Long-Term Survival Rate of Autogenous Tooth Transplantation: Up to 162 Months
Abstract
1. Introduction
2. Materials and Methods
2.1. Surgical Technique
2.2. Statistical Methods
3. Results
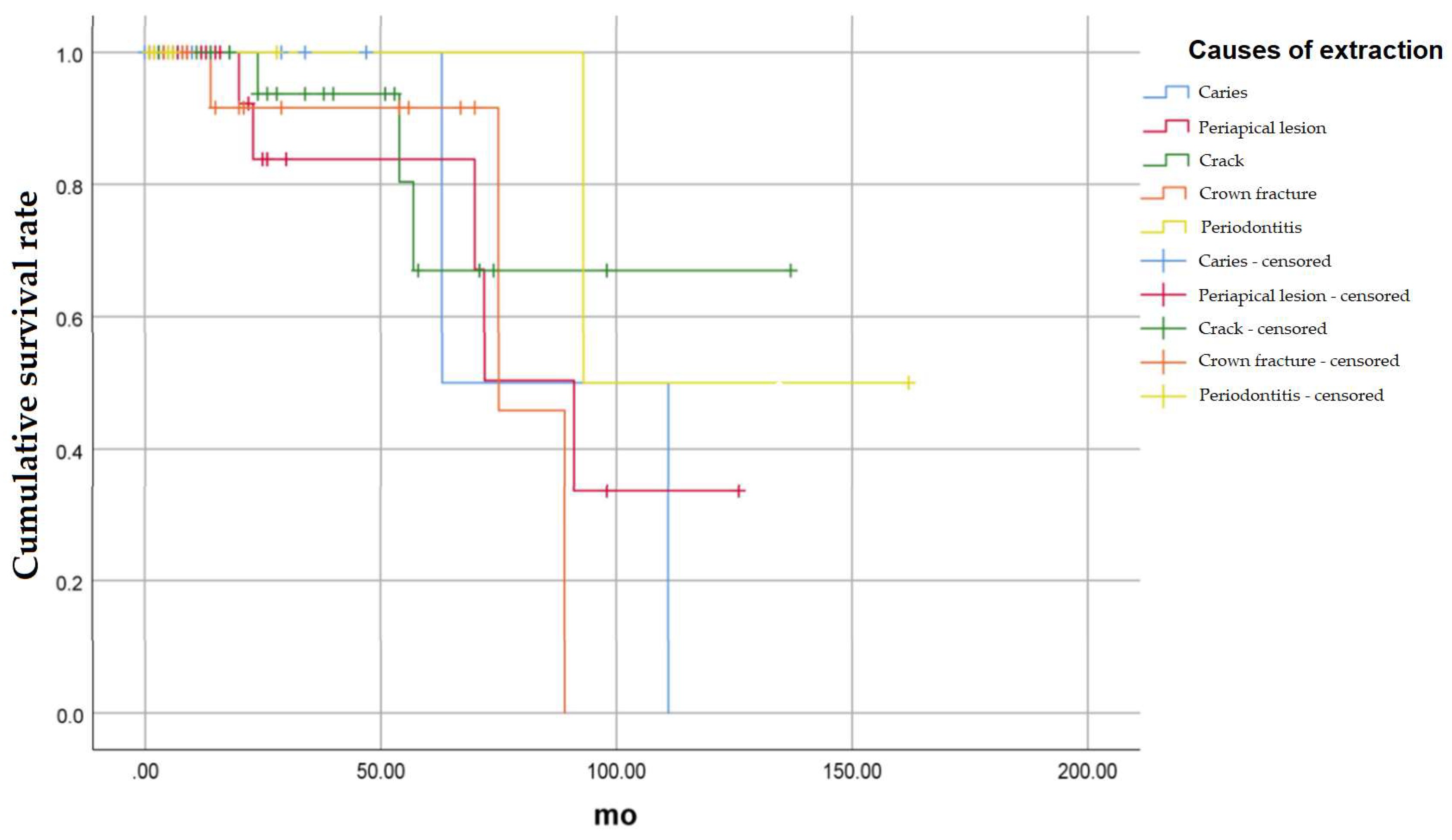
3.1. Cumulative Survival Rate According to the Cause of Extraction of the Recipient Teeth
3.1.1. Caries
3.1.2. Periapical Lesion
3.1.3. Crack
3.1.4. Crown Fracture
3.1.5. Periodontitis
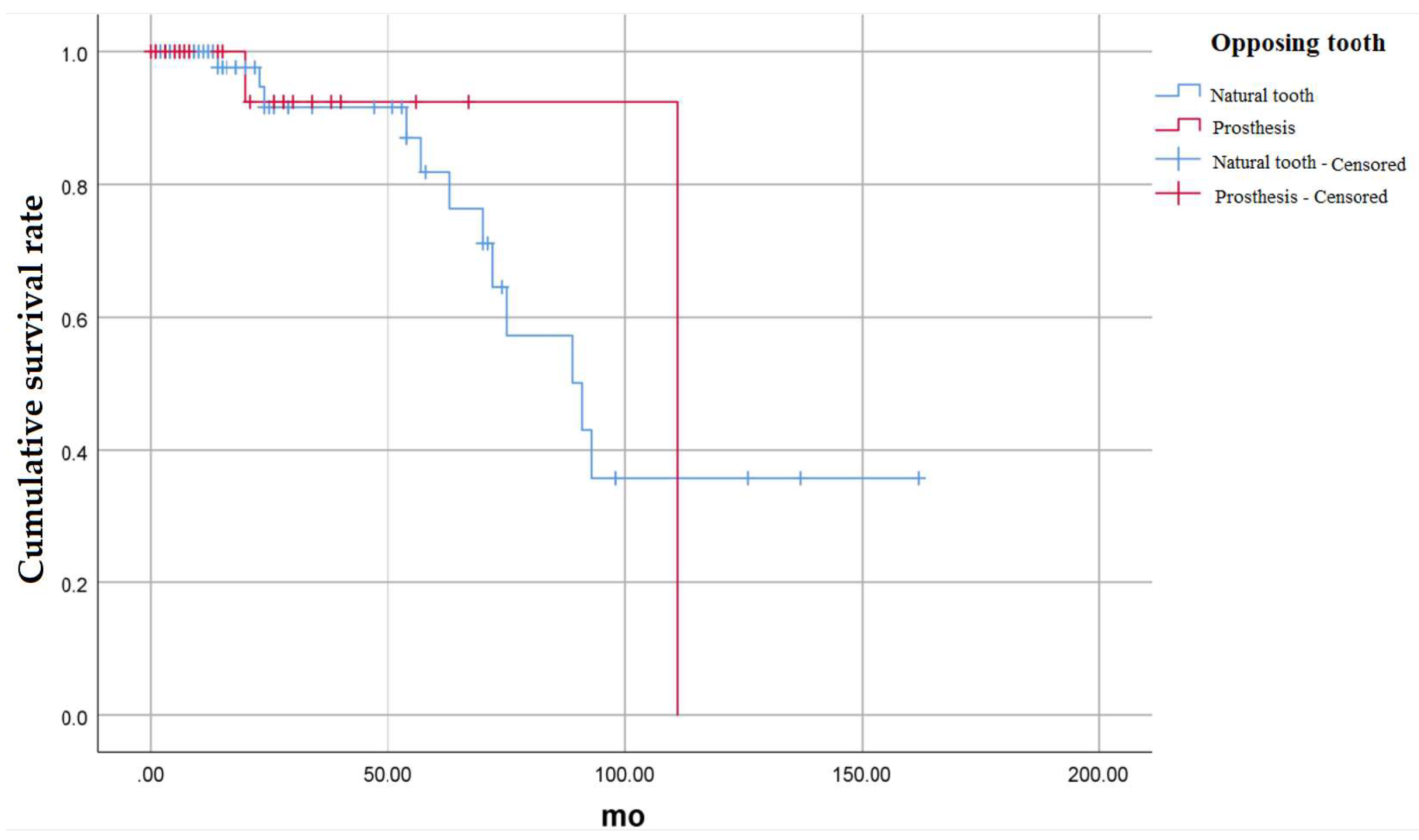
3.2. Cumulative Survival Rate According to the Condition of Opposing Teeth
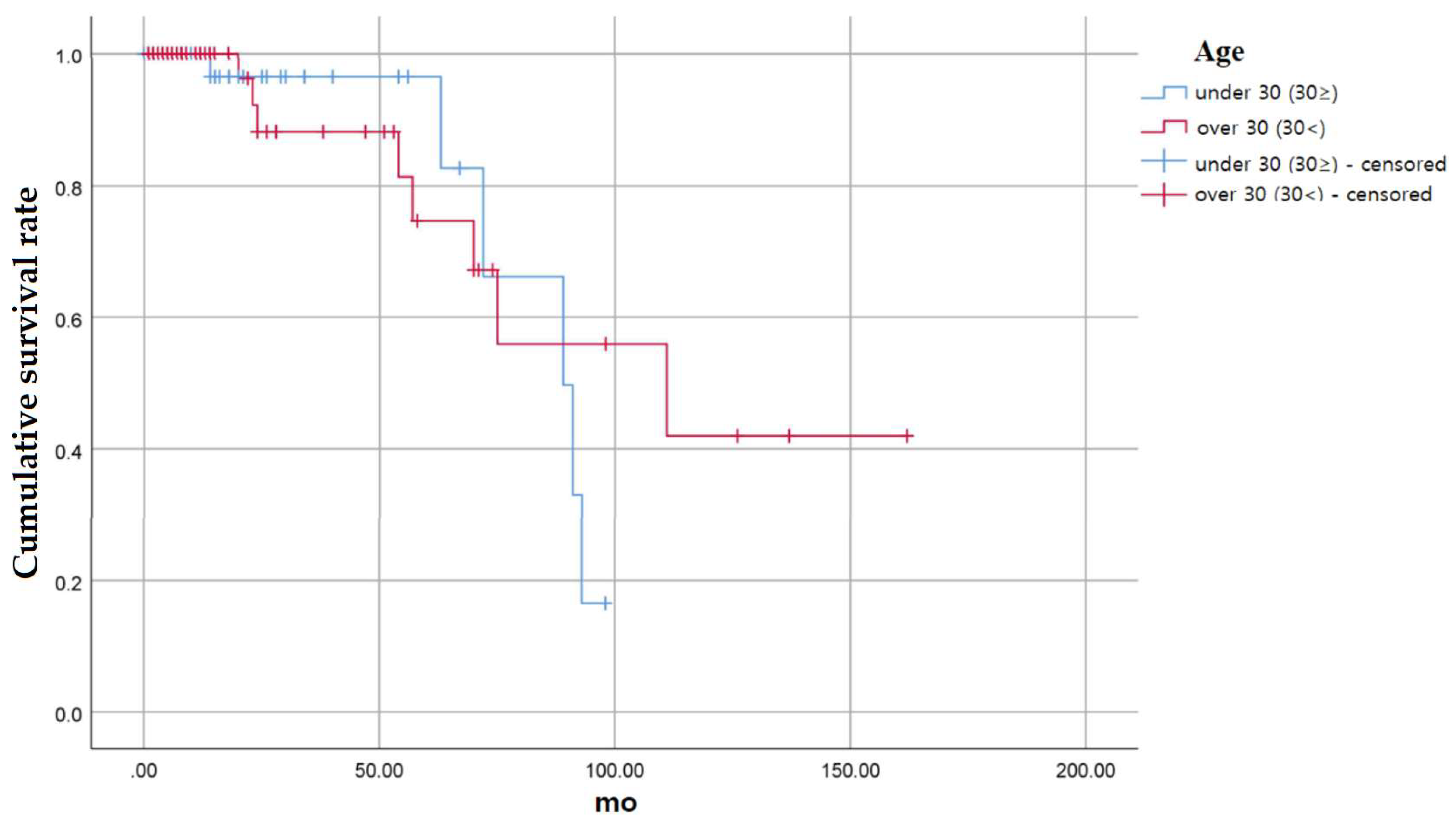
3.3. Cumulative Survival Rate According to the Age of Patients
4. Discussion
5. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Conflicts of Interest
References
- Natiella, J.R.; Armitage, J.E.; Greene, G.W. The replantation and transplantation of teeth: A review. Oral Surg. Oral Med. Oral Pathol. 1970, 29, 397–419. [Google Scholar] [CrossRef]
- Ml, H. Autogenous transplants. Oral Surg. Oral Med. Oral Pathol. 1956, 9, 76–83. [Google Scholar]
- Reich, P.P. Autogenous transplantation of maxillary and mandibular molars. J. Oral Maxillofac. Surg. 2008, 66, 2314–2317. [Google Scholar] [CrossRef] [PubMed]
- Verweij, J.P.; Toxopeus, E.E.; Fiocco, M.; Mensink, G.; van Merkesteyn, J.R. Success and survival of autotransplanted premolars and molars during short-term clinical follow-up. J. Clin. Periodontol. 2016, 43, 167–172. [Google Scholar] [CrossRef]
- Polson, A.M.; Hanes, P. The root surface and periodontal regeneration. In Periodontal Regeneration: Current Status and Concepts Quintessence; Quintessence Publishing: Chicago, IL, USA, 1994; pp. 41–52. [Google Scholar]
- Andreasen, J. Periodontal healing after replantation and autotransplantation of incisors in monkeys. Int. J. Oral Surg. 1981, 10, 54–61. [Google Scholar] [CrossRef]
- Ivanovski, S.; Gronthos, S.; Shi, S.; Bartold, P. Stem cells in the periodontal ligament. Oral Dis. 2006, 12, 358–363. [Google Scholar] [CrossRef]
- Marques-Ferreira, M.; Rabaça-Botelho, M.-F.; Carvalho, L.; Oliveiros, B.; Palmeirão-Carrilho, E.-V. Autogenous tooth transplantation: Evaluation of pulp tissue regeneration. Med. Oral Patol. Oral Y Cir. Bucal 2011, 16, e984–e989. [Google Scholar] [CrossRef]
- Klokkevold, P.R. Current status of dental implants: A periodontal perspective. Int. J. Oral Maxillofac. Implant. 2000, 15, 56–65. [Google Scholar]
- Lundberg, T.; Isaksson, S. A clinical follow-up study of 278 autotransplanted teeth. Br. J. Oral Maxillofac. Surg. 1996, 34, 181–185. [Google Scholar] [CrossRef]
- Cate, A.T.; Deporter, D. The degradative role of the fibroblast in the remodelling and turnover of collagen in soft connective tissue. Anat. Rec. 1975, 182, 1–13. [Google Scholar] [CrossRef]
- Yoshino, K.; Kariya, N.; Namura, D.; Noji, I.; Mitsuhashi, K.; Kimura, H.; Fukuda, A.; Kikukawa, I.; Hayashi, T.; Yamazaki, N.; et al. Risk factors affecting third molar autotransplantation in males: A retrospective survey in dental clinics. J. Oral Rehabil. 2012, 39, 821–829. [Google Scholar] [CrossRef] [PubMed]
- Tsukiboshi, M. Autotransplantation of teeth: Requirements for predictable success. Dent. Traumatol. 2002, 18, 157–180. [Google Scholar] [CrossRef] [PubMed]
- Andreasen, J.; Hjørting-Hansen, E.; Jølst, O. A clinical and radiographic study of 76 autotransplanted third molars. Eur. J. Oral Sci. 1970, 78, 512–523. [Google Scholar] [CrossRef] [PubMed]
- Mendes, R.A.; Rocha, G. Mandibular third molar autotransplantation-literature review with clinical cases. J. Can. Dent. Assoc. 2004, 70, 761–766. [Google Scholar]
- Cohen, A.S.; Shen, T.; Pogrel, M.A. Transplanting teeth successfully: Autografts and allografts that work. J. Am. Dent. Assoc. 1995, 126, 481–485. [Google Scholar] [CrossRef]
- Schatz, J.-P.; Joho, J.-P. Long-term clinical and radiologic evaluation of autotransplanted teeth. Int. J. Oral Maxillofac. Surg. 1992, 21, 271–275. [Google Scholar] [CrossRef]
- Northway, W.M.; Konigsberg, S. Autogenic tooth transplantation the “state of the art”. Am. J. Orthod. 1980, 77, 146–162. [Google Scholar] [CrossRef]
- Yoon, Y.; Kim, Y.-G.; Suh, J.-Y.; Lee, J.-M. The prognosis of autotransplanted tooth on molar region: 5 years follow up cases. Oral Biol. Res. 2017, 41, 147–152. [Google Scholar] [CrossRef]
- Sugai, T.; Yoshizawa, M.; Kobayashi, T.; Ono, K.; Takagi, R.; Kitamura, N.; Okiji, T.; Saito, C. Clinical study on prognostic factors for autotransplantation of teeth with complete root formation. Int. J. Oral Maxillofac. Surg. 2010, 39, 1193–1203. [Google Scholar] [CrossRef]
- Almpani, K.; Papageorgiou, S.N.; Papadopoulos, M.A. Autotransplantation of teeth in humans: A systematic review and meta-analysis. Clin. Oral Investig. 2015, 19, 1157–1179. [Google Scholar] [CrossRef]
- Tsukiboshi, M.; Yamauchi, N.; Tsukiboshi, Y. Long-term outcomes of autotransplantation of teeth: A case series. J. Endod. 2019, 45, S72–S83. [Google Scholar] [CrossRef] [PubMed]
- Inoue, T. Osteogenic activity of periodontal ligament rat incisor, in vivo and in vitro. J. Dent. Res. 2019, 67, 401. [Google Scholar]
- Tsukiboshi, M.; Tsukiboshi, T. Bone morphology after delayed tooth replantation–case series. Dent. Traumatol. 2014, 30, 477–483. [Google Scholar] [CrossRef] [PubMed]
- Schwartz, O.; Bergmann, P.; Klausen, B. Autotransplantation of human teeth: A life-table analysis of prognostic factors. Int. J. Oral Surg. 1985, 14, 245–258. [Google Scholar] [CrossRef]
- Kallu, R.; Vinckier, F.; Politis, C.; Mwalili, S.; Willems, G. Tooth transplantations: A descriptive retrospective study. Int. J. Oral Maxillofac. Surg. 2005, 34, 745–755. [Google Scholar] [CrossRef] [PubMed]
- Van Westerveld, K.; Verweij, J.; Toxopeus, E.; Fiocco, M.; Mensink, G.; van Merkesteyn, J. Long-term outcomes 1–20 years after autotransplantation of teeth: Clinical and radiographic evaluation of 66 premolars and 8 molars. Br. J. Oral Maxillofac. Surg. 2019, 57, 666–671. [Google Scholar] [CrossRef]
- Andreasen, J.; Paulsen, H.; Yu, Z.; Bayer, T. A long-term study of 370 autotransplanted premolars. Part IV. Root development subsequent to transplantation. Eur. J. Orthod. 1990, 12, 38–50. [Google Scholar] [CrossRef]
- Andreasen, J.; Paulsen, H.; Yu, Z.; Bayer, T.; Schwartz, O. A long-term study of 370 autotransplanted premolars. Part II. Tooth survival and pulp healing subsequent to transplantation. Eur. J. Orthod. 1990, 12, 14–24. [Google Scholar] [CrossRef]
- Raikar, S.; Talukdar, P.; Kumari, S.; Panda, S.; Oommen, V.; Prasad, A. Factors affecting the survival rate of dental implants: A retrospective study. J. Int. Soc. Prev. Community Dent. 2017, 7, 351. [Google Scholar] [CrossRef]
- Kokai, S.; Kanno, Z.; Koike, S.; Uesugi, S.; Takahashi, Y.; Ono, T.; Soma, K. Retrospective study of 100 autotransplanted teeth with complete root formation and subsequent orthodontic treatment. Am. J. Orthod. Dentofac. Orthop. 2015, 148, 982–989. [Google Scholar] [CrossRef]
- Czochrowska, E.M.; Stenvik, A.; Album, B.; Zachrisson, B.U. Autotransplantation of premolars to replace maxillary incisors: A comparison with natural incisors. Am. J. Orthod. Dentofac. Orthop. 2000, 118, 592–600. [Google Scholar] [CrossRef] [PubMed]
- Kobayashi, T.; Blatz, M.B. Autotransplantation: An Alternative to Dental Implants—Case Report with 4-Year Follow-Up. Compendium 2018, 39, 6. [Google Scholar]
- Paulsen, H.U.; Andreasen, J.O. Eruption of premolars subsequent to autotransplantation. A longitudinal radiographic study. Eur. J. Orthod. 1998, 20, 45–55. [Google Scholar] [CrossRef] [PubMed]


| Sex | Number | Age (Years) | Age Range |
|---|---|---|---|
| All | 111 | 36.5 ± 13.0 | 13–65 |
| Male | 56 (50.5) | 39.3 ± 13.9 | 13–63 |
| Female | 55 (49.5) | 33.7 ± 11.7 | 15–65 |
| Recipient Site | Donor Site | |
|---|---|---|
| Incisor | 1 (1) | 1 (1) |
| Canine | 0 | 0 |
| Premoalr | 2 (2) | 2 (2) |
| First Molar | 48 (43) | 0 |
| Second Molar | 60 (54) | 4 (3) |
| Third Molar | 0 | 104 (94) |
| Variable | Overall | Causes of Extraction | Opposing Teeth | Age | ||||||
|---|---|---|---|---|---|---|---|---|---|---|
| Overall (n = 111) | Caries (n = 21) | Periapical Lesion (n = 35) | Crack (n = 30) | Crown Fracture (n = 30) | Periodontitis (n = 8) | Natural Teeth (n = 87) | Prosthesis (n = 24) | Under 30 (n = 47) | Over 30 (n = 64) | |
| Period (year) | ||||||||||
| 1 | 100.0 | 100.0 | 100.0 | 100.0 | 100.0 | 100.0 | 100.0 | 100.0 | 100.0 | 100.0 |
| 2 | 91.7 | 100.0 | 83.9 | 93.8 | 91.7 | 100.0 | 91.5 | 92.3 | 96.4 | 88.1 |
| 3 | 91.7 | 100.0 | 83.9 | 93.8 | 91.7 | 100.0 | 91.5 | 92.3 | 96.4 | 88.1 |
| 4 | 91.7 | 100.0 | 83.9 | 93.8 | 91.7 | 100.0 | 91.5 | 92.3 | 96.4 | 88.1 |
| 5 | 83.1 | 100.0 | 83.9 | 67.0 | 91.7 | 100.0 | 81.8 | 92.3 | 96.4 | 74.6 |
| 6 | 66.9 | 50.0 | 50.3 | 67.0 | 91.7 | 100.0 | 64.5 | 92.3 | 66.1 | 67.1 |
| 7 | 60.2 | 50.0 | 50.3 | 67.0 | 45.8 | 100.0 | 57.3 | 92.3 | 66.1 | 55.9 |
| 8 | 40.1 | 50.0 | 33.6 | 67.0 | 0.0 | 50.0 | 35.8 | 92.3 | 16.5 | 55.9 |
| 9 | 40.1 | 50.0 | 33.6 | 67.0 | 50.0 | 35.8 | 92.3 | 55.9 | ||
| 10 | 30.1 | 0.0 | 33.6 | 67.0 | 50.0 | 35.8 | 0.0 | 42.0 | ||
| 11 | 30.1 | 33.6 | 67.0 | 50.0 | 35.8 | 42.0 | ||||
| 12 | 30.1 | 67.0 | 50.0 | 35.8 | 42.0 | |||||
| 13 | 30.1 | 50.0 | 35.8 | 42.0 | ||||||
| p-value | 0.772 | 0.576 | 0.555 | 0.560 | 0.407 | 0.831 | 0.692 | |||
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2022 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Park, J.-H.; Kim, Y.-G.; Suh, J.-Y.; Jin, M.-U.; Lee, J.-M. Long-Term Survival Rate of Autogenous Tooth Transplantation: Up to 162 Months. Medicina 2022, 58, 1517. https://doi.org/10.3390/medicina58111517
Park J-H, Kim Y-G, Suh J-Y, Jin M-U, Lee J-M. Long-Term Survival Rate of Autogenous Tooth Transplantation: Up to 162 Months. Medicina. 2022; 58(11):1517. https://doi.org/10.3390/medicina58111517
Chicago/Turabian StylePark, Jin-Han, Yong-Gun Kim, Jo-Young Suh, Myoung-Uk Jin, and Jae-Mok Lee. 2022. "Long-Term Survival Rate of Autogenous Tooth Transplantation: Up to 162 Months" Medicina 58, no. 11: 1517. https://doi.org/10.3390/medicina58111517
APA StylePark, J.-H., Kim, Y.-G., Suh, J.-Y., Jin, M.-U., & Lee, J.-M. (2022). Long-Term Survival Rate of Autogenous Tooth Transplantation: Up to 162 Months. Medicina, 58(11), 1517. https://doi.org/10.3390/medicina58111517






