Central Sensitization Is Associated with Inferior Patient-Reported Outcomes and Increased Osteotomy Site Pain in Patients Undergoing Medial Opening-Wedge High Tibial Osteotomy
Abstract
1. Introduction
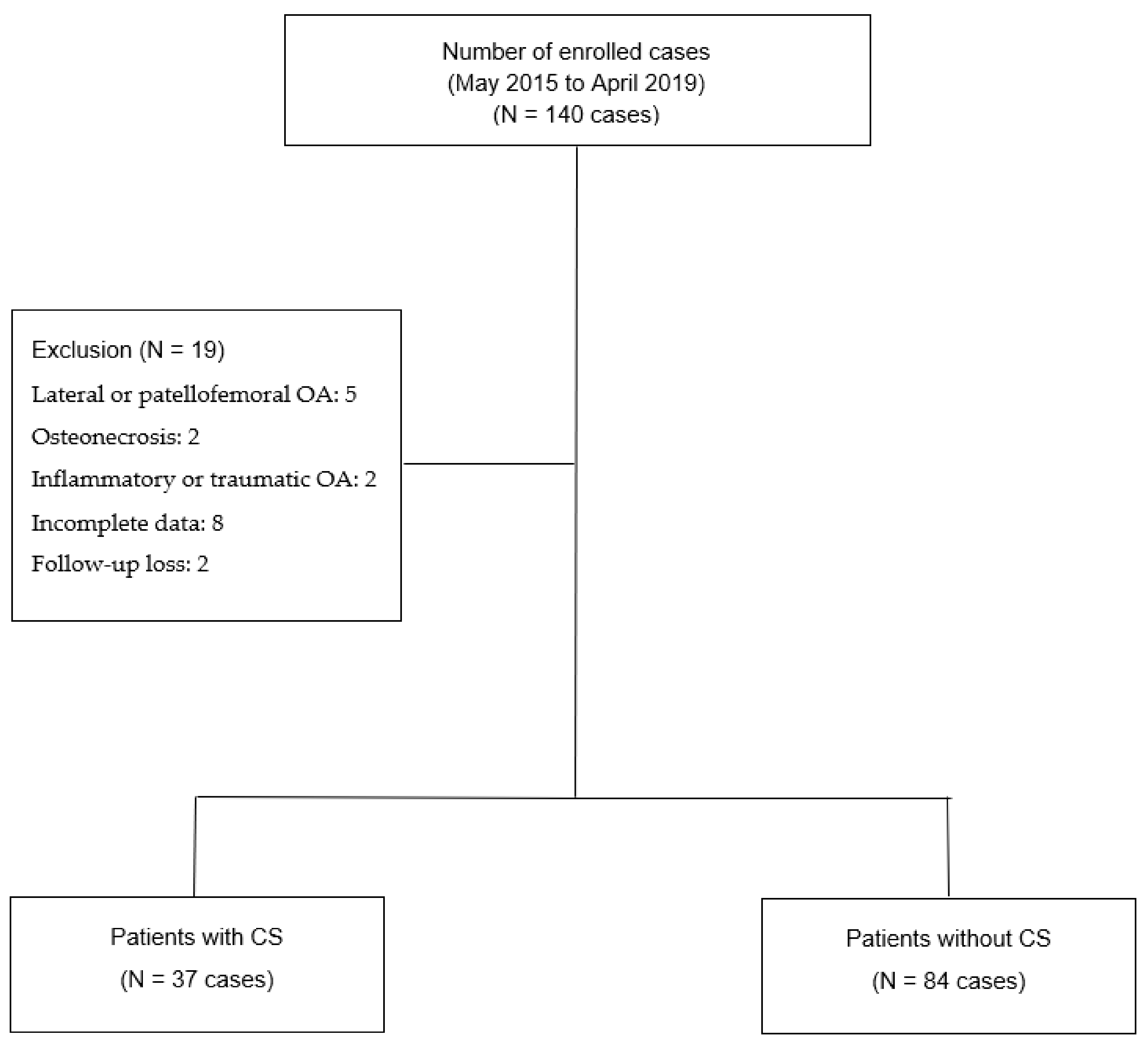
2. Materials and Methods
- Surgical procedure
- Postoperative rehabilitation
- Clinical assessment and Radiographic evaluation
- Statistical Analysis
3. Results
4. Discussion
5. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Conflicts of Interest
References
- Ogawa, H.; Matsumoto, K.; Ogawa, T.; Takeuchi, K.; Akiyama, H. Preoperative varus laxity correlates with overcorrection in medial opening wedge high tibial osteotomy. Arch. Orthop. Trauma. Surg. 2016, 136, 1337–1342. [Google Scholar] [CrossRef] [PubMed]
- Song, S.J.; Bae, D.K. Computer-Assisted Navigation in High Tibial Osteotomy. Clin. Orthop. Surg. 2016, 8, 349–357. [Google Scholar] [CrossRef] [PubMed]
- Sabzevari, S.; Ebrahimpour, A.; Roudi, M.K.; Kachooei, A.R. High Tibial Osteotomy: A Systematic Review and Current Concept. Arch. Bone Jt. Surg. 2016, 4, 204–212. [Google Scholar] [PubMed]
- Goshima, K.; Sawaguchi, T.; Shigemoto, K.; Iwai, S.; Fujita, K.; Yamamuro, Y. Open-wedge high tibial osteotomy for spontaneous osteonecrosis of the medial tibial plateau shows excellent clinical outcomes. J. Exp. Orthop. 2020, 7, 14. [Google Scholar] [CrossRef] [PubMed]
- Lee, S.C.; Jung, K.A.; Nam, C.H.; Jung, S.H.; Hwang, S.H. The Short-term Follow-up Results of Open Wedge High Tibial Osteotomy with Using an Aescula Open Wedge Plate and an Allogenic Bone Graft: The Minimum 1-Year Follow-up Results. Clin. Orthop. Surg. 2010, 2, 47–54. [Google Scholar] [CrossRef]
- Sterett, W.I.; Steadman, J.R.; Huang, M.J.; Matheny, L.M.; Briggs, K.K. Chondral Resurfacing and High Tibial Osteotomy in the Varus Knee: Survivorship Analysis. Am. J. Sport. Med. 2010, 38, 1420–1424. [Google Scholar] [CrossRef]
- Scott, C.E.; Howie, C.R.; MacDonald, D.; Biant, L.C. Predicting dissatisfaction following total knee replacement: A prospective study of 1217 patients. J. Bone Jt. Surg. 2010, 92, 1253–1258. [Google Scholar] [CrossRef]
- Petersen, K.K.; Graven-Nielsen, T.; Simonsen, O.; Laursen, M.B.; Arendt-Nielsen, L. Preoperative pain mechanisms assessed by cuff algometry are associated with chronic postoperative pain relief after total knee replacement. Pain 2016, 157, 1400–1406. [Google Scholar] [CrossRef]
- Kim, M.S.; Koh, I.J.; Lee, S.Y.; In, Y. Central sensitization is a risk factor for wound complications after primary total knee arthroplasty. Knee Surg. Sport. Traumatol. Arthrosc. 2018, 26, 3419–3428. [Google Scholar] [CrossRef]
- Kim, S.H.; Yoon, K.B.; Yoon, D.M.; Yoo, J.H.; Ahn, K.R. Influence of Centrally Mediated Symptoms on Postoperative Pain in Osteoarthritis Patients Undergoing Total Knee Arthroplasty: A Prospective Observational Evaluation. Pain Pract. 2015, 15, E46–E53. [Google Scholar] [CrossRef]
- Koh, I.J.; Kim, M.S.; Sohn, S.; Song, K.Y.; Choi, N.Y.; In, Y. Duloxetine reduces pain and improves quality of recovery following total knee arthroplasty in centrally sensitized patients: A prospective, randomized controlled study. J. Bone Jt. Surg. Am. 2019, 101, 64–73. [Google Scholar] [CrossRef]
- Kurien, T.; Arendt-Nielsen, L.; Petersen, K.K.; Graven-Nielsen, T.; Scammell, B.E. Preoperative Neuropathic Pain-like Symptoms and Central Pain Mechanisms in Knee Osteoarthritis Predicts Poor Outcome 6 Months After Total Knee Replacement Surgery. J. Pain 2018, 19, 1329–1341. [Google Scholar] [CrossRef]
- Gagnier, J.J. Patient reported outcomes in orthopaedics. J. Orthop. Res. 2017, 35, 2098–2108. [Google Scholar] [CrossRef]
- McConnell, S.; Kolopack, P.; Davis, A. The Western Ontario and McMaster Universities Osteoarthritis Index (WOMAC): A review of its utility and measurement properties. Arthritis Rheum. 2001, 45, 453–461. [Google Scholar] [CrossRef]
- Webb, M.; Dewan, V.; Elson, D. Functional results following high tibial osteotomy: A review of the literature. Eur. J. Orthop. Surg. Traumatol. 2018, 28, 555–563. [Google Scholar] [CrossRef]
- Wei, W.; Shen, J. Effectiveness of double-plane high tibial osteotomy in treatment of medial compartment osteoarthritis. Chin. J. Reparative Reconstr. Surg. 2018, 32, 1406–1410. [Google Scholar]
- Ccedilelik, D.; Çoban, Ö.; Kılıçoğlu, Ö. Minimal clinically important difference of commonly used hip-, knee-, foot-, and ankle-specific questionnaires: A systematic review. J. Clin. Epidemiol. 2019, 113, 44–57. [Google Scholar] [CrossRef]
- Maredupaka, S.; Meshram, P.; Chatte, M.; Kim, W.H.; Kim, T.K. Minimal clinically important difference of commonly used patient-reported outcome measures in total knee arthroplasty: Review of terminologies, methods and proposed values. Knee Surg. Relat. Res. 2020, 32, 19. [Google Scholar] [CrossRef]
- Copay, A.G.; Subach, B.R.; Glassman, S.D.; Polly, D.W., Jr.; Schuler, T.C. Understanding the minimum clinically important difference: A review of concepts and methods. Spine J. 2007, 7, 541–546. [Google Scholar] [CrossRef]
- Lee, D.C.; Byun, S.J. High tibial osteotomy. Knee Surg. Relat. Res. 2012, 24, 61–69. [Google Scholar] [CrossRef]
- Fujisawa, Y.; Masuhara, K.; Shiomi, S. The Effect of High Tibial Osteotomy on Osteoarthritis of the Knee: An arthroscopic study of 54 knee joints. Orthop. Clin. North Am. 1979, 10, 585–608. [Google Scholar] [CrossRef] [PubMed]
- Kim, M.S.; Son, J.M.; Koh, I.J.; Bahk, J.H.; In, Y. Intraoperative adjustment of alignment under valgus stress reduces outliers in patients undergoing medial opening-wedge high tibial osteotomy. Arch. Orthop. Trauma Surg. 2017, 137, 1035–1045. [Google Scholar] [CrossRef] [PubMed]
- Mayer, T.G.; Neblett, R.; Cohen, H.; Howard, K.J.; Choi, Y.H.; Williams, M.J.; Perez, Y.; Gatchel, R.J. The Development and Psychometric Validation of the Central Sensitization Inventory. Pain Pract. 2012, 12, 276–285. [Google Scholar] [CrossRef] [PubMed]
- Neblett, R.; Cohen, H.; Choi, Y.; Hartzell, M.M.; Williams, M.; Mayer, T.G.; Gatchel, R.J. The Central Sensitization Inventory (CSI): Establishing Clinically Significant Values for Identifying Central Sensitivity Syndromes in an Outpatient Chronic Pain Sample. J. Pain 2013, 14, 438–445. [Google Scholar] [CrossRef] [PubMed]
- Bellamy, N.; Buchanan, W.W.; Goldsmith, C.H.; Campbell, J.; Stitt, L.W. Validation study of WOMAC: A health status instrument for measuring clinically important patient relevant outcomes to antirheumatic drug therapy in patients with osteoarthritis of the hip or knee. J. Rheumatol. 1988, 15, 1833–1840. [Google Scholar]
- Kim, M.S.; Koh, I.J.; Choi, K.Y.; Sung, Y.G.; Park, D.C.; Lee, H.J.; In, Y. The Minimal Clinically Important Difference (MCID) for the WOMAC and Factors Related to Achievement of the MCID after Medial Opening Wedge High Tibial Osteotomy for Knee Osteoarthritis. Am. J. Sports Med. 2021, 49, 2406–2415. [Google Scholar] [CrossRef]
- Kohn, M.D.; Sassoon, A.A.; Fernando, N.D. Classifications in Brief: Kellgren-Lawrence Classification of Osteoarthritis. Clin. Orthop. Relat. Res. 2016, 474, 1886–1893. [Google Scholar] [CrossRef]
- Song, S.J.; Kim, K.I.; Bae, D.K.; Park, C.H. Mid-term lifetime survivals of octogenarians following primary and revision total knee arthroplasties were satisfactory: A retrospective single center study in contemporary period. Knee Surg. Relat. Res. 2020, 32, 50. [Google Scholar] [CrossRef]
- Takamura, D.; Iwata, K.; Sueyoshi, T.; Yasuda, T.; Moriyama, H. Relationship between early physical activity after total knee arthroplasty and postoperative physical function: Are these related? Knee Surg. Relat. Res. 2021, 33, 35. [Google Scholar] [CrossRef]
- Lape, E.C.; Selzer, F.; Collins, J.E.; Losina, E.; Katz, J.N. Stability of Measures of Pain Catastrophizing and Widespread Pain Following Total Knee Replacement. Arthritis Care Res. 2020, 72, 1096–1103. [Google Scholar] [CrossRef]
- Dave, A.; Selzer, F.; Losina, E.; Usiskin, I.; Collins, J.; Lee, Y.; Band, P.; Dalury, D.; Iorio, R.; Kindsfater, K.; et al. The association of pre-operative body pain diagram scores with pain outcomes following total knee arthroplasty. Osteoarthr. Cartil. 2016, 25, 667–675. [Google Scholar] [CrossRef]
- Wylde, V.; Palmer, S.; Learmonth, I.; Dieppe, P. The association between pre-operative pain sensitisation and chronic pain after knee replacement: An exploratory study. Osteoarthr. Cartil. 2013, 21, 1253–1256. [Google Scholar] [CrossRef]
- Wylde, V.; Sayers, A.; Lenguerrand, E.; Gooberman-Hill, R.; Pyke, M.; Beswick, A.D.; Dieppe, P.; Blom, A.W. Preoperative widespread pain sensitization and chronic pain after hip and knee replacement: A cohort analysis. Pain 2015, 156, 47–54. [Google Scholar] [CrossRef]
- Angst, F.; Aeschlimann, A.; Angst, J. The minimal clinically important difference raised the significance of outcome effects above the statistical level, with methodological implications for future studies. J. Clin. Epidemiol. 2017, 82, 128–136. [Google Scholar] [CrossRef]
- Clement, N.D.; MacDonald, D.; Simpson, A.H.R.W. The minimal clinically important difference in the Oxford knee score and Short Form 12 score after total knee arthroplasty. Knee Surg. Sport. Traumatol. Arthrosc. 2013, 22, 1933–1939. [Google Scholar] [CrossRef]
- Arendt-Nielsen, L.; Sluka, K.A.; Nie, H.L. Experimental muscle pain impairs descending inhibition. Pain 2008, 140, 465–471. [Google Scholar] [CrossRef]
- Law, L.A.F.; Sluka, K.; McMullen, T.; Lee, J.; Arendt-Nielsen, L.; Graven-Nielsen, T. Acidic buffer induced muscle pain evokes referred pain and mechanical hyperalgesia in humans. Pain 2008, 140, 254–264. [Google Scholar] [CrossRef]
- Fillingim, R.B.; Maixner, W.; Kincaid, S.; Silva, S. Sex differences in temporal summation but not sensory-discriminative processing of thermal pain. Pain 1998, 75, 121–127. [Google Scholar] [CrossRef]
- Kim, M.S.; Koh, I.J.; Choi, K.Y.; Yang, S.C.; In, Y. Efficacy of duloxetine compared with opioid for postoperative pain control following total knee arthroplasty. PLoS ONE 2021, 16, e0253641. [Google Scholar] [CrossRef]
- Kim, M.; Koh, I.; Sung, Y.; Park, D.; Na, J.; In, Y. Preemptive Duloxetine Relieves Postoperative Pain and Lowers Wound Temperature in Centrally Sensitized Patients Undergoing Total Knee Arthroplasty: A Randomized, Double-Blind, Placebo-Controlled Trial. J. Clin. Med. 2021, 10, 2809. [Google Scholar] [CrossRef]
- Otsuki, S.; Okamoto, Y.; Ikeda, K.; Wakama, H.; Okayoshi, T.; Neo, M. Perioperative duloxetine administration reduces pain after high tibial osteotomy and non-steroidal anti-inflammatory administration: A prospective, controlled study. Knee 2022, 38, 42–49. [Google Scholar] [CrossRef] [PubMed]
- Song, S.J.; Kang, S.G.; Park, C.H.; Bae, D.K. Comparison of Clinical Results and Risk of Patellar Injury between Attune and PFC Sigma Knee Systems. Knee Surg. Relat. Res. 2018, 30, 334–340. [Google Scholar] [CrossRef] [PubMed]
- Yoo, J.-H.; Kim, J.-G.; Chung, K.; Lee, S.H.; Oh, H.-C.; Park, S.-H.; Seok, S.-O. Vascular Calcification in Patients Undergoing Total Knee Arthroplasty: Frequency and Effects on the Surgery. Clin. Orthop. Surg. 2020, 12, 171–177. [Google Scholar] [CrossRef] [PubMed]
- Koh, I.J.; Kim, T.K.; Chang, C.B.; Cho, H.J.; In, Y. Trends in Use of Total Knee Arthroplasty in Korea from 2001 to 2010. Clin. Orthop. Relat. Res. 2013, 471, 1441–1450. [Google Scholar] [CrossRef] [PubMed]
- Koh, I.J.; Cho, W.-S.; Choi, N.Y.; Kim, T.K. Causes, Risk Factors, and Trends in Failures After TKA in Korea Over the Past 5 Years: A Multicenter Study. Clin. Orthop. Relat. Res. 2014, 472, 316–326. [Google Scholar] [CrossRef]
- Kim, M.S.; Koh, I.J.; Choi, K.Y.; Seo, J.Y.; In, Y. Minimal Clinically Important Differences for Patient-Reported Outcomes After TKA Depend on Central Sensitization. J. Bone Jt. Surg. 2021, 103, 1374–1382. [Google Scholar] [CrossRef]
- Kim, M.S.; Koh, I.J.; Choi, K.Y.; Ju, G.I.; In, Y. Centrally sensitized patients undergoing total knee arthroplasty have higher expectations than do non-centrally sensitized patients. Knee Surg. Sport. Traumatol. Arthrosc. 2021, 30, 1257–1265. [Google Scholar] [CrossRef]
- Hochman, J.; Gagliese, L.; Davis, A.; Hawker, G. Neuropathic pain symptoms in a community knee OA cohort. Osteoarthr. Cartil. 2011, 19, 647–654. [Google Scholar] [CrossRef]
- Ohtori, S.; Orita, S.; Yamashita, M.; Ishikawa, T.; Ito, T.; Shigemura, T.; Nishiyama, H.; Konno, S.; Ohta, H.; Takaso, M.; et al. Existence of a Neuropathic Pain Component in Patients with Osteoarthritis of the Knee. Yonsei Med. J. 2012, 53, 801–805. [Google Scholar] [CrossRef]
| Variables | CS Group (n = 37) | Non-CS Group (n = 84) | p Value |
|---|---|---|---|
| Age (years) | 57.6 ± 5.8 | 55.9 ± 6.1 | 0.170 |
| Sex | 0.064 | ||
| Male | 1 (2.7%) | 12 (14.3%) | |
| Female | 36(97.3%) | 72 (85.7%) | |
| Operation side | 0.891 | ||
| Right | 18 (48.6%) | 42 (50.0%) | |
| Left | 19 (51.4%) | 42 (50.0%) | |
| Body mass index (kg/m2) | 26.1 ± 4.1 | 26.2 ± 3.1 | 0.817 |
| CSI score | 45.3 ± 6.7 | 21.2 ± 8.6 | 0.000 |
| K-L grade | 0.415 | ||
| 2 | 11 (29.7%) | 17 (20.2%) | |
| 3 | 25 (67.5%) | 61 (72.6%) | |
| 4 | 1 (2.7%) | 6 (7.1%) | |
| Preoperative HKA angle, deg | 6.9 ± 2.9 | 7.2 ± 2.8 | 0.529 |
| Preoperative WBL ratio, % | 19.3 ± 11.9 | 16.8 ± 11.3 | 0.267 |
| Postoperative two-year HKA angle, deg | −1.4 ± 2.0 | −0.9 ± 2.5 | 0.277 |
| Postoperative two-year WBL ratio, % | 55.1 ± 10.9 | 53.5 ± 9.8 | 0.447 |
| Surgical correction angle | 10.5 ± 2.7 | 11.2 ± 2.7 | 0.243 |
| ASA score | 0.275 | ||
| 1 | 15 (40.5%) | 23 (27.3%) | |
| 2 | 22 (59.4%) | 59 (70.2%) | |
| 3 | 0 (0.0%) | 2 (2.3%) | |
| Diabetes | 5 (13.5%) | 7 (8.3%) | 0.510 |
| Hypertension | 12 (32.4%) | 24 (28.6%) | 0.669 |
| Alcohol consumption | 6 (16.2%) | 16 (19.0%) | 0.710 |
| Smoking | 5 (13.5%) | 8 (9.5%) | 0.534 |
| Variables | CS Group (n = 37) | Non-CS Group (n = 84) | p Value |
|---|---|---|---|
| Preoperative WOMAC | |||
| Pain | 11.8 ± 3.0 | 9.3 ± 3.3 | 0.000 |
| Stiffness | 5.0 ± 1.7 | 4.4 ± 2.2 | 0.198 |
| Function | 41.8 ± 9.3 | 35.6 ± 11.7 | 0.003 |
| Total | 58.7 ± 12.5 | 49.4 ± 16.1 | 0.001 |
| Postoperative two-year WOMAC | |||
| Pain | 7.8 ± 2.2 | 3.9 ± 3.5 | 0.000 |
| Stiffness | 2.7 ± 1.1 | 2.2 ± 1.6 | 0.067 |
| Function | 26.5 ± 4.8 | 15.6 ± 11.3 | 0.000 |
| Total | 37.1 ± 6.2 | 21.8 ± 14.6 | 0.000 |
| Change WOMAC | |||
| Pain | 3.9 ± 2.1 | 5.3 ± 3.0 | 0.016 |
| Stiffness | 2.3 ± 1.6 | 2.2 ± 2.1 | 0.897 |
| Function | 15.3 ± 8.7 | 19.9 ± 14.3 | 0.031 |
| Total | 21.5 ± 9.7 | 27.5 ± 17.6 | 0.019 |
| Postoperative two-year osteotomy site pain VAS | 4.8 ± 1.8 | 2.2 ± 2.1 | 0.000 |
| Variables | CS Group (n = 37) | Non-CS Group (n = 84) | p Value |
|---|---|---|---|
| MCID achievement | |||
| Pain | 23 (62.2%) | 67 (79.8%) | 0.041 |
| Stiffness | 19 (51.4%) | 44 (52.4%) | 0.917 |
| Function | 21 (56.8%) | 64 (76.2%) | 0.031 |
| Total | 21 (56.8%) | 64 (76.2%) | 0.031 |
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2022 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Kim, J.-J.; Koh, I.-J.; Kim, M.-S.; Choi, K.-Y.; Kang, K.-H.; In, Y. Central Sensitization Is Associated with Inferior Patient-Reported Outcomes and Increased Osteotomy Site Pain in Patients Undergoing Medial Opening-Wedge High Tibial Osteotomy. Medicina 2022, 58, 1752. https://doi.org/10.3390/medicina58121752
Kim J-J, Koh I-J, Kim M-S, Choi K-Y, Kang K-H, In Y. Central Sensitization Is Associated with Inferior Patient-Reported Outcomes and Increased Osteotomy Site Pain in Patients Undergoing Medial Opening-Wedge High Tibial Osteotomy. Medicina. 2022; 58(12):1752. https://doi.org/10.3390/medicina58121752
Chicago/Turabian StyleKim, Jae-Jung, In-Jun Koh, Man-Soo Kim, Keun-Young Choi, Ki-Ho Kang, and Yong In. 2022. "Central Sensitization Is Associated with Inferior Patient-Reported Outcomes and Increased Osteotomy Site Pain in Patients Undergoing Medial Opening-Wedge High Tibial Osteotomy" Medicina 58, no. 12: 1752. https://doi.org/10.3390/medicina58121752
APA StyleKim, J.-J., Koh, I.-J., Kim, M.-S., Choi, K.-Y., Kang, K.-H., & In, Y. (2022). Central Sensitization Is Associated with Inferior Patient-Reported Outcomes and Increased Osteotomy Site Pain in Patients Undergoing Medial Opening-Wedge High Tibial Osteotomy. Medicina, 58(12), 1752. https://doi.org/10.3390/medicina58121752









