Spontaneous Heterotopic Pregnancy: Case Report and Literature Review
Abstract
:1. Introduction
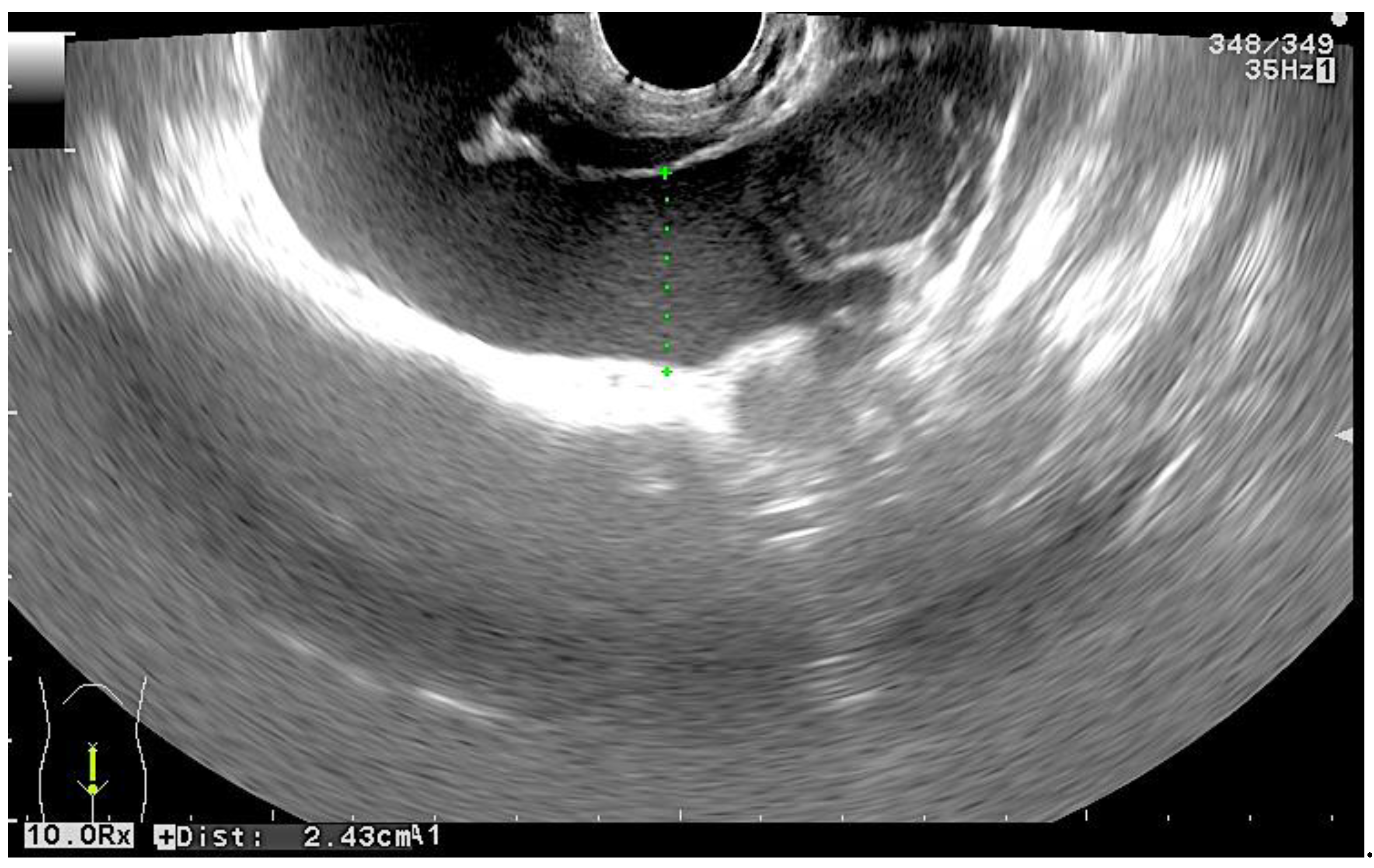
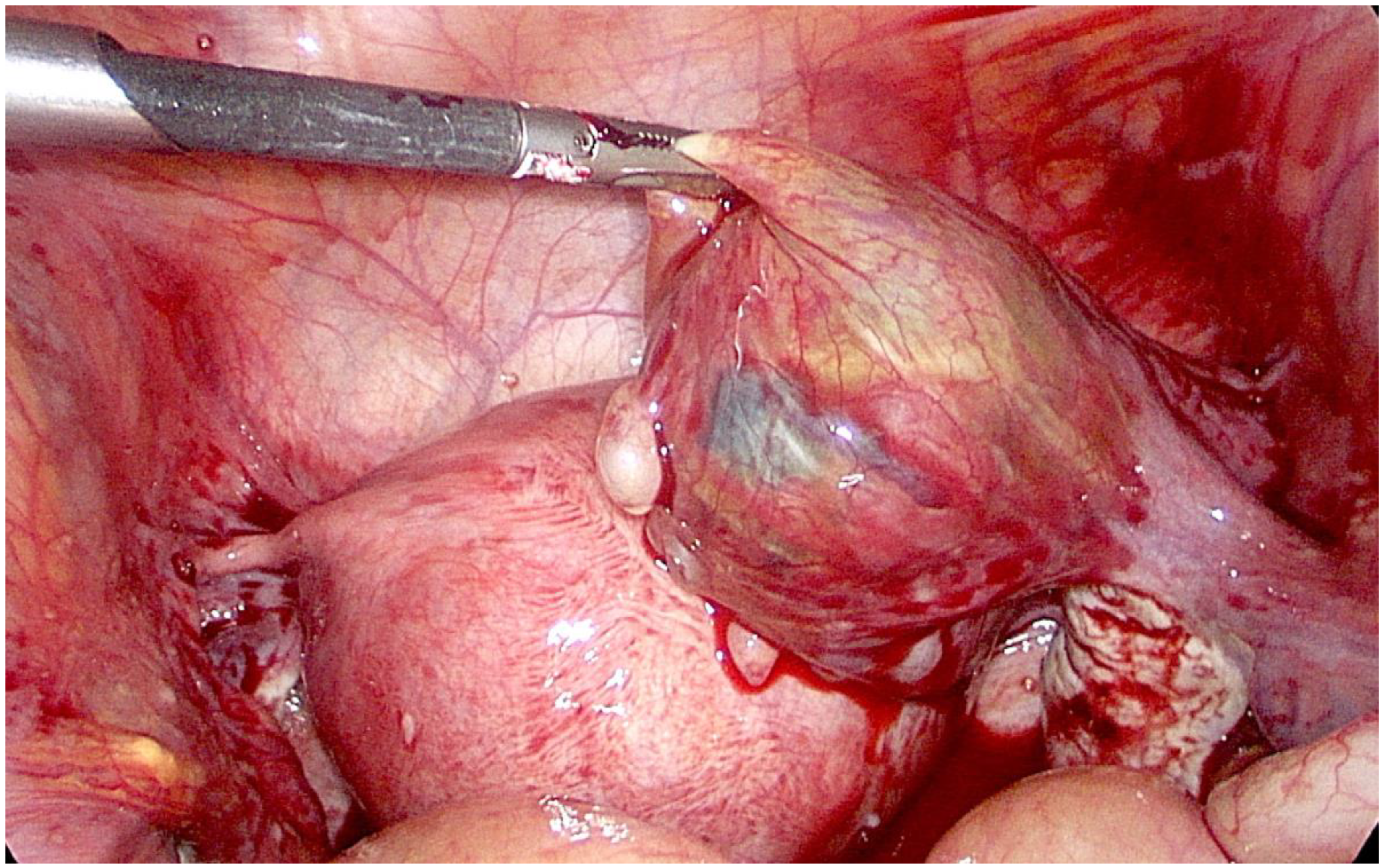
2. Case Presentation
3. Discussion
4. Conclusions
Author Contributions
Funding
Conflicts of Interest
References
- DeVoe, R.W.; Pratt, J.H. Simultaneous intrauterine and extrauterine pregnancy. Am. J. Obstet. Gynecol. 1948, 56, 1119–1126. [Google Scholar] [CrossRef]
- Tal, J.; Haddad, S.; Gordon, N.; Timor-Tritsch, I. Heterotopic pregnancy after ovulation induction and assisted reproductive technologies: A literature review from 1971 to 1993. Fertil. Steril. 1996, 66, 1–12. [Google Scholar] [PubMed]
- Yu, Y.; Xu, W.; Xie, Z.; Huang, Q.; Li, S. Management and outcome of 25 heterotopic pregnancies in Zhejiang, China. Eur. J. Obstet. Gynecol. Reprod. Biol. 2014, 180, 157. [Google Scholar] [CrossRef] [PubMed]
- Nabi, U.; Yousaf, A.; Ghaffar, F.; Sajid, S.; Ahmed, M.M.H. Heterotopic Pregnancy—A Diagnostic Challenge. Six Case Reports and Literature Review. Cureus 2019, 11, e6080. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Li, J.-B.; Kong, L.-Z.; Yang, J.-B.; Niu, G.; Fan, L.; Huang, J.-Z.; Chen, S.-Q. Management of Heterotopic Pregnancy: Experience From 1 Tertiary Medical Center. Medicine (Baltimore) 2016, 95, e2570. [Google Scholar] [CrossRef] [PubMed]
- Oron, G.; Tulandi, T. A pragmatic and evidence-based management of ectopic pregnancy. J. Minim. Invasive Gynecol. 2013, 20, 446–454. [Google Scholar] [CrossRef] [PubMed]
- Chukus, A.; Tirada, N.; Restrepo, R.; Reddy, N.I. Uncommon Implantation Sites of Ectopic Pregnancy: Thinking beyond the Complex Adnexal Mass. Radiographics 2015, 35, 946–959. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Rojansky, N.; Schenker, J.G. Heterotopic pregnancy and assisted reproduction—An update. J. Assist. Reprod. Genet. 1996, 13, 594–601. [Google Scholar] [CrossRef] [PubMed]
- Seffah, J.D. Ultrasonography and ectopic pregnancy—A review. Int. J. Gynaecol. Obstet. 2000, 71, 263–264. [Google Scholar] [CrossRef]
- Shah, N.H.; Shah, R.J.; Kshirsagar, S. Laparoscopic management of heterotopic pregnancy in an IVF conception. Int. J. Reprod. Contracept. Obstet. Gynecol. 2018, 7, 1255–1258. [Google Scholar] [CrossRef] [Green Version]
- Baxi, A.; Kaushal, M.; Karmalkar, H.K.; Sahu, P.; Kadhi, P.; Daval, B. Successful expectant management of tubal heterotopic pregnancy. J. Hum. Reprod. Sci. 2010, 3, 108–110. [Google Scholar] [PubMed]
- Weedin, E.; Kort, J.; Quaas, A.; Baker, V.-L.; Hansen, R.-K. Progesterone supplementation for luteal phase support in non-assisted reproductive technology treatments-prevalence of use and practice patterns among infertility specialists. In Fertility and Sterility; American Society for Reproductive Medicine: Birmingham, AL, USA, 2016; Volume 106, pp. e326–e327. [Google Scholar]
- Haas, D.M.; Ramsey, P.S. Progestogen for preventing miscarriage. Cochrane Database Syst. Rev. 2008, 2, CD003511. [Google Scholar]
- Coomarasamy, A.; Devall, A.J.; Cheed, V.; Harb, H.; Middleton, L.-J.; Williams, H.; Roberts, T.; Goranitis, I.; Ahmed, A.; Gallos, I.D.; et al. A Randomized Trial of Progesterone in Women with Bleeding in Early Pregnancy. N. Engl. J. Med. 2019, 380, 1815–1824. [Google Scholar] [CrossRef]
- Haas, D.M.; Hathaway, T.J.; Ramsey, P.S. Progestogen for preventing miscarriage in women with recurrent miscarriage of unclear etiology. Cochrane Database Syst. Rev. 2019, 20, 2019. [Google Scholar] [CrossRef]

© 2020 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (http://creativecommons.org/licenses/by/4.0/).
Share and Cite
Černiauskaitė, M.; Vaigauskaitė, B.; Ramašauskaitė, D.; Šilkūnas, M. Spontaneous Heterotopic Pregnancy: Case Report and Literature Review. Medicina 2020, 56, 365. https://doi.org/10.3390/medicina56080365
Černiauskaitė M, Vaigauskaitė B, Ramašauskaitė D, Šilkūnas M. Spontaneous Heterotopic Pregnancy: Case Report and Literature Review. Medicina. 2020; 56(8):365. https://doi.org/10.3390/medicina56080365
Chicago/Turabian StyleČerniauskaitė, Miglė, Brigita Vaigauskaitė, Diana Ramašauskaitė, and Mindaugas Šilkūnas. 2020. "Spontaneous Heterotopic Pregnancy: Case Report and Literature Review" Medicina 56, no. 8: 365. https://doi.org/10.3390/medicina56080365
APA StyleČerniauskaitė, M., Vaigauskaitė, B., Ramašauskaitė, D., & Šilkūnas, M. (2020). Spontaneous Heterotopic Pregnancy: Case Report and Literature Review. Medicina, 56(8), 365. https://doi.org/10.3390/medicina56080365



