Sodium Toxicity in the Nutritional Epidemiology and Nutritional Immunology of COVID-19
Abstract
1. Introduction
2. Current Perspective of Viral Infection
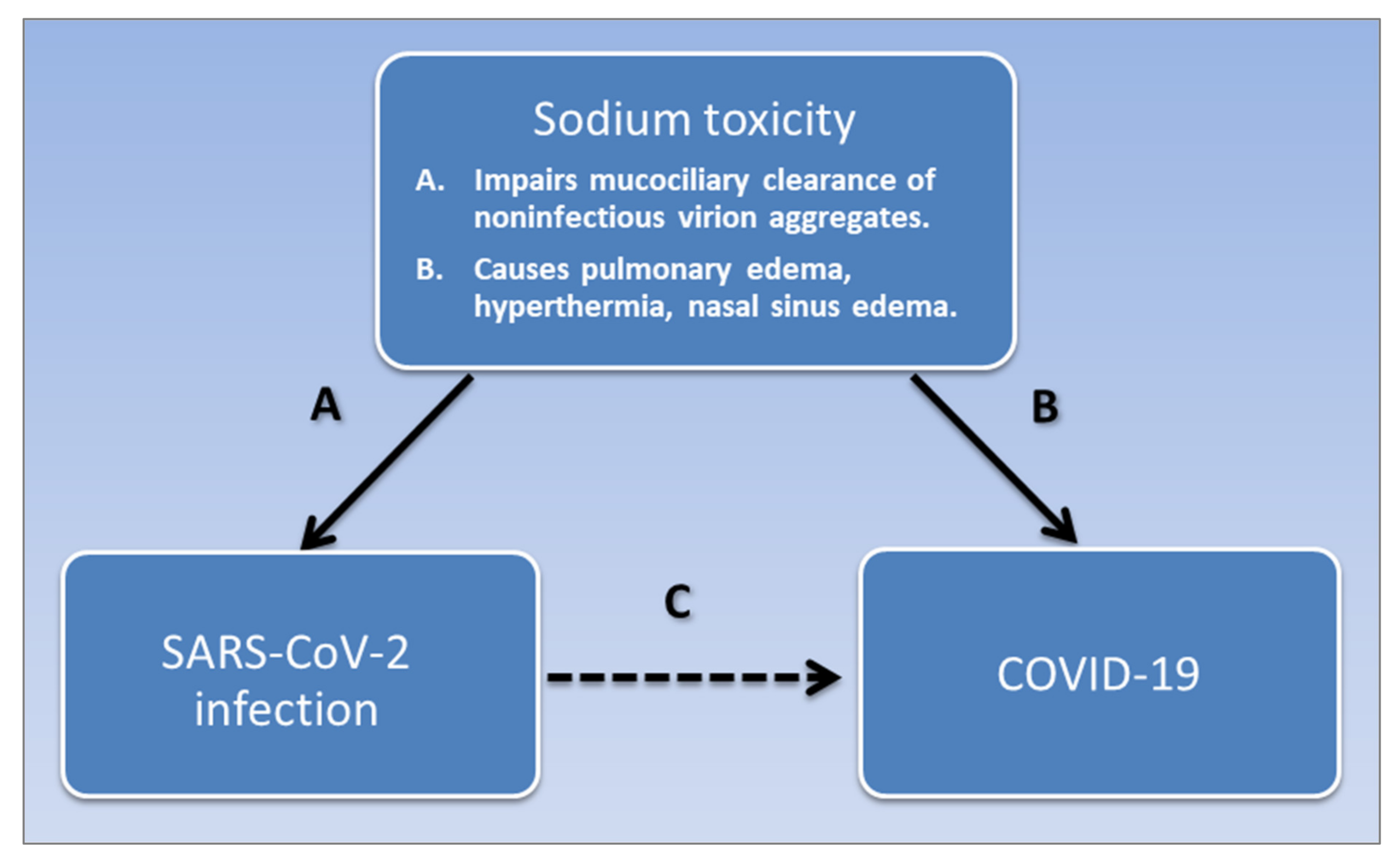
3. Risk Factors Associated with COVID-19
4. SARS-CoV-2 Infection and Sodium Toxicity
5. Sodium Toxicity and Immune Response in COVID-19
6. Sodium Toxicity and COVID-19 Symptoms
“…various neurohumoral responses to positive-pressure ventilation lead to retention of sodium and water, as a homeostatic response to raised intrathoracic pressure. A major consequence of this response is expanded plasma volume, and a tendency toward systemic and pulmonary edema [164].”
7. Determinants of Sodium Toxicity
“Our taxpayer-funded, government-run institutions focus on meeting legal nutritional guidelines for the lowest price… Many people facing illness or incarceration are without options or a voice. They are reduced to eating the most processed, least nutritious food available, entirely because it’s cheapest for the rest of us” [245].
8. Conclusions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Conflicts of Interest
References
- Cucinotta, D.; Vanelli, M. WHO Declares COVID-19 a Pandemic. Acta Bio-Med. Atenei Parm. 2020, 91, 157. [Google Scholar]
- Thigpen, C.L.; Funk, C. Most Americans Expect a COVID-19 Vaccine within a Year: 72% Say they would get vaccinated. Available online: https://www.pewresearch.org/fact-tank/2020/05/21/most-americans-expect-a-covid-19-vaccine-within-a-year-72-say-they-would-get-vaccinated/ (accessed on 21 May 2020).
- Glasziou, P.P.; Sanders, S.; Hoffmann, T. Waste in covid-19 research. BMJ 2020, 369, m1847. [Google Scholar] [CrossRef]
- Schrack, J.A.; Wanigatunga, A.A.; Juraschek, S.P. After the COVID-19 Pandemic: The Next Wave of Health Challenges for Older Adults. J. Gerontol. Ser. A 2020. [Google Scholar] [CrossRef] [PubMed]
- WHO. WHO Surveillance Case Definitions for ILI and SARI. Available online: https://www.who.int/influenza/surveillance_monitoring/ili_sari_surveillance_case_definition/en/ (accessed on 26 April 2020).
- Koene, R.J.; Prizment, A.E.; Blaes, A.; Konety, S.H. Shared risk factors in cardiovascular disease and cancer. Circulation 2016, 133, 1104–1114. [Google Scholar] [CrossRef] [PubMed]
- Mozaffarian, D.; Rosenberg, I.; Uauy, R. History of modern nutrition science—Implications for current research, dietary guidelines, and food policy. BMJ 2018, 361, k2392. [Google Scholar] [CrossRef] [PubMed]
- Kupiec, T.C.; Goldenring, J.M.; Raj, V. A non-fatal case of sodium toxicity. J. Anal. Toxicol. 2004, 28, 526–528. [Google Scholar] [CrossRef]
- Metheny, N.A.; Krieger, M.M. Salt Toxicity: A Systematic Review and Case Reports. J. Emerg. Nurs. 2020, 46, 428–439. [Google Scholar] [CrossRef]
- Afshin, A.; Sur, P.J.; Fay, K.A.; Cornaby, L.; Ferrara, G.; Salama, J.S.; Mullany, E.C.; Abate, K.H.; Abbafati, C.; Abebe, Z. Health effects of dietary risks in 195 countries, 1990–2017: A systematic analysis for the Global Burden of Disease Study 2017. Lancet 2019, 393, 1958–1972. [Google Scholar] [CrossRef]
- Zabetakis, I.; Lordan, R.; Norton, C.; Tsoupras, A. COVID-19: The Inflammation Link and the Role of Nutrition in Potential Mitigation. Nutrients 2020, 12, 1466. [Google Scholar] [CrossRef]
- Sun, J.; de Vos, P. Immunomodulatory functions of nutritional ingredients in health and disease. Front. Immunol. 2019, 10, 50. [Google Scholar] [CrossRef]
- WHO. Infections and Infectious Diseases: A Manual for Nurses and Midwives in the WHO European Region. Available online: https://www.euro.who.int/__data/assets/pdf_file/0013/102316/e79822.pdf (accessed on 5 October 2020).
- Esser, C.; Hochrath, K.; Schikowski, T.; Haarmann-Stemmann, T. COVID-19 research: Toxicological input urgently needed! Arch. Toxicol. 2020. [Google Scholar] [CrossRef]
- Wolfswinkel, J.F.; Furtmueller, E.; Wilderom, C.P.M. Using grounded theory as a method for rigorously reviewing literature. Eur. J. Inf. Syst. 2013, 22, 45–55. [Google Scholar] [CrossRef]
- Brown, R.B. Breakthrough knowledge synthesis in the Age of Google. Philosophies 2020, 5, 4. [Google Scholar] [CrossRef]
- Lodish, H.; Berk, A.; Zipursky, S.L.; Matsudaira, P.; Baltimore, D.; Darnell, J. Viruses: Structure, function, and uses. In Molecular Cell Biology, 4th ed.; WH Freeman: New York, NY, USA, 2000. [Google Scholar]
- Zou, S.; Caler, L.; Colombini-Hatch, S.; Glynn, S.; Srinivas, P. Research on the Human Virome: Where are We and What Is Next; Springer: Berlin/Heidelberg, Germany, 2016. [Google Scholar] [CrossRef]
- Delwart, E. Viruses of the Human Body: Some of Our Resident Viruses may be Beneficial. Available online: https://www.the-scientist.com/features/viruses-of-the-human-body-32614 (accessed on 25 May 2020).
- Kim, D.; Lee, J.-Y.; Yang, J.-S.; Kim, J.W.; Kim, V.N.; Chang, H. The architecture of SARS-CoV-2 transcriptome. Cell 2020, 181, 914–921. [Google Scholar] [CrossRef] [PubMed]
- Shokolenko, I.N.; Alexeyev, M.F. Mitochondrial DNA: A disposable genome? Biochim. Biophys. Acta Mol. Basis Dis. 2015, 1852, 1805–1809. [Google Scholar] [CrossRef]
- Bogenhagen, D.F. Mitochondrial DNA nucleoid structure. Biochim. Biophys. Acta Gene Regul. Mech. 2012, 1819, 914–920. [Google Scholar] [CrossRef] [PubMed]
- Cole, L.W. The evolution of per-cell organelle number. Front. Cell Dev. Biol. 2016, 4, 85. [Google Scholar] [CrossRef] [PubMed]
- Griswold, A. Genome packaging in prokaryotes: The circular chromosome of E. coli. Nat. Educ. 2008, 1, 57. [Google Scholar]
- Dance, A. How Cells Take out the Trash. Available online: https://www.nigms.nih.gov/education/Inside-Life-Science/Pages/How-Cells-Take-Out-the-Trash.aspx (accessed on 27 May 2020).
- Gerba, C.P.; Betancourt, W.Q. Viral aggregation: Impact on virus behavior in the environment. Environ. Sci. Technol. 2017, 51, 7318–7325. [Google Scholar] [CrossRef]
- Yuana, Y.; Sturk, A.; Nieuwland, R. Extracellular vesicles in physiological and pathological conditions. Blood Rev. 2013, 27, 31–39. [Google Scholar] [CrossRef]
- Nolte, E.; Cremer, T.; Gallo, R.C.; Margolis, L.B. Extracellular vesicles and viruses: Are they close relatives? Proc. Natl. Acad. Sci. USA 2016, 113, 9155–9161. [Google Scholar] [CrossRef]
- Cobb, M. Who discovered messenger RNA? Curr. Biol. 2015, 25, R526–R532. [Google Scholar] [CrossRef]
- Shyu, A.B.; Wilkinson, M.F.; Van Hoof, A. Messenger RNA regulation: To translate or to degrade. EMBO J. 2008, 27, 471–481. [Google Scholar] [CrossRef] [PubMed]
- Barchiesi, A.; Vascotto, C. Transcription, processing, and decay of mitochondrial RNA in health and disease. Int. J. Mol. Sci. 2019, 20, 2221. [Google Scholar] [CrossRef] [PubMed]
- Batagov, A.O.; Kurochkin, I.V. Exosomes secreted by human cells transport largely mRNA fragments that are enriched in the 3′-untranslated regions. Biol. Direct 2013, 8, 12. [Google Scholar] [CrossRef]
- Fenner, F.J.; White, D.O. Chapter 2—Virus Replication. In Fenner’s Veterinary Virology, 4th ed.; MacLachlan, N.J., Dubovi, E.J., Eds.; Academic Press: San Diego, CA, USA, 2011. [Google Scholar] [CrossRef]
- Brooke, C.B. Biological activities of ‘noninfectious’ influenza A virus particles. Future Virol. 2014, 9, 41–51. [Google Scholar] [CrossRef] [PubMed]
- Joynt, G.M.; Wu, W.K. Understanding COVID-19: What does viral RNA load really mean? Lancet Infect. Dis. 2020, 20, 635–636. [Google Scholar] [CrossRef]
- Sansone, P.; Savini, C.; Kurelac, I.; Chang, Q.; Amato, L.B.; Strillacci, A.; Stepanova, A.; Iommarini, L.; Mastroleo, C.; Daly, L. Packaging and transfer of mitochondrial DNA via exosomes regulate escape from dormancy in hormonal therapy-resistant breast cancer. Proc. Natl. Acad. Sci. USA 2017, 114, E9066–E9075. [Google Scholar] [CrossRef]
- Andreu-Moreno, I.; Sanjuán, R. Collective Viral Spread Mediated by Virion Aggregates Promotes the Evolution of Defective Interfering Particles. MBio 2020, 11, e02156-19. [Google Scholar] [CrossRef]
- Spriggs, C.C.; Harwood, M.C.; Tsai, B. How non-enveloped viruses hijack host machineries to cause infection. Adv. Virus Res. 2019, 104, 97–122. [Google Scholar] [CrossRef] [PubMed]
- Katsnelson, A. What do We Know about the Novel Coronavirus’s 29 proteins? Available online: https://cen.acs.org/biological-chemistry/infectious-disease/know-novel-coronaviruss-29-proteins/98/web/2020/04 (accessed on 12 July 2020).
- Atkinson, B.; Petersen, E. SARS-CoV-2 shedding and infectivity. Lancet 2020, 395, 1339–1340. [Google Scholar] [CrossRef]
- Noda, T.; Kawaoka, Y. Packaging of influenza virus genome: Robustness of selection. Proc. Natl. Acad. Sci. USA 2012, 109, 8797–8798. [Google Scholar] [CrossRef]
- Sanjuán, R.; Thoulouze, M.-I. Why viruses sometimes disperse in groups. Virus Evol. 2019, 5, vez014. [Google Scholar] [CrossRef] [PubMed]
- Iba, T.; Ogura, H. Role of extracellular vesicles in the development of sepsis-induced coagulopathy. J. Intensive Care 2018, 6, 68. [Google Scholar] [CrossRef] [PubMed]
- Li, H.; Liu, L.; Zhang, D.; Xu, J.; Dai, H.; Tang, N.; Su, X.; Cao, B. SARS-CoV-2 and viral sepsis: Observations and hypotheses. Lancet 2020, 395, 1517–1520. [Google Scholar] [CrossRef]
- Lin, G.-L.; McGinley, J.P.; Drysdale, S.B.; Pollard, A.J. Epidemiology and immune pathogenesis of viral sepsis. Front. Immunol. 2018, 9, 2147. [Google Scholar] [CrossRef]
- oie.int. Questions and Answers on COVID-19. Available online: https://www.oie.int/en/scientific-expertise/specific-information-and-recommendations/questions-and-answers-on-2019novel-coronavirus/ (accessed on 1 July 2020).
- Pan, L.; Mu, M.; Ren, H. Clinical characteristics of COVID-19 patients with digestive symptoms in Hubei, China: A descriptive, cross-sectional, multicenter study. Am. J. Gastroenterol. 2020. [Google Scholar] [CrossRef]
- Rothan, H.A.; Byrareddy, S.N. The epidemiology and pathogenesis of coronavirus disease (COVID-19) outbreak. J. Autoimmun. 2020, 109, 102433. [Google Scholar] [CrossRef]
- Kurpiers, L.A.; Schulte-Herbrüggen, B.; Ejotre, I.; Reeder, D.M. Bushmeat and emerging infectious diseases: Lessons from Africa. In Problematic Wildlife; Springer: Cham, Switzerland, 2016; pp. 507–551. [Google Scholar]
- Hu, B.; Zeng, L.-P.; Yang, X.-L.; Ge, X.-Y.; Zhang, W.; Li, B.; Xie, J.-Z.; Shen, X.-R.; Zhang, Y.-Z.; Wang, N. Discovery of a rich gene pool of bat SARS-related coronaviruses provides new insights into the origin of SARS coronavirus. PLoS Pathog. 2017, 13, e1006698. [Google Scholar] [CrossRef]
- Peng, A.W.; Juraschek, S.P.; Appel, L.J.; Miller, E.R.I.; Mueller, N.T. Effects of the DASH Diet and Sodium Intake on Bloating: Results From the DASH–Sodium Trial. Off. J. Am. Coll. Gastroenterol. 2019, 114, 1109–1115. [Google Scholar] [CrossRef]
- Moore, P.S. Pathogens and disease: Issues in determining causality. In The Infectious Etiology of Chronic Diseases: Defining the Relationship, Enhancing the Research, and Mitigating the Effects: Workshop Summary; National Academies Press: Washington, DC, USA, 2004; p. 140. [Google Scholar]
- WHO. “Immunity Passports” in the Context of COVID-19. Available online: https://www.who.int/news-room/commentaries/detail/immunity-passports-in-the-context-of-covid-19 (accessed on 26 April 2020).
- Cook, D.J.; Marshall, J.C.; Fowler, R.A. Critical Illness in Patients With COVID-19: Mounting an Effective Clinical and Research Response. JAMA 2020, 323, 1559–1560. [Google Scholar] [CrossRef]
- Barakat, A.; Ihazmad, H.; El Falaki, F.; Tempia, S.; Cherkaoui, I.; El Aouad, R. 2009 Pandemic influenza A virus subtype H1N1 in Morocco, 2009–2010: Epidemiology, transmissibility, and factors associated with fatal cases. J. Infect. Dis. 2012, 206, S94–S100. [Google Scholar] [CrossRef] [PubMed]
- Ji, H.; Gu, Q.; Chen, L.-L.; Xu, K.; Ling, X.; Bao, C.-J.; Tang, F.-Y.; Qi, X.; Wu, Y.-Q.; Ai, J. Epidemiological and clinical characteristics and risk factors for death of patients with avian influenza A H7N9 virus infection from Jiangsu Province, Eastern China. PLoS ONE 2014, 9, e89581. [Google Scholar] [CrossRef] [PubMed]
- Grillo, A.; Salvi, L.; Coruzzi, P.; Salvi, P.; Parati, G. Sodium intake and hypertension. Nutrients 2019, 11, 1970. [Google Scholar] [CrossRef] [PubMed]
- Tan, M.; He, F.J.; Wang, C.; MacGregor, G.A. Twenty-Four-Hour Urinary Sodium and Potassium Excretion in China: A Systematic Review and Meta-Analysis. J. Am. Heart Assoc. 2019, 8, e012923. [Google Scholar] [CrossRef]
- Lu, J.; Lu, Y.; Wang, X.; Li, X.; Linderman, G.C.; Wu, C.; Cheng, X.; Mu, L.; Zhang, H.; Liu, J. Prevalence, awareness, treatment, and control of hypertension in China: Data from 1· 7 million adults in a population-based screening study (China PEACE Million Persons Project). Lancet 2017, 390, 2549–2558. [Google Scholar] [CrossRef]
- Donfrancesco, C.; Lo Noce, C.; Russo, O.; Minutoli, D.; Di Lonardo, A.; Buttari, B.; Profumo, E.; Galeone, D.; Giampaoli, S.; Bellisario, P. Abstract P352: Trend of Salt Consumption in Italy from 2008 to 2018: Preliminary Results of the Cuore Project. Circulation 2020, 141, AP352. [Google Scholar] [CrossRef]
- Torlasco, C.; Faini, A.; Makil, E.; Bilo, G.; Pengo, M.; Beaney, T.; Xia, X.; Borghi, C.; Poulter, N.R.; Tocci, G. Nation-wide hypertension screening in Italy: Data from May Measurements Month 2017—Europe. Eur. Heart J. Suppl. 2019, 21, D66–D70. [Google Scholar] [CrossRef]
- Onder, G.; Rezza, G.; Brusaferro, S. Case-fatality rate and characteristics of patients dying in relation to COVID-19 in Italy. JAMA 2020, 323, 1775–1776. [Google Scholar] [CrossRef]
- Thout, S.R.; Santos, J.A.; McKenzie, B.; Trieu, K.; Johnson, C.; McLean, R.; Arcand, J.; Campbell, N.R.; Webster, J. The Science of Salt: Updating the evidence on global estimates of salt intake. J. Clin. Hypertens. 2019, 21, 710–721. [Google Scholar] [CrossRef]
- Mao, L.; Jin, H.; Wang, M.; Hu, Y.; Chen, S.; He, Q.; Chang, J.; Hong, C.; Zhou, Y.; Wang, D. Neurologic Manifestations of Hospitalized Patients with Coronavirus Disease 2019 in Wuhan, China. JAMA Neurol. 2020, 77, 683–690. [Google Scholar] [CrossRef]
- Magro, C.; Mulvey, J.J.; Berlin, D.; Nuovo, G.; Salvatore, S.; Harp, J.; Baxter-Stoltzfus, A.; Laurence, J. Complement associated microvascular injury and thrombosis in the pathogenesis of severe COVID-19 infection: A report of five cases. Transl. Res. 2020, 220, 1–13. [Google Scholar] [CrossRef] [PubMed]
- Bhatla, A.; Mayer, M.M.; Adusumalli, S.; Hyman, M.C.; Oh, E.; Tierney, A.; Moss, J.; Chahal, A.A.; Anesi, G.; Denduluri, S. COVID-19 and Cardiac Arrhythmias. Heart Rhythm 2020, 17, 1439–1444. [Google Scholar] [CrossRef]
- Madjid, M.; Safavi-Naeini, P.; Solomon, S.D.; Vardeny, O. Potential effects of coronaviruses on the cardiovascular system: A review. JAMA Cardiol. 2020, 5, 831–840. [Google Scholar] [CrossRef]
- Lighter, J.; Phillips, M.; Hochman, S.; Sterling, S.; Johnson, D.; Francois, F.; Stachel, A. Obesity in patients younger than 60 years is a risk factor for Covid-19 hospital admission. Clin. Infect. Dis. 2020, 71, 896–897. [Google Scholar] [CrossRef] [PubMed]
- Rubino, F.; Amiel, S.A.; Zimmet, P.; Alberti, G.; Bornstein, S.; Eckel, R.H.; Mingrone, G.; Boehm, B.; Cooper, M.E.; Chai, Z. New-Onset Diabetes in Covid-19. New Engl. J. Med. 2020, 383, 789–790. [Google Scholar] [CrossRef] [PubMed]
- Cheng, Y.; Luo, R.; Wang, K.; Zhang, M.; Wang, Z.; Dong, L.; Li, J.; Yao, Y.; Ge, S.; Xu, G. Kidney disease is associated with in-hospital death of patients with COVID-19. Kidney Int. 2020, 97, 829–838. [Google Scholar] [CrossRef] [PubMed]
- Wu, J.; Song, S.; Cao, H.-C.; Li, L.-J. Liver diseases in COVID-19: Etiology, treatment and prognosis. World J. Gastroenterol. 2020, 26, 2286. [Google Scholar] [CrossRef]
- Salter, A.; Fox, R.J.; Newsome, S.D.; Halper, J.; Li, D.K.; Kanellis, P.; Costello, K.; Bebo, B.; Rammohan, K.; Cutter, G.R. Outcomes and risk factors associated with SARS-CoV-2 Infection in a North American registry of patients with multiple sclerosis. JAMA Neurol. 2021, 78, 699–708. [Google Scholar] [CrossRef]
- Denton, C.P.; Campochiaro, C.; Bruni, C.; Distler, O.; Iagnocco, A.; Matucci Cerinic, M. COVID-19 and systemic sclerosis: Rising to the challenge of a pandemic. J. Scleroderma Relat. Disord. 2020, 6, 58–65. [Google Scholar] [CrossRef]
- Sampaio Rocha-Filho, P.A.; Magalhães, J.E. Headache associated with COVID-19: Frequency, characteristics and association with anosmia and ageusia. Cephalalgia 2020, 40, 1443–1451. [Google Scholar] [CrossRef]
- Almufarrij, I.; Munro, K.J. One year on: An updated systematic review of SARS-CoV-2, COVID-19 and audio-vestibular symptoms. Int. J. Audiol. 2021, 1–11. [Google Scholar] [CrossRef] [PubMed]
- Lima, M.A.; Silva, M.T.T.; Soares, C.N.; Coutinho, R.; Oliveira, H.S.; Afonso, L.; Espíndola, O.; Leite, A.C.; Araujo, A. Peripheral facial nerve palsy associated with COVID-19. J. Neurovirol. 2020, 26, 941–944. [Google Scholar] [CrossRef] [PubMed]
- Subramanian, A.; Anand, A.; Adderley, N.J.; Okoth, K.; Toulis, K.A.; Gokhale, K.; Sainsbury, C.; O’Reilly, M.W.; Arlt, W.; Nirantharakumar, K. Increased COVID-19 infections in women with polycystic ovary syndrome: A population-based study. Eur. J. Endocrinol. 2021, 184, 637–645. [Google Scholar] [CrossRef] [PubMed]
- Wang, D.; Hu, B.; Hu, C.; Zhu, F.; Liu, X.; Zhang, J.; Wang, B.; Xiang, H.; Cheng, Z.; Xiong, Y. Clinical characteristics of 138 hospitalized patients with 2019 novel coronavirus–infected pneumonia in Wuhan, China. JAMA 2020, 323, 1061–1069. [Google Scholar] [CrossRef] [PubMed]
- Li, Q. An outbreak of NCIP (2019-nCoV) infection in China—Wuhan, Hubei province, 2019−2020. China CDC Wkly. 2020, 2, 79–80. [Google Scholar] [CrossRef]
- Schmidt-Pogoda, A.; Strecker, J.-K.; Liebmann, M.; Massoth, C.; Beuker, C.; Hansen, U.; König, S.; Albrecht, S.; Bock, S.; Breuer, J. Dietary salt promotes ischemic brain injury and is associated with parenchymal migrasome formation. PLoS ONE 2018, 13, e0209871. [Google Scholar] [CrossRef]
- Dmitrieva, N.I.; Burg, M.B. Secretion of von Willebrand factor by endothelial cells links sodium to hypercoagulability and thrombosis. Proc. Natl. Acad. Sci. USA 2014, 111, 6485–6490. [Google Scholar] [CrossRef]
- Pääkkö, T.J.W.; Perkiömäki, J.S.; Silaste, M.-L.; Bloigu, R.; Huikuri, H.V.; Antero Kesäniemi, Y.; Ukkola, O.H. Dietary sodium intake is associated with long-term risk of new-onset atrial fibrillation. Ann. Med. 2018, 50, 694–703. [Google Scholar] [CrossRef]
- He, M.; Mu, J.; Liu, F.; Ren, K.; Wang, Y.; Guo, T.; Wang, D. Effects of a high salt intake and potassium supplementation on QT interval dispersion in normotensive healthy subjects. Intern. Med. 2015, 54, 295–301. [Google Scholar] [CrossRef][Green Version]
- Zhou, L.; Stamler, J.; Chan, Q.; Van Horn, L.; Daviglus, M.L.; Dyer, A.R.; Miura, K.; Okuda, N.; Wu, Y.; Ueshima, H. Salt intake and prevalence of overweight/obesity in Japan, China, the United Kingdom, and the United States: The INTERMAP Study. Am. J. Clin. Nutr. 2019, 110, 34–40. [Google Scholar] [CrossRef]
- ScienceDaily.com. Sodium (Salt) Intake is Associated with a Risk of Developing Type 2 Diabetes. Available online: https://www.sciencedaily.com/releases/2017/09/170914210621.htm (accessed on 20 July 2020).
- Maruta, Y.; Hasegawa, T.; Yamakoshi, E.; Nishiwaki, H.; Koiwa, F.; Imai, E.; Hishida, A. Association between serum Na–Cl level and renal function decline in chronic kidney disease: Results from the chronic kidney disease Japan cohort (CKD-JAC) study. Clin. Exp. Nephrol. 2019, 23, 215–222. [Google Scholar] [CrossRef]
- Wang, G.; Yeung, C.-K.; Wong, W.-Y.; Zhang, N.; Wei, Y.-F.; Zhang, J.-L.; Yan, Y.; Wong, C.-Y.; Tang, J.-J.; Chuai, M. Liver fibrosis can be induced by high salt intake through excess reactive oxygen species (ROS) production. J. Agric. Food Chem. 2016, 64, 1610–1617. [Google Scholar] [CrossRef]
- Zostawa, J.; Adamczyk, J.; Sowa, P.; Adamczyk-Sowa, M. The influence of sodium on pathophysiology of multiple sclerosis. Neurol. Sci. 2017, 38, 389–398. [Google Scholar] [CrossRef]
- Kopp, C.; Beyer, C.; Linz, P.; Dahlmann, A.; Hammon, M.; Jantsch, J.; Neubert, P.; Rosenhauer, D.; Müller, D.N.; Cavallaro, A. Na+ deposition in the fibrotic skin of systemic sclerosis patients detected by 23Na-magnetic resonance imaging. Rheumatology 2017, 56, 556–560. [Google Scholar] [CrossRef]
- Ghaffari, H.; Grant, S.C.; Petzold, L.R.; Harrington, M.G. Regulation of CSF and brain tissue sodium levels by the blood-CSF and blood-brain barriers during migraine. Front. Comput. Neurosci. 2020, 14, 4. [Google Scholar] [CrossRef]
- Henry, J.A.; Zaugg, T.L.; Myers, P.J.; Kendall, C.J.; Michaelides, E.M. A triage guide for tinnitus. J. Fam. Pract. 2010, 59, 389. [Google Scholar]
- Sardana, D.; Bahadur, S. Effect of compression in the etiology of experimental Bell’s palsy. Indian J. Otolaryngol. Head Neck Surg. 1979, 31, 61. [Google Scholar]
- Shishehgar, F.; Ramezani Tehrani, F.; Mirmiran, P.; Hajian, S.; Baghestani, A.R.; Moslehi, N. Comparison of Dietary Intake between Polycystic Ovary Syndrome Women and Controls. Glob. J. Health Sci. 2016, 8, 54801. [Google Scholar] [CrossRef]
- Wilder, T.; Drake, T. Metabolism of chloride and total fixed base in pneumonia and the relation to salt and water retention. J. Clin. Investig. 1929, 7, 353–364. [Google Scholar] [CrossRef]
- cdc.gov. Multisystem Inflammatory Syndrome in Children (MIS-C) Associated with Coronavirus Disease 2019 (COVID-19). Available online: https://emergency.cdc.gov/han/2020/han00432.asp (accessed on 30 May 2020).
- Sayyahfar, S.; Hoseini, R. Kawasaki Disease and Hypertension in an Infant. Arch. Pediatric Infect. Dis. 2017, 5. [Google Scholar] [CrossRef]
- Prangwatanagul, W.; Limsuwan, A. Ischemic stroke in Kawasaki disease. Pediatrics Int. 2017, 59, 92–96. [Google Scholar] [CrossRef]
- Belhadjer, Z.; Méot, M.; Bajolle, F.; Khraiche, D.; Legendre, A.; Abakka, S.; Auriau, J.; Grimaud, M.; Oualha, M.; Beghetti, M. Acute heart failure in multisystem inflammatory syndrome in children (MIS-C) in the context of global SARS-CoV-2 pandemic. Circulation 2020, 142, 429–436. [Google Scholar] [CrossRef] [PubMed]
- Chuang, G.-T.; Tsai, I.-J.; Lin, M.-T.; Chang, L.-Y. Acute kidney injury in patients with Kawasaki disease. Pediatric Res. 2016, 80, 224–227. [Google Scholar] [CrossRef]
- NHLBI. Implementing Recommendations for Dietary Salt Reduction: Where Are We? Where Are We Going? How Do We Get There? A Summary of an NHLBI Workshop; National Institutes of Health, National Heart, Lung, and Blood Institute: Bethesda, MD, USA, 1996. [Google Scholar]
- hsph.harvard.edu. Salt and Sodium. Available online: https://www.hsph.harvard.edu/nutritionsource/salt-and-sodium/ (accessed on 4 June 2020).
- Bommaraju, T.V.; Orosz, P.J.; Sokol, E.A. Brine Electrolysis. Available online: https://knowledge.electrochem.org/encycl/art-b01-brine.htm (accessed on 6 June 2020).
- Roux, B. Ion channels and ion selectivity. Essays Biochem. 2017, 61, 201–209. [Google Scholar] [CrossRef]
- sciencemediacentre.org. Expert Reaction to Study Looking at Salt Consumption and Health Risks. Available online: https://www.sciencemediacentre.org/expert-reaction-to-study-looking-at-salt-consumption-and-health-risks/ (accessed on 4 June 2020).
- Johnston, I. Lancet Attacked for Publishing Study Claiming Low-Salt Diet Could Kill You. Available online: https://www.independent.co.uk/news/science/salt-diet-heart-disease-death-lancet-a7040546.html (accessed on 4 June 2020).
- Yeates, K.E.; Singer, M.; Morton, A.R. Salt and water: A simple approach to hyponatremia. CMAJ 2004, 170, 365–369. [Google Scholar]
- Fortune, B.E.; Garcia-Tsao, G. Hypervolemic hyponatremia: Clinical significance and management. Clin. Liver Dis. 2013, 2, 109. [Google Scholar] [CrossRef]
- Braun, M.M.; Barstow, C.; Pyzocha, N. Diagnosis and management of sodium disorders: Hyponatremia and hypernatremia. Am. Fam. Physician 2015, 91, 299–307. [Google Scholar] [PubMed]
- Frontera, J.A.; Valdes, E.; Huang, J.; Lewis, A.; Lord, A.S.; Zhou, T.; Kahn, D.E.; Melmed, K.; Czeisler, B.M.; Yaghi, S. Prevalence and impact of hyponatremia in patients with coronavirus disease 2019 in New York City. Crit. Care Med. 2020. [Google Scholar] [CrossRef] [PubMed]
- Tezcan, M.E.; Gokce, G.D.; Sen, N.; Kaymak, N.Z.; Ozer, R. Baseline electrolyte abnormalities would be related to poor prognosis in hospitalized coronavirus disease 2019 patients. N. Microbes N. Infect. 2020, 37, 100753. [Google Scholar] [CrossRef]
- Torres-Macho, J.; Ryan, P.; Valencia, J.; Pérez-Butragueño, M.; Jiménez, E.; Fontán-Vela, M.; Izquierdo-García, E.; Fernandez-Jimenez, I.; Álvaro-Alonso, E.; Lazaro, A. The PANDEMYC Score. An Easily Applicable and Interpretable Model for Predicting Mortality Associated with COVID-19. J. Clin. Med. 2020, 9, 3066. [Google Scholar] [CrossRef]
- Berni, A.; Malandrino, D.; Parenti, G.; Maggi, M.; Poggesi, L.; Peri, A. Hyponatremia, IL-6, and SARS-CoV-2 (COVID-19) infection: May all fit together? J. Endocrinol. Investig. 2020, 43, 1137–1139. [Google Scholar] [CrossRef]
- Corona, G.; Giuliani, C.; Parenti, G.; Norello, D.; Verbalis, J.G.; Forti, G.; Maggi, M.; Peri, A. Moderate hyponatremia is associated with increased risk of mortality: Evidence from a meta-analysis. PLoS ONE 2013, 8, e80451. [Google Scholar] [CrossRef]
- Christ-Crain, M.; Hoorn, E.J.; Sherlock, M.; Thompson, C.J.; Wass, J.A. Endocrinology in the time of COVID-19: Management of diabetes insipidus and hyponatraemia. Eur. J. Endocrinol. 2020, 183, G9–G15. [Google Scholar] [CrossRef]
- Hu, W.; Li, C.; Xu, Y.; Qi, Y.; Zhang, Z.; Li, M.; Cai, F.; Liu, D.; Yue, J.; Ye, M. Disorders of sodium balance and its clinical implications in COVID-19 patients: A multicenter retrospective study. Intern. Emerg. Med. 2021, 16, 853–862. [Google Scholar] [CrossRef]
- Post, A.; Dullaart, R.P.; Bakker, S.J. Sodium status and kidney involvement during COVID-19 infection. Virus Res. 2020, 286, 198034. [Google Scholar] [CrossRef]
- Post, A.; Dullaart, R.P.; Bakker, S.J. Is low sodium intake a risk factor for severe and fatal COVID-19 infection? Eur. J. Intern. Med. 2020, 75, 109. [Google Scholar] [CrossRef]
- Lippi, G.; South, A.M.; Henry, B.M. Electrolyte imbalances in patients with severe coronavirus disease 2019 (COVID-19). Ann. Clin. Biochem. 2020, 57, 262–265. [Google Scholar] [CrossRef]
- Królicka, A.L.; Kruczkowska, A.; Krajewska, M.; Kusztal, M.A. Hyponatremia in Infectious Diseases—A Literature Review. Int. J. Environ. Res. Public Health 2020, 17, 5320. [Google Scholar] [CrossRef]
- Yang, M.-W.; Chen, F.; Zhu, D.-J.; Li, J.-Z.; Zhu, J.-L.; Zeng, W.; Qu, S.-L.; Zhang, Y. Clinical efficacy of Matrine and Sodium Chloride Injection in treatment of 40 cases of COVID-19. Zhongguo Zhong Yao Za Zhi. 2020, 45, 2221–2231. [Google Scholar]
- Thomas, C.P.; Batuman, V. Syndrome of Inappropriate Antidiuretic Hormone Secretion. Available online: https://emedicine.medscape.com/article/246650-overview (accessed on 22 June 2021).
- Sugiura, T.; Takase, H.; Ohte, N.; Dohi, Y. Dietary salt intake is a significant determinant of impaired kidney function in the general population. Kidney Blood Press. Res. 2018, 43, 1245–1254. [Google Scholar] [CrossRef]
- Oppelaar, J.J.; Vogt, L. Body Fluid-Independent Effects of Dietary Salt Consumption in Chronic Kidney Disease. Nutrients 2019, 11, 2779. [Google Scholar] [CrossRef]
- dietaryguidelines.gov. Dietary Guidelines for Americans 2020–2025. Available online: https://www.dietaryguidelines.gov/sites/default/files/2020-12/Dietary_Guidelines_for_Americans_2020-2025.pdf (accessed on 23 June 2021).
- Campbell, N.R.; Train, E.J. A systematic review of fatalities related to acute ingestion of salt. A need for warning labels? Nutrients 2017, 9, 648. [Google Scholar] [CrossRef]
- Ma, J.; Strub, P.; Lv, N.; Xiao, L.; Camargo, C.A.; Buist, A.S.; Lavori, P.W.; Wilson, S.R.; Nadeau, K.C.; Rosas, L.G. Pilot randomised trial of a healthy eating behavioural intervention in uncontrolled asthma. Eur. Respir. J. 2016, 47, 122–132. [Google Scholar] [CrossRef] [PubMed]
- Suadicani, P.; Hein, H.O.; Gyntelberg, F. High salt intake and risk of chronic bronchitis: The Copenhagen Male Study—A 10-year followup. ISRN Pulmonol. 2011, 2011, 257979. [Google Scholar] [CrossRef]
- Newton, A.H.; Cardani, A.; Braciale, T.J. The host immune response in respiratory virus infection: Balancing virus clearance and immunopathology. Semin. Immunopathol. 2016, 38, 471–482. [Google Scholar] [CrossRef]
- Chace, K.V.; Naziruddin, B.; Desai, V.C.; Flux, M.; Sachdev, G.P. Physical properties of purified human respiratory mucus glycoproteins: Effects of sodium chloride concentration on the aggregation properties and shape. Exp. Lung Res. 1989, 15, 721–737. [Google Scholar] [CrossRef] [PubMed]
- Fu, Y.; Tong, J.; Meng, F.; Hoeltig, D.; Liu, G.; Yin, X.; Herrler, G. Ciliostasis of airway epithelial cells facilitates influenza A virus infection. Vet. Res. 2018, 49, 65. [Google Scholar] [CrossRef]
- Centers for Disease Control and Prevention. Interim Guidelines for Collecting, Handling, and Testing Clinical Specimens from Persons for Coronavirus Disease 2019 (COVID-19). Available online: https://www.cdc.gov/coronavirus/2019-ncov/lab/guidelines-clinical-specimens.html (accessed on 26 April 2020).
- Koparal, M.; Kurt, E.; Altuntas, E.E.; Dogan, F. Assessment of mucociliary clearance as an indicator of nasal function in patients with COVID-19: A cross-sectional study. Eur Arch. Otorhinolaryngol. 2021, 278, 1863–1868. [Google Scholar] [CrossRef] [PubMed]
- De Freitas, G.; Gudur, A.; Vela-Ortiz, M.; Jodelka, J.; Livert, D.; Krishnamurthy, M. Where there is sodium there may be sepsis. J. Commun. Hosp. Intern. Med. Perspect. 2019, 9, 296–299. [Google Scholar] [CrossRef]
- Cereda, D.; Tirani, M.; Rovida, F.; Demicheli, V.; Ajelli, M.; Poletti, P.; Merler, S. The early phase of the COVID-19 outbreak in Lombardy, Italy. arXiv 2020, arXiv:2003.09320. [Google Scholar]
- He, X.; Lau, E.H.; Wu, P.; Deng, X.; Wang, J.; Hao, X.; Lau, Y.C.; Wong, J.Y.; Guan, Y.; Tan, X. Temporal dynamics in viral shedding and transmissibility of COVID-19. Nat. Med. 2020, 26, 672–675. [Google Scholar] [CrossRef] [PubMed]
- Oran, D.P.; Topol, E.J. Prevalence of asymptomatic SARS-CoV-2 infection: A narrative review. Ann. Intern. Med. 2020, 173, 362–367. [Google Scholar] [CrossRef]
- Nalbandian, A.; Sehgal, K.; Gupta, A.; Madhavan, M.V.; McGroder, C.; Stevens, J.S.; Cook, J.R.; Nordvig, A.S.; Shalev, D.; Sehrawat, T.S. Post-acute COVID-19 syndrome. Nat. Med. 2021, 27, 601–615. [Google Scholar] [CrossRef]
- Liu, Y.; Yan, L.-M.; Wan, L.; Xiang, T.-X.; Le, A.; Liu, J.-M.; Peiris, M.; Poon, L.L.; Zhang, W. Viral dynamics in mild and severe cases of COVID-19. Lancet Infect. Dis. 2020, 20, 656–657. [Google Scholar] [CrossRef]
- webmd.com. Are Warnings Against NSAIDs in COVID-19 Warranted? Available online: https://www.webmd.com/lung/news/20200318/coronavirus-nsaids-experts (accessed on 24 July 2020).
- Yasir, M.; Goyal, A.; Bansal, P.; Sonthalia, S. Corticosteroid Adverse Effects. Available online: https://www.ncbi.nlm.nih.gov/books/NBK531462/ (accessed on 24 July 2020).
- Kim, S.; Joo, K.W. Electrolyte and acid-base disturbances associated with non-steroidal anti-inflammatory drugs. Electrolytes Blood Press. 2007, 5, 116. [Google Scholar] [CrossRef]
- Afsar, B.; Kuwabara, M.; Ortiz, A.; Yerlikaya, A.; Siriopol, D.; Covic, A.; Rodriguez-Iturbe, B.; Johnson, R.J.; Kanbay, M. Salt intake and immunity. Hypertension 2018, 72, 19–23. [Google Scholar] [CrossRef]
- Matthias, J.; Maul, J.; Noster, R.; Meinl, H.; Chao, Y.-Y.; Gerstenberg, H.; Jeschke, F.; Gasparoni, G.; Welle, A.; Walter, J. Sodium chloride is an ionic checkpoint for human TH2 cells and shapes the atopic skin microenvironment. Sci. Transl. Med. 2019, 11. [Google Scholar] [CrossRef]
- Wu, C.; Yosef, N.; Thalhamer, T.; Zhu, C.; Xiao, S.; Kishi, Y.; Regev, A.; Kuchroo, V.K. Induction of pathogenic T H 17 cells by inducible salt-sensing kinase SGK1. Nature 2013, 496, 513–517. [Google Scholar] [CrossRef]
- Jantsch, J.; Schatz, V.; Friedrich, D.; Schröder, A.; Kopp, C.; Siegert, I.; Maronna, A.; Wendelborn, D.; Linz, P.; Binger, K.J. Cutaneous Na+ storage strengthens the antimicrobial barrier function of the skin and boosts macrophage-driven host defense. Cell Metab. 2015, 21, 493–501. [Google Scholar] [CrossRef]
- Min, B.; Fairchild, R.L. Over-salting ruins the balance of the immune menu. J. Clin. Investig. 2015, 125, 4002–4004. [Google Scholar] [CrossRef]
- Vabret, N.; Britton, G.J.; Gruber, C.; Hegde, S.; Kim, J.; Kuksin, M.; Levantovsky, R.; Malle, L.; Moreira, A.; Park, M.D. Immunology of COVID-19: Current state of the science. Immunity 2020, 52, 910–941. [Google Scholar] [CrossRef]
- Rubins, J.B. Alveolar macrophages: Wielding the double-edged sword of inflammation. Am. J. Respir. Crit. Care Med. 2003, 167, 103–104. [Google Scholar] [CrossRef] [PubMed]
- Berger, R.C.M.; Vassallo, P.F.; de Oliveira Crajoinas, R.; Oliveira, M.L.; Martins, F.L.; Nogueira, B.V.; Motta-Santos, D.; Araújo, I.B.; Forechi, L.; Girardi, A.C.C. Renal effects and underlying molecular mechanisms of long-term salt content diets in spontaneously hypertensive rats. PLoS ONE 2015, 10, e0141288. [Google Scholar] [CrossRef] [PubMed]
- Richmond, C. David Tyrrell. BMJ 2005, 330, 1451. [Google Scholar]
- Cole, D. New COVID Variants have Changed the Game, and Vaccines will not be Enough. We Need Global ‘Maximum Suppression’. Available online: https://theconversation.com/new-covid-variants-have-changed-the-game-and-vaccines-will-not-be-enough-we-need-global-maximum-suppression-157870 (accessed on 4 May 2021).
- World Health Organization. Q&A on Coronaviruses (COVID-19). Available online: https://www.who.int/news-room/q-a-detail/q-a-coronaviruses (accessed on 26 April 2020).
- Aucott, J.N.; Rebman, A.W. Long-haul COVID: Heed the lessons from other infection-triggered illnesses. Lancet 2021, 397, 967–968. [Google Scholar] [CrossRef]
- Hutchin, P.; Terzi, R.; Hollandsworth, L.; Johnson, G., Jr.; Peters, R. Pulmonary congestion following infusion of large fluid loads in thoracic surgical patients. Ann. Thorac. Surg. 1969, 8, 339–347. [Google Scholar] [CrossRef]
- Moon, R.E.; Long, R.J. Drowning and near-drowning. Emerg. Med. 2002, 14, 377–386. [Google Scholar] [CrossRef]
- Cozzi, D.; Cavigli, E.; Moroni, C.; Smorchkova, O.; Zantonelli, G.; Pradella, S.; Miele, V. Ground-glass opacity (GGO): A review of the differential diagnosis in the era of COVID-19. Jpn. J. Radiol. 2021, 1–12. [Google Scholar] [CrossRef]
- Licker, M.; Triponez, F.; Ellenberger, C.; Karenovics, W. Fluid therapy in thoracic surgery: A zero-balance target is always best! Turk. J. Anaesthesiol. Reanim. 2016, 44, 227. [Google Scholar] [CrossRef]
- Casas-Aparicio, G.A.; León-Rodríguez, I.; de Jesus Hernandez-Zenteno, R.; Castillejos-López, M.; Alvarado-de la Barrera, C.; Ormsby, C.E.; Reyes-Terán, G. Aggressive fluid accumulation is associated with acute kidney injury and mortality in a cohort of patients with severe pneumonia caused by influenza A H1N1 virus. PLoS ONE 2018, 13, e0192592. [Google Scholar] [CrossRef] [PubMed]
- Azzam, Z.S.; Sznajder, J.I. Lung edema clearance: Relevance to patients with lung injury. Rambam Maimonides Med. J. 2015, 6. [Google Scholar] [CrossRef]
- Elton, N.W.; Elton, W.J.; Nazareno, J.P. Pathology of acute salt poisoning in infants. Am. J. Clin. Pathol. 1963, 39, 252–264. [Google Scholar] [CrossRef]
- Zhou, F.; Yu, T.; Du, R.; Fan, G.; Liu, Y.; Liu, Z.; Xiang, J.; Wang, Y.; Song, B.; Gu, X. Clinical course and risk factors for mortality of adult inpatients with COVID-19 in Wuhan, China: A retrospective cohort study. Lancet 2020, 395, 1054–1062. [Google Scholar] [CrossRef]
- mayoclinic.org. ARDS. Mayo Foundation for Medical Education and Research. Available online: https://www.mayoclinic.org/diseases-conditions/ards/symptoms-causes/syc-20355576?p=1 (accessed on 26 April 2020).
- Gattinoni, L.; Coppola, S.; Cressoni, M.; Busana, M.; Chiumello, D. Covid-19 does not lead to a “typical” acute respiratory distress syndrome. Am. J. Respir. Crit. Care Med. 2020, 201, 1299–1300. [Google Scholar] [CrossRef] [PubMed]
- Bersten, A.D. Chapter 65. Fluid Management in the Ventilated Patient. In Principles and Practice of Mechanical Ventilation, 3rd ed.; Tobin, M.J., Ed.; The McGraw-Hill Companies: New York, NY, USA, 2013. [Google Scholar]
- Begley, S. With Ventilators Running Out, Doctors Say the Machines are Overused for Covid-19. statnews.com. Available online: https://www.statnews.com/2020/04/08/doctors-say-ventilators-overused-for-covid-19/ (accessed on 26 April 2020).
- Cummings, M.J.; Baldwin, M.R.; Abrams, D.; Jacobson, S.D.; Meyer, B.J.; Balough, E.M.; Aaron, J.G.; Claassen, J.; Rabbani, L.E.; Hastie, J. Epidemiology, clinical course, and outcomes of critically ill adults with COVID-19 in New York City: A prospective cohort study. Lancet 2020, 395, 1763–1770. [Google Scholar] [CrossRef]
- Carter, C.; Aedy, H.; Notter, J. COVID-19 disease: Non-Invasive Ventilation and high frequency nasal oxygenation. Clin. Integr. Care 2020, 1, 100006. [Google Scholar] [CrossRef]
- Carlson, R.W.; Schaeffer, R.C., Jr.; Michaels, S.G.; Weil, M. Pulmonary edema fluid. Spectrum of features in 37 patients. Circulation 1979, 60, 1161–1169. [Google Scholar] [CrossRef]
- Aydin, E.A.; Demir, S.; Aydin, O.; Bilginer, Y.; Ozen, S. Pleural effusion as an atypical presentation of Kawasaki disease: A case report and review of the literature. J. Med. Case Rep. 2019, 13, 344. [Google Scholar] [CrossRef]
- mayoclinic.org. Pulmonary Edema. Available online: https://www.mayoclinic.org/diseases-conditions/pulmonary-edema/symptoms-causes/syc-20377009 (accessed on 26 June 2021).
- fda.gov. 0.9% Sodium Chloride Injection. Available online: https://www.accessdata.fda.gov/drugsatfda_docs/label/2017/016366s214lbl.pdf (accessed on 3 June 2020).
- rxlist.com. Normal Saline. Available online: https://www.rxlist.com/normal-saline-drug.htm (accessed on 19 April 2021).
- Semler, M.W.; Self, W.H.; Wanderer, J.P.; Ehrenfeld, J.M.; Wang, L.; Byrne, D.W.; Stollings, J.L.; Kumar, A.B.; Hughes, C.G.; Hernandez, A. Balanced crystalloids versus saline in critically ill adults. New Engl. J. Med. 2018, 378, 829–839. [Google Scholar] [CrossRef]
- Long, B.; Brady, W.J.; Koyfman, A.; Gottlieb, M. Cardiovascular complications in COVID-19. Am. J. Emerg. Med. 2020, 38, 1504–1507. [Google Scholar] [CrossRef]
- Joseph, S.M.; Cedars, A.M.; Ewald, G.A.; Geltman, E.M.; Mann, D.L. Acute decompensated heart failure: Contemporary medical management. Tex. Heart Inst. J. 2009, 36, 510. [Google Scholar] [PubMed]
- Stokes, J.B.; Fraer, M. Volume disorders. In Nephrology Secrets; Elsevier: Amsterdam, The Netherlands, 2012; pp. 511–521. [Google Scholar]
- WHO. Allergic Rhinitis and Sinusitis. Available online: https://www.who.int/respiratory/other/Rhinitis_sinusitis/en/ (accessed on 3 June 2020).
- Masood, A.; Moumoulidis, I.; Panesar, J. Acute rhinosinusitis in adults: An update on current management. Postgrad. Med. J. 2007, 83, 402–408. [Google Scholar] [CrossRef]
- Gambeta, E.; Chichorro, J.G.; Zamponi, G.W. Trigeminal neuralgia: An overview from pathophysiology to pharmacological treatments. Mol. Pain 2020, 16, 1744806920901890. [Google Scholar] [CrossRef] [PubMed]
- Pogoda, J.M.; Gross, N.B.; Arakaki, X.; Fonteh, A.N.; Cowan, R.P.; Harrington, M.G. Severe headache or migraine history is inversely correlated with dietary sodium intake: NHANES 1999–2004. Headache J. Head Face Pain 2016, 56, 688–698. [Google Scholar] [CrossRef]
- Stanton, A.A. Migraine Cause and Treatment. Ment. Health Fam. Med. 2015, 11, 69–72. [Google Scholar] [CrossRef]
- Pogoda, J.M.; Gross, N.B.; Arakaki, X.; Fonteh, A.N.; Cowan, R.P.; Harrington, M.G. Severe Headache or Migraine History Is Inversely Correlated with Dietary Sodium Intake: NHANES 1999–2004: A Response. Headache 2016, 56, 1216–1218. [Google Scholar] [CrossRef]
- Yeager, A. Lost Smell and Taste Hint COVID-19 can Target the Nervous System. Available online: https://www.the-scientist.com/news-opinion/lost-smell-and-taste-hint-covid-19-can-target-the-nervous-system-67312 (accessed on 3 June 2020).
- Trescot, A.; Brown, M. Peripheral nerve entrapment, hydrodissection, and neural regenerative strategies. Tech. Reg. Anesth. Pain Manag. 2015, 19, 85–93. [Google Scholar] [CrossRef]
- Feldberg, W.; Saxena, P. Mechanism of action of pyrogen. J. Physiol. 1970, 211, 245–261. [Google Scholar] [CrossRef]
- Roberts, C.; Noakes, M. Fatal outcome from administration of a salt emetic. Postgrad. Med. J. 1974, 50, 513–515. [Google Scholar] [CrossRef] [PubMed]
- drugs.com. Sodium Chloride side Effects. Available online: https://www.drugs.com/sfx/sodium-chloride-side-effects.html (accessed on 4 June 2020).
- Mirza, F.N.; Malik, A.A.; Omer, S.B.; Sethi, A. Dermatologic manifestations of COVID-19: A comprehensive systematic review. Int. J. Dermatol. 2020, 60, 418–450. [Google Scholar] [CrossRef]
- Castells, M.C.; Phillips, E.J. Maintaining Safety with SARS-CoV-2 Vaccines. New Engl. J. Med. 2020, 384, 643–649. [Google Scholar] [CrossRef] [PubMed]
- Vaillant, A.A.J.; Vashisht, R.; Zito, P.M. Immediate Hypersensitivity Reactions. Available online: https://www.ncbi.nlm.nih.gov/books/NBK513315/ (accessed on 24 June 2021).
- Polack, F.P.; Thomas, S.J.; Kitchin, N.; Absalon, J.; Gurtman, A.; Lockhart, S.; Perez, J.L.; Pérez Marc, G.; Moreira, E.D.; Zerbini, C. Safety and efficacy of the BNT162b2 mRNA covid-19 vaccine. New Engl. J. Med. 2020, 383, 2603–2615. [Google Scholar] [CrossRef] [PubMed]
- Baden, L.R.; El Sahly, H.M.; Essink, B.; Kotloff, K.; Frey, S.; Novak, R.; Diemert, D.; Spector, S.A.; Rouphael, N.; Creech, C.B. Efficacy and safety of the mRNA-1273 SARS-CoV-2 vaccine. New Engl. J. Med. 2020, 384, 403–416. [Google Scholar] [CrossRef]
- Bejaoui, M. Polyethylene glycol as a potential adjuvant treatment for COVID-19-induced ARDS. Authorea Preprints 2020. [Google Scholar] [CrossRef]
- cdc.gov. Pfizer-BioNTech COVID-19 Vaccine: Vaccine Preparation. Available online: https://www.cdc.gov/vaccines/covid-19/info-by-product/pfizer/downloads/diluent-poster.pdf (accessed on 18 July 2021).
- WHO. Influenza (Seasonal). Available online: https://www.who.int/news-room/fact-sheets/detail/influenza-(seasonal) (accessed on 2 June 2020).
- Geier, D.A.; Kern, J.K.; Geier, M.R. A longitudinal ecological study of seasonal influenza deaths in relation to climate conditions in the United States from 1999 through 2011. Infect. Ecol. Epidemiol. 2018, 8, 1474708. [Google Scholar] [CrossRef]
- Pica, N.; Bouvier, N.M. Environmental factors affecting the transmission of respiratory viruses. Curr. Opin. Virol. 2012, 2, 90–95. [Google Scholar] [CrossRef]
- Shahar, D.R.; Froom, P.; Harari, G.; Yerushalmi, N.; Lubin, F.; Kristal-Boneh, E. Changes in dietary intake account for seasonal changes in cardiovascular disease risk factors. Eur. J. Clin. Nutr. 1999, 53, 395–400. [Google Scholar] [CrossRef]
- Ersoy, N.; Taşçi, İ.; Özgürtaş, T.; Salih, B.; Doruk, H.; Rakicioğlu, N. Effect of seasonal changes on nutritional status and biochemical parameters in Turkish older adults. Nutr. Res. Pr. 2018, 12, 315–323. [Google Scholar] [CrossRef]
- Rossato, S.; Olinto, M.; Henn, R.; Moreira, L.; Camey, S.; Anjos, L.; Wahrlich, V.; Waissmann, W.; Fuchs, F.; Fuchs, S. Seasonal variation in food intake and the interaction effects of sex and age among adults in southern Brazil. Eur. J. Clin. Nutr. 2015, 69, 1015–1022. [Google Scholar] [CrossRef]
- Van der Toorn, J.E.; Cepeda, M.; Kiefte-de Jong, J.C.; Franco, O.H.; Voortman, T.; Schoufour, J.D. Seasonal variation of diet quality in a large middle-aged and elderly Dutch population-based cohort. Eur. J. Nutr. 2020, 59, 493–504. [Google Scholar] [CrossRef] [PubMed]
- Hashimoto, J.; Imai, Y.; Minami, N.; Munakata, M.; Sakuma, H.; Sekino, H.; Imai, K.; Sasaki, S.; Yoshinaga, K.; Abe, K. Compliance with long-term dietary salt restriction in hypertensive outpatients. Clin. Exp. Hypertens. 1994, 16, 729–739. [Google Scholar] [CrossRef] [PubMed]
- Visscher, T.; Seidell, J. Time trends (1993–1997) and seasonal variation in body mass index and waist circumference in the Netherlands. Int. J. Obes. 2004, 28, 1309–1316. [Google Scholar] [CrossRef] [PubMed]
- cdc.gov. Sodium and the Dietary Guidelines. Available online: https://www.cdc.gov/salt/pdfs/sodium_dietary_guidelines.pdf (accessed on 27 June 2021).
- Chen, S.; Prettner, K.; Kuhn, M.; Geldsetzer, P.; Wang, C.; Bärnighausen, T.; Bloom, D.E. Climate and the spread of COVID-19. Sci. Rep. 2021, 11, 1–6. [Google Scholar]
- Lam, T.; VoPham, T.; Munger, K.L.; Laden, F.; Hart, J.E. Long-term effects of latitude, ambient temperature, and ultraviolet radiation on the incidence of multiple sclerosis in two cohorts of US women. Environ. Epidemiol. 2020, 4. [Google Scholar] [CrossRef]
- Cortese, M.; Yuan, C.; Chitnis, T.; Ascherio, A.; Munger, K.L. No association between dietary sodium intake and the risk of multiple sclerosis. Neurology 2017, 89, 1322–1329. [Google Scholar] [CrossRef]
- Whelton, P.K.; Appel, L.J.; Sacco, R.L.; Anderson, C.A.; Antman, E.M.; Campbell, N.; Dunbar, S.B.; Frohlich, E.D.; Hall, J.E.; Jessup, M. Sodium, blood pressure, and cardiovascular disease: Further evidence supporting the American Heart Association sodium reduction recommendations. Circulation 2012, 126, 2880–2889. [Google Scholar] [CrossRef]
- Eskandarieh, S.; Heydarpour, P.; Minagar, A.; Pourmand, S.; Sahraian, M.A. Multiple sclerosis epidemiology in east Asia, South East Asia and South Asia: A systematic review. Neuroepidemiology 2016, 46, 209–221. [Google Scholar] [CrossRef]
- Bates, G.P.; Miller, V.S. Sweat rate and sodium loss during work in the heat. J. Occup. Med. Toxicol. 2008, 3, 4. [Google Scholar] [CrossRef]
- Sigal, C.B.; Dobson, R.L. The effect of salt intake on sweat gland function. J. Investig. Dermatol. 1968, 50, 451–455. [Google Scholar] [CrossRef][Green Version]
- Nieman, D.C.; Henson, D.A.; Austin, M.D.; Sha, W. Upper respiratory tract infection is reduced in physically fit and active adults. Br. J. Sports Med. 2011, 45, 987–992. [Google Scholar] [CrossRef]
- Wimbish, J. NBA Announces Zero Players Tested Positive for COVID-19 Inside Disney Bubble for Fifth Straight Week. Available online: https://www.cbssports.com/nba/news/nba-announces-zero-players-tested-positive-for-covid-19-inside-disney-bubble-for-fifth-straight-week/ (accessed on 19 August 2020).
- Osterberg, K.L.; Horswill, C.A.; Baker, L.B. Pregame urine specific gravity and fluid intake by National Basketball Association players during competition. J. Athl. Train. 2009, 44, 53–57. [Google Scholar] [CrossRef] [PubMed]
- Cohen, J.; Pfeiffer, K.; Francis, J.A. Warm Arctic episodes linked with increased frequency of extreme winter weather in the United States. Nat. Commun. 2018, 9, 1–12. [Google Scholar] [CrossRef]
- Stuckler, D.; McKee, M.; Ebrahim, S.; Basu, S. Manufacturing epidemics: The role of global producers in increased consumption of unhealthy commodities including processed foods, alcohol, and tobacco. PLoS Med. 2012, 9, e1001235. [Google Scholar] [CrossRef] [PubMed]
- Moodie, R.; Stuckler, D.; Monteiro, C.; Sheron, N.; Neal, B.; Thamarangsi, T.; Lincoln, P.; Casswell, S.; Group, L.N.A. Profits and pandemics: Prevention of harmful effects of tobacco, alcohol, and ultra-processed food and drink industries. Lancet 2013, 381, 670–679. [Google Scholar] [CrossRef]
- zupreem.com. Exotic Feline Diet Canned. Available online: https://www.zupreem.com/products/zoo-animals/exotic-feline/ (accessed on 26 April 2020).
- Animal and Plant Health Inspection Service, United States Department of Agriculture. USDA Statement on the Confimation of COVID-19 in a Tiger in New York. Available online: https://www.aphis.usda.gov/aphis/newsroom/news/sa_by_date/sa-2020/ny-zoo-covid-19 (accessed on 26 April 2020).
- Everts, S. Processed: Food Science and the Modern Meal. Available online: https://www.sciencehistory.org/distillations/processed-food-science-and-the-modern-meal (accessed on 4 June 2020).
- bbc.com.uk. What did People Eat During World War One? Available online: https://www.bbc.co.uk/bitesize/topics/zqhyb9q/articles/z8kv34j (accessed on 4 June 2020).
- Roos, D. Why the Second Wave of the 1918 Spanish Flu was so Deadly. Available online: https://www.history.com/news/spanish-flu-second-wave-resurgence (accessed on 4 June 2020).
- Taubenberger, J.K.; Morens, D.M. 1918 Influenza: The mother of all pandemics. Rev. Biomed. 2006, 17, 69–79. [Google Scholar] [CrossRef]
- Maver, M.B. Nutritional edema and war dropsy. J. Am. Med. Assoc. 1920, 74, 934–941. [Google Scholar] [CrossRef][Green Version]
- Shope, R.E. Influenza: History, epidemiology, and speculation: The RE Dyer lecture. Public Health Rep. 1958, 73, 165. [Google Scholar] [CrossRef]
- Patrozou, E.; Mermel, L.A. Does influenza transmission occur from asymptomatic infection or prior to symptom onset? Public Health Rep. 2009, 124, 193–196. [Google Scholar] [CrossRef]
- Savvides, C.; Siegel, R. Asymptomatic and presymptomatic transmission of SARS-CoV-2: A systematic review. Medrxiv: Prepr. Serv. Health Sci. 2020. [Google Scholar] [CrossRef]
- cdc.gov. How Flu Spreads. Available online: https://www.cdc.gov/flu/about/disease/spread.htm (accessed on 27 June 2021).
- Sanjuán, R. Collective Infectious Units in Viruses. Trends Microbiol. 2017, 25, 402–412. [Google Scholar] [CrossRef]
- Hobday, R.A.; Cason, J.W. The open-air treatment of pandemic influenza. Am. J. Public Health 2009, 99, S236–S242. [Google Scholar] [CrossRef]
- Ernst, E.; Pecho, E.; Wirz, P.; Saradeth, T. Regular sauna bathing and the incidence of common colds. Ann. Med. 1990, 22, 225–227. [Google Scholar] [CrossRef]
- Zaccardi, F.; Laukkanen, T.; Willeit, P.; Kunutsor, S.K.; Kauhanen, J.; Laukkanen, J.A. Sauna bathing and incident hypertension: A prospective cohort study. Am. J. Hypertens. 2017, 30, 1120–1125. [Google Scholar] [CrossRef]
- Fictum, D. Salt Pork, Ship’s Biscuit, and Burgoo: Sea Provisions for Common Sailors and Pirates. Available online: https://csphistorical.com/2016/01/24/salt-pork-ships-biscuit-and-burgoo-sea-provisions-for-common-sailors-and-pirates-part-1/ (accessed on 9 February 2021).
- Price, C. The Age of Scurvy. Available online: https://www.sciencehistory.org/distillations/magazine/the-age-of-scurvy (accessed on 9 February 2021).
- McCann, A.W. Two Hundred and Fifty-Five Days! In This Famishing World; George H. Doran Company: New York, NY, USA, 1918. [Google Scholar]
- Mallapaty, S. What the cruise-ship outbreaks reveal about COVID-19. Nature 2020, 580, 18. [Google Scholar] [CrossRef]
- Lau, Y.-Y.; Yip, T.L. The procurement of food on board liner ships: The role of the international labor organization. J. Shipp. Trade 2017, 2, 6. [Google Scholar] [CrossRef]
- Stein, R.A.; Ometa, O. When Public Health Crises Collide: Social Disparities and COVID-19. Int. J. Clin. Pract. 2020, e13524. [Google Scholar] [CrossRef]
- De Mestral, C.; Mayén, A.-L.; Petrovic, D.; Marques-Vidal, P.; Bochud, M.; Stringhini, S. Socioeconomic determinants of sodium intake in adult populations of high-income countries: A systematic review and meta-analysis. Am. J. Public Health 2017, 107, e1–e12. [Google Scholar] [CrossRef]
- Kakol, M.; Upson, D.; Sood, A. Susceptibility of Southwestern American Indian Tribes to Coronavirus Disease 2019 (COVID-19). J. Rural Health. 2021, 37, 197–199. [Google Scholar] [CrossRef]
- Lansbury, L.E.; Brown, C.S.; Nguyen-Van-Tam, J.S. Influenza in long-term care facilities. Influenza Other Respir. Viruses 2017, 11, 356–366. [Google Scholar] [CrossRef]
- Barnett, M.L.; Grabowski, D.C. Nursing homes are ground zero for COVID-19 pandemic. JAMA Health Forum 2020, 1, e200369. [Google Scholar] [CrossRef]
- Dharmarajan, T.S.; Manalo, M.; Manalac, M.; Kanagala, M. Hypothermia in the nursing home: Adverse outcomes in two older men. J. Am. Med. Dir. Assoc. 2001, 2, 29–33. [Google Scholar] [CrossRef]
- Hawks, L.; Woolhandler, S.; McCormick, D. COVID-19 in Prisons and Jails in the United States. JAMA Intern. Med. 2020, 180, 1041–1042. [Google Scholar] [CrossRef]
- Mintz, C. Food in Hospitals and Prisons is Terrible—But it doesn’t have to be that Way. Available online: https://www.theglobeandmail.com/life/food-and-wine/food-trends/food-in-hospitals-prisons-is-notoriously-bad-but-it-doesnt-have-to-be-that-way/article29951216/ (accessed on 4 June 2020).

Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2021 by the author. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Brown, R.B. Sodium Toxicity in the Nutritional Epidemiology and Nutritional Immunology of COVID-19. Medicina 2021, 57, 739. https://doi.org/10.3390/medicina57080739
Brown RB. Sodium Toxicity in the Nutritional Epidemiology and Nutritional Immunology of COVID-19. Medicina. 2021; 57(8):739. https://doi.org/10.3390/medicina57080739
Chicago/Turabian StyleBrown, Ronald B. 2021. "Sodium Toxicity in the Nutritional Epidemiology and Nutritional Immunology of COVID-19" Medicina 57, no. 8: 739. https://doi.org/10.3390/medicina57080739
APA StyleBrown, R. B. (2021). Sodium Toxicity in the Nutritional Epidemiology and Nutritional Immunology of COVID-19. Medicina, 57(8), 739. https://doi.org/10.3390/medicina57080739





