Ethical and Legal Challenges of Telemedicine in the Era of the COVID-19 Pandemic
Abstract
:1. Introduction
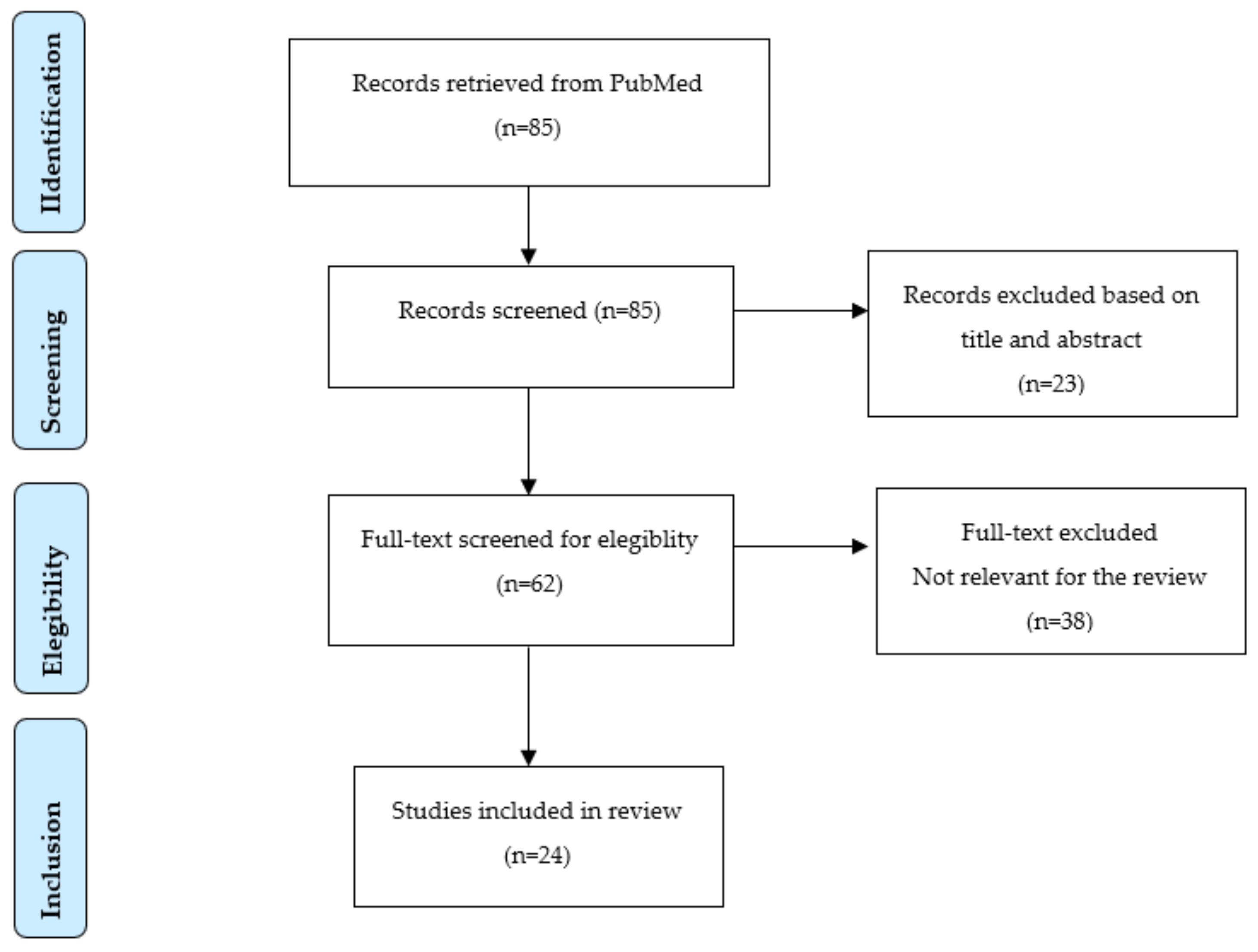
2. Materials and Methods
3. Results
| Medical or Health Service | Ethical and/or Legal Issues | Medical Purposes/Disciplines | Article Type | Location | Reference |
|---|---|---|---|---|---|
| Telemedicine and Telehealth | Data privacy, security and storage; Clear regulations/laws for legal security of patients and professionals; Informed consent: practice guidelines and standardized informed consent forms (risks and benefits of remote therapy and research) are recommended; Professional secrecy; Patients medical records availability; Noncompliance; Autonomy; Professional–patient relationship; Nonmaleficence and beneficence (minimize harm); Service quality and effectiveness; How frameworks, codes of conduct, or guidelines, are being used to improve ethical telehealth practice; Confidentiality; Liability; Reimbursement; Access for rural/remote populations, patients of diverse races, ethnicities, socioeconomic statuses (equity, justice); Licensing requirements; Risk of malpractice and insurance coverage; Establishment of protocols for managing laboratory tests, prescriptions, and scheduling; Recording issues: doctors must obtain consent before recording, patients do not need a doctor’s consent to record a consultation; Tailoring services to each patient; Patient and clinicians responsibilities; Commercialization; Cybersecurity and software safety; Evaluation as an ethical imperative (sound evidence on which to base analyses, decisions, and services); Compliance with ethical principles; Legality of patient recording depends on the state or territory: in certain jurisdictions, patients can secretly record a consultation without the consent of the clinician and this recording may be used in legal or disciplinary proceedings; Patient’s medical records will generally be held and owned by the clinician or health care organization, but patients are entitled to access and take a copy of their records; Safeguarding risks (patient self-harm); Safety (such as how to deal with a patient falling in their home during a consultation): guidance to ensure the safety of patients and clinicians in delivering virtual consultations is needed; Health Insurance Portability and Accountability Act (HIPAA) law revision; Fidelity and responsibility (trusting relationships); Integrity (no fraudulent behavior nor personal gain); Respect for people’s rights and dignity (protect privacy and safeguarding); Need of ethics code; Boundaries of competence; Unfair discrimination in treatment delivery; Digital communication with patients must be compliant with the country’s and organization’s data protection and telehealth regulations that are rapidly evolving and subject to change. | Nursing; Radiology; Neurology; Dermatology; Psychotherapy and mental health. Clinical and routinehealth care; Follow-up care and of chronic diseases; Chronic medical illnesses and malignancies care; Visits to determine the urgency of medical or surgical interventions; COVID-19 severe cases screening; Monitoring clinically stable patients; Maintaining outpatient care; Mental health care; Radiology; Cardiological diagnosis; Dermatology care; Ophthalmology care; Otorhinolaryngology care; Non urgent clinical care; Second opinions and medical check-ups; Complementary service to face-to-face consultations; Virtual Orthopaedic and Musculoskeletal care; Daily clinical practice such as perinatal and neonatal care; Preventive care; Diagnosis and treatment of a health condition; Psychological care; Management of diabetes, hypertension, asthma, stroke, cancers, and chronic pain; Triage and management of a wide range of acute conditions. | Systematic Review; 5 Reviews; Special Article; Ethics and Law article; Research Article; Legislation Article; Legal issues and risk management article; Ethics Article; Recommendations | Various, USA; India; Brazil; UK; Various; Spain; Australia; | [16] [19] [21] [23] [26] [11] [6] [28] [29] [30] [31] [33] [34] |
| Pediatric and adolescent telehealth; Behavioral telehealth. | Privacy and security challenges; Inequitable access to care; Unsustainable costs in a fee-for-service system; Lack of quality metrics for novel care-delivery modalities; Telehealth policies and regulations (e.g., payer restrictions on telehealth reimbursement, complex medication-prescribing regulations for virtual care). | Pediatric ambulatory care; Adolescent care; Screening; Presurgical visit; Chronic condition management; Follow-up appointments; Behavioral and mental health (ADHD, Depression). | Review | USA | [10] |
| Telemedicine for abortion | Informed consent; Safeguarding support; Good-quality care; Equity of access. | Abortion medication and care. | Review (viewpoint) | Various | [17] |
| Teledermatology | Informed consent; Medical ethics; Lack of personal relationship between the patient and the dermatologist is a main ethical concern; Strictness of law varies from country to country; Malpractice or risk of telemalpractice (phantom patient); Risk of abuse and breaches of patient confidentiality; Patient’s autonomy; Privacy; Data protection. | Dermatology care and treatment; Chronic skin conditions with co-morbidities; Skin disorders; Skin diseases care; Diagnostic and treatment purposes; Follow-up appointments. | 2 Reviews; Research Article. | India; Various. | [18] [20] [27] |
| Teleneurology | Malpractice coverage; Data protection; Informed consent; Patient privacy; Validation and development of best practice standards. | Neurology outpatient care; Follow-up visits. | Review | USA | [22] |
| Sport and exercise medicine telehealth | Ensure patient safety; Secure and effective communication methods; Ensure that patient feedback mechanisms are in place; Evaluate and ensure patient satisfaction; Informed care and shared treatment decisions; Promoting open communication and consent; Mutual respect; Access to health information; Physician autonomy and responsibilities. | Clinical care in the broad field of sports medicine; Follow-up consultations. | Review | Various | [24] |
| Telepsychiatry, Teleanalysis or Teletherapy | Telemedicine use; Privacy; Confidentiality; Data protection; Security; Informed consent; Physician’s malpractice and liability. Patient benefice; Justice (support/access is variable); Autonomy; Licensing and reimbursement; New guidelines to ensure patient privacy and quality of care. | Psychiatric and mental health care services and assistance; Psychoanalysis; Psychotherapy. | Review; Healthcare ethics article | Various; USA. | [25] [32] [8] |
| Telecardiology; Telemonitoring in dialysis; Telemonitoring in diabetes; Perinatal Telemonitoring. | Authorization and accreditation; Protection of patient confidentiality; Professional liability (e.g.,: incorrect diagnosis: erroneous reading of the report or to the poor quality of transmitted images); Absence of specific regulatory provisions; Physician–patient relationship; Privacy; Informed consent; Data sharing; Malpractice; Information security; Patient self-determination; Standardization of the practices; Economic reimbursement. | COVID-19 care; Chronically ill out-of-hospital patients (cardiology, diabetes); Nephrology; Endocrinology; Gynecology. | Commentary | Italy | [1] |
4. Discussion
- -
- Conducting telehealth in private settings, such as a doctor in a clinic or office connecting to a patient who is at home or at another clinic. Providers should always use private locations and patients should not receive telehealth services in public or semi-public settings, absent patient consent or exigent circumstances;
- -
- Obtaining patients’ consent verbally and noting it in the medical record. For a signed form, the patient portal or the mail should be used to obtain a signature. It is not necessary to wait for a signed consent form. A telehealth visit can be conducted with patients giving their consent verbally.
- -
- Treat telehealth appointments in the same way as an in-person appointment and the patient should not hesitate to ask questions and request explanations or clarifications [39].
5. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Acknowledgments
Conflicts of Interest
References
- Ferorelli, D.; Nardelli, L.; Spagnolo, L.; Corradi, S.; Silvestre, M.; Misceo, F.; Marrone, M.; Zotti, F.; Mandarelli, G.; Solarino, B.; et al. Medical Legal Aspects of Telemedicine in Italy: Application Fields, Professional Liability and Focus on Care Services During the COVID-19 Health Emergency. J. Prim. Care Community Health 2020, 11, 2150132720985055. [Google Scholar] [CrossRef] [PubMed]
- World Health Organization. A Health Telematics Policy in Support of WHO’s Health-For-All Strategy for Global Health Development: Report of the WHO Group Consultation on Health Telematics. 1998. Available online: http://apps.who.int/iris/bitstream/10665/63857/1/WHO_DGO_98.1.pdf (accessed on 15 September 2021).
- Centers for Medicare and Medicaid Services. Medicare Telemedicine Health Care Provider Fact Sheet. 2020. Available online: https://www.cms.gov/newsroom/fact-sheets/medicare-telemedicine-health-care-provider-fact-sheet (accessed on 15 September 2021).
- World Medical Association. WMA Statement on the Ethics of Telemedicine. Adopted by the 58th WMA General Assembly, Copenhagen, Denmark, October 2007 and amended by the 69th WMA General Assembly, Reykjavik, Iceland, October 2018. Available online: https://www.wma.net/policies-post/wma-statement-on-the-ethics-of-telemedicine/ (accessed on 24 September 2021).
- Mittal, M.; Battineni, G.; Goyal, L.M.; Chhetri, B.; Oberoi, S.V.; Chintalapudi, N.; Amenta, F. Cloud-based framework to mitigate the impact of COVID-19 on seafarers’ mental health. Int. Marit. Health 2020, 71, 213–214. [Google Scholar] [CrossRef] [PubMed]
- Gil Membrado, C.; Barrios, V.; Cosín-Sales, J.; Gámez, J.M. Telemedicine, ethics, and law in times of COVID-19. A look towards the future. Rev. Clin. Esp. 2021, 221, 408–410. [Google Scholar] [CrossRef] [PubMed]
- Nittari, G.; Khuman, R.; Baldoni, S.; Palllotta, G.; Battineni, G.; Sirignano, A.; Amenta, F.; Ricci, G. Telemedicine Practice: Review of the Current Ethical and Legal Challenges. Telemed. J. Health 2020, 26, 1427–1437. [Google Scholar] [CrossRef] [Green Version]
- Merchant, J. Working online due to the COVID-19 pandemic: A research and literature review. J. Anal. Psychol. 2021, 66, 484–505. [Google Scholar] [CrossRef]
- Scharff, S. In response to Kristin White “Practising as an analyst in Berlin in times of the coronavirus”. Int. J. Psychoanal. 2020, 101, 585–588. [Google Scholar] [CrossRef]
- Curfman, A.; McSwain, S.D.; Chuo, J.; Yeager-McSwain, B.; Schinasi, D.A.; Marcin, J.; Herendeen, N.; Chung, S.L.; Rheuban, K.; Olson, C.A. Pediatric Telehealth in the COVID-19 Pandemic Era and Beyond. Pediatrics 2021, 148, e2020047795. [Google Scholar] [CrossRef]
- Kaplan, B. Revisiting Health Information Technology Ethical, Legal, And Social Issues And Evaluation: Telehealth/Telemedicine And COVID-19. Int. J. Med. Inform. 2020, 143, 104239. [Google Scholar] [CrossRef]
- Battineni, G.; Nittari, G.; Sirignano, A.; Amenta, F. Are Telemedicine Systems Effective Healthcare Solutions during the COVID-19 Pandemic? J. Taibah. Univ. Med. Sci. 2021, 16, 305–306. [Google Scholar] [CrossRef]
- Bashshur, R.; Doarn, C.R.; Frenk, J.M.; Kvedar, J.C.; Woolliscroft, J.O. Telemedicine and the COVID-19 pandemic, lessons for the future. Telemed. J. Health 2020, 26, 571–573. [Google Scholar] [CrossRef] [Green Version]
- Stipa, G.; Gabbrielli, F.; Rabbito, C.; Di Lazzaro, V.; Amantini, A.; Grippo, A.; Carrai, R.; Pasqui, R.; Barloscio, D.; Olivi, D.; et al. Telemedicine Working Group. The Italian technical/administrative recommendations for telemedicine in clinical neurophysiology. Neurol. Sci. 2021, 42, 1923–1931. [Google Scholar] [CrossRef]
- Hollander, J.E.; Carr, B.G. Virtually perfect? Telemedicine for covid-19. N. Engl. J. Med. 2020, 382, 1679–1681. [Google Scholar] [CrossRef]
- Keenan, A.J.; Tsourtos, G.; Tieman, J. The Value of Applying Ethical Principles in Telehealth Practices: Systematic Review. J. Med. Internet Res. 2021, 23, e25698. [Google Scholar] [CrossRef]
- Romanis, E.C.; Parsons, J.A.; Salter, I.; Hampton, T. Safeguarding and teleconsultation for abortion. Lancet 2021, 398, 555–558. [Google Scholar] [CrossRef]
- Vashisht, D.; Neema, S.; Venugopalan, R.; Pathania, V.; Sandhu, S.; Vasudevan, B. Dermatology practice in the times of the COVID-19 pandemic. Indian J. Dermatol. Venereol. Leprol. 2021, 87, 603–610. [Google Scholar] [CrossRef]
- Kronenfeld, J.P.; Penedo, F.J. Novel Coronavirus (COVID-19): Telemedicine and Remote Care Delivery in a Time of Medical Crisis, Implementation, and Challenges. Transl. Behav. Med. 2021, 11, 659–663. [Google Scholar] [CrossRef]
- Arimany-Manso, J.; Pujol, R.M.; García-Patos, V.; Saigí, U.; Martin-Fumadó, C. Medicolegal Aspects of Teledermatology. Actas Dermosifiliogr. 2020, 111, 815–821. [Google Scholar] [CrossRef]
- Ghosh, A.; Gupta, R.; Misra, A. Telemedicine for diabetes care in India during COVID19 pandemic and national lockdown period: Guidelines for physicians. Diabetes Metab. Syndr. 2020, 14, 273–276. [Google Scholar] [CrossRef]
- Roy, B.; Nowak, R.J.; Roda, R.; Khokhar, B.; Patwa, H.S.; Lloyd, T.; Rutkove, S.B. Teleneurology during the COVID-19 pandemic: A step forward in modernizing medical care. J. Neurol. Sci. 2020, 414, 116930. [Google Scholar] [CrossRef]
- Caetano, R.; Silva, A.B.; Guedes, A.C.C.M.; Paiva, C.C.N.; Ribeiro, G.D.R.; Santos, D.L.; Silva, R.M.D. Challenges and opportunities for telehealth during the COVID-19 pandemic: Ideas on spaces and initiatives in the Brazilian context. Cad. Saude Publica 2020, 36, e00088920. [Google Scholar] [CrossRef]
- Dijkstra, H.P.; Ergen, E.; Holtzhausen, L.; Beasley, I.; Alonso, J.M.; Geertsema, L.; Geertsema, C.; Nelis, S.; Ngai, A.S.H.; Stankovic, I.; et al. Remote assessment in sport and exercise medicine (SEM): A narrative review and teleSEM solutions for and beyond the COVID-19 pandemic. Br. J. Sports Med. 2020, 54, 1162–1167. [Google Scholar] [CrossRef]
- Di Carlo, F.; Sociali, A.; Picutti, E.; Pettorruso, M.; Vellante, F.; Verrastro, V.; Martinotti, G.; di Giannantonio, M. Telepsychiatry and other cutting-edge technologies in COVID-19 pandemic: Bridging the distance in mental health assistance. Int. J. Clin. Pract. 2021, 75, e13716. [Google Scholar] [CrossRef]
- Howgego, G.; Sharma, I.; Kalu, P. The rules for online clinical engagement in the COVID era. J. Plast Reconstr. Aesthet. Surg. 2020, 73, 2127–2135. [Google Scholar] [CrossRef]
- Manuelyan, K.; Shahid, M.; Vassilev, V.; Drenovska, K.; Vassileva, S. Direct patient-to-physician teledermatology: Not a flash in the pan(demic). Clin. Dermatol. 2021, 39, 45–51. [Google Scholar] [CrossRef]
- Farmer, C.C.; Pang, S.C.; Kevat, D.; Dean, J.; Panaccio, D.; Mahar, P.D. Medico-legal implications of audiovisual recordings of telehealth encounters. Med. J. Aust. 2021, 214, 357–359.e1. [Google Scholar] [CrossRef]
- Gilbert, A.W.; Booth, G.; Betts, T.; Goldberg, A. A mixed-methods survey to explore issues with virtual consultations for musculoskeletal care during the COVID-19 pandemic. BMC Musculoskelet. Disord. 2021, 22, 245. [Google Scholar] [CrossRef]
- Theodos, K.; Sittig, S. Health Information Privacy Laws in the Digital Age: HIPAA Doesn’t Apply. Perspect. Health Inf. Manag. 2020, 18, 11. [Google Scholar]
- Cypher, R.L. Telehealth and Telemedicine During a Crisis. J. Perinat. Neonatal. Nurs. 2020, 34, 205–207. [Google Scholar] [CrossRef]
- Chin, H.P.; Palchik, G. Telepsychiatry in the Age of COVID: Some Ethical Considerations. Camb. Q. Healthc. Ethic. 2021, 30, 37–41. [Google Scholar] [CrossRef]
- Chenneville, T.; Schwartz-Mette, R. Ethical Considerations for Psychologists in the Time of COVID-19. Am. Psychol. 2020, 75, 644–654. [Google Scholar] [CrossRef]
- Car, J.; Koh, G.C.; Foong, P.S.; Wang, C.J. Video consultations in primary and specialist care during the covid-19 pandemic and beyond. BMJ. 2020 Oct 20;371:m3945. BMJ Clin. Res. Ed. 2020, 371, m3945. [Google Scholar] [CrossRef]
- Di Trana, A.; Busardò, F.; Ricci, G.; Sirignano, A. Commentary: Tele-COVID-19: Does it improve the provision of health services? Eur. Rev. Med. Pharmacol. Sci. 2021, 25, 2152–2153. [Google Scholar] [CrossRef] [PubMed]
- Gabbrielli, F.; Bertinato, L.; De Filippis, G.; Bonomini, M.; Cipolla, M. Indicazioni ad Interim per Servizi Assistenziali di Telemedicina Durante L’emergenza Sanitaria COVID-19. Versione del 13 Aprile 2020; Rapporto ISS COVID-19, n. 12/2020; Istituto Superiore di Sanità: Roma, Italy, 2020. [Google Scholar]
- Baldoni, S.; Amenta, F.; Ricci, G. Telepharmacy Services: Present Status and Future Perspectives: A Review. Medicina 2019, 55, 327. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Baldoni, S.; Pallotta, G.; Traini, E.; Sagaro, G.G.; Nittari, G.; Amenta, F. A survey on feasibility of telehealth services among young Italian pharmacists. Pharm. Pract. 2020, 18, 1926. [Google Scholar] [CrossRef]
- Health Resources and Services Administration (HRSA). Telehealth: Health Care from the Safety of Our Homes. Available online: https://telehealth.hhs.gov/ (accessed on 2 November 2021).
- American Medical Association (AMA). Ethical Practice in Telemedicine. Available online: https://www.ama-assn.org/delivering-care/ethics/ethical-practice-telemedicine (accessed on 2 November 2021).
- American Psychological Association (APA). How to do Group Therapy Using Telehealth. Group Therapists Are Responding to COVID-19 by Rapidly Transitioning from in-Person to Online Therapies. Available online: https://www.apaservices.org/practice/legal/technology/group-therapy-telehealth-covid-19 (accessed on 2 November 2021).
- Kaiser Family Foundation (KFF). Opportunities and Barriers for Telemedicine in the U.S. During the COVID-19 Emergency and Beyond. Available online: https://www.kff.org/womens-health-policy/issue-brief/opportunities-and-barriers-for-telemedicine-in-the-u-s-during-the-covid-19-emergency-and-beyond/ (accessed on 2 November 2021).
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2021 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Solimini, R.; Busardò, F.P.; Gibelli, F.; Sirignano, A.; Ricci, G. Ethical and Legal Challenges of Telemedicine in the Era of the COVID-19 Pandemic. Medicina 2021, 57, 1314. https://doi.org/10.3390/medicina57121314
Solimini R, Busardò FP, Gibelli F, Sirignano A, Ricci G. Ethical and Legal Challenges of Telemedicine in the Era of the COVID-19 Pandemic. Medicina. 2021; 57(12):1314. https://doi.org/10.3390/medicina57121314
Chicago/Turabian StyleSolimini, Renata, Francesco Paolo Busardò, Filippo Gibelli, Ascanio Sirignano, and Giovanna Ricci. 2021. "Ethical and Legal Challenges of Telemedicine in the Era of the COVID-19 Pandemic" Medicina 57, no. 12: 1314. https://doi.org/10.3390/medicina57121314
APA StyleSolimini, R., Busardò, F. P., Gibelli, F., Sirignano, A., & Ricci, G. (2021). Ethical and Legal Challenges of Telemedicine in the Era of the COVID-19 Pandemic. Medicina, 57(12), 1314. https://doi.org/10.3390/medicina57121314








