Management of a Mycotic Aneurysm in a Patient with COVID-19: A Case Report
Abstract
:1. Introduction
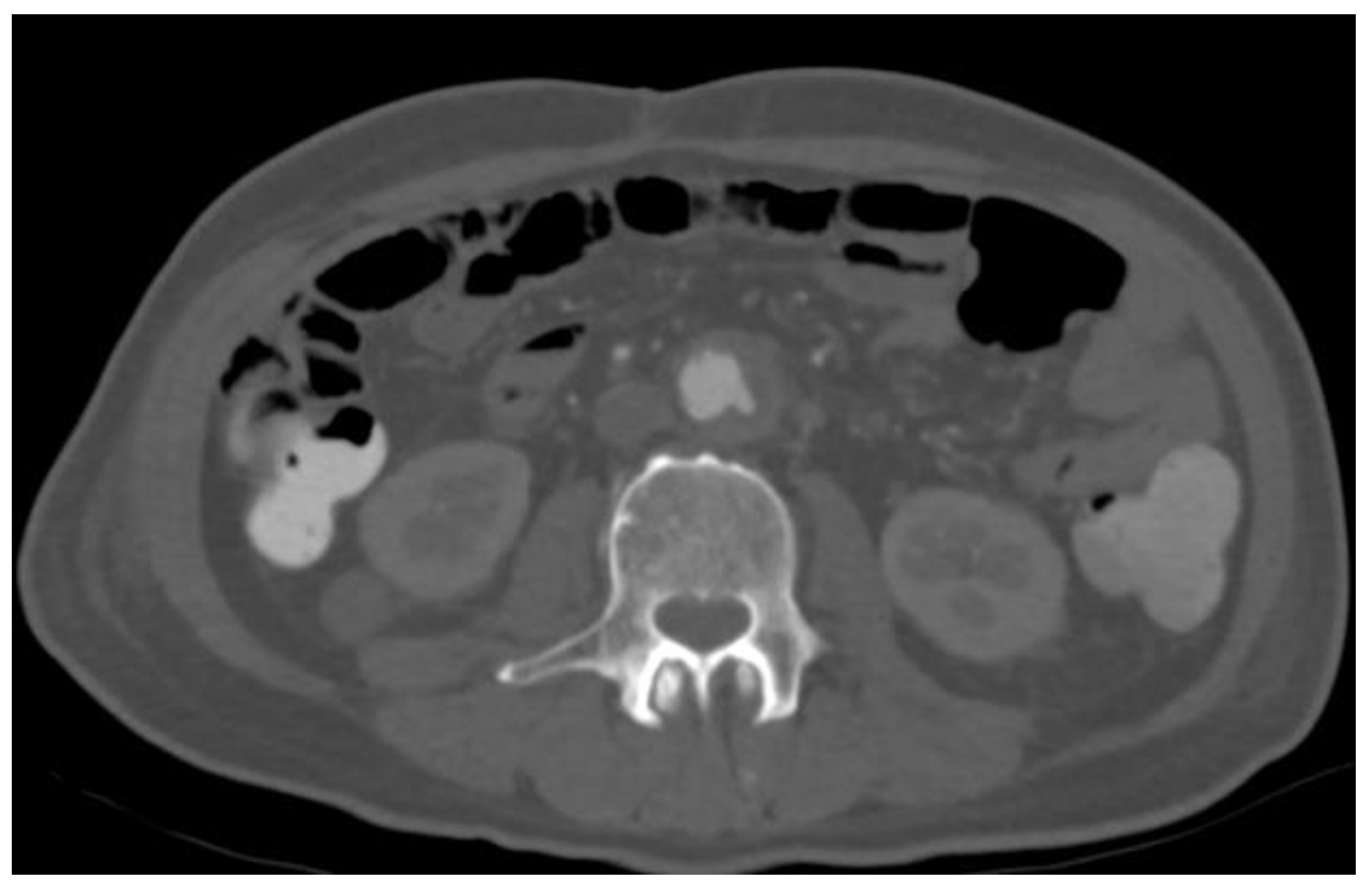
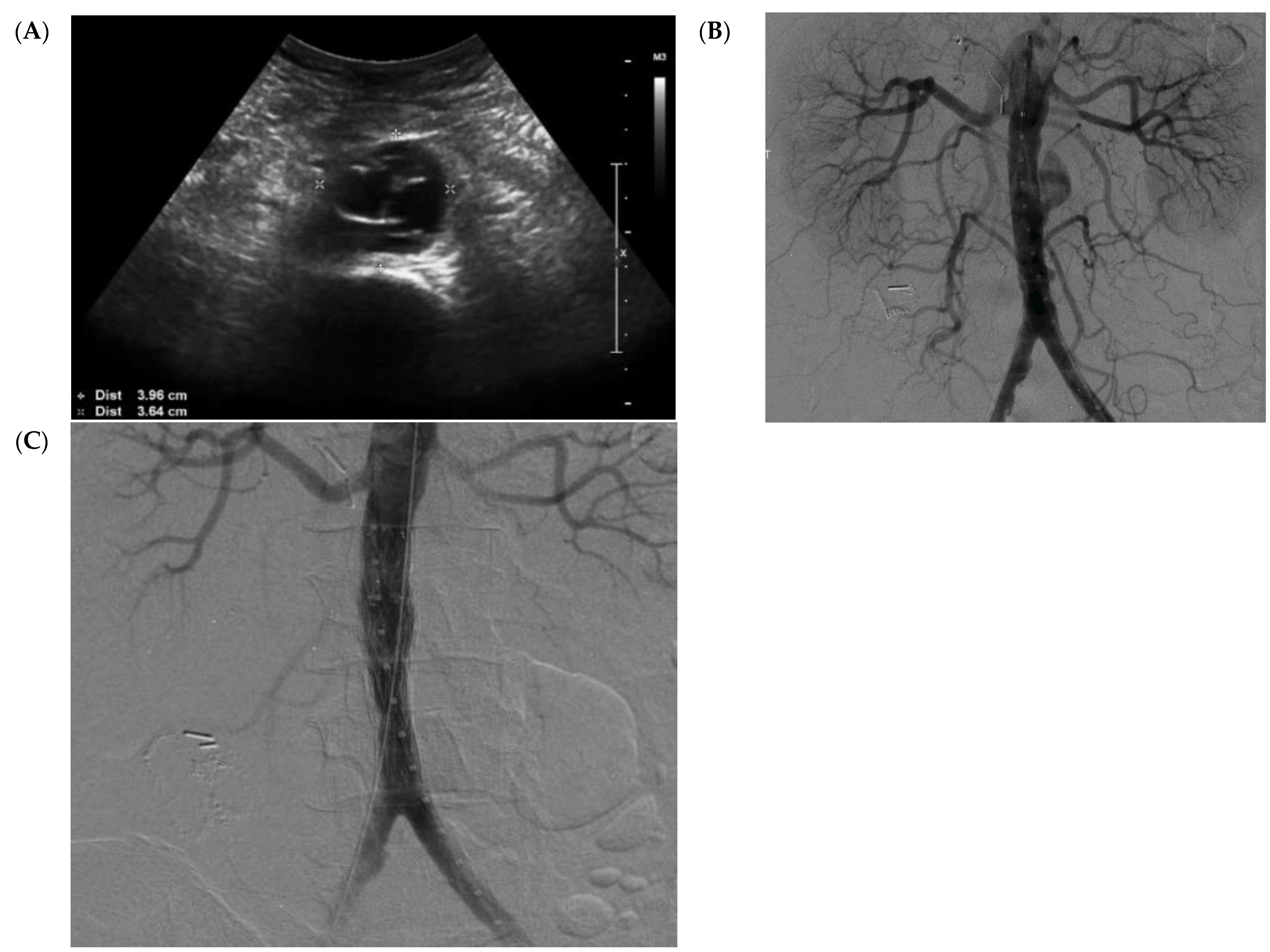
2. Case Report
3. Discussion
4. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Conflicts of Interest
References
- Zhu, N.; Zhang, D.; Wang, W.; Li, X.; Yang, B.; Song, J.; Zhao, X.; Huang, B.; Shi, W.; Lu, R. A novel coronavirus from patients with pneumonia in China, 2019. N. Engl. J. Med. 2020, 382, 727–733. [Google Scholar] [CrossRef] [PubMed]
- Wu, Z.; McGoogan, J.M. Characteristics of and important lessons from the coronavirus disease 2019 (COVID-19) outbreak in China: Summary of a report of 72,314 cases from the Chinese Center for Disease Control and Prevention. Jama 2020, 323, 1239–1242. [Google Scholar] [CrossRef] [PubMed]
- Dong, E.; Du, H.; Gardner, L. An interactive web-based dashboard to track COVID-19 in real time. Lancet Infect. Diseases 2020, 20, 533–534. [Google Scholar] [CrossRef]
- Sörelius, K.; Mani, K.; Björck, M.; Sedivy, P.; Wahlgren, C.-M.; Taylor, P.; Clough, R.E.; Lyons, O.; Thompson, M.; Brownrigg, J. Endovascular treatment of mycotic aortic aneurysms: A European multicenter study. Circulation 2014, 130, 2136–2142. [Google Scholar] [CrossRef] [PubMed]
- Müller, B.T.; Wegener, O.R.; Grabitz, K.; Pillny, M.; Thomas, L.; Sandmann, W. Mycotic aneurysms of the thoracic and abdominal aorta and iliac arteries: Experience with anatomic and extra-anatomic repair in 33 cases. J. Vasc. Surg. 2001, 33, 106–113. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Hsu, R.-B.; Chen, R.J.; Wang, S.-S.; Chu, S.-H. Infected aortic aneurysms: Clinical outcome and risk factor analysis. J. Vasc. Surg. 2004, 40, 30–35. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Weis-Müller, B.T.; Rascanu, C.; Sagban, A.; Grabitz, K.; Godehardt, E.; Sandmann, W. Single-center experience with open surgical treatment of 36 infected aneurysms of the thoracic, thoracoabdominal, and abdominal aorta. Ann. Vasc. Surg. 2011, 25, 1020–1025. [Google Scholar] [CrossRef] [PubMed]
- Shahi, N.; Kwon, J.J.; Arosemena, M.; Salvatore, D.M.; DiMuzio, P.J.; Abai, B. Endovascular repair of ruptured infected arteries as a temporizing measure versus destination therapy. Vasc. Endovasc. Surg. 2016, 50, 373–379. [Google Scholar] [CrossRef] [PubMed]
- Hennessey, H.; Luckham, E.; Kayssi, A.; Wheatcroft, M.D.; Greco, E.; Al-Omran, M.; Harlock, J.; Qadura, M. Optimization of rifampin coating on covered Dacron endovascular stent grafts for infected aortic aneurysms. J. Vasc. Surg. 2019, 69, 242–248.e241. [Google Scholar] [CrossRef] [PubMed]
- McDougal, E.G.; Burnham, S.J.; Johnson, G., Jr. Rifampin protection against experimental graft sepsis. J. Vasc. Surg. 1986, 4, 5–7. [Google Scholar] [CrossRef] [Green Version]
- Avramovic, J.; Fletcher, J. Rifampicin impregnation of a protein-sealed Dacron graft: An infection-resistant prosthetic vascular graft. Aust. N. Z. J. Surg. 1991, 61, 436–440. [Google Scholar] [CrossRef] [PubMed]
- Young, R.M.; Cherry, K.J., Jr.; Davis, P.M.; Gloviczki, P.; Bower, T.C.; Panneton, J.M.; Hallett, J.W., Jr. The results of in situ prosthetic replacement for infected aortic grafts. Am. J. Surg. 1999, 178, 136–140. [Google Scholar] [CrossRef]
- Osler, W. The Gulstonian lectures, on malignant endocarditis. Br. Med. J. 1885, 1, 522. [Google Scholar] [CrossRef] [PubMed]
- Sörelius, K.; Wanhainen, A.; Furebring, M.; Björck, M.; Gillgren, P.; Mani, K.; the Swedish Collaborator Group for Mycotic Abdominal Aortic Aneurysms; Lindström, D.; Hultgren, R.; Wahlgren, C.-M.; et al. Nationwide study of the treatment of mycotic abdominal aortic aneurysms comparing open and endovascular repair. Circulation 2016, 134, 1822–1832. [Google Scholar] [CrossRef] [PubMed]
- Kan, C.-D.; Lee, H.-L.; Yang, Y.-J. Outcome after endovascular stent graft treatment for mycotic aortic aneurysm: A systematic review. J. Vasc. Surg. 2007, 46, 906–912. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Sörelius, K.; Mani, K.; Björck, M.; Nyman, R.; Wanhainen, A. Endovascular repair of mycotic aortic aneurysms. J. Vasc. Surg. 2009, 50, 269–274. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Lew, W.K.; Rowe, V.L.; Cunningham, M.J.; Weaver, F.A. Endovascular management of mycotic aortic aneurysms and associated aortoaerodigestive fistulas. Ann. Vasc. Surg. 2009, 23, 81–89. [Google Scholar] [CrossRef] [PubMed]
- Sörelius, K.; Wanhainen, A.; Wahlgren, C.-M.; Langenskiöld, M.; Roos, H.; Resch, T.; Vaccarino, R.; Arvidsson, B.; Gillgren, P.; Bilos, L. Nationwide study on treatment of mycotic thoracic aortic aneurysms. Eur. J. Vasc. Endovasc. Surg. 2019, 57, 239–246. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Puppala, S.; Cuthbert, G.; Tingerides, C.; Russell, D.; McPherson, S. Endovascular management of mycotic aortic aneurysms-A 20-year experience from a single UK centre. Clin. Radiol. 2020, 75, 712.e13–712.e21. [Google Scholar] [CrossRef] [PubMed]


Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2021 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Syed, M.H.; Wheatcroft, M.; Marcuzzi, D.; Hennessey, H.; Qadura, M. Management of a Mycotic Aneurysm in a Patient with COVID-19: A Case Report. Medicina 2021, 57, 620. https://doi.org/10.3390/medicina57060620
Syed MH, Wheatcroft M, Marcuzzi D, Hennessey H, Qadura M. Management of a Mycotic Aneurysm in a Patient with COVID-19: A Case Report. Medicina. 2021; 57(6):620. https://doi.org/10.3390/medicina57060620
Chicago/Turabian StyleSyed, Muzammil H., Mark Wheatcroft, Danny Marcuzzi, Hooman Hennessey, and Mohammad Qadura. 2021. "Management of a Mycotic Aneurysm in a Patient with COVID-19: A Case Report" Medicina 57, no. 6: 620. https://doi.org/10.3390/medicina57060620
APA StyleSyed, M. H., Wheatcroft, M., Marcuzzi, D., Hennessey, H., & Qadura, M. (2021). Management of a Mycotic Aneurysm in a Patient with COVID-19: A Case Report. Medicina, 57(6), 620. https://doi.org/10.3390/medicina57060620







