Prevalence of Cardiovascular Risk Factors in Middle-Aged Lithuanian Men Based on Body Mass Index and Waist Circumference Group Results from the 2006–2016 Lithuanian High Cardiovascular Risk Prevention Program
Abstract
1. Introduction
2. Material and Methods
3. Results
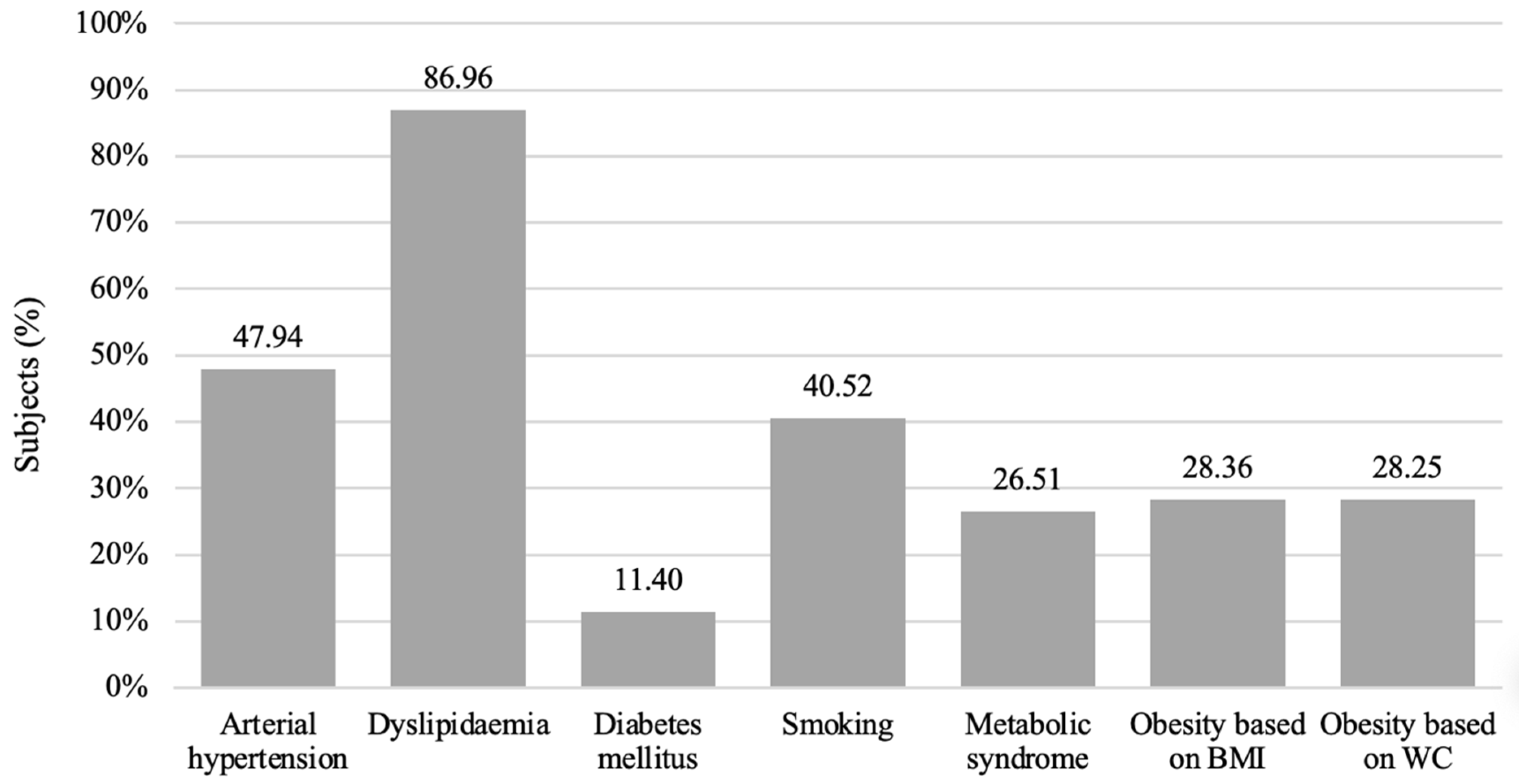
3.1. Sample Characteristics
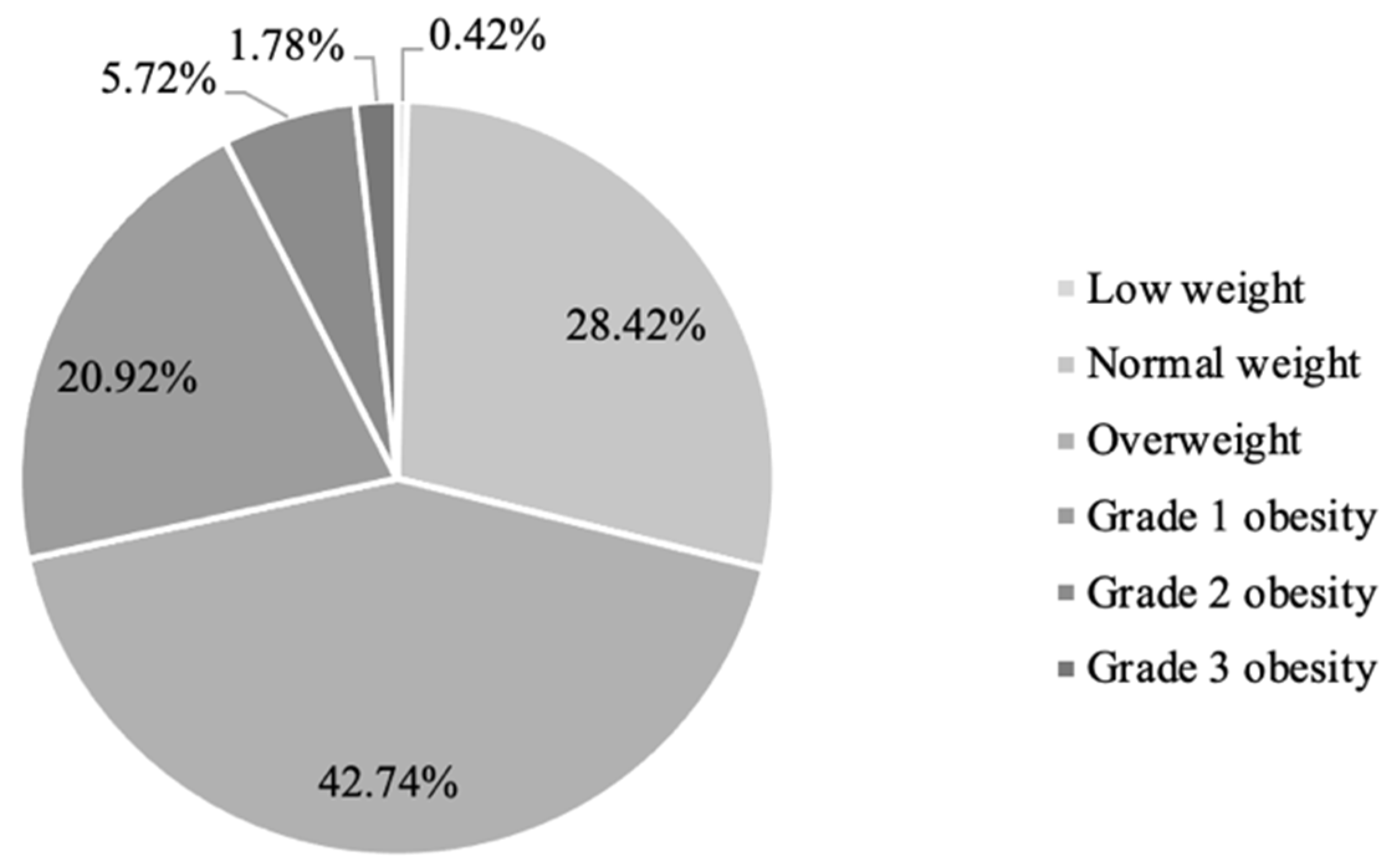
3.2. Characteristics of The Study Sample Based on BMI
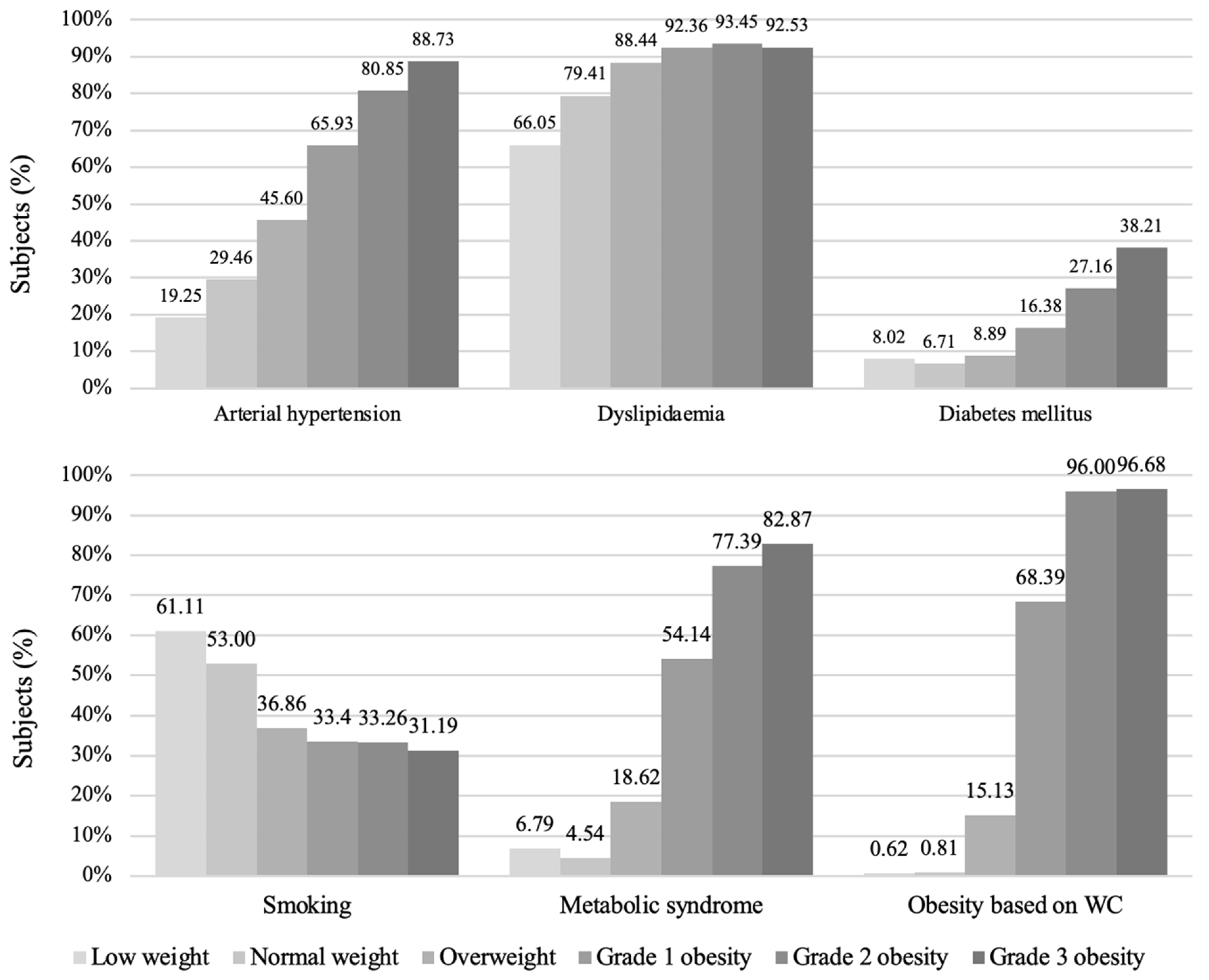
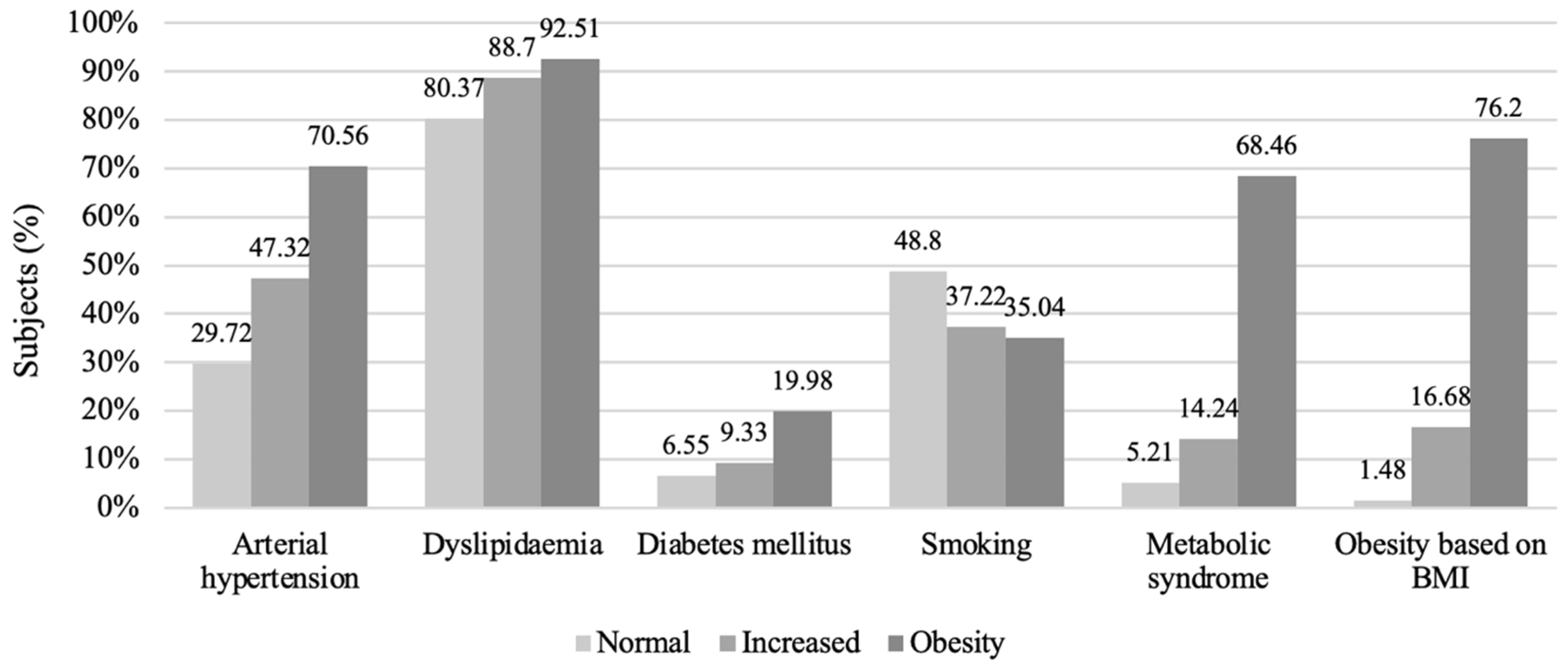
Cardiovascular Risk Factors in BMI Groups
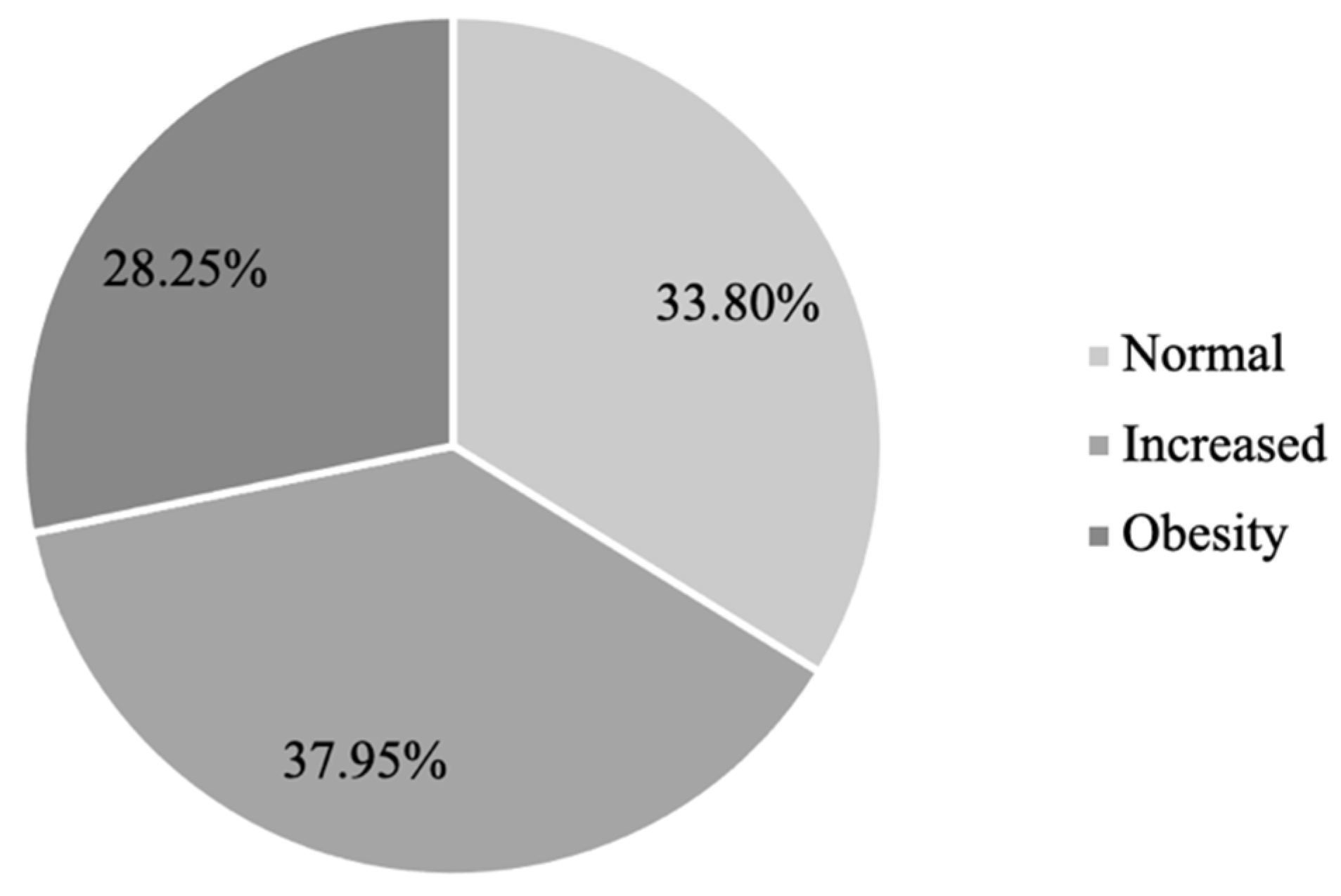
3.3. Characteristics of the Study Sample Based on WC
Prevalences of Cardiovascular Factors in WC Groups
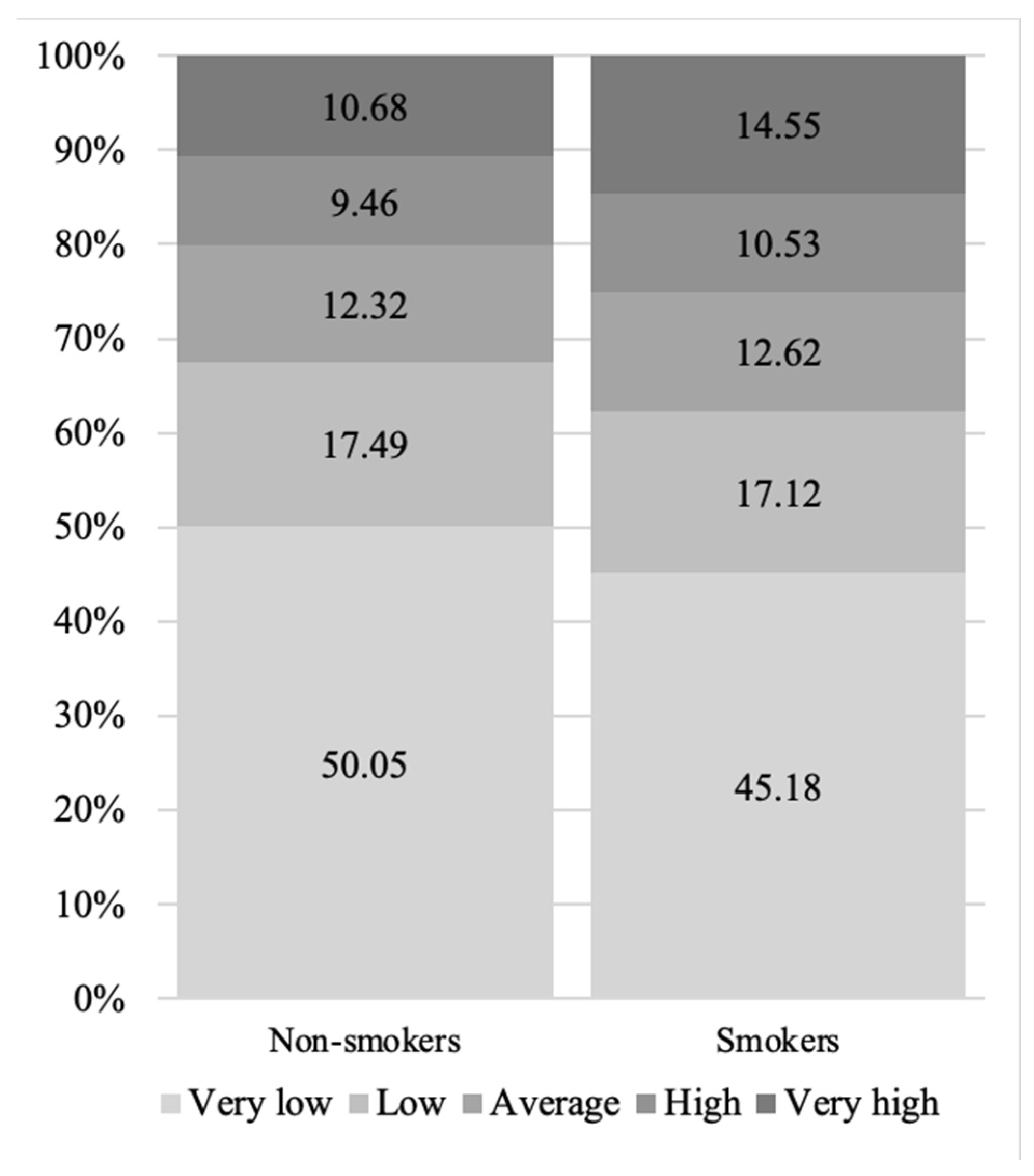
3.4. ABSI and Smoking
4. Discussion
5. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Conflicts of Interest
References
- World Health Organization. Global Health Observatory (GHO) Data. World Health Organization Website. Available online: https://www.who.int/data/gho (accessed on 11 October 2022).
- Janssen, F.; Bardoutsos, A.; Vidra, N. Obesity Prevalence in the Long-Term Future in 18 European Countries and in the USA. Obes. Facts 2020, 13, 514–527. [Google Scholar] [CrossRef]
- World Health Organization. Obesity and Overweight. World Health Organization Website. Available online: https://www.who.int/news-room/fact-sheets/detail/obesity-and-overweight (accessed on 11 October 2022).
- Hruby, A.; Hu, F.B. The Epidemiology of Obesity: A Big Picture. PharmacoEconomics 2014, 33, 673–689. [Google Scholar] [CrossRef] [PubMed]
- Lopez, A.D.; Adair, T. Is the long-term decline in cardiovascular-disease mortality in high-income countries over? Evidence from national vital statistics. Int. J. Epidemiol. 2019, 48, 1815–1823. [Google Scholar] [CrossRef]
- Mensah, G.A.; Wei, G.S.; Sorlie, P.D.; Fine, L.J.; Rosenberg, Y.; Kaufmann, P.G.; Mussolino, M.E.; Hsu, L.; Addou, E.; Engelgau, M.M.; et al. Decline in Cardiovascular Mortality. Circ. Res. 2017, 120, 366–380. [Google Scholar] [CrossRef] [PubMed]
- The Emerging Risk Factors Collaboration. Separate and combined associations of body-mass index and abdominal adiposity with cardiovascular disease: Collaborative analysis of 58 prospective studies. Lancet 2011, 377, 1085–1095. [Google Scholar] [CrossRef]
- Vidra, N.; Trias-Llimós, S.; Janssen, F. Impact of obesity on life expectancy among different European countries: Secondary analysis of population-level data over the 1975–2012 period. BMJ Open 2019, 9, e028086. [Google Scholar] [CrossRef]
- Kolip, P.; Lange, C. Gender inequality and the gender gap in life expectancy in the European Union. Eur. J. Public Health 2018, 28, 869–872. [Google Scholar] [CrossRef] [PubMed]
- Hossin, M.Z. The male disadvantage in life expectancy: Can we close the gender gap? Int. Health 2021, 13, 482–484. [Google Scholar] [CrossRef]
- Neeland, I.J.; Poirier, P.; Després, J.-P. Cardiovascular and Metabolic Heterogeneity of Obesity: Clinical Challenges and Implications for Management. Circulation 2018, 137, 1391–1406. [Google Scholar] [CrossRef] [PubMed]
- Visseren, F.L.J.; Mach, F.; Smulders, Y.M.; Carballo, D.; Koskinas, K.C.; Bäck, M.; Benetos, A.; Biffi, A.; Boavida, J.-M.; Capodanno, D.; et al. 2021 ESC Guidelines on cardiovascular disease prevention in clinical practice: Developed by the Task Force for cardio-vascular disease prevention in clinical practice with representatives of the European Society of Cardiology and 12 medical societies With the special contribution of the European Association of Preventive Cardiology (EAPC). Eur. Heart J. 2021, 42, 3227–3337. [Google Scholar] [CrossRef] [PubMed]
- Laucevičius, A.; Kasiulevičius, V.; Jatužis, D.; Žaneta, P.; Ryliškytė, L.; Rinkūnienė, E.; Badarienė, J.; Ypienė, A.; Gustienė, O.; Šlapikas, R. Lithuanian High Cardiovascular Risk (LitHiR) primary prevention programme-rationale and design. Semin. Cardiovasc. Med. 2012, 18, 1–6. [Google Scholar] [CrossRef]
- Krakauer, N.Y.; Krakauer, J.C. A New Body Shape Index Predicts Mortality Hazard Independently of Body Mass Index. PLoS ONE 2012, 7, e39504. [Google Scholar] [CrossRef] [PubMed]
- Lumley, T.; Diehr, P.; Emerson, S.; Chen, L. The importance of the normality assumption in large public health data sets. Annu. Rev. Public Health 2002, 23, 151–169. [Google Scholar] [CrossRef]
- Kutkienė, S. The Assessment and Modification of Dyslipidemias: Effects on Etiopathogenesis, the Prevention of Cardiovascular Diseases and the Relationship with other Atherosclerotic Risk Factors. Ph.D. Thesis, Vilnius University, Vilnius, Lithuania, 2018. (In Lithuanian). [Google Scholar]
- Nguyen, N.T.; Magno, C.P.; Lane, K.T.; Hinojosa, M.W.; Lane, J.S. Association of Hypertension, Diabetes, Dyslipidemia, and Metabolic Syndrome with Obesity: Findings from the National Health and Nutrition Examination Survey, 1999 to 2004. J. Am. Coll. Surg. 2008, 207, 928–934. [Google Scholar] [CrossRef]
- Sigit, F.S.; Tahapary, D.L.; Sartono, E.; Trompet, S.; Yazdanbakhsh, M.; Rosendaal, F.; de Mutsert, R. The Prevalence Of Metabolic Syndrome And Its Association With Body Fat Distribution In A Dutch And Indonesian Population. Atherosclerosis 2019, 287, 135–136. [Google Scholar] [CrossRef]
- Paccaud, F.; Schlüter-Fasmeyer, V.; Wietlisbach, V.; Bovet, P. Dyslipidemia and abdominal obesity: An assessment in three general populations. J. Clin. Epidemiol. 2000, 53, 393–400. [Google Scholar] [CrossRef]
- Wang, M.; Yi, Y.; Roebothan, B.; Colbourne, J.; Maddalena, V.; Wang, P.P.; Sun, G. Body Mass Index Trajectories among Middle-Aged and Elderly Canadians and Associated Health Outcomes. J. Environ. Public Health 2016, 2016, 7014857. [Google Scholar] [CrossRef] [PubMed]
- Kuwabara, M.; Kuwabara, R.; Niwa, K.; Hisatome, I.; Smits, G.; Roncal-Jimenez, C.A.; MacLean, P.S.; Yracheta, J.M.; Ohno, M.; Lanaspa, M.A.; et al. Different Risk for Hypertension, Diabetes, Dyslipidemia, and Hyperuricemia According to Level of Body Mass Index in Japanese and American Subjects. Nutrients 2018, 10, 1011. [Google Scholar] [CrossRef] [PubMed]
- Abdullah, A.; Peeters, A.; de Courten, M.; Stoelwinder, J. The magnitude of association between overweight and obesity and the risk of diabetes: A meta-analysis of prospective cohort studies. Diabetes Res. Clin. Pract. 2010, 89, 309–319. [Google Scholar] [CrossRef]
- Guh, D.P.; Zhang, W.; Bansback, N.; Amarsi, Z.; Birmingham, C.L.; Anis, A.H. The incidence of co-morbidities related to obesity and overweight: A systematic review and meta-analysis. BMC Public Health 2009, 9, 88. [Google Scholar] [CrossRef]
- Bell, J.A.; Kivimaki, M.; Hamer, M. Metabolically healthy obesity and risk of incident type 2 diabetes: A meta-analysis of prospective cohort studies. Obes. Rev. 2014, 15, 504–515. [Google Scholar] [CrossRef]
- Field, A.E.; Coakley, E.H.; Must, A.; Spadano, J.L.; Laird, N.; Dietz, W.H.; Rimm, E.; Colditz, G.A. Impact of Overweight on the Risk of Developing Common Chronic Diseases During a 10-Year Period. Arch. Intern. Med. 2001, 161, 1581–1586. [Google Scholar] [CrossRef] [PubMed]
- Vekic, J.; Zeljkovic, A.; Stefanovic, A.; Jelic-Ivanovic, Z.; Spasojevic-Kalimanovska, V. Obesity and dyslipidemia. Metabolism 2019, 92, 71–81. [Google Scholar] [CrossRef]
- Audrain-McGovern, J.; Benowitz, N.L. Cigarette Smoking, Nicotine, and Body Weight. Clin. Pharmacol. Ther. 2011, 90, 164–168. [Google Scholar] [CrossRef]
- Sikorski, C.; Luppa, M.; Weyerer, S.; König, H.-H.; Maier, W.; Schön, G.; Petersen, J.J.; Gensichen, J.; Fuchs, A.; Bickel, H.; et al. Obesity and Associated Lifestyle in a Large Sample of Multi-Morbid German Primary Care Attendees. PLoS ONE 2014, 9, e102587. [Google Scholar] [CrossRef]
- Morris, R.W.; Taylor, A.E.; Fluharty, M.E.; Bjørngaard, J.H.; Åsvold, B.O.; Gabrielsen, M.E.; Campbell, A.; Marioni, R.; Kumari, M.; Korhonen, T.; et al. Heavier smoking may lead to a relative increase in waist circumference: Evidence for a causal relationship from a Mendelian randomisation meta-analysis. The CARTA consortium. BMJ Open 2015, 5, e008808. [Google Scholar] [CrossRef] [PubMed]
- Lv, J.; Chen, W.; Sun, D.; Li, S.; Millwood, I.Y.; Smith, M.; Guo, Y.; Bian, Z.; Yu, C.; Zhou, H.; et al. Gender-Specific Association between Tobacco Smoking and Central Obesity among 0.5 Million Chinese People: The China Kadoorie Biobank Study. PLoS ONE 2015, 10, e0124586. [Google Scholar] [CrossRef]
- Tuovinen, E.-L.; Saarni, S.E.; Männistö, S.; Borodulin, K.; Patja, K.; Kinnunen, T.H.; Kaprio, J.; Korhonen, T. Smoking status and abdominal obesity among normal- and overweight/obese adults: Population-based FINRISK study. Prev. Med. Rep. 2016, 4, 324–330. [Google Scholar] [CrossRef]
- Jo, Y.-H.; Talmage, D.A.; Role, L.W. Nicotinic receptor-mediated effects on appetite and food intake. J. Neurobiol. 2002, 53, 618–632. [Google Scholar] [CrossRef] [PubMed]
- Tian, J.; Venn, A.; Otahal, P.; Gall, S. The association between quitting smoking and weight gain: A systemic review and meta-analysis of prospective cohort studies. Obes. Rev. 2015, 16, 883–901. [Google Scholar] [CrossRef] [PubMed]
- Harris, K.K.; Zopey, M.; Friedman, T.C. Metabolic effects of smoking cessation. Nat. Rev. Endocrinol. 2016, 12, 299–308. [Google Scholar] [CrossRef]
- Nuttall, F.Q. Body Mass Index. Nutr. Today 2015, 50, 117–128. [Google Scholar] [CrossRef] [PubMed]
- Okorodudu, D.O.; Jumean, M.F.; Montori, V.M.; Romero-Corral, A.; Somers, V.K.; Erwin, P.J.; Lopez-Jimenez, F. Diagnostic performance of body mass index to identify obesity as defined by body adiposity: A systematic review and meta-analysis. Int. J. Obes. 2010, 34, 791–799. [Google Scholar] [CrossRef] [PubMed]
- Tran, N.T.T.; Blizzard, C.L.; Luong, K.N.; Le Van Truong, N.; Tran, B.Q.; Otáhal, P.; Nelson, M.; Magnussen, C.; Gall, S.; Van Bui, T.; et al. The importance of waist circumference and body mass index in cross-sectional relationships with risk of cardiovascular disease in Vietnam. PLoS ONE 2018, 13, e0198202. [Google Scholar] [CrossRef] [PubMed]
- Darbandi, M.; Pasdar, Y.; Moradi, S.; Mohamed, H.J.J.; Hamzeh, B.; Salimi, Y. Discriminatory Capacity of Anthropometric Indices for Cardiovascular Disease in Adults: A Systematic Review and Meta-Analysis. Prev. Chronic Dis. 2020, 17, 200112. [Google Scholar] [CrossRef]
- O’Súilleabháin, P.S.; Sutin, A.R.; Gerstorf, D. Body mass index, waist circumference, and mortality risks over 27 years of follow-up in old age. Ann. Epidemiol. 2020, 46, 20–23. [Google Scholar] [CrossRef] [PubMed]
| Sample (n = 38,412) | |
|---|---|
| Mean ± SD | |
| WC (cm) | 96.76 ± 12.42 |
| BMI (kg/m2) | 27.90 ± 4.72 |
| sBP (mmHg) | 132.80 ± 15.58 |
| dBP (mmHg) | 83.25 ± 9.62 |
| HR (bpm) | 71.71 ± 9.06 |
| Fasting glycemia (mmol/L) | 5.56 ± 1.26 |
| Total cholesterol (mmol/L) | 5.84 ± 1.20 |
| LDL-C(mmol/L) | 3.73 ± 1.06 |
| HDL-C (mmol/L) | 1.40 ± 0.46 |
| Triglycerides (mmol/L) | 1.74 ± 1.40 |
| SCORE | 1.90 ± 1.74 |
| LW (n = 325) | NW (n = 13,659) | OW (n = 19,001) | G1O (n = 13,005) | G2O (n = 5529) | G3O (n = 2442) | NW vs. OW | NW vs. G3O | OW vs. G3O | NW vs. LW | LW vs. G3O | |
|---|---|---|---|---|---|---|---|---|---|---|---|
| Mean ± SD | Mean ± SD | Mean ± SD | Mean ± SD | Mean ± SD | Mean ± SD | p | p | p | p | p | |
| Age (years) | 47.60 ± 4.68 | 46.82 ± 4,42 | 48.98 ± 4.38 | 47.06 ± 4.39 | 47.11 ± 4.34 | 46.95 ± 4.35 | ** | ** | ** | ** | ** |
| WC (cm) | 76.55 ± 8.69 | 85.81 ± 7.42 | 95.57 ± 7.28 | 106.11 ± 7.45 | 117.09 ± 8.41 | 129.45 ± 12.12 | ** | ** | ** | ** | ** |
| sBP (mmHg) | 122.43 ± 15.20 | 127.68 ± 13.68 | 131.89 ± 14.45 | 137.74 ± 15.95 | 142.87 ± 16.93 | 148.59 ± 18.37 | ** | ** | ** | ** | ** |
| dBP (mmHg) | 77.47 ± 8.99 | 80.28 ± 8.53 | 82.85 ± 9.05 | 86.09 ± 9.96 | 88.65 ± 10.64 | 90.99 ± 11.28 | ** | ** | ** | * | ** |
| HR (bpm) | 76.00 ± 12.44 | 71.29 ± 9.19 | 71.22 ± 8.80 | 72.39 ± 9.03 | 73.36 ± 9.11 | 75.97 ± 10.02 | 0.982 | ** | ** | ** | 0.982 |
| Fasting glycemia (mmol/L) | 5.49 ± 1.26 | 5.36 ± 1.07 | 5.47 ± 1.07 | 5.77 ± 1.41 | 6.20 ± 1.93 | 6.54 ± 2.19 | ** | ** | ** | 0.763 | ** |
| TC (mmol/L) | 5.08 ± 1.35 | 5.63 ± 1.16 | 5.90 ± 1.19 | 6.02 ± 1.22 | 5.89 ± 1.16 | 5.82 ± 1.17 | ** | * | 0.499 | ** | ** |
| LDL-C (mmol/L) | 3.03 ± 1.12 | 3.51 ± 1.05 | 3.81 ± 1.06 | 3.87 ± 1.05 | 3.73 ± 1.01 | 3.71 ± 1.01 | ** | ** | 0.198 | ** | ** |
| HDL-C (mmol/L) | 1.61 ± 0.63 | 1.59 ± 0.52 | 1.39 ± 0.43 | 1.26 ± 0.36 | 1.18 ± 0.32 | 1.15 ± 0.30 | ** | ** | ** | 0.999 | ** |
| TGs (mmol/L) | 1.12 ± 0.56 | 1.27 ± 0.90 | 1.70 ± 1.26 | 2.19 ± 1.77 | 2.47 ± 1.86 | 2.40 ± 1.49 | ** | ** | ** | * | ** |
| SCORE | 1.67 ± 1.5 | 1.73 ± 1.57 | 1.83 ± 1.65 | 2.12 ± 1.91 | 2.26 ± 2.07 | 2.63 ± 2.35 | ** | ** | ** | 0.996 | ** |
| Normal WC (n = 12,498) | Increased WC (n = 11,908) | Obesity (n = 29,555) | 1 vs. 2 vs. 3 | 1 vs. 2 | 1 vs. 3 | 2 vs. 3 | |
|---|---|---|---|---|---|---|---|
| Mean ± SD | Mean ± SD | Mean ± SD | p | p | p | p | |
| Age (yrs.) | 46.66 ± 4.41 | 47.00 ± 4.38 | 47.26 ± 4.36 | ** | ** | ** | ** |
| BMI (kg/m2) | 24.06 ± 2.60 | 27.54 ± 2.63 | 32.96 ± 4.24 | ** | ** | ** | ** |
| sBP (mmHg) | 127.72 ± 13.59 | 132.24 ± 14.56 | 139.65 ± 16.58 | ** | ** | ** | ** |
| dBP (mmHg) | 80.29 ± 8.44 | 83.02 ± 9.07 | 87.09 ± 10.34 | ** | ** | ** | ** |
| HR (bpm) | 71.03 ± 8.96 | 71.41 ± 8.94 | 72.93 ± 9.23 | ** | ** | ** | ** |
| Fasting glycemia (mmol/L) | 5.35 ± 1.03 | 5.50 ± 1.08 | 5.90 ± 1.63 | ** | ** | ** | ** |
| TC (mmol/L) | 5.65 ± 1.16 | 5.91 ± 1.19 | 5.98 ± 1.22 | ** | ** | ** | ** |
| LDL-C (mmol/L) | 3.55 ± 1.05 | 3.81 ± 1.06 | 3.83 ± 1.04 | ** | ** | ** | 0.281 |
| HDL-C (mmol/L) | 1.55 ± 0.51 | 1.39 ± 0.44 | 1.24 ± 0.35 | ** | ** | ** | ** |
| TGs (mmol/L) | 1.32 ± 0.97 | 1.73 ± 1.32 | 2.24 ± 1.73 | ** | ** | ** | ** |
| SCORE | 1.65 ± 1.50 | 1.85 ± 1.64 | 2.23 ± 2.04 | ** | ** | ** | ** |
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2022 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Rinkūnienė, E.; Petrulionytė, E.; Dženkevičiūtė, V.; Petrulionienė, Ž.; Senulytė, A.; Puronaitė, R.; Laucevičius, A. Prevalence of Cardiovascular Risk Factors in Middle-Aged Lithuanian Men Based on Body Mass Index and Waist Circumference Group Results from the 2006–2016 Lithuanian High Cardiovascular Risk Prevention Program. Medicina 2022, 58, 1718. https://doi.org/10.3390/medicina58121718
Rinkūnienė E, Petrulionytė E, Dženkevičiūtė V, Petrulionienė Ž, Senulytė A, Puronaitė R, Laucevičius A. Prevalence of Cardiovascular Risk Factors in Middle-Aged Lithuanian Men Based on Body Mass Index and Waist Circumference Group Results from the 2006–2016 Lithuanian High Cardiovascular Risk Prevention Program. Medicina. 2022; 58(12):1718. https://doi.org/10.3390/medicina58121718
Chicago/Turabian StyleRinkūnienė, Egidija, Emilija Petrulionytė, Vilma Dženkevičiūtė, Žaneta Petrulionienė, Augustė Senulytė, Roma Puronaitė, and Aleksandras Laucevičius. 2022. "Prevalence of Cardiovascular Risk Factors in Middle-Aged Lithuanian Men Based on Body Mass Index and Waist Circumference Group Results from the 2006–2016 Lithuanian High Cardiovascular Risk Prevention Program" Medicina 58, no. 12: 1718. https://doi.org/10.3390/medicina58121718
APA StyleRinkūnienė, E., Petrulionytė, E., Dženkevičiūtė, V., Petrulionienė, Ž., Senulytė, A., Puronaitė, R., & Laucevičius, A. (2022). Prevalence of Cardiovascular Risk Factors in Middle-Aged Lithuanian Men Based on Body Mass Index and Waist Circumference Group Results from the 2006–2016 Lithuanian High Cardiovascular Risk Prevention Program. Medicina, 58(12), 1718. https://doi.org/10.3390/medicina58121718






