Energy Devices for Clipless–Sutureless Laparoscopic Appendectomy: A Systematic Review and Meta-Analysis on Utility and Safety
Abstract
:1. Introduction
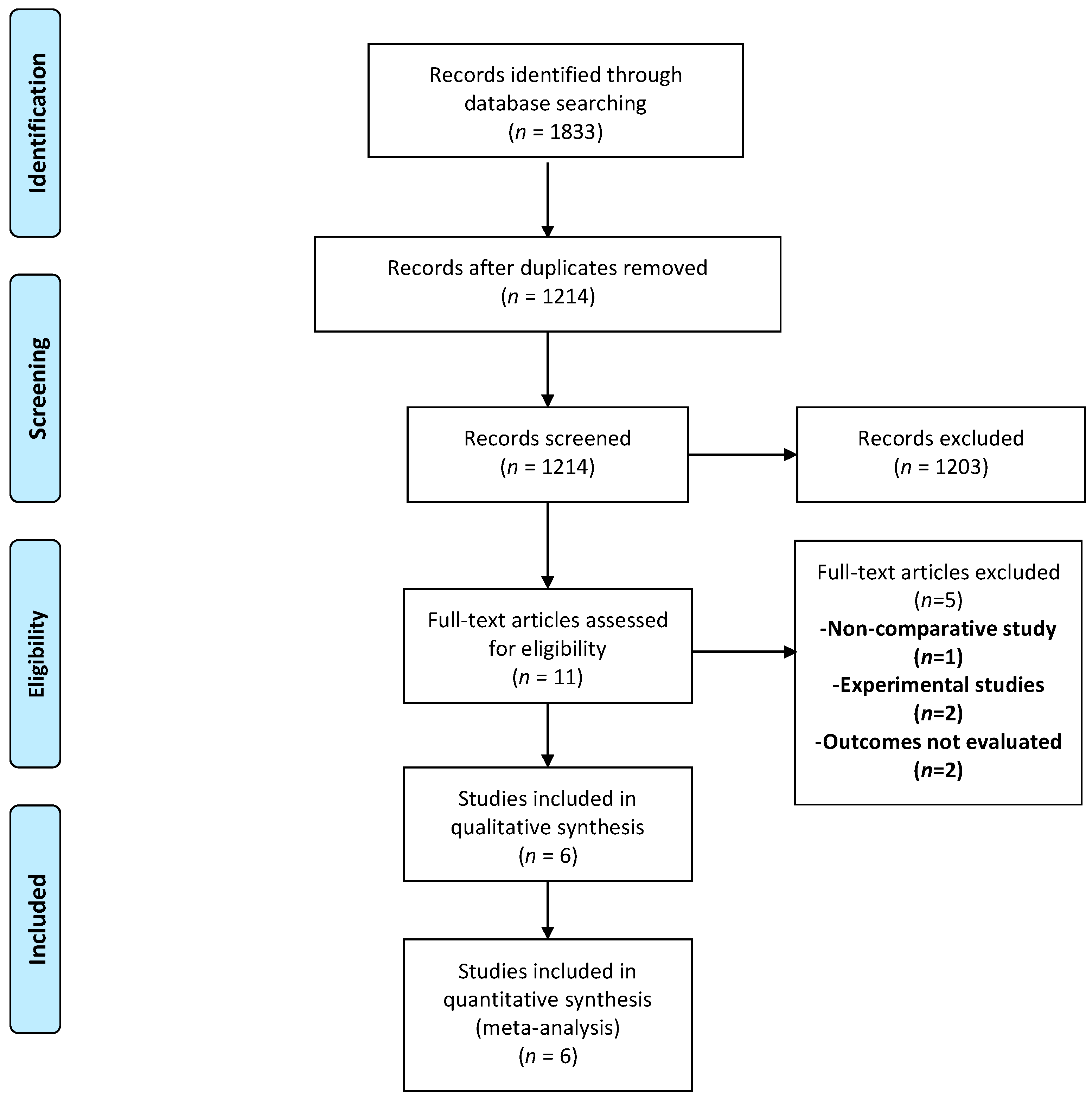
2. Materials and Methods
2.1. Search Strategy
2.2. Eligibility Criteria
2.3. Data Synthesis
2.4. Quality Assessment
2.5. Statistical Analysis
3. Results
3.1. Study Characteristics
3.2. Summary of the Included Studies
- Aydogan et al., 2009 [23]
- Sucullu et al., 2009 [25]
- Lee et al., 2014 [26]
- Park et al., 2019 [27]
- Gupta et al., 2020 [13]
- Pogorelić et al., 2021 [24]
3.3. Quality Assessment
3.4. Meta-Analysis
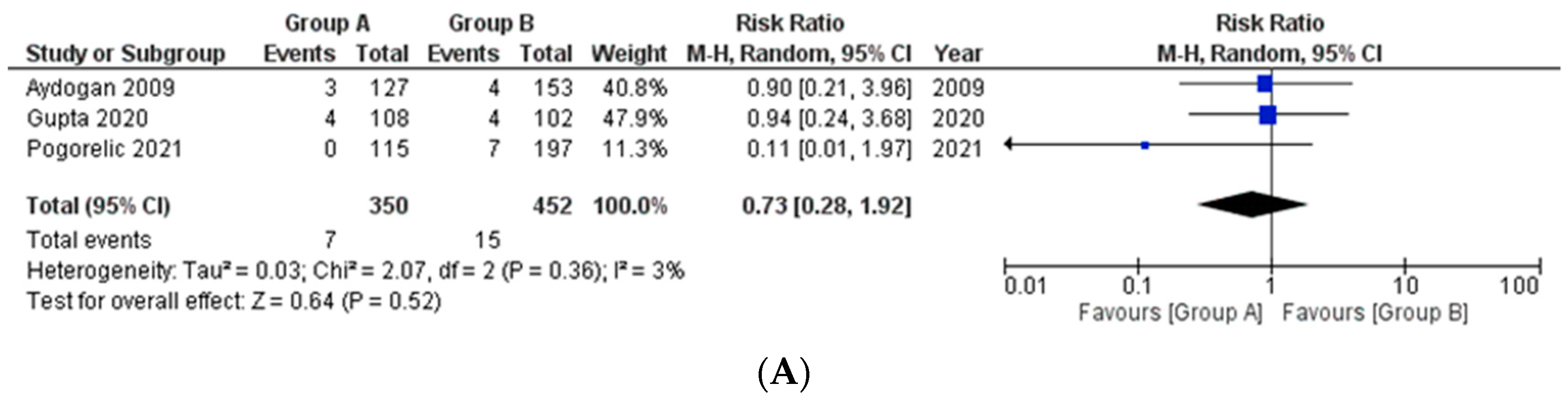
- (a)
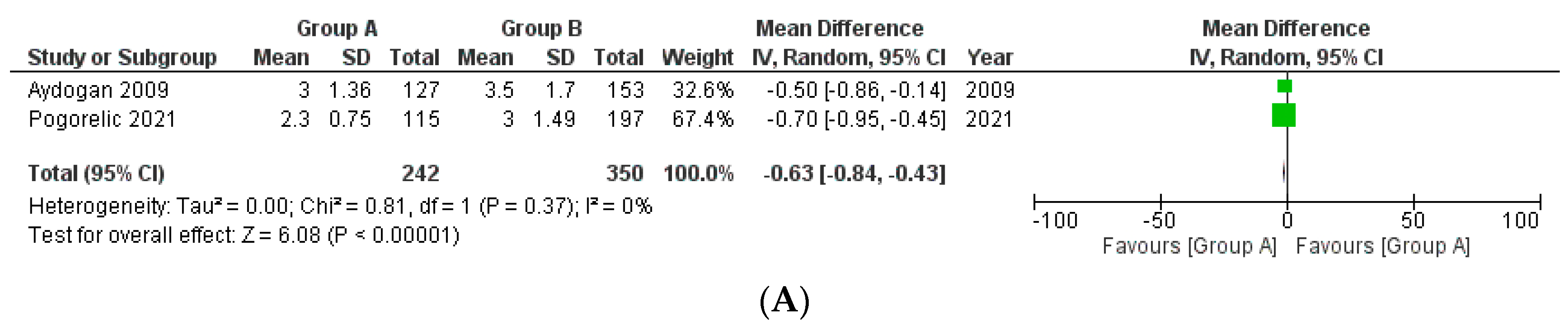
- Surgical site infections (SSI)/Intra-abdominal collections
- (b)
- Postoperative Ileus
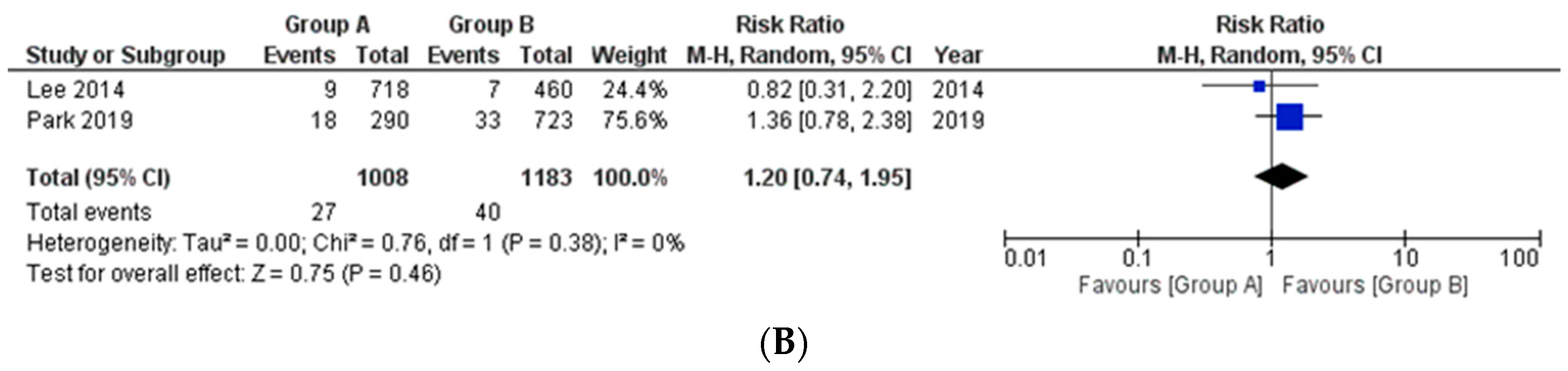
- (c)
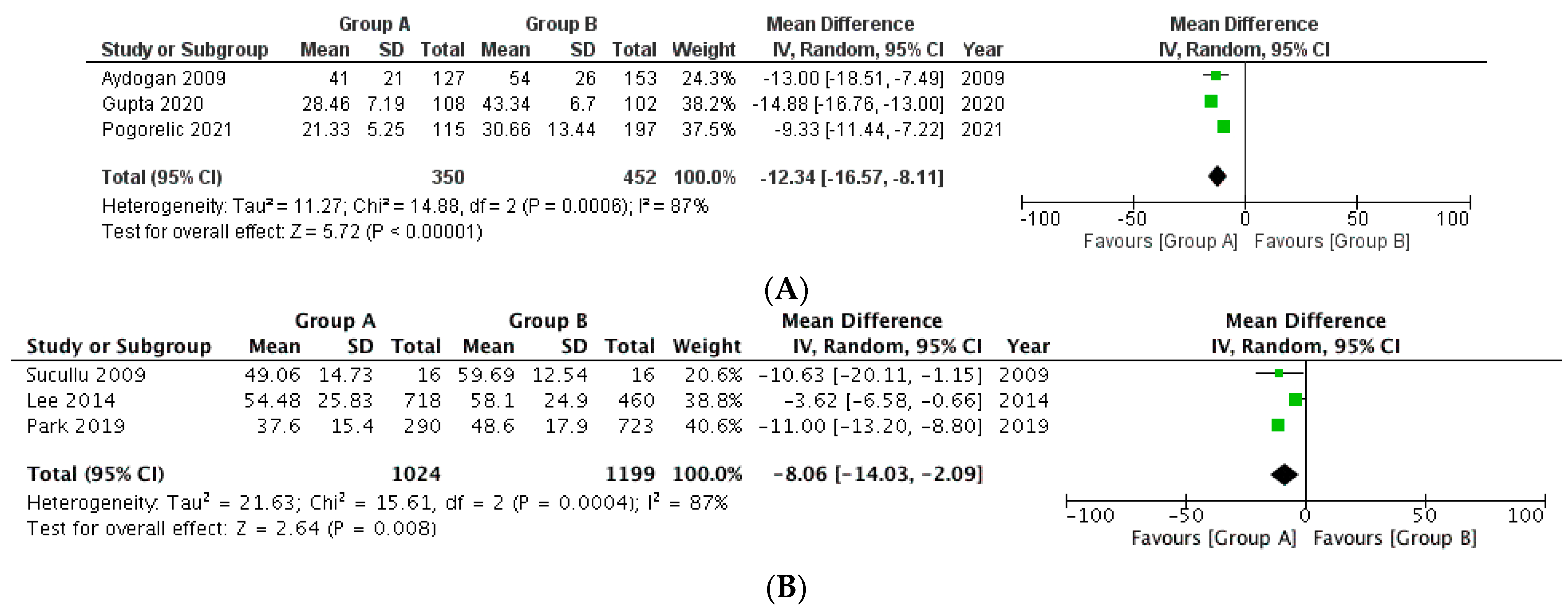
- Operative Time
- (d)
- Hospital stay
4. Discussion
4.1. Application to Clinical Practice
4.2. Strengths and Limitations
5. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Conflicts of Interest
References
- Schier, F. Laparoscopic appendectomy with 1.7-mm instruments. Pediatr. Surg. Int. 1998, 14, 142–143. [Google Scholar] [CrossRef] [PubMed]
- Flores, J.V.; Avila, A.L.V.; Cruz, I.D.A.; Jimenez, S.D.L.; Pacheco, J.S.; Ancona, J.F.N.; Valdes, J.V.; Roman, E.B. Zaragoza technique of laparoscopic appendicectomy. Ann. Med. Surg. 2021, 65, 102331. [Google Scholar] [CrossRef] [PubMed]
- Neogi, S.; Banerjee, A.; Panda, S.S.; Ratan, S.K.; Narang, R.J. Laparoscopic versus open appendicectomy for complicated appendicitis in children: A systematic review and meta-analysis. J Pediatr. Surg. 2022, 57, 394–405. [Google Scholar] [CrossRef]
- Sauerland, S.; Jaschinski, T.; Neugebauer, E.A. Laparoscopic versus open surgery for suspected appendicitis. Cochrane Database Syst. Rev. 2010, 10, CD001546. [Google Scholar] [CrossRef]
- Krisher, S.L.; Browne, A.; Dibbins, A.; Tkacz, N.; Curci, M. Intra-abdominal Abscess After Laparoscopic Appendectomy for Perforated Appendicitis. Arch. Surg. 2001, 136, 438–441. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Mannu, S.G.; Sudul, M.K.; Bettencourt-Silva, J.H.; Cumber, E.; Li, F.; Clark, A.B.; Loke, Y.K. Closure methods of the appendix stump for complications during laparoscopic appendectomy. Cochrane Database Syst. Rev. 2017, 11, CD006437. [Google Scholar] [CrossRef]
- Slakey, D.P. Laparoscopic liver resection using a bipolar vessel-sealing device: LigaSure. HPB 2008, 10, 253–255. [Google Scholar] [CrossRef] [Green Version]
- Meurisse, M.; Defechereux, T.; Maweja, S.; Degauque, C.; Vandelaer, M.; Hamoir, E. Evaluation of the ultracision dissector in thyroid surgery: Prospective randomized study. Ann. Chir. 2000, 125, 468–472. [Google Scholar] [CrossRef]
- Pons, Y.; Gauthier, J.; Ukkola-Pons, E.; Clément, P.; Roguet, E.; Poncet, J.L.; Conessa, C. Comparison of LigaSure vessel sealing system, harmonic scalpel, and conventional hemostasis in total thyroidectomy. Otolaryngol. Head Neck Surg. 2009, 141, 496–501. [Google Scholar] [CrossRef]
- Upadhyaya, A.; Hu, T.; Meng, Z.; Li, X.; He, X.; Tian, W.; Jia, Q.; Tan, J. Harmonic versus LigaSure hemostasis technique in thyroid surgery: A meta-analysis. Biomed. Rep. 2016, 5, 221–227. [Google Scholar] [CrossRef]
- Charalambides, M.; Afxentiou, T.; Pellino, G.; Powar, M.P.; Fearnhead, N.S.; Davies, R.J.; Wheeler, J.; Simillis, C. A systematic review and network meta-analysis comparing energy devices used in colorectal surgery. Tech. Coloproctol. 2022, 26, 413–423. [Google Scholar] [CrossRef] [PubMed]
- Khanna, S.; Khurana, S.; Vij, S. No clip, no ligature laparoscopic appendectomy. Surg. Laparosc. Endosc. Percutan. Tech. 2004, 14, 201–203. [Google Scholar] [CrossRef] [PubMed]
- Gupta, V.; Singh, P.S.; Singh, P.S.; Bansal, M.; Pandey, A. Sutureless Appendectomy by Using Harmonic Scalpel: Is It Possible? J. Laparoendosc. Adv. Surg. Tech. A 2020, 30, 429–432. [Google Scholar] [CrossRef] [PubMed]
- Raza, V.F.; Arshad, D.; Bhatti, L.A.; Talal, A.; Ahmad, S.; Khan, K.J. Laparoscopic harmonic appendectomy: A novel approach. Glob. J. Surg. 2020, 8, 32–36. [Google Scholar]
- Moher, D.; Liberati, A.; Tetzlaff, J.; Altman, D.G. Preferred reporting items for systematic reviews and meta-analyses: The PRISMA statement. PLoS Med. 2009, 6, e1000097. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Downs, S.H.; Black, N. The feasibility of creating a checklist for the assessment of the methodological quality both of randomised and non-randomised studies of health care interventions. J. Epidemiol. Community Health 1998, 52, 377–384. [Google Scholar] [CrossRef] [Green Version]
- Landis, J.R.; Koch, G.G. The measurement of observer agreement for categorical data. Biometrics 1997, 33, 159–174. [Google Scholar] [CrossRef] [Green Version]
- Yang, H.R.; Wang, Y.C.; Chung, P.K.; Jeng, L.B.; Chen, R.J. Laparoscopic appendectomy using the LigaSure Vessel Sealing System. J. Laparoendosc. Adv. Surg. Tech. A 2005, 15, 353–356. [Google Scholar] [CrossRef]
- Yavuz, A.; Bulus, H.; Taş, A.; Aydın, A. Evaluation of Stump Pressure in Three Types of Appendectomy: Harmonic Scalpel, LigaSure, and Conventional Technique. J. Laparoendosc. Adv. Surg. Tech. A 2016, 26, 950–953. [Google Scholar] [CrossRef]
- Gündüz, U.R.; Karakoyun, R.; Özdemir, Ş.; ÇalıŞ, H.; Habibi, M.; Öner, O.Z. The feasibility of bipolar tissue sealer for appendix stump closure. Minim. Invasive Ther. Allied Technol. 2015, 24, 377–380. [Google Scholar] [CrossRef]
- Davila, D.; Russek, K.; Franklin, M.E., Jr. Laparoscopic appendectomy: Vascular control of the appendicular artery using monopolar cauterization versus clips. J. Laparoendosc. Adv. Surg. Tech. A 2012, 22, 165–167. [Google Scholar] [CrossRef] [PubMed]
- Qaiser, M.U.; Nazir, A.; Khan, M.S.; Butt, H.K.; Anwar, M. Comparison of Ultrasonic Dissection and Suture Ligation for Mesoappendix in Laparoscopic Appendectomy. Cureus 2021, 13, e14316. [Google Scholar] [CrossRef] [PubMed]
- Aydogan, F.; Saribeyoglu, K.; Simsek, O.; Salihoglu, Z.; Carkman, S.; Salihoglu, T.; Karatas, A.; Baca, B.; Kucuk, O.; Yavuz, N.; et al. Comparison of the electrothermal vessel-sealing system versus endoclip in laparoscopic appendectomy. J. Laparoendosc. Adv. Surg. Tech. A 2009, 19, 375–378. [Google Scholar] [CrossRef]
- Pogorelić, Z.; Beara, V.; Jukić, M.; Rashwan, H.; Šušnjar, T. A new approach to laparoscopic appendectomy in children-clipless/sutureless Harmonic scalpel laparoscopic appendectomy. Langenbecks Arch. Surg. 2022, 407, 779–787. [Google Scholar] [CrossRef] [PubMed]
- Sucullu, I.; Filiz, A.I.; Kurt, Y.; Yilmaz, I.; Yildiz, M. The effects of LigaSure on the laparoscopic management of acute appendicitis: "LigaSure assisted laparoscopic appendectomy". Surg. Laparosc. Endosc. Percutan Tech. 2009, 19, 333–335. [Google Scholar] [CrossRef] [PubMed]
- Lee, J.S.; Hong, T.H. Comparison of various methods of mesoappendix dissection in laparoscopic appendectomy. J. Laparoendosc. Adv. Surg. Tech. A 2014, 24, 28–31. [Google Scholar] [CrossRef] [PubMed]
- Park, J.; Suh, S.W.; Kim, M.K.; Park, B.K.; Lee, S.E.; Kim, J.W.; Park, J.M.; Choi, Y.S.; Kim, B.G.; Park, Y.G. Less Pain and Reduced Risk of Early Postoperative Ileus After Clipless Versus Conventional Laparoscopic Appendectomy. Surg. Laparosc. Endosc. Percutan. Tech. 2019, 29, 543–547. [Google Scholar] [CrossRef] [PubMed]
- Addiss, D.G.; Shaffer, N.; Fowler, B.S.; Tauxe, R.V. The epidemiology of appendicitis and appendectomy in the United States. Am. J. Epidemiol. 1990, 132, 910–925. [Google Scholar] [CrossRef]
- Wilms, I.M.; Hoog, D.E.; Visser, D.C.; Janzing, H.M. Appendectomy versus antibiotic treatment for acute appendicitis. Cochrane Database Syst. Rev. 2011, 11, CD008359. [Google Scholar] [CrossRef]
- Santacroce, L.; Geibel, J.; Ochoa, J.B.; Hines, O.J.; Talavera, F. Appendectomy. 2017. Available online: http://emedicine.medscape.com/article/195778-overview (accessed on 18 June 2022).
- Dingemann, J.; Metzelder, M.L.; Szavay, P.O. Current status of laparoscopic appendectomy in children: A nation wide survey in Germany. Eur. J. Pediatr. Surg. 2013, 23, 226–233. [Google Scholar] [CrossRef]
- Kazemier, G.; Hof, K.H.; Saad, S.; Bonjer, H.J.; Sauerland, S. Securing the appendiceal stump in laparoscopic appendectomy: Evidence for routine stapling? Surg. Endosc. 2006, 20, 1473–1476. [Google Scholar] [CrossRef] [PubMed]
- Low, Z.X.; Bonney, G.K.; So, J.B.Y.; Loh, D.L.; Ng, J.J. Laparoscopic versus open appendectomy in pediatric patients with complicated appendicitis: A meta-analysis. Surg. Endosc. 2019, 33, 4066–4077. [Google Scholar] [CrossRef] [PubMed]
- Shaikh, F.M.; Bajwa, R.; McDonnell, C.O. Management of appendiceal stump in laparoscopic appendectomy—Clips or ligature: A systematic review and meta-analysis. J. Laparoendosc. Adv. Surg. Tech. A 2015, 25, 21–27. [Google Scholar] [CrossRef]
- Nataraja, R.; Loukogeorgakis, S.P.; Sherwood, W.J.; Clark, S.A.; Haddad, M.J. The incidence of intraabdominal abscess formation following laparoscopic appendicectomy in children: A systematic review and meta-analysis. J. Laparoendosc. Adv. Surg. Tech. A 2013, 23, 795–802. [Google Scholar] [CrossRef] [PubMed]
- Li, X.; Zhang, J.; Sang, L.; Zhang, W.; Chu, Z.; Li, X.; Liu, Y. Laparoscopic versus conventional appendectomy—A meta-analysis of randomized controlled trials. BMC Gastroenterol. 2010, 10, 129. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Botteri, E.; Podda, M.; Arezzo, A.; Vettoretto, N.; Sartori, A.; Agrusa, A.; Allaix, M.E.; Anania, G.; Contul, R.B.; Caracino, V.; et al. Current status on the adoption of high energy devices in Italy: An Italian Society for Endoscopic Surgery and New Technologies (SICE) national survey. Surg. Endosc. 2021, 35, 6201–6211. [Google Scholar] [CrossRef]
- Sisko, A.M.; Keehan, S.P.; Poisal, J.A.; Cuckler, G.A.; Smith, S.D.; Madison, A.J.; Rennie, K.E.; Hardesty, J.C. National Health Expenditure Projections, 2016-25: Price Increases, Aging Push Sector to 20 Percent Of Economy. Health Aff.(Millwood). 2019, 38, 491–501. [Google Scholar] [CrossRef]
- Kim, S.-H.; Kim, H.-Y.; Lee, S.-H.; Yang, K.; Park, B.-S.; Choi, B.-H.; Jung, H.J. Recuding Supply Cost by Standardization of Surgical Equipment in Laparoscopic Appendectomy. Qual. Manag. Health Care 2021, 30, 259–266. [Google Scholar] [CrossRef]
- DeMare, A.M.; Luehmann, N.C.; Kawak, S.; Abbott, E.E.; Long, J.; Akay, B.; Brahmamdam, P.; Iacco, A.A.; Novotny, N.M. Cost-Effective Approach to the Laparoscopic Appendectomy: Balancing Disposable Instrument Cost With Operative Time. Am. Surg. 2020, 86, 715–720. [Google Scholar] [CrossRef]
- Reighard, C.; Junaid, S.; Jackson, W.M.; Arif, A.; Waddington, H.; Whitehouse, A.J.O.; Ing, C. Anesthetic Exposure During Childhood and Neurovedelopmental Outcomes: A Systematic Review and Meta-analysis. JAMA Netw. Open 2022, 5, 42217427. [Google Scholar] [CrossRef]
| Author | Study Design | Sample Size (n) | Gangrenous/Perforated Appendicitis (n) | Converted to Open Approach (n) | |||
|---|---|---|---|---|---|---|---|
| A | B | A | B | A | B | ||
| Aydoganet al., 2009 [23] | Retro | 127 | 153 | 30 | 38 | 12 | 17 |
| Suculluet al., 2009 [25] | Pro | 16 | 16 | 3 | 3 | 0 | 0 |
| Lee et al., 2014 [26] | Retro | 718 * | 460 | 126 | 67 | 1 | 1 |
| Park et al., 2019 [27] | Retro | 290 | 723 | 21 | 35 | 0 | 1 |
| Gupta et al., 2011 [13] | Ambi | 108 | 102 | ** | ** | - | - |
| Pogorelić et al., 2021 [24] | Pro | 115 | 197 | 52 | 96 | - | - |
| Assessment by Observer 1 | ||||||
|---|---|---|---|---|---|---|
| Study | Reporting | External Validity | Internal Validity- Bias | Internal Validity-Confounding | Power | Total Scores |
| Aydogan et al., 2009 [23] | 7 | 3 | 4 | 2 | 0 | 16 |
| Sucullu et al., 2009 [25] | 8 | 3 | 4 | 3 | 0 | 18 |
| Lee et al., 2014 [26] | 8 | 3 | 4 | 2 | 0 | 17 |
| Park et al., 2019 [27] | 8 | 3 | 5 | 3 | 0 | 19 |
| Gupta et al., 2020 [13] | 6 | 3 | 4 | 1 | 0 | 14 |
| Pogorelić et al., 2021 [24] | 8 | 3 | 5 | 3 | 0 | 19 |
| Assessment by observer 2 | ||||||
| Study | Reporting | External validity | Internal validity- bias | Internal validity-confounding | Power | Total scores |
| Aydogan et al., 2009 [23] | 8 | 3 | 4 | 3 | 0 | 18 |
| Sucullu et al., 2009 [25] | 7 | 3 | 5 | 3 | 0 | 18 |
| Lee et al., 2014 [26] | 8 | 3 | 3 | 3 | 0 | 17 |
| Park et al., 2019 [27] | 9 | 3 | 5 | 3 | 0 | 20 |
| Gupta et al., 2020 [13] | 7 | 3 | 4 | 1 | 0 | 15 |
| Pogorelić et al., 2021 [24] | 8 | 3 | 5 | 3 | 0 | 19 |
| Cumulative assessment | ||||||
| Study | Rater 1 | Rater 2 | Mean | Kappa value | p | |
| Aydogan et al., 2009 [23] | 16 | 18 | 17 | 0.8918 | <0.0001 | |
| Sucullu et al., 2009 [25] | 18 | 18 | 18 | |||
| Lee et al., 2014 [26] | 17 | 17 | 17 | |||
| Park et al., 2019 [27] | 19 | 20 | 19.5 | |||
| Gupta et al., 2020 [13] | 14 | 15 | 14.5 | |||
| Pogorelić et al., 2021 [24] | 19 | 19 | 19 | |||
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2022 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Singh, A.; Anand, S.; Pakkasjärvi, N.; Verma, A.; Bajpai, M. Energy Devices for Clipless–Sutureless Laparoscopic Appendectomy: A Systematic Review and Meta-Analysis on Utility and Safety. Medicina 2022, 58, 1535. https://doi.org/10.3390/medicina58111535
Singh A, Anand S, Pakkasjärvi N, Verma A, Bajpai M. Energy Devices for Clipless–Sutureless Laparoscopic Appendectomy: A Systematic Review and Meta-Analysis on Utility and Safety. Medicina. 2022; 58(11):1535. https://doi.org/10.3390/medicina58111535
Chicago/Turabian StyleSingh, Apoorv, Sachit Anand, Niklas Pakkasjärvi, Ajay Verma, and Minu Bajpai. 2022. "Energy Devices for Clipless–Sutureless Laparoscopic Appendectomy: A Systematic Review and Meta-Analysis on Utility and Safety" Medicina 58, no. 11: 1535. https://doi.org/10.3390/medicina58111535






