Avascular Necrosis Bone Complication after Active COVID-19 Infection: Preliminary Results
Abstract
:1. Introduction
2. Materials and Methods
2.1. Patient Selection
2.2. Study Group Characteristics
2.3. Radiological Imaging Technique
- -
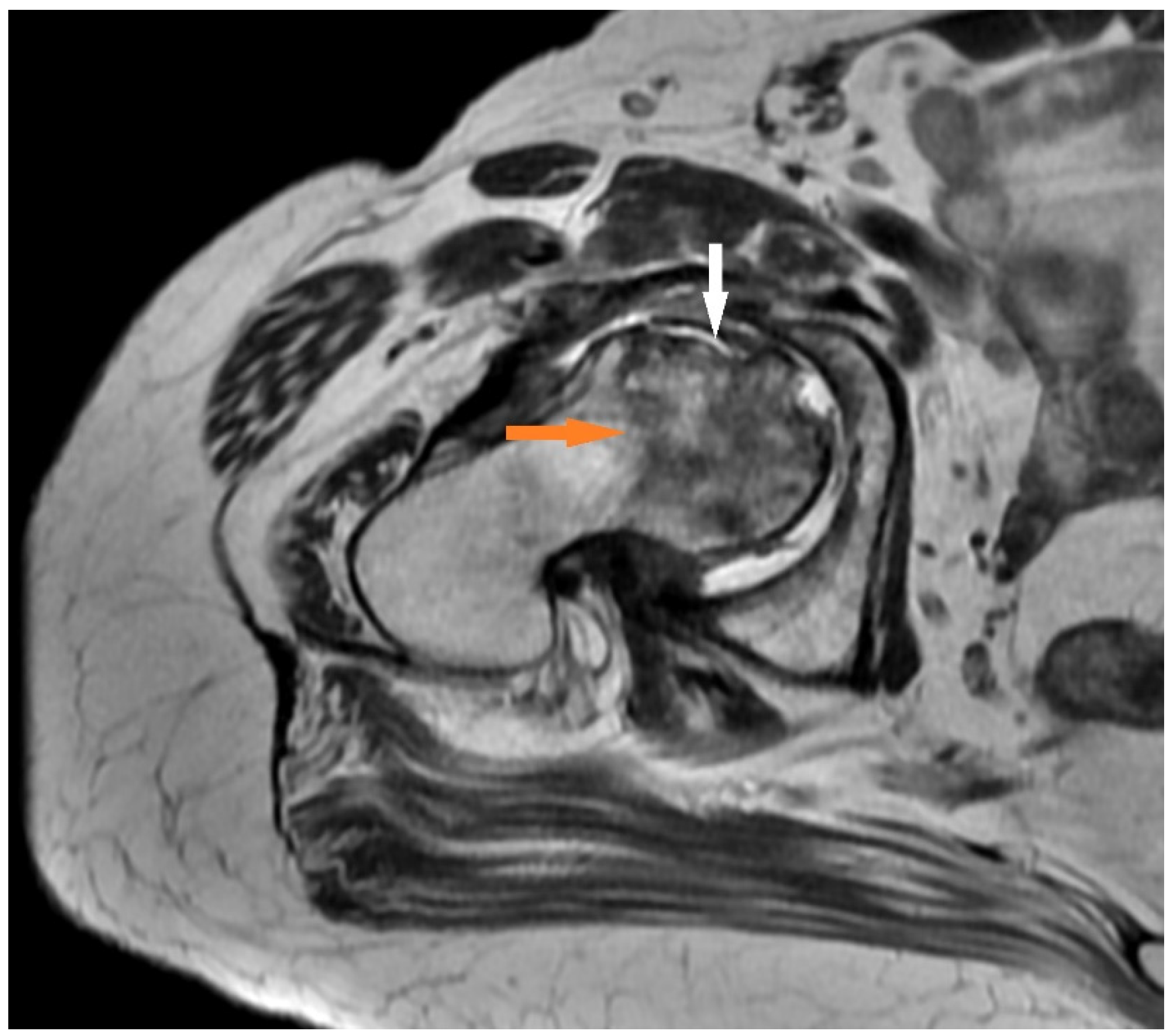
- T1 FSE: the initial specific findings are areas of low signal representing edema, which can be bordered by a hyperintense line, which represents blood products;
- -
- T2 FR FSE: This may show a second hyperintense inner line between normal marrow and ischemic marrow. This appearance is highly specific for AVN of the hip and is known as the “double line sign”.
2.4. AVN Classification
3. Results
3.1. Case Presentation
3.1.1. Case 1 (Patient No. 5)
3.1.2. Case 2 (Patient No. 1)
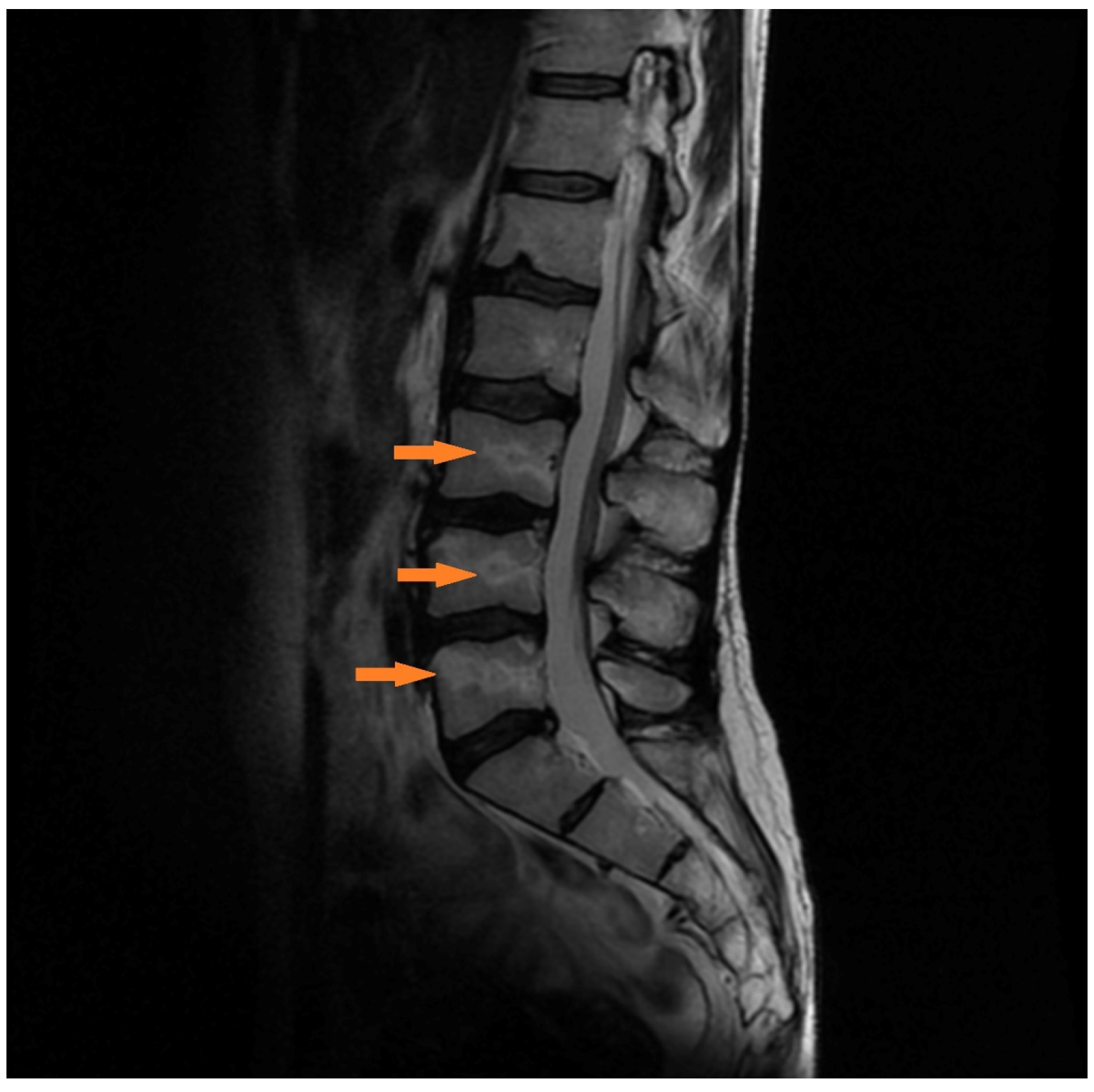
3.1.3. Case 3 (Patient No. 7)
4. Discussion
4.1. Pathophysiology of MSK Diseases after COVID-19
4.2. Corticosteroids Therapy
4.3. Clinical Reports
4.4. Limitations
5. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Conflicts of Interest
References
- Disser, N.P.; De Micheli, A.J.; Schonk, M.M.; Konnaris, M.A.; Piacentini, A.N.; Edon, D.L.; Tresdahl, B.G.; Rodeo, S.A.; Casey, E.K.; Mendias, C.L. Musculoskeletal Consequences of COVID-19. J. Bone Jt. Surg. Am. 2020, 102, 1197–1204. [Google Scholar] [CrossRef]
- Huang, C.; Wang, Y.; Li, X.; Zhao, J.; Hu, Y.; Zhang, I.; Fan, G.; Xu, J.; Gu, X.; Cheng, Z.; et al. Clinical features of patients infected with 2019 novel coronavirus in Wuhan, China. Lancet 2020, 395, 497–506. [Google Scholar] [CrossRef] [Green Version]
- Liu, J.; Li, S.; Liang, B.; Wang, X.; Wang, H.; Li, W.; Tong, Q.; Yi, J.; Zhao, L.; Xiong, L.; et al. Longitudinal characteristics of lymphocyte responses and cytokine profiles in the peripheral blood of SARS-CoV-2 infected patients. EBioMedicine 2020, 55, 102763. [Google Scholar] [CrossRef] [PubMed]
- Shen, J.; Liang, B.L.; Zeng, Q.S.; Chen, J.Y.; Liu, Q.Y.; Chen, R.C.; Zhong, N.S. Report on the investigation of lower extremity osteonecrosis with magnetic resonance imaging in recovered severe acute respiratory syndrome in Guangzhou. Zhonghua Yi Xue Za Zhi 2004, 84, 1814–1817. [Google Scholar]
- Griffith, J.F. Musculoskeletal complications of severe acute respiratory syndrome. Semin Musculoskelet Radiol. 2011, 15, 554–560. [Google Scholar] [CrossRef] [PubMed]
- Glickstein, M.F.; Burk, D.L., Jr.; Schiebler, M.L.; Cohen, E.K.; Dalinka, M.K.; Steinberg, M.E.; Kressel, H.Y. Avascular necrosis versus other diseases of the hip: Sensitivity of MR imaging. Radiology 1988, 169, 213–215. [Google Scholar] [CrossRef]
- Verity, R.; Okell, L.C.; Dorigatti, I.; Winskill, P.; Whittaker, C.; Imai, N.; Cuomo-Dannenburg, G.; Thompson, H.; Walker, P.G.T.; Fu, H.; et al. Estimates of the severity of coronavirus disease 2019: A model-based analysis. Lancet Infect. Dis. 2020, 20, 669–677. [Google Scholar] [CrossRef]
- Steinberg, M.E.; Hayken, G.D.; Steinberg, D.R. A quantitative system for staging avascular necrosis. J. Bone Jt. Surg. Br. 1995, 77, 34–41. [Google Scholar] [CrossRef]
- Li, K.; Huang, B.; Wu, M.; Zhong, A.; Li, L.; Cai, Y.; Wang, Z.; Wu, L.; Zhu, M.; Li, J.; et al. Dynamic changes in anti-SARS-CoV-2 antibodies during SARS-CoV-2 infection and recovery from COVID-19. Nat. Commun. 2020, 11, 6044. [Google Scholar] [CrossRef]
- Ahmad, I.; Rathore, F.A. Neurological manifestations and complications of COVID-19: A literature review. J. Clin. Neurosci. 2020, 77, 8–12. [Google Scholar] [CrossRef]
- Zacharias, H.; Dubey, S.; Koduri, G.; D’Cruz, D. Rheumatological complications of Covid 19. Autoimmun. Rev. 2021, 20, 102883. [Google Scholar] [CrossRef] [PubMed]
- Aghagoli, G.; Gallo Marin, B.; Soliman, L.B.; Sellke, F.W. Cardiac involvement in COVID-19 patients: Risk factors, predictors, and complications: A review. J. Card. Surg. 2020, 35, 1302–1305. [Google Scholar] [CrossRef] [PubMed]
- Dasgupta, A.; Kalhan, A.; Kalra, S. Long term complications and rehabilitation of COVID-19 patients. J. Pak. Med. Assoc. 2020, 70, 131–135. [Google Scholar] [CrossRef] [PubMed]
- Simões, E.S.A.C.; Teixeira, M.M. ACE inhibition, ACE2 and angiotensin-(1-7) axis in kidney and cardiac inflammation and fibrosis. Pharmacol. Res. 2016, 107, 154–162. [Google Scholar] [CrossRef] [PubMed]
- Jia, H. Pulmonary angiotensin-converting enzyme 2 (ACE2) and inflammatory lung disease. Shock 2016, 46, 239–248. [Google Scholar] [CrossRef] [PubMed]
- Salvio, G.; Gianfelice, C.; Firmani, F.; Lunetti, S.; Balercia, G.; Giacchetti, G. Bone Metabolism in SARS-CoV-2 Disease: Possible Osteoimmunology and Gender Implications. Clin. Rev. Bone Miner. Metab. 2020, 18, 51–57. [Google Scholar] [CrossRef] [PubMed]
- Tao, H.; Bai, J.; Zhang, W.; Zheng, K.; Guan, P.; Ge, G.; Li, M.; Geng, D. Bone biology and COVID-19 infection: Is ACE2 a potential influence factor? Med. Hypotheses 2020, 144, 110178. [Google Scholar] [CrossRef]
- Barlow, A.; Landolf, K.M.; Barlow, B.; Yeung, S.Y.A.; Heavner, J.J.; Claassen, C.W.; Heavner, M.S. Review of Emerging Pharmacotherapy for the Treatment of Coronavirus Disease 2019. Pharmacother. J. Hum. Pharmacol. Drug Ther. 2020, 40, 416–437. [Google Scholar] [CrossRef] [Green Version]
- Dubrovsky, A.M.; Lim, M.J.; Lane, N.E. Osteoporosis in Rheumatic Diseases: Anti-rheumatic Drugs and the Skeleton. Calcif Tissue Int. 2018, 102, 607–618. [Google Scholar] [CrossRef]
- Agarwala, S.R.; Vijayvargiya, M.; Pandey, P. Avascular necrosis as a part of ‘long COVID-19’. BMJ Case Rep. 2021, 14, e242101. [Google Scholar] [CrossRef]
- Singh, A.K.; Majumdar, S.; Singh, R.; Misra, A. Role of corticosteroid in the management of COVID-19: A systemic review and a Clinician’s perspective. Diabetes Metab. Syndr. 2020, 14, 971–978. [Google Scholar] [CrossRef] [PubMed]
- Shah, K.N.; Racine, J.; Jones, L.C.; Aaron, R.K. Pathophysiology and risk factors for osteonecrosis. Curr. Rev. Musculoskelet Med. 2015, 8, 201–209. [Google Scholar] [CrossRef] [Green Version]
- Zhou, F.; Yu, T.; Du, R.; Fan, G.; Liu, Y.; Liu, Z.; Xiang, J.; Wang, Y.; Song, B.; Gu, X.; et al. Clinical course and risk factors for mortality of adult inpatients with COVID-19 in Wuhan, China: A retrospective cohort study. Lancet 2020, 395, 1054–1062. [Google Scholar] [CrossRef]
- Lv, H.; de Vlas, S.J.; Liu, W.; Wang, T.B.; Cao, Z.Y.; Li, C.P.; Cao, W.C.; Richardus, J.H. Avascular osteonecrosis after treatment of SARS: A 3-year longitudinal study. Trop. Med. Int. Health 2009, 14, 79–84. [Google Scholar] [CrossRef]
- Hong, N.; Du, X.K. Avascular necrosis of bone in severe acute respiratory syndrome. Clin. Radiol. 2004, 59, 602–608. [Google Scholar] [CrossRef] [Green Version]
- Cibulka, M.T.; White, D.M.; Woehrle, J.; Harris-Hayes, M.; Enseki, K.; Fagerson, T.L.; Slover, J.; Godges, J.J. Hip pain and mobility deficits—Hip osteoarthritis: Clinical practice guidelines linked to the international classification of functioning, disability, and health from the orthopaedic section of the American Physical Therapy Association. J. Orthop. Sports Phys. Ther. 2009, 39, A1–A25. [Google Scholar] [CrossRef] [PubMed] [Green Version]

| Patient No. | Age | Sex | Chronic Diseases | BMI | Severity of COVID-19 | COVID-19 Therapy/Steroids |
|---|---|---|---|---|---|---|
| 1 | 62 | M | DM | 23 | severe | no |
| 2 | 56 | M | DM | 30 | mild | no |
| 3 | 57 | F | no | 26 | severe | yes |
| 4 | 70 | F | no | 25 | moderate | no |
| 5 | 43 | F | Hypertension | 26 | moderate | yes |
| 6 | 54 | M | Depression | 22 | moderate | yes |
| 7 | 66 | F | no | 20 | moderate | no |
| 8 | 39 | F | no | 19 | severe | yes |
| 9 | 68 | F | no | 26 | mild | no |
| 10 | 73 | M | no | 27 | moderate | no |
| mean SD | 58.8 11.3 | 24.4 3.37 |
| No. | Joint | Time of Onset of Joint Symptoms from the Beginning of Infection | Arthroplasty | Steinberg Scale | Follow-Up (Months) | VAS Pain Initially | Pain Follow Up VAS |
|---|---|---|---|---|---|---|---|
| 1 | hip | 11 | yes | 4 | 10 | 8 | 2 |
| 2 | knee | 10 | no | 2 | 9 | 9 | 0 |
| 3 | shoulder | 11 | no | 2 | 7 | 6 | 0 |
| 4 | hip | 7 | yes | 4 | 7 | 8 | 0 |
| 5 | both knees | 21 | no | 2 | 8 | 7 | 1 |
| 6 | knee | 17 | no | 3 | 10 | 8 | 0 |
| 7 | lumbar spine | 14 | no | 2 | 8 | 8 | 1 |
| 8 | sacrum | 14 | no | 2 | 5 | 8 | 1 |
| 9 | hip | 22 | no | 2 | 5 | 7 | 0 |
| 10 | knee | 17 | yes | 4 | 4 | 8 | 0 |
| mean | 14 | 3 | 7 | 8 | 0,5 |
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2021 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Sulewski, A.; Sieroń, D.; Szyluk, K.; Dąbrowski, M.; Kubaszewski, Ł.; Lukoszek, D.; Christe, A. Avascular Necrosis Bone Complication after Active COVID-19 Infection: Preliminary Results. Medicina 2021, 57, 1311. https://doi.org/10.3390/medicina57121311
Sulewski A, Sieroń D, Szyluk K, Dąbrowski M, Kubaszewski Ł, Lukoszek D, Christe A. Avascular Necrosis Bone Complication after Active COVID-19 Infection: Preliminary Results. Medicina. 2021; 57(12):1311. https://doi.org/10.3390/medicina57121311
Chicago/Turabian StyleSulewski, Adam, Dominik Sieroń, Karol Szyluk, Mikołaj Dąbrowski, Łukasz Kubaszewski, Dawid Lukoszek, and Andreas Christe. 2021. "Avascular Necrosis Bone Complication after Active COVID-19 Infection: Preliminary Results" Medicina 57, no. 12: 1311. https://doi.org/10.3390/medicina57121311
APA StyleSulewski, A., Sieroń, D., Szyluk, K., Dąbrowski, M., Kubaszewski, Ł., Lukoszek, D., & Christe, A. (2021). Avascular Necrosis Bone Complication after Active COVID-19 Infection: Preliminary Results. Medicina, 57(12), 1311. https://doi.org/10.3390/medicina57121311







