Cognitive Status Epilepticus: Two Case Reports
Abstract
:1. Introduction
2. Case Presentation
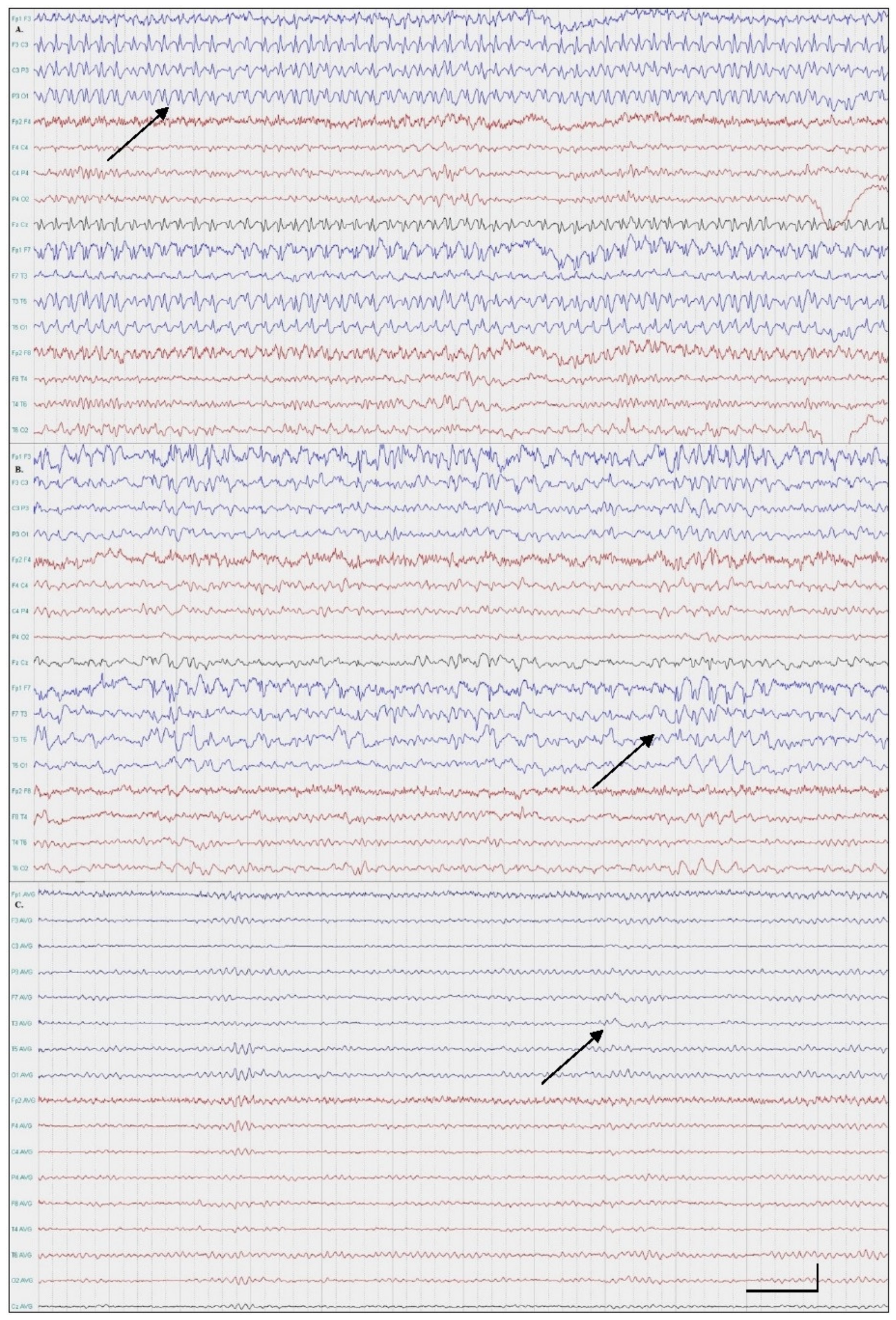
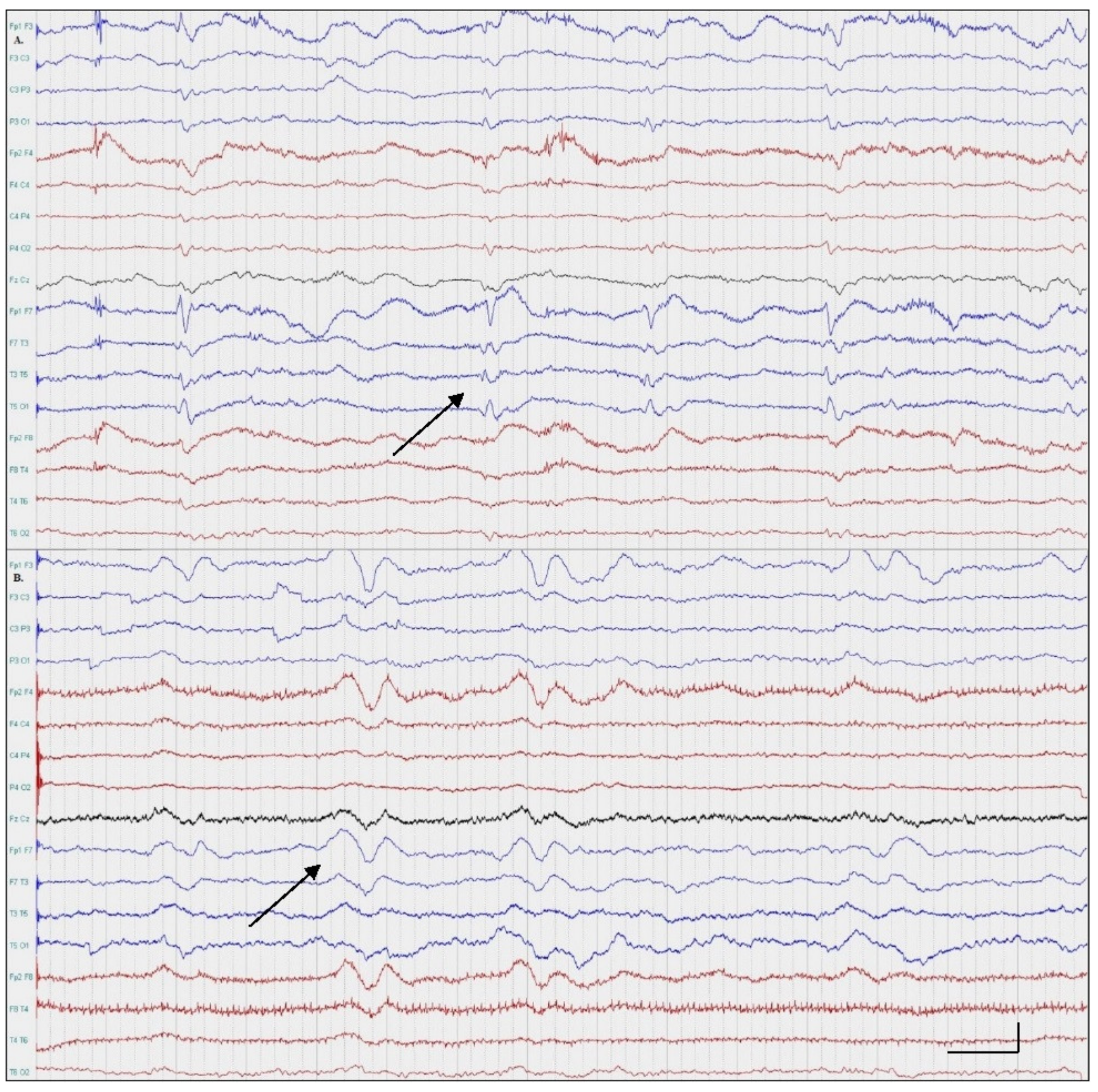
2.1. Patient One; Amnestic SE
2.2. Patient Two; Aphasic SE
3. Discussion
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Conflicts of Interest
References
- Brodie, M.J.; Zuberi, S.M.; Scheffer, I.E.; Fisher, R.S. Seminar in Epileptology. The 2017 ILAE classification of seizure types and the epilepsies: What do people with epilepsy and their caregivers need to know? Epileptic Disord. 2018, 20, 77–87. [Google Scholar] [PubMed]
- Panayiotopoulos, C.P. A Clinical Guide to Epileptic Syndromes and Their Treatment; Springer: London, UK, 2007. [Google Scholar]
- Krishnan, V.; Drislane, F.W.; Benatar, M.G. Cognitive Manifestations of Focal Status Epilepticus. In Status Epilepticus; Springer International Publishing: Cham, Switzerlnad, 2018; pp. 259–273. [Google Scholar]
- Leitinger, M.; Beniczky, S.; Rohracher, A.; Gardella, E.; Kalss, G.; Qerama, E.; Höfler, J.; Lindberg-Larsen, A.H.; Kuchukhidze, G.; Dobesberger, J.; et al. Salzburg Consensus Criteria for Non-Convulsive Status Epilepticus—Approach to clinical application. Epilepsy Behav. 2015, 49, 158–163. [Google Scholar] [CrossRef]
- Arena, J.E.; Rabinstein, A.A. Transient Global Amnesia. Mayo Clin. Proc. 2015, 90, 264–272. [Google Scholar] [CrossRef] [PubMed] [Green Version]
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2021 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Karantali, E.; Chatzikonstantinou, S.; Mavroudis, I.; Trus, C.; Kazis, D. Cognitive Status Epilepticus: Two Case Reports. Medicina 2021, 57, 799. https://doi.org/10.3390/medicina57080799
Karantali E, Chatzikonstantinou S, Mavroudis I, Trus C, Kazis D. Cognitive Status Epilepticus: Two Case Reports. Medicina. 2021; 57(8):799. https://doi.org/10.3390/medicina57080799
Chicago/Turabian StyleKarantali, Eleni, Symela Chatzikonstantinou, Ioannis Mavroudis, Constantin Trus, and Dimitrios Kazis. 2021. "Cognitive Status Epilepticus: Two Case Reports" Medicina 57, no. 8: 799. https://doi.org/10.3390/medicina57080799
APA StyleKarantali, E., Chatzikonstantinou, S., Mavroudis, I., Trus, C., & Kazis, D. (2021). Cognitive Status Epilepticus: Two Case Reports. Medicina, 57(8), 799. https://doi.org/10.3390/medicina57080799





