, 18, 1649–1659. [Google Scholar] [CrossRef]
- Bulik, C.M.; von Holle, A.; Siega-Riz, A.M.; Torgersen, L.; Lie, K.K.; Hamer, R.M.; Ma, C.K.B.; Sullivan, P.; Reichborn-Kjennerud, T. Birth outcomes in women with eating disorders in the Norwegian Mother and Child cohort study (MoBa). Int. J. Eat. Disord. 2009, 42, 9–18. [Google Scholar] [CrossRef]
- Magnus, P.; Irgens, L.M.; Haug, K.; Nystad, W.; Skjærven, R.; Stoltenberg, C. Cohort profile: The Norwegian Mother and Child Cohort Study (MoBa). Int. J. Epidemiol. 2006, 35, 1146–1150. [Google Scholar] [CrossRef]
- Magnus, P. The Norwegian Mother and Child Cohort Study (MoBa)—New research possibilities. Norsk Epidemiol. 2007, 17, 107–110. [Google Scholar] [CrossRef][Green Version]
- Golding, J.; Pembrey, M.; Jones, R.; Study, A. Study methodology ALSPAC±The Avon Longitudinal Study of Parents and Children I. Study methodology The study structure Historical background. Paediatr. Perinat. Epidemiol. 2001, 15, 74–87. [Google Scholar] [CrossRef]
- Drehmer, M.; Camey, S.; Schmidt, M.I.; Olinto, M.T.A.; Giacomello, A.; Buss, C.; Melere, C.; Hoffmann, J.; Manzolli, P.; Soares, R.M.; et al. Socioeconomic, demographic and nutritional factors associated with maternal weight gain in general practices in Southern Brazil. Cadernos Saúde Pública 2010, 26, 1024–1034. [Google Scholar] [CrossRef][Green Version]
- Klipstein-Grobusch, K.; Breeijen, J.H.D.; A Goldbohm, R.; Geleijnse, J.M.; Hofman, A.; Grobbee, D.E.; Witteman, J. Dietary assessment in the elderly: Validation of a semiquantitative food frequency questionnaire. Eur. J. Clin. Nutr. 1998, 52, 588–596. [Google Scholar] [CrossRef]
- Zerwas, S.; Von Holle, A.; Torgersen, L.; Reichborn-Kjennerud, T.; Stoltenberg, C.; Bulik, C.M. Maternal eating disorders and infant temperament: Findings from the norwegian mother and child cohort study. Int. J. Eat. Disord. 2012, 45, 546–555. [Google Scholar] [CrossRef] [PubMed]
- Stice, E.; Fisher, M.; Martinez, E. Eating Disorder Diagnostic Scale: Additional Evidence of Reliability and Validity. Psychol. Assess. 2004, 16, 60–71. [Google Scholar] [CrossRef] [PubMed]
- Zerwas, S.; Von Holle, A.; Perrin, E.M.; Skinner, A.C.; Reba-Harrelson, L.; Hamer, R.M.; Stoltenberg, C.; Torgersen, L.; Reichborn-Kjennerud, T.; Bulik, C.M. Gestational and postpartum weight change patterns in mothers with eating disorders. Eur. Eat. Disord. Rev. 2014, 22, 397–404. [Google Scholar] [CrossRef] [PubMed]
- Easter, A.; Naumann, U.; Northstone, K.; Schmidt, U.; Treasure, J.; Micali, N. A Longitudinal Investigation of Nutrition and Dietary Patterns in Children of Mothers with Eating Disorders. J. Pediatr. 2013, 163, 173–178.e1. [Google Scholar] [CrossRef] [PubMed]
- Glasofer, D.R.; Brown, A.J.; Riegel, M. Structured Clinical Interview for DSM-IV (SCID). In Encyclopedia of Feeding and Eating Disorders; Springer Science and Business Media LLC: Singapore, Singapore, 2015; pp. 1–4. [Google Scholar]
- State-Trait Anxiety Inventory for Adults Sampler Set Manual, Instrument and Scoring Guide Permission for Ashley Pasen to Reproduce 1 Copy within One Year of; Consulting Psychologists Press: Palo Alto, CA, USA, 2010.
- Beck, A.T.; Ward, C.H.; Mendelson, M.; Mock, J.; Erbaugh, J. An Inventory for Measuring Depression. Arch. Gen. Psychiatry 1961, 4, 561–571. [Google Scholar] [CrossRef] [PubMed]
- Cohen, S. Perceived Stress Scale; Mind Garden, Inc.: Menlo Park, CA, USA, 1994. [Google Scholar]
- Huizink, A.C.; Delforterie, M.J.; Scheinin, N.M.; Tolvanen, M.; Karlsson, L.; Karlsson, H. Adaption of pregnancy anxiety questionnaire–revised for all pregnant women regardless of parity: PRAQ-R. Arch. Women’s Ment. Health 2015, 19, 125–132. [Google Scholar] [CrossRef]
- Jaddoe, V.W.V.; Van Duijn, C.M.; Franco, O.H.; Van Der Heijden, A.J.; Van Iizendoorn, M.H.; De Jongste, J.C.; Van Der Lugt, A.; MacKenbach, J.P.; Moll, H.A.; Raat, H.; et al. The Generation R Study: Design and cohort update. Eur. J. Epidemiol. 2012, 27, 739–756. [Google Scholar] [CrossRef]
- Chan, C.Y.; Lee, A.M.; Koh, Y.W.; Lam, S.K.; Lee, C.P.; Leung, K.Y.; Tang, C.S.K. Course, risk factors, and adverse outcomes of disordered eating in pregnancy. Int. J. Eat. Disord. 2019, 52, 652–658. [Google Scholar] [CrossRef]
- Garner, D.M.; Olmsted, M.P.; Bohr, Y.; Garfinkel, P.E. The Eating Attitudes Test: Psychometric features and clinical correlates. Psychol. Med. 1982, 12, 871–878. [Google Scholar] [CrossRef] [PubMed]
- Leung, C.M.; Ho, S.; Kan, C.S.; Hung, C.H.; Chen, C.N. Evaluation of the Chinese version of the Hospital Anxiety and Depression Scale. A cross-cultural perspective. Int. J. Psychosom. Off. Publ. Int. Psychosom. Inst. 1993, 40, 29–34. [Google Scholar]
- Cox, J.L.; Holden, J.M.; Sagovsky, R. Detection of postnatal depression: Development of the 10-item Edinburgh Postnatal Depression Scale. Br. J. Psychiatry 1987, 150, 782–786. [Google Scholar] [CrossRef] [PubMed]
- McLeland, K.C.; Sutton, G.W.; Schumm, W.R. Marital Satisfaction before and after Deployments Associated with the Global War on Terror. Psychol. Rep. 2008, 103, 836–844. [Google Scholar] [CrossRef]
- Baughcum, A.E.; Powers, S.W.; Johnson, S.B.; Chamberlin, L.A.; Deeks, C.M.; Jain, A.; Whitaker, R.C. Maternal Feeding Practices and Beliefs and Their Relationships to Overweight in Early Childhood. J. Dev. Behav. Pediatr. 2001, 22, 391–408. [Google Scholar] [CrossRef]
- Watson, H.J.; Diemer, E.W.; Zerwas, S.; Gustavson, K.; Knudsen, G.P.; Torgersen, L.; Reichborn-Kjennerud, T.; Bulik, C.M. Prenatal and perinatal risk factors for eating disorders in women: A population cohort study. Int. J. Eat. Disord. 2019, 52, 643–651. [Google Scholar] [CrossRef]
- Mouanoutoua, V.L.; Brown, L.G. Hopkins Symptom Checklist-25, Hmong Version: A Screening Instrument for Psychological Distress. J.Pers. Assess. 1995, 64, 376–383. [Google Scholar] [CrossRef]
- Behar, R.; González, J.; Ariza, M.; Aguirre, A. Trastornos de la conducta alimentaria en mujeres embarazadas controladas en atención primaria. Rev. Chil. Obstet. Ginecol. 2008, 73, 155–162. [Google Scholar] [CrossRef]
- Berger, K.E.; Masterson, J.; Mascardo, J.; Grapa, J.; Appanaitis, I.; Temengil, E.; Watson, B.M.; Cash, H.L. The Effects of Chewing Betel Nut with Tobacco and Pre-pregnancy Obesity on Adverse Birth Outcomes Among Palauan Women. Matern. Child Health J. 2016, 20, 1696–1703. [Google Scholar] [CrossRef]
- Linna, M.S.; Raevuori, A.; Haukka, J.; Suvisaari, J.; Suokas, J.T.; Gissler, M. Pregnancy, obstetric, and perinatal health outcomes in eating disorders. Am. J. Obstet. Gynecol. 2014, 211, 392.e1–392.e8. [Google Scholar] [CrossRef]
- Watson, H.J.; von Holle, A.; Hamer, R.M.; Knoph Berg, C.; Torgersen, L.; Magnus, P.; Stoltenberg, C.; Sullivan, P.; Reichborn-Kjennerud, T.; Bulik, C.M. Remission, continuation and incidence of eating disorders during early pregnancy: A validation study in a population-based birth cohort. Psychol. Med. 2013, 43, 1723–1734. [Google Scholar] [CrossRef] [PubMed]
- Watson, H.J.; von Holle, A.; Knoph, C.; Hamer, R.M.; Torgersen, L.; Reichborn-Kjennerud, T.; Stoltenberg, C.; Magnus, P.; Bulik, C.M. Psychosocial factors associated with bulimia nervosa during pregnancy: An internal validation study. Int. J. Eat. Disord. 2014, 48, 654–662. [Google Scholar] [CrossRef] [PubMed]
- Eik-Nes, T.; Horn, J.; Strohmaier, S.; Holmen, T.L.; Micali, N.; Bjørnelv, S. Impact of eating disorders on obstetric outcomes in a large clinical sample: A comparison with the HUNT study. Int. J. Eat. Disord. 2018, 51, 1134–1143. [Google Scholar] [CrossRef] [PubMed]
- Rogers, S.L.; Blissett, J.; Blissett, J. Breastfeeding duration and its relation to weight gain, eating behaviours and positive maternal feeding practices in infancy. Appetite 2017, 108, 399–406. [Google Scholar] [CrossRef] [PubMed]
- Larsson, G.; Andersson-Ellström, A. Experiences of pregnancy-related body shape changes and of breast-feeding in women with a history of eating disorders. Eur. Eat. Disord. Rev. 2003, 11, 116–124. [Google Scholar] [CrossRef]
- Micali, N.; Simonoff, E.; Treasure, J. Infant Feeding and Weight in the First Year of Life in Babies of Women with Eating Disorders. J. Pediatr. 2009, 154, 55–60.e1. [Google Scholar] [CrossRef]
- Bakker, R.; Steegers, E.A.; Obradov, A.; Raat, H.; Hofman, A.; Jaddoe, V.W. Maternal caffeine intake from coffee and tea, fetal growth, and the risks of adverse birth outcomes: The Generation R Study. Am. J. Clin. Nutr. 2010, 91, 1691–1698. [Google Scholar] [CrossRef] [PubMed]
- Abraham, S.; Abraham, S.F.; Hart, S.; Luscombe, G.; Russell, J. Fluid Intake, Personality and Behaviour in Patients with Eating Disorders. Eat Weight Disord. 2006, 11, 30–34. [Google Scholar] [CrossRef] [PubMed]
- Reba-Harrelson, L.; Von Holle, A.; Hamer, R.M.; Torgersen, L.; Reichborn-Kjennerud, T.; Bulik, C.M.; Reba-Harreleson, L. Patterns of maternal feeding and child eating associated with eating disorders in the Norwegian Mother and Child Cohort Study (MoBa). Eat. Behav. 2010, 11, 54–61. [Google Scholar] [CrossRef]
- Pasternak, Y.; Weintraub, A.Y.; Shoham-Vardi, I.; Sergienko, R.; Guez, J.; Wiznitzer, A.; Shalev, H.; Sheiner, E. Obstetric and Perinatal Outcomes in Women with Eating Disorders. J. Women’s Health 2012, 21, 61–65. [Google Scholar] [CrossRef] [PubMed]
- Baskin, R.; Hill, B.; Jacka, F.N.; O’Neil, A.; Skouteris, H. The association between diet quality and mental health during the perinatal period. A systematic review. Appetite 2015, 91, 41–47. [Google Scholar] [CrossRef] [PubMed]
- Astrachan-Fletcher, E.; Veldhuis, C.B.; Lively, N.; Fowler, C.; Marcks, B. The Reciprocal Effects of Eating Disorders and the Postpartum Period: A Review of the Literature and Recommendations for Clinical Care. J. Women’s Health 2008, 17, 227–239. [Google Scholar] [CrossRef] [PubMed]
- Assessment of Caffeine Consumption, Altered Caffeine Metabolism and Pregnancy Outcome|Food Standards Agency. Available online: https://www.food.gov.uk/research/national-diet-and-nutrition-survey/assessment-of-caffeine-consumption-altered-caffeine-metabolism-and-pregnancy-outcome (accessed on 13 May 2019).
- Triunfo, S.; Lanzone, A. Impact of maternal under nutrition on obstetric outcomes. J. Endocrinol. Investig. 2014, 38, 31–38. [Google Scholar] [CrossRef] [PubMed]
- Torgersen, L.; von Holle, A.; Reichborn-Kjennerud, T.; Ma, C.K.B.; Hamer, R.; Sullivan, P.; Bulik, C.M. Nausea and vomiting of pregnancy in women with bulimia nervosa and eating disorders not otherwise specified. Int. J. Eat. Disord. 2008, 41, 722–727. [Google Scholar] [CrossRef]
- Hartge, P. Participation in Population Studies. Epidemiology 2006, 17, 252–254. [Google Scholar] [CrossRef]
- Onyango, A.W.; Nommsen-Rivers, L.; Siyam, A.; Borghi, E.; De Onis, M.; Garza, C.; Lartey, A.; Baerug, A.; Bhandari, N.; Dewey, K.G.; et al. Post-partum weight change patterns in the WHO Multicentre Growth Reference Study. Matern. Child Nutr. 2011, 7, 228–240. [Google Scholar] [CrossRef]
- Meyer, C.; McPartlan, L.; Sines, J.; Waller, G. Accuracy of self-reported weight and height: Relationship with eating psychopathology among young women. Int. J. Eat. Disord. 2009, 42, 379–381. [Google Scholar] [CrossRef]
| Lead Author, Year | Type of Study | Population Study | Measurement Tools | Results |
|---|---|---|---|---|
| Rafael Marques Soares, 2009 [37] | Prospective cohort study of pregnant mothers | Pregnant women who participated in the ECCAGE (The Study of Food Intake and Eating Behaviors in Pregnancy-) [44,45,46] | EDE-Q [47] FFQ [48] | The prevalence of BED in pregnant women is 17.3% (IC 14.5–20). It is higher in those who present anxiety symptoms, depressive symptoms. Inappropriate eating behaviors before pregnancy persisted during pregnancy. A low pre-gestational BMI (<19.8 kg/m2) is significantly associated with binge eating during pregnancy. The most common symptoms of EDs during pregnancy are binge eating and weight concerns. |
| Cynthia M Bulik, 2009 [49] | Prospective cohort study of pregnant mothers | Pregnant women who participated in the Norwegian Mother and Child Cohort Study (MoBa) [50] | Blood tests Urine analysis MBRN—MoBa MoBa Questionnaire 1 [51] MoBa Questionnaire 4 [51] | Out of 35.929 mothers; 35 reported AN (0.09%), 306 BN (0.85%), 1812 BED (5.04%), and 36 EDNOS (0.1%). In all groups of EDs, the smoking rate is high. Mothers with ED except EDNOS have greater weight gain during pregnancy than healthy mothers. Those with BN or BED, this increase may be related to eating behaviors. Those with AN, gaining adequate weight during pregnancy may mitigate the adverse effects. |
| Rebecca A. Swann, 2009 [34] | Prospective cohort study of pregnant mothers | Pregnant women who participated in the Norwegian Mother and Child Cohort Study (MoBa) [50] | Blood tests Urine analysis MBRN—MoBa MoBa Questionnaire 1 [51] MoBa Questionnaire 3 [51] MoBa Questionnaire 4 [51] | Out of 35.929 pregnant mothers; 35 AN (0.09%), 304 BN (0.85%), 36 EDNOS (0.1%), 1812 (5.04%) BED, and 33,742 (93.9%) healthy. The presence of EDs is associated with a concern about weight gain during pregnancy. The increase is greater in those who are concerned about gain than those who are not. |
| Leila Torgersen, 2010 [30] | Prospective cohort study of pregnant mothers | Pregnant women who participated in the Norwegian Mother and Child Cohort Study (MoBa) [50] | MBRN—MoBa MoBa Questionnaire 1 [51] MoBa Questionnaire 4 [51] | Of the mothers who started giving BM, 98% did so predominantly, with no difference between mothers with EDs-healthy mothers. At six months, 83% of the mothers were still breastfeeding, but only 15% were predominantly feeding. The risk of abandonment is higher in mothers with AN and EDNOS. There are no significant differences between the early abandonment of mothers with EDs and healthy mothers. |
| Anna Maria Siega-Riz PhD, RD, 2011 [31] | Cross-sectional cohort study | Pregnant women who participated in the Norwegian Mother and Child Cohort Study (MoBa) [50] | MBRN—MoBa MoBa Questionnaire 1 [51] MoBa Questionnaire 3 [51] MoBa Questionnaire 4 [51] | The average weight gain of the population was: 2.5 kg at 17–20.1 weeks, 9.3 kg at 27.4–29.7, and 15 kg at delivery. Women with BN and BED gained significantly more weight on average. |
| A Easter, 2011 [35] | Prospective longitudinal study of a birth cohort | Pregnant women who participated in the Avon Longitudinal Study of Parents and Children (ALSPAC) [52] | Socio-demographic, fertility, reaction to pregnancy questionnaires [53] | Women with AN and AN + BN smoke more during pregnancy than healthy women. Women with AN have a higher percentage of unwanted pregnancies, 41.5% vs. 28.3% of the general population. Mothers with AN tend to have negative feelings about pregnancy, usually related to weight gain. |
| Nadia Micali, 2012 [36] | Prospective longitudinal study of a birth cohort | Pregnant women who have participated in the Avon Longitudinal Study of Parents and Children (ALSPAC) [52] | Sociodemographic and anthropometric questionnaires [53] FFQ [54] | Mothers with ED consume less butter and whole milk and more legumes and soy drink compared to healthy mothers. They have a lower intake of sugars and saturated fats. Fat–protein–carbohydrate intake is the same as in unexposed mothers. They are more likely to consume >2500 mg caffeine/week. Although it is observed that the intake is adequate in terms of quality, it is not known if it is adequate in terms of quantity. |
| Stephanie Zerwas, 2012 [55] | Prospective cohort study of pregnant mothers | Pregnant women who participated in the Norwegian Mother and Child Cohort Study (MoBa) [50] | MBRN—MoBa MoBa Questionnaire 1 [51] MoBa Questionnaire 4 [51] | Mothers with AN, BN, EDNOS, and BED gained weight more quickly during pregnancy and lost weight more quickly over the first six months postpartum than mothers without EDs. |
| Maria Angelica Nunes, 2012 [38] | Prospective cohort study of pregnant mothers | Pregnant women who have participated in ECCAGE (The Study of Food Intake and Eating Behaviors in Pregnancy) [44,45,46] | ECCAGE Specific Questionnaire EDE-Q [47] | 17.1% (n = 119) have binges during pregnancy. The weight gain is significantly higher in mothers who have BED (15.2 kg) than in healthy mothers (13.6 kg). It seems that it is due to the increase in these behaviors and therefore an excess in food intake. |
| Knoph C, 2013 [32] | Prospective cohort study of pregnant mothers | Pregnant women who participated in the Norwegian Mother and Child Cohort Study [50] | MBRN—MoBa MoBa Questionnaire 1 [51] MoBa Questionnaire 4 [51] MoBa Questionnaire 5 [51] MoBa Questionnaire 6 [51] Hopkins Symptom Checklist-25 | For the BN, 40% and 30% remitted at 18 and 36 months, respectively. For BED; 45% and 42%. It is associated with dietary patterns of increased sugar and fat intake and weight gain. |
| Abigail Easter, 2013 [14] | Prospective cohort study | Pregnant women at King’s College Hospital, London | EDDS [56] | The prevalence of EDs during pregnancy is: 0.5% AN, 0.1% BN, and 1.8% BED, 0.1% used purging and 5% EDNOS. Binge eating behaviors were followed by 8.8% and 2.3% adopted compensatory behaviors regularly. 23.4% reported high weight and shape concerns. |
| Stephanie C. Zerwas, 2014 [57] | Prospective cohort study | Pregnant women who participated in the Norwegian Mother and Child Cohort Study [50] | MBRN—MoBa MoBa Questionnaire 1 [51] MoBa Questionnaire 3 [51] MoBa Questionnaire 4 [51] MoBa Questionnaire 5 [51] MoBa Questionnaire 6 [51] | Mothers with AN, BN, EDNOS, and BED gained weight more quickly during pregnancy and lost weight more quickly during the six months after delivery than mothers without EDs. |
| Maria Angelica Nunes, 2014 [39] | Prospective cohort study | Pregnant women who have participated in ECCAGE (The Study of Food Intake and Eating Behaviors in Pregnancy) [44,45,46] | ECCAGE Specific Questionnaire EDE-Q [47] | Excess weight gained during pregnancy and postpartum retention are associated with EDs. Self-induced binging and vomiting decreased in pregnancy and postpartum compared to pre-pregnancy. The frequency of EDs decreases during the gestation period and appears at five months. |
| Cecilia Brundin Petterson, 2016 [43] | Cross-sectional study | Pregnant women and recent births from clinics in Stockholm | EDE-Q [47] | The prevalence of ED is 3% and 7.2% in pre and postpartum, respectively. Women with elevated EDE-Q values before pregnancy may experience greater conflict after delivery, finding it challenging to balance the desire to restrict caloric intake and the desire to eat. |
| A.Easter, 2017 [40] | Prospective cohort study | Women who participated in the Nutrition and Stress During Pregnancy (NEST-p) study and their children [58] | SCID-I [59] EDE-Q [47] STAI [60] BDI [61] PSS [62] PRAQ-R [63] | Women with active EDs have low morning cortisol levels, suggesting that they have a significantly smaller decrease in cortisol throughout the day compared to the healthy mothers, in both adjusted and unadjusted analyses. It is therefore claimed that pregnancy in women with EDs results in dysfunction of the hypothalamic–pituitary–adrenal axis. |
| Anh N. Nguyen, 2017 [42] | Estudio de cohortes | Women and their children from a Generation R Study cohort in the Netherlands [64] | 293-item FFQ [54] Postnatal Breastfeeding Questionnaires | Women with a history of ED have a higher quality diet than those without any history of ED. There are no statistically significant differences between mothers with and without ED in terms of initiation and duration of breastfeeding. |
| Chui Yi Chan, 2018 [65] | Prospective cohort study | Pregnant women in Hong Kong hospitals | EAT-26 [66] Anxiety Subscale of the Hospital Anxiety and Depression Scale [67] Edinburgh Postnatal Depression Scale [68] 10-item Rosenberg Self-Esteem Scale Kansas Marital Satisfaction Scale Chinese Version [69] | There is a significant non-linear relationship between time and ED, with the presence being lower during the pregnancy period and increasing in the postpartum period to levels higher than before pregnancy. Smoking is related to the presence of pre-pregnancy EDs. |
| Maria Giulia Martini, 2018 [41] | Prospective cohort study of pregnant mothers and her babies | Women who participated in the Nutrition and Stress During Pregnancy (NEST-p) study and their children [58] | SCID-I [59] EDE-Q [47] IFQ [70] | 60.6% of the mothers gave BM as exclusive feed at eight weeks, 64% used it partially or totally at six months, and there was no difference between mothers with and without ED. EDs are related to concerns and inappropriate feeding behaviors. |
| Hunna J Watson [71] | Prospective cohort study | Pregnant women who participated in the Norwegian Mother and Child Cohort Study [50] | MoBa Questionnaires | Higher birth weight and large-for-gestational-age in mothers were associated with BED in adjusted models. Mothers born at a lower birth weight were more likely to develop AN. Lifetime BN was not associated with perinatal factors. In this first known investigation into birth characteristics and purging disorder, no significant associations were found. |
© 2020 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (http://creativecommons.org/licenses/by/4.0/).
Share and Cite
Martínez-Olcina, M.; Rubio-Arias, J.A.; Reche-García, C.; Leyva-Vela, B.; Hernández-García, M.; Hernández-Morante, J.J.; Martínez-Rodríguez, A. Eating Disorders in Pregnant and Breastfeeding Women: A Systematic Review. Medicina 2020, 56, 352. https://doi.org/10.3390/medicina56070352
Martínez-Olcina M, Rubio-Arias JA, Reche-García C, Leyva-Vela B, Hernández-García M, Hernández-Morante JJ, Martínez-Rodríguez A. Eating Disorders in Pregnant and Breastfeeding Women: A Systematic Review. Medicina. 2020; 56(7):352. https://doi.org/10.3390/medicina56070352
Chicago/Turabian StyleMartínez-Olcina, María, Jacobo A. Rubio-Arias, Cristina Reche-García, Belén Leyva-Vela, María Hernández-García, Juan José Hernández-Morante, and Alejandro Martínez-Rodríguez. 2020. "Eating Disorders in Pregnant and Breastfeeding Women: A Systematic Review" Medicina 56, no. 7: 352. https://doi.org/10.3390/medicina56070352
APA StyleMartínez-Olcina, M., Rubio-Arias, J. A., Reche-García, C., Leyva-Vela, B., Hernández-García, M., Hernández-Morante, J. J., & Martínez-Rodríguez, A. (2020). Eating Disorders in Pregnant and Breastfeeding Women: A Systematic Review. Medicina, 56(7), 352. https://doi.org/10.3390/medicina56070352








