Treatment of Navicular Stress Fracture Accompanied by Os Supranaviculare: A Case Report
Abstract
:1. Introduction
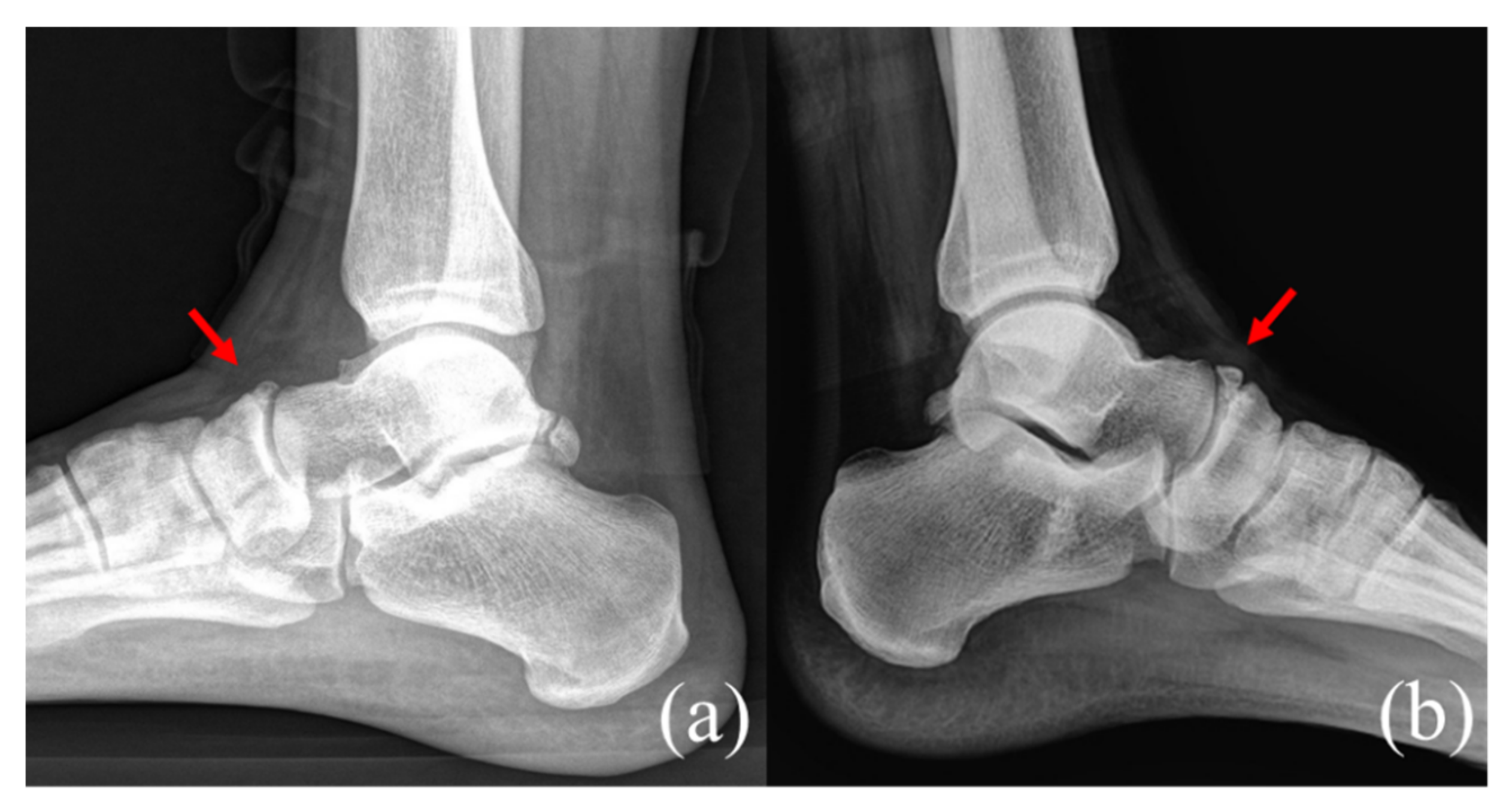
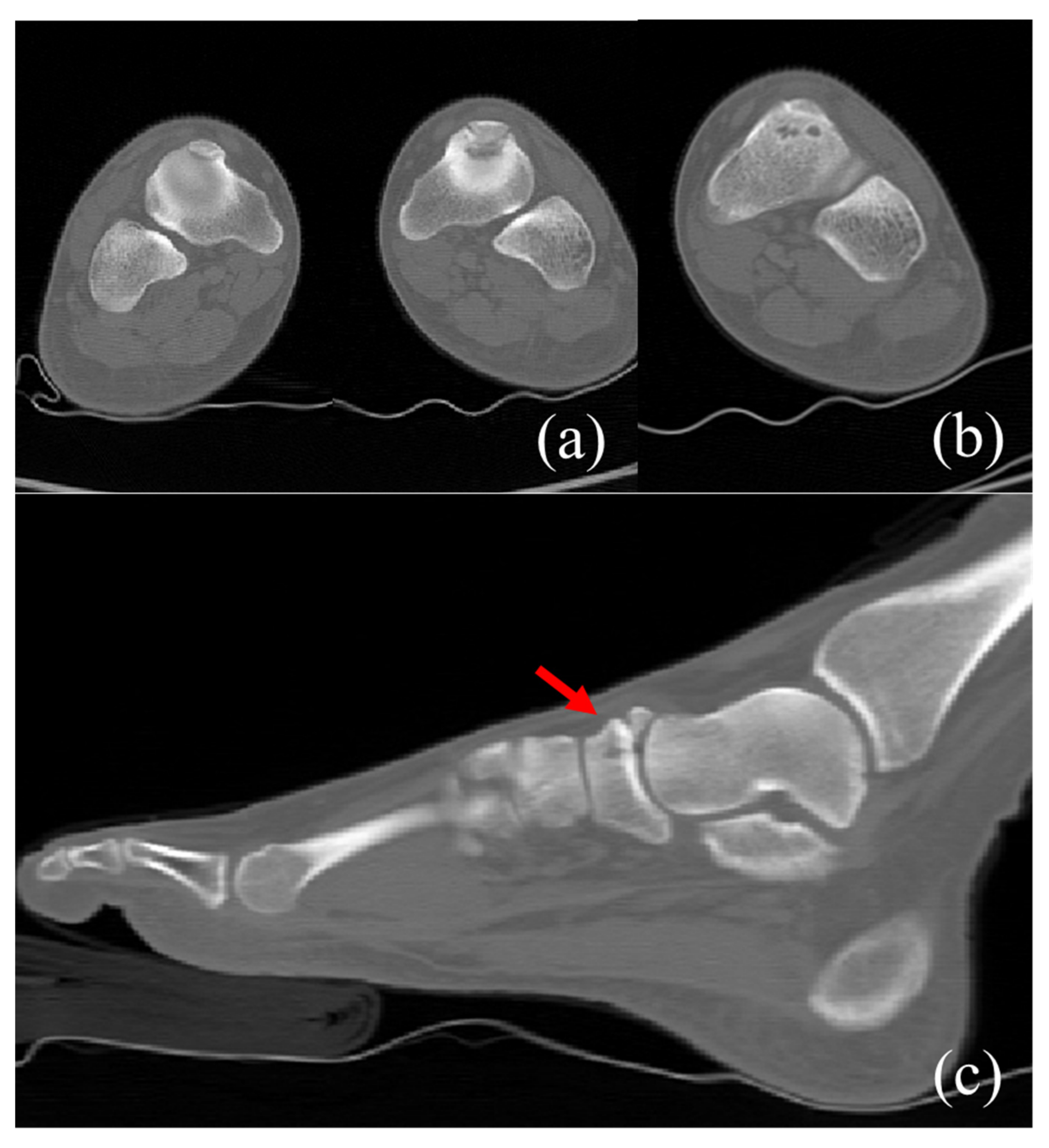
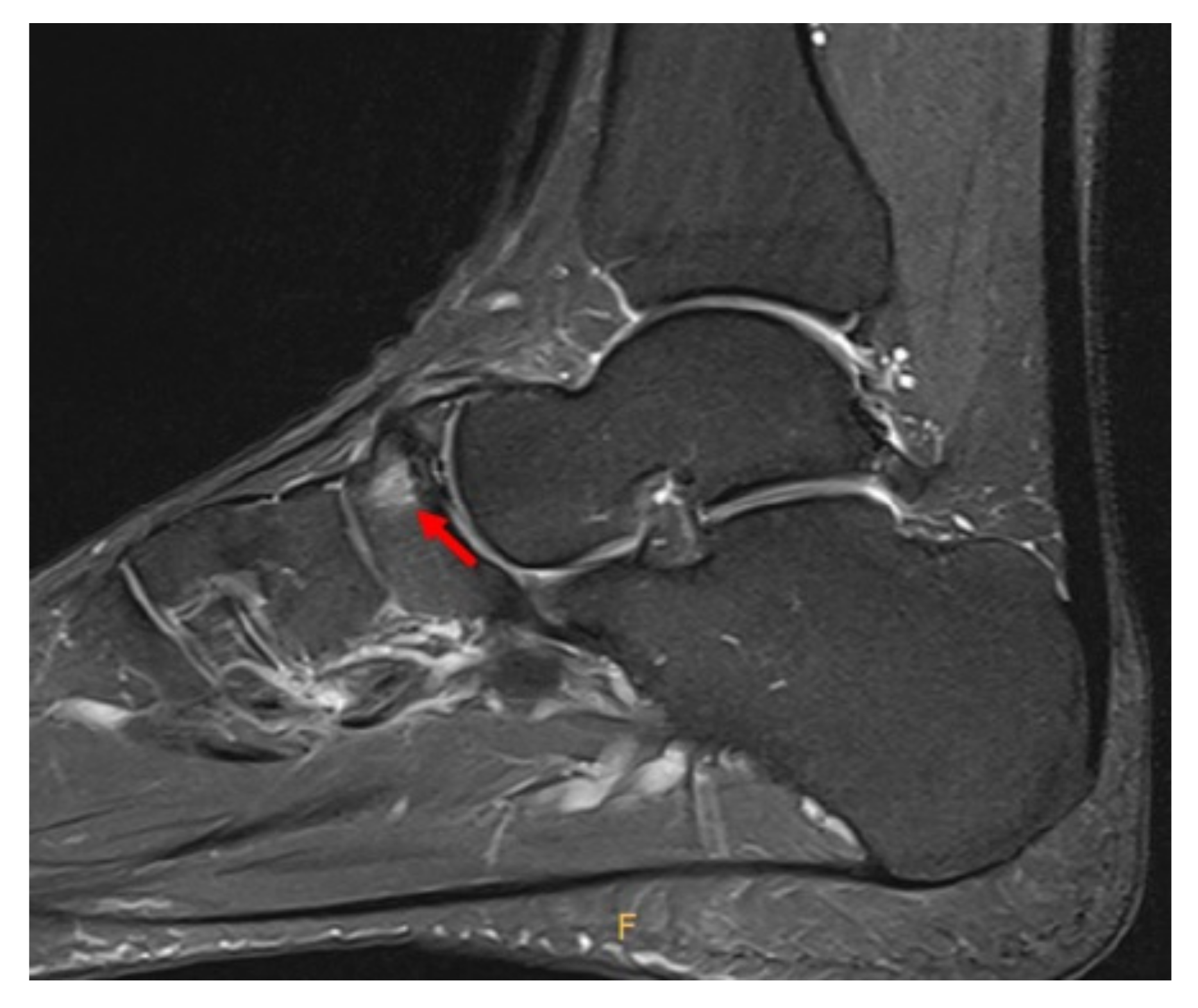
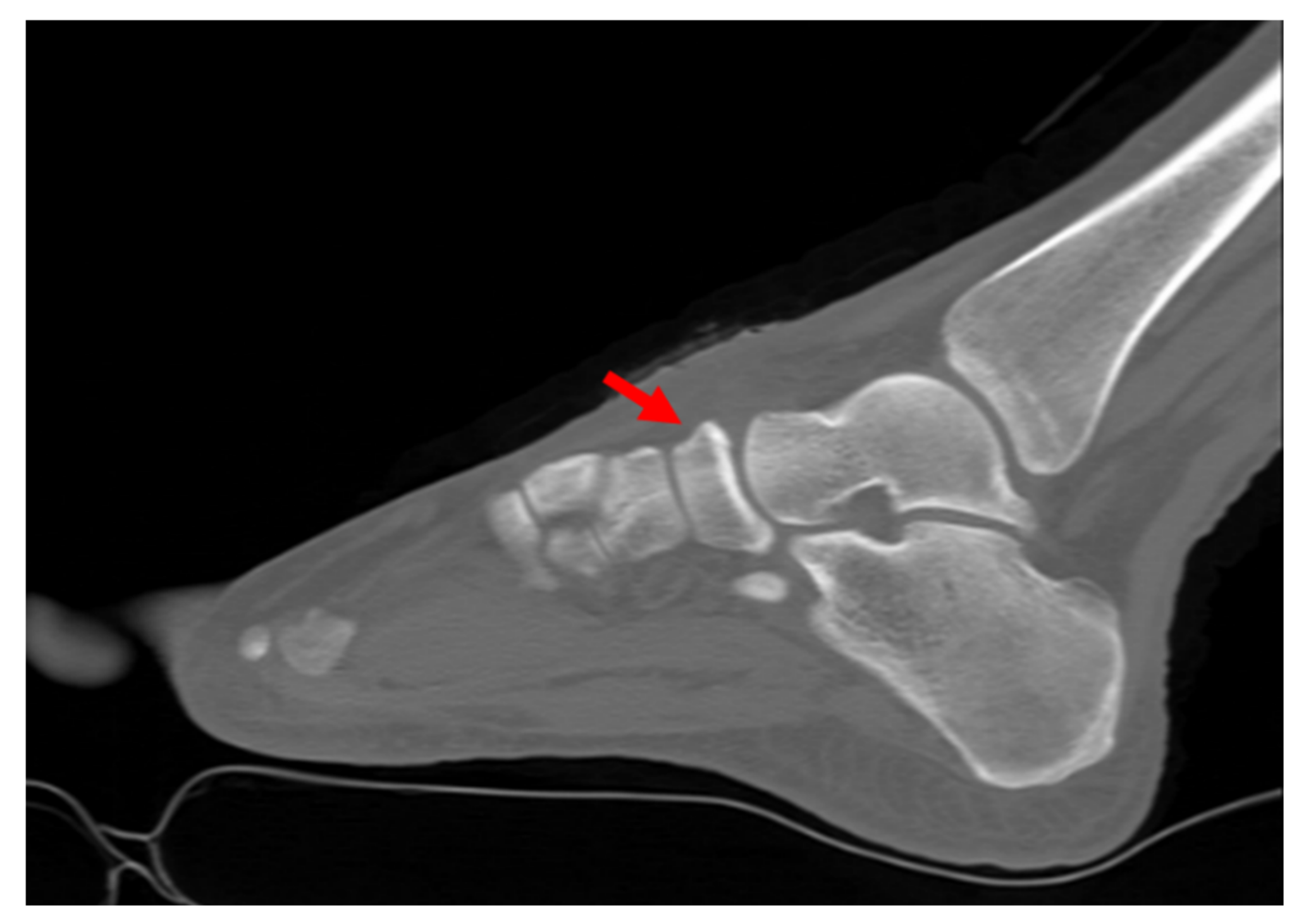
2. Case Presentation
3. Discussion
4. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Conflicts of Interest
Abbreviations
References
- Towne, L.C.; Blazina, M.E.; Cozen, L.N. Fatigue fracture of the tarsal navicular. JBJS 1970, 52, 376–378. [Google Scholar] [CrossRef]
- Fowler, J.R.; Gaughan, J.P.; Boden, B.P.; Pavlov, H.; Torg, J.S. The non-surgical and surgical treatment of tarsal navicular stress fractures. Sports Med. 2011, 41, 613–619. [Google Scholar] [CrossRef] [PubMed]
- Tsuruta, T.; Shiokawa, Y.; Kato, A.; Matsumoto, T.; Yamazoe, Y.; Oike, T.; Sugiyama, T.; Saito, M. Radiological study of the accessory skeletal elements in the foot and ankle (author’s transl). Nihon Seikeigeka Gakkai Zasshi 1981, 55, 357–370. [Google Scholar] [PubMed]
- Ingalls, J.; Wissman, R. The os supranaviculare and navicular stress fractures. Skelet. Radiol. 2011, 40, 937–941. [Google Scholar] [CrossRef]
- Kiter, E.; Günal, İ.; Turgut, A.; Köse, N. Evaluation of simple excision in the treatment of symptomatic accessory navicular associated with flat feet. J. Orthop. Sci. 2000, 5, 333–335. [Google Scholar] [CrossRef]
- Golano, P.; Fariñas, O.; Sáenz, I. The anatomy of the navicular and periarticular structures. Foot Ankle Clin. 2004, 9, 1–23. [Google Scholar] [CrossRef]
- Hossain, M.; Clutton, J.; Ridgewell, M.; Lyons, K.; Perera, A. Stress fractures of the foot. Clin. Sports Med. 2015, 34, 769–790. [Google Scholar] [CrossRef]
- Waugh, W. The ossification and vascularisation of the tarsal navicular and their relation to koìˆhler’s disease. J. Bone Jt. Surg. Br. Vol. 1958, 40, 765–777. [Google Scholar] [CrossRef]
- McInnis, K.C.; Ramey, L.N. High-risk stress fractures: Diagnosis and management. PMR 2016, 8, S113–S124. [Google Scholar] [CrossRef]
- Coris, E.E.; Lombardo, J.A. Tarsal navicular stress fractures. Am. Fam. Physician 2003, 67, 85–90. [Google Scholar]
- Torg, J.S.; Moyer, J.; Gaughan, J.P.; Boden, B.P. Management of tarsal navicular stress fractures: Conservative versus surgical treatment: A meta-analysis. Am. J. Sports Med. 2010, 38, 1048–1053. [Google Scholar] [CrossRef]
- Pavlov, H.; Torg, J.; Freiberger, R. Tarsal navicular stress fractures: Radiographic evaluation. Radiology 1983, 148, 641–645. [Google Scholar] [CrossRef]
- Coskun, N.; Yuksel, M.; Cevener, M.; Arican, R.Y.; Ozdemir, H.; Bircan, O.; Sindel, T.; Ilgi, S.; Sindel, M. Incidence of accessory ossicles and sesamoid bones in the feet: A radiographic study of the Turkish subjects. Surg. Radiol. Anat. 2009, 31, 19–24. [Google Scholar] [CrossRef]
- Eichenholtz, S.N.; Levine, D.B. Fractures of the tarsal navicular bone. Clin. Orthop. Relat. Res. 1964, 34, 142–160. [Google Scholar] [CrossRef]
- Lee, S.; Anderson, R.B. Stress fractures of the tarsal navicular. Foot Ankle Clin. 2004, 9, 85–104. [Google Scholar] [CrossRef]
- Saxena, A.; Fullem, B.; Hannaford, D. Results of treatment of 22 navicular stress fractures and a new proposed radiographic classification system. J. Foot Ankle Surg. 2000, 39, 96–103. [Google Scholar] [CrossRef]
- Fitch, K.; Blackwell, J.; Gilmour, W. Operation for non-union of stress fracture of the tarsal navicular. J. Bone Jt. Surg. Br. Vol. 1989, 71, 105–110. [Google Scholar] [CrossRef] [Green Version]
- Burne, S.; Mahoney, C.; Forster, B. Long-term outcome and clinico-radiological correlation using both computed tomography and magnetic resonance imaging. Am. J. Sports Med. 2005, 33, 1875–1881. [Google Scholar] [CrossRef]
- Gross, C.E.; Nunley, J.A. Navicular stress fractures. Foot Ankle Int. 2015, 36, 1117–1122. [Google Scholar] [CrossRef]
- Khan, K.M.; Fuller, P.J.; Brukner, P.D.; Kearney, C.; Burry, H.C. Outcome of conservative and surgical management of navicular stress fracture in athletes: Eighty-six cases proven with computerized tomography. Am. J. Sports Med. 1992, 20, 657–666. [Google Scholar] [CrossRef]
- De Clercq, P.; Bevernage, B.D.; Leemrijse, T. Stress fracture of the navicular bone. Acta Orthop. Belg. 2008, 74, 725–734. [Google Scholar]
- Shakked, R.J.; Walters, E.E.; O’Malley, M.J. Tarsal navicular stress fractures. Curr. Rev. Musculoskelet. Med. 2017, 10, 122–130. [Google Scholar] [CrossRef] [Green Version]
- Perisano, C.; Greco, T.; Vitiello, R.; Maccauro, G.; Liuzza, F.; Tamburelli, F.; Forconi, F. Mueller-Weiss disease: Review of the literature. J. Biol. Regul. Homeost. Agents 2018, 32 (Suppl. 1), 157–162. [Google Scholar]
- Ramadorai, M.U.E.; Beuchel, M.W.; Sangeorzan, B.J. Fractures and dislocations of the tarsal navicular. JAAOS-J. Am. Acad. Orthop. Surg. 2016, 24, 379–389. [Google Scholar] [CrossRef]
- Saxena, A.; Behan, S.A.; Valerio, D.L.; Frosch, D.L. Navicular stress fracture outcomes in athletes: Analysis of 62 injuries. J. Foot Ankle Surg. 2017, 56, 943–948. [Google Scholar] [CrossRef]
- Torg, J.S.; Pavlov, H.; Roberts, M.M.; Eremus, J.; Drakos, M.C.; Arnoczky, S.P. The tarsal navicular stress fracture revisited: The unequivocal case for conservative, non-surgical management. Foot Ankle Orthop. 2016, 1, 2473011416S00018. [Google Scholar] [CrossRef] [Green Version]
- Currey, J. The Mechanical Adaptations of Bones; Princeton University Press: Princeton, NJ, USA, 1984; pp. 38–68. [Google Scholar]

Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2021 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Kim, W.-J.; Jung, K.-J.; Yeo, E.-D.; Lee, H.-S.; Won, S.-H.; Lee, D.-W.; Ji, J.-Y.; Yoon, S.-J.; Hong, Y.-C. Treatment of Navicular Stress Fracture Accompanied by Os Supranaviculare: A Case Report. Medicina 2022, 58, 27. https://doi.org/10.3390/medicina58010027
Kim W-J, Jung K-J, Yeo E-D, Lee H-S, Won S-H, Lee D-W, Ji J-Y, Yoon S-J, Hong Y-C. Treatment of Navicular Stress Fracture Accompanied by Os Supranaviculare: A Case Report. Medicina. 2022; 58(1):27. https://doi.org/10.3390/medicina58010027
Chicago/Turabian StyleKim, Woo-Jong, Ki-Jin Jung, Eui-Dong Yeo, Hong-Seop Lee, Sung-Hun Won, Dhong-Won Lee, Jae-Young Ji, Sung-Joon Yoon, and Yong-Cheol Hong. 2022. "Treatment of Navicular Stress Fracture Accompanied by Os Supranaviculare: A Case Report" Medicina 58, no. 1: 27. https://doi.org/10.3390/medicina58010027
APA StyleKim, W.-J., Jung, K.-J., Yeo, E.-D., Lee, H.-S., Won, S.-H., Lee, D.-W., Ji, J.-Y., Yoon, S.-J., & Hong, Y.-C. (2022). Treatment of Navicular Stress Fracture Accompanied by Os Supranaviculare: A Case Report. Medicina, 58(1), 27. https://doi.org/10.3390/medicina58010027






