Cartilage Regeneration Using Human Umbilical Cord Blood Derived Mesenchymal Stem Cells: A Systematic Review and Meta-Analysis
Abstract
1. Introduction
2. Materials and Methods
2.1. Search Strategy
2.2. Study Selection with Eligibility Criteria
2.3. Data Extraction and Quality Assessment
2.4. Data and Statistical Analyses
3. Results
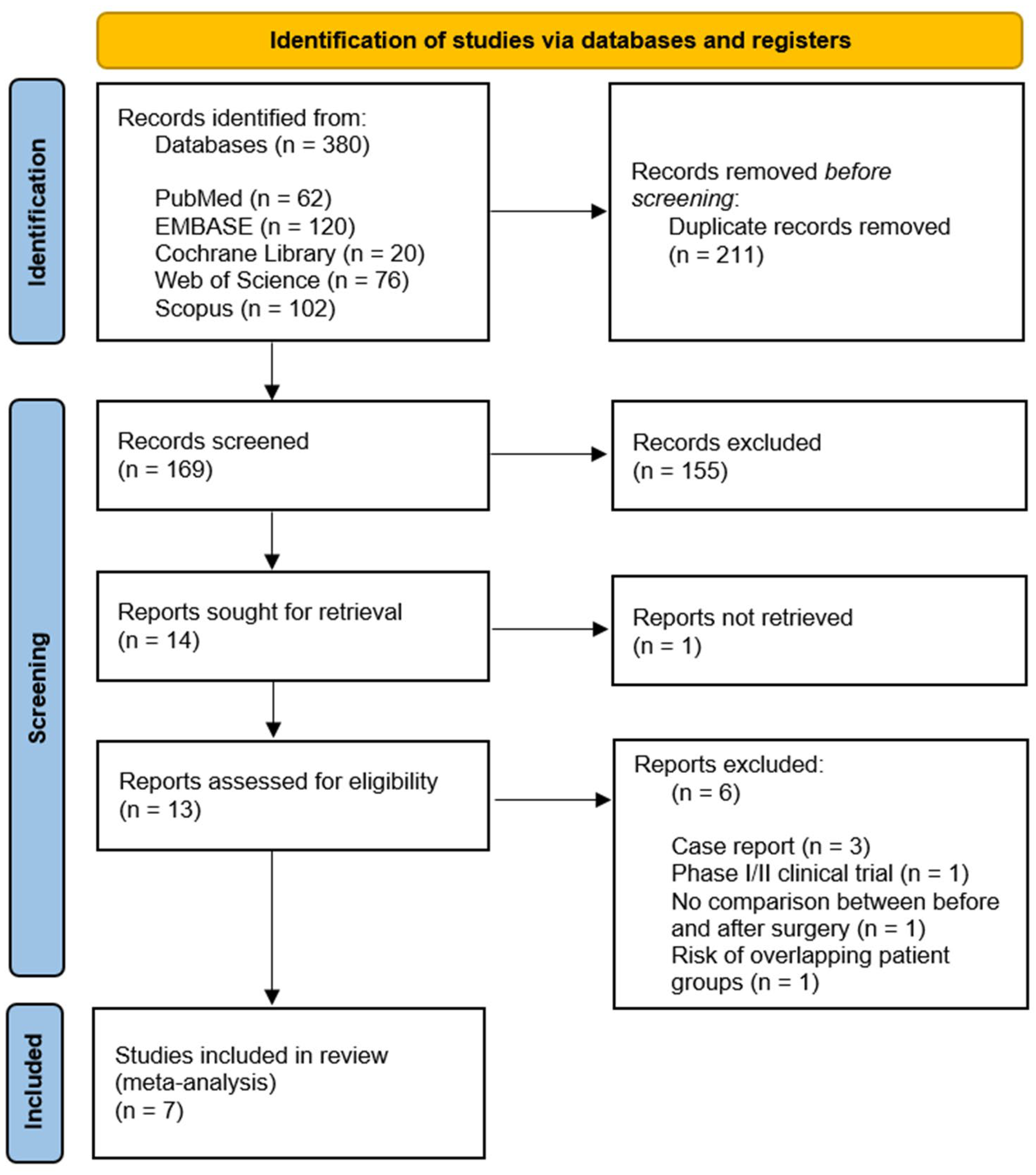
3.1. Identification of Studies
3.2. Characteristics of Included Studies
3.3. Subgroup Analysis of Included Studies
3.4. Study Outcome
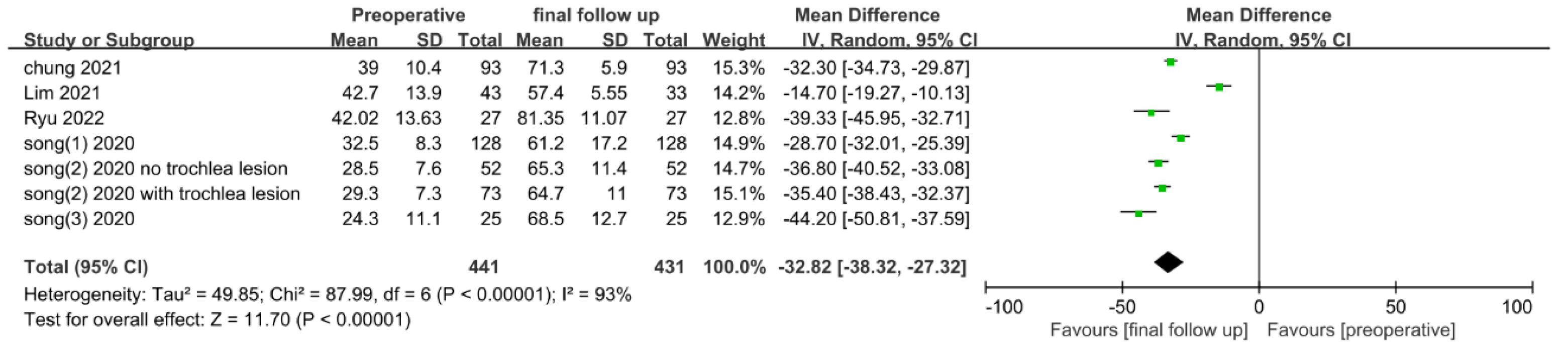
3.4.1. IKDC Score
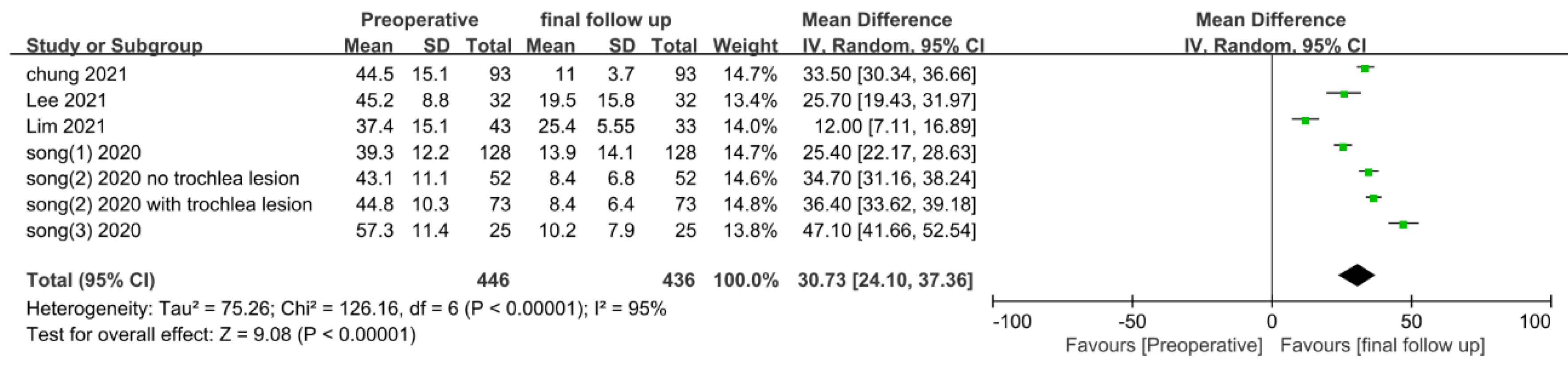
3.4.2. WOMAC Score
3.4.3. VAS Score
3.4.4. M-MOCART Score
3.4.5. Comparison with BMAC and Microfracture Procedures
4. Discussion
5. Conclusions
Supplementary Materials
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Acknowledgments
Conflicts of Interest
References
- Angadi, D.S.; Macdonald, H.; Atwal, N. Autologous cell-free serum preparations in the management of knee osteoarthritis: What is the current clinical evidence? Knee Surg. Relat. Res. 2020, 32, 16. [Google Scholar] [CrossRef]
- Hodler, J.; Resnick, D. Current status of imaging of articular cartilage. Skelet. Radiol. 1996, 25, 703–709. [Google Scholar] [CrossRef]
- Williams, R.J., III; Harnly, H.W. Microfracture: Indications, technique, and results. Instr. Course Lect. 2007, 56, 419–428. [Google Scholar]
- Orth, P.; Gao, L.; Madry, H. Microfracture for cartilage repair in the knee: A systematic review of the contemporary literature. Knee Surg. Sport. Traumatol. Arthrosc. 2020, 28, 670–706. [Google Scholar] [CrossRef]
- Lee, D.H.; Kim, S.J.; Kim, S.A.; Ju, G.I. Past, present, and future of cartilage restoration: From localized defect to arthritis. Knee Surg. Relat. Res. 2022, 34, 1. [Google Scholar] [CrossRef]
- Zamborsky, R.; Danisovic, L. Surgical techniques for knee cartilage repair: An updated large-scale systematic review and network meta-analysis of randomized controlled trials. Arthrosc. J. Arthrosc. Relat. Surg. 2020, 36, 845–858. [Google Scholar] [CrossRef] [PubMed]
- Letsiou, S.; Felix, R.C.; Cardoso, J.C.R.; Anjos, L.; Mestre, A.L.; Gomes, H.L.; Power, D.M. Cartilage acidic protein 1 promotes increased cell viability, cell proliferation and energy metabolism in primary human dermal fibroblasts. Biochimie 2020, 171–172, 72–78. [Google Scholar] [CrossRef] [PubMed]
- Na, H.S.; Lee, S.-Y.; Lee, D.H.; Woo, J.S.; Choi, S.-Y.; Cho, K.-H.; Kim, S.; Go, E.J.; Lee, A.R.; Choi, J.-W. Soluble CCR2 gene therapy controls joint inflammation, cartilage damage, and the progression of osteoarthritis by targeting MCP-1 in a monosodium iodoacetate (MIA)-induced OA rat model. J. Transl. Med. 2022, 20, 482. [Google Scholar] [CrossRef] [PubMed]
- Park, Y.-B.; Ha, C.-W.; Rhim, J.H.; Lee, H.-J. Stem cell therapy for articular cartilage repair: Review of the entity of cell populations used and the result of the clinical application of each entity. Am. J. Sport. Med. 2018, 46, 2540–2552. [Google Scholar] [CrossRef]
- Jeyaraman, M.; Muthu, S.; Ganie, P.A. Does the source of mesenchymal stem cell have an effect in the management of osteoarthritis of the knee? Meta-analysis of randomized controlled trials. Cartilage 2021, 13, 1532S–1547S. [Google Scholar] [CrossRef]
- Moon, S.W.; Park, S.; Oh, M.; Wang, J.H. Outcomes of human umbilical cord blood-derived mesenchymal stem cells in enhancing tendon-graft healing in anterior cruciate ligament reconstruction: An exploratory study. Knee Surg. Relat. Res. 2021, 33, 32. [Google Scholar] [CrossRef] [PubMed]
- Harris, D.T. Cord blood stem cells: A review of potential neurological applications. Stem Cell Rev. 2008, 4, 269–274. [Google Scholar] [CrossRef] [PubMed]
- Harris, D.T. Non-haematological uses of cord blood stem cells. Br. J. Haematol. 2009, 147, 177–184. [Google Scholar] [CrossRef] [PubMed]
- Klontzas, M.E.; Kenanidis, E.I.; Heliotis, M.; Tsiridis, E.; Mantalaris, A. Bone and cartilage regeneration with the use of umbilical cord mesenchymal stem cells. Expert. Opin. Biol. Ther. 2015, 15, 1541–1552. [Google Scholar] [CrossRef]
- Page, M.J.; McKenzie, J.E.; Bossuyt, P.M.; Boutron, I.; Hoffmann, T.C.; Mulrow, C.D.; Shamseer, L.; Tetzlaff, J.M.; Akl, E.A.; Brennan, S.E. The PRISMA 2020 statement: An updated guideline for reporting systematic reviews. Syst. Rev. 2021, 10, 89. [Google Scholar] [CrossRef]
- Wells, G.; Shea, B.; O’connell, D.; Peterson, J.; Welch, V.; Losos, M.; Tugwell, P. The Newcastle-Ottawa Scale (NOS) for Assessing the Quality of Nonrandomised Studies in Meta-Analyses. Available online: http://www3.med.unipmn.it/dispense_ebm/2009-2010/Corso%20Perfezionamento%20EBM_Faggiano/NOS_oxford.pdf (accessed on 13 May 2020).
- Lim, H.C.; Park, Y.B.; Ha, C.W.; Cole, B.J.; Lee, B.K.; Jeong, H.J.; Kim, M.K.; Bin, S.I.; Choi, C.H.; Choi, C.H.; et al. Allogeneic Umbilical Cord Blood-Derived Mesenchymal Stem Cell Implantation Versus Microfracture for Large, Full-Thickness Cartilage Defects in Older Patients: A Multicenter Randomized Clinical Trial and Extended 5-Year Clinical Follow-up. Orthop. J. Sport. Med. 2021, 9, 2325967120973052. [Google Scholar] [CrossRef]
- Song, J.S.; Hong, K.T.; Kong, C.G.; Kim, N.M.; Jung, J.Y.; Park, H.S.; Kim, Y.J.; Chang, K.B.; Kim, S.J. High tibial osteotomy with human umbilical cord blood-derived mesenchymal stem cells implantation for knee cartilage regeneration. World J. Stem Cells 2020, 12, 514–526. [Google Scholar] [CrossRef]
- Song, J.S.; Hong, K.T.; Kim, N.M.; Jung, J.Y.; Park, H.S.; Lee, S.H.; Cho, Y.J.; Kim, S.J. Implantation of allogenic umbilical cord blood-derived mesenchymal stem cells improves knee osteoarthritis outcomes: Two-year follow-up. Regen. Ther. 2020, 14, 32–39. [Google Scholar] [CrossRef] [PubMed]
- Ryu, D.J.; Jeon, Y.S.; Park, J.S.; Bae, G.C.; Kim, J.S.; Kim, M.K. Comparison of Bone Marrow Aspirate Concentrate and Allogenic Human Umbilical Cord Blood Derived Mesenchymal Stem Cell Implantation on Chondral Defect of Knee: Assessment of Clinical and Magnetic Resonance Imaging Outcomes at 2-Year Follow-Up. Cell Transpl. 2020, 29, 963689720943581. [Google Scholar] [CrossRef] [PubMed]
- Song, J.S.; Hong, K.T.; Kim, N.M.; Park, H.S.; Choi, N.H. Human umbilical cord blood-derived mesenchymal stem cell implantation for osteoarthritis of the knee. Arch. Orthop. Trauma Surg. 2020, 140, 503–509. [Google Scholar] [CrossRef]
- Lee, N.H.; Na, S.M.; Ahn, H.W.; Kang, J.K.; Seon, J.K.; Song, E.K. Allogenic Human Umbilical Cord Blood-Derived Mesenchymal Stem Cells Are More Effective Than Bone Marrow Aspiration Concentrate for Cartilage Regeneration After High Tibial Osteotomy in Medial Unicompartmental Osteoarthritis of Knee. Arthroscopy 2021, 37, 2521–2530. [Google Scholar] [CrossRef]
- Chung, Y.W.; Yang, H.Y.; Kang, S.J.; Song, E.K.; Seon, J.K. Allogeneic umbilical cord blood-derived mesenchymal stem cells combined with high tibial osteotomy: A retrospective study on safety and early results. Int. Orthop. 2021, 45, 481–488. [Google Scholar] [CrossRef]
- Anderson, D.E.; Williams III, R.J.; DeBerardino, T.M.; Taylor, D.C.; Ma, C.B.; Kane, M.S.; Crawford, D.C. Magnetic resonance imaging characterization and clinical outcomes after NeoCart surgical therapy as a primary reparative treatment for knee cartilage injuries. Am. J. Sport. Med. 2017, 45, 875–883. [Google Scholar] [CrossRef]
- De Windt, T.S.; Welsch, G.H.; Brittberg, M.; Vonk, L.A.; Marlovits, S.; Trattnig, S.; Saris, D.B. Is magnetic resonance imaging reliable in predicting clinical outcome after articular cartilage repair of the knee? A systematic review and meta-analysis. Am. J. Sport. Med. 2013, 41, 1695–1702. [Google Scholar] [CrossRef] [PubMed]
- Koh, I.J.; Kim, M.W.; Kim, J.H.; Han, S.Y.; In, Y. Trends in high tibial osteotomy and knee arthroplasty utilizations and demographics in Korea from 2009 to 2013. J. Arthroplast. 2015, 30, 939–944. [Google Scholar] [CrossRef]
- Taghizadeh, R.; Cetrulo, K.; Cetrulo, C. Wharton’s Jelly stem cells: Future clinical applications. Placenta 2011, 32, S311–S315. [Google Scholar] [CrossRef] [PubMed]
- Park, Y.B.; Ha, C.W.; Lee, C.H.; Yoon, Y.C.; Park, Y.G. Cartilage Regeneration in Osteoarthritic Patients by a Composite of Allogeneic Umbilical Cord Blood-Derived Mesenchymal Stem Cells and Hyaluronate Hydrogel: Results from a Clinical Trial for Safety and Proof-of-Concept with 7 Years of Extended Follow-Up. Stem Cells Transl. Med. 2017, 6, 613–621. [Google Scholar] [CrossRef] [PubMed]
- Zhang, X.; Hirai, M.; Cantero, S.; Ciubotariu, R.; Dobrila, L.; Hirsh, A.; Igura, K.; Satoh, H.; Yokomi, I.; Nishimura, T. Isolation and characterization of mesenchymal stem cells from human umbilical cord blood: Reevaluation of critical factors for successful isolation and high ability to proliferate and differentiate to chondrocytes as compared to mesenchymal stem cells from bone marrow and adipose tissue. J. Cell. Biochem. 2011, 112, 1206–1218. [Google Scholar] [PubMed]
- Song, J.S.; Hong, K.T.; Kim, N.M.; Jung, J.Y.; Park, H.S.; Kim, Y.C.; Shetty, A.A.; Kim, S.J. Allogenic umbilical cord blood-derived mesenchymal stem cells implantation for the treatment of juvenile osteochondritis dissecans of the knee. J. Clin. Orthop. Trauma 2019, 10, S20–S25. [Google Scholar] [CrossRef]
- Liang, X.; Ding, Y.; Zhang, Y.; Tse, H.-F.; Lian, Q. Paracrine mechanisms of mesenchymal stem cell-based therapy: Current status and perspectives. Cell Transplant. 2014, 23, 1045–1059. [Google Scholar] [CrossRef]
- Gnecchi, M.; Danieli, P.; Malpasso, G.; Ciuffreda, M.C. Paracrine mechanisms of mesenchymal stem cells in tissue repair. Mesenchymal Stem Cells 2016, 1416, 123–146. [Google Scholar]
- Jo, C.H.; Chai, J.W.; Jeong, E.C.; Oh, S.; Shin, J.S.; Shim, H.; Yoon, K.S. Intra-articular injection of mesenchymal stem cells for the treatment of osteoarthritis of the knee: A 2-year follow-up study. Am. J. Sport. Med. 2017, 45, 2774–2783. [Google Scholar] [CrossRef] [PubMed]
- Mithoefer, K.; McAdams, T.; Williams, R.J.; Kreuz, P.C.; Mandelbaum, B.R. Clinical efficacy of the microfracture technique for articular cartilage repair in the knee: An evidence-based systematic analysis. Am. J. Sport. Med. 2009, 37, 2053–2063. [Google Scholar] [CrossRef]
- Goyal, D.; Keyhani, S.; Lee, E.H.; Hui, J.H.P. Evidence-based status of microfracture technique: A systematic review of level I and II studies. Arthrosc. J. Arthrosc. Relat. Surg. 2013, 29, 1579–1588. [Google Scholar] [CrossRef] [PubMed]
- Bert, J.M. Abandoning microfracture of the knee: Has the time come? Arthrosc. J. Arthrosc. Relat. Surg. 2015, 31, 501–505. [Google Scholar] [CrossRef] [PubMed]
- Suh, D.W.; Han, S.B.; Yeo, W.J.; Cheong, K.; So, S.Y.; Kyung, B.S. Human umbilical cord-blood-derived mesenchymal stem cell can improve the clinical outcome and Joint space width after high tibial osteotomy. Knee 2021, 33, 31–37. [Google Scholar] [CrossRef]
- Yang, H.Y.; Song, E.K.; Kang, S.J.; Kwak, W.K.; Kang, J.K.; Seon, J.K. Allogenic umbilical cord blood-derived mesenchymal stromal cell implantation was superior to bone marrow aspirate concentrate augmentation for cartilage regeneration despite similar clinical outcomes. Knee Surg. Sport. Traumatol Arthrosc. 2022, 30, 208–218. [Google Scholar] [CrossRef]

Inclusion criteria
|
Exclusion criteria
|
| Study | Inclusion Criteria | Number of Patients | Age, Mean ± SD | BMI, kg/m2, Mean ± SD | Defect, cm2, Mean ± SD | Follow-Up | Outcome | Concomitant Intervention (HTO) | Study Design | etc. | |
|---|---|---|---|---|---|---|---|---|---|---|---|
| Total | Each Group | ||||||||||
| chung 2021 [23] | younger than 65 years, ICRS grade III or IV cartilage defects (>2 cm2), mechanical femorotibial varus angles > 3°, and KL grade 3 | 93 | N/A | 56.6 years (43–65) | 25.8 kg/m2 (20.9–33.2) | median 6.5 cm2 (2.0–12.8) | mean 1.7 Y (1.0–3.5 Y) | IKDC, WOMAC, KSS, HSS, and ICRS | with HTO | retrospective cohort | N/A |
| song 2020 (1) [19] | older than 40 years, ICRS IV (>2 cm2), KL grade 1–3, and femorotibial angle (varus or valgus) < 8° | 128 | N/A | 56.5 ± 7.9 (40–78) | 24.6 ± 3.6 kg/m2 (17–45.8) | one/two/three, 67 (4.5 ± 1.3)/49 (7.3 ± 2.9)/12 (9.8 ± 3.6) | 36.1 ± 6.4 M (25–47 M) | VAS, WOMAC, IKDC, and MOCART (for 34 pts) | without HTO | retrospective cohort | subgroup analysis: trochlea lesion, age, and lesion size |
| song 2020 (2) [18] | older than 40 years, ICRS IV (>4 cm2) in medial compartment, KL grade 1–3, and femorotibial angle varus > 5° | 125 | with trochlea lesion: 73 | 58.3 ± 6.8 (43–74) | 25.6 ± 2.7 kg/m2 (19.2–35.5) | 6.9 ± 2 cm2 | 3 Y | VAS, WOMAC, IKDC, and ICRS | with HTO | retrospective cohort | subgroup analysis: age, obesity, lesion size, location, and number of lesions |
| without trochlea lesion: 52 | |||||||||||
| song 2020 (3) [21] | older than 60 years with a kissing lesion of the medial compartment, full-thickness chondral defect ≥ 4 cm2 of MFC, and varus deformity ≥3° | 25 | N/A | 64.9 ± 4.4 (60–76) | 24.9 ± 3.1 kg/m2 (19.2–34.2) | total: 9.4 ± 3.1 cm2 (5.3–18.9 cm2), MFC: 7.2 ± 1.9 cm2 (4.2–12.8 cm2), and MTC: 2.2 ± 1.1 cm2 (0.2–6.1 cm2) | 26.7 ± 1.8 M (24–31 M) | VAS, WOMAC, IKDC, and ICRS | with HTO | retrospective cohort | with kissing lesion subgroup analysis: age, BMI, and lesion size |
| Lee 2021 [22] | ICRS ≥ 3B with kissing lesion in medial compartment | 74 | BMAC: 42 | 60.7 ± 4.1 | 26.1 ± 2.8 kg/m2 | 6.5 ± 2.9 cm2 | 20.7 ± 6.1 M | HSS, WOMAC, KSS, and ICRS | with HTO | retrospective cohort | with kissing lesion |
| hUCB-MSC: 32 | 58.1 ± 3.6 | 26.6 ± 3.0 kg/m2 | 7.0 ± 1.9 cm2 | 15.6 ± 2.8 M | |||||||
| Ryu 2022 [20] | KL grade ≤ 2, ICRS IV, older than 15 years, and lesion size 2–10 cm2 (BMAC 15–50 yrs) | 52 | BMAC: 25 | 39.64 ± 9.83 | 26.19 ± 3.74 kg/m2 | 4.33 ± 1.66 cm2 | VAS, IKDC, KOOS, and MOCART | 5 pts with HTO | retrospective cohort | subgroup analysis based on age (45 yrs) | |
| hUCB-MSC: 27 | 53.93 ± 8.6 | 26.38 ± 3.54 kg/m2 | 4.77 ± 1.81 cm2 | 2 Y | 8 pts with HTO | ||||||
| Lim 2021 [17] | aged > 18 years, full-thickness chondral defect 2–9 cm2, ICRS 4, and KL grade 1–3 | 89 | hUCB-MSC: 43 | 55.3 ± 8.9 | 25.7 ± 2.8 kg/m2 | 4.9 ± 2.0 cm2 | 2 Y | VAS, IKDC, WOMAC, and ICRS | without HTO | extended study after RCT | subgroup analysis: age, lesion size |
| microfracture: 46 | 54.4 ± 10.8 | 26.7 ± 3.9 kg/m2 | 4.0 ± 1.8 cm2 | 2 Y | |||||||
| numbers of patients (extended follow-up data after RCT) | 73 | hUCB-MSC: 36 | 36 M: 33 (3 loss) | 48 M: 28 (4 loss, 3 withdrew consent, and 1 AE) | 60 M: 29 (3 loss, 3 withdrew consent, and 1 AE) | 5 Y | |||||
| microfracture: 37 | 36 M: 36 (1 loss) | 48 M: 30 (6 withdrew consent, 1 reintervention) | 60 M: 28 (7 withdrew consent, 2 reintervention) | 5 Y | |||||||
| Selection | Comparability | Outcome | |||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|
| Study | Representativeness of the Exposed Cohort | Selection of Non-exposed Cohort | Ascertainment of Exposure | Outcome of Interest | Cohorts | Control for Additional Factor | Assessment of Outcome | Sufficient Follow-Up | Adequacy of Follow-Up | Total | Quality |
| chung 2021 [23] | * | 0 | * | * | * | 0 | * | * | 0 | 6 | moderate |
| song 2020 (1) [19] | * | 0 | * | * | * | 0 | * | * | 0 | 6 | moderate |
| song 2020 (2) [18] | * | 0 | * | * | * | 0 | * | * | 0 | 6 | moderate |
| song 2020 (3) [21] | * | 0 | * | * | * | 0 | * | * | 0 | 6 | moderate |
| Lee 2021 [22] | * | * | * | * | * | 0 | * | * | 0 | 7 | high |
| Ryu 2022 [20] | * | 0 | * | * | * | 0 | * | * | * | 7 | high |
| Lim 2021 [17] | * | * | * | * | * | 0 | * | * | * | 8 | high |
| Study | Follow-Up | Treatment and Subgroup | IKDC | WOMAC | VAS | ||||||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
| chung 2021 [23] | mean 1.7 Y (1.0–3.5) | hUCB-MSC | pre | final | pre | final | N/A | ||||||||||
| 39.0 ± 10.4 | 71.3 ± 5.9 | 44.5 ± 15.1 | 11.0 ± 3.7 | ||||||||||||||
| song (1) 2020 [19] | 36.1 ± 6.4 M (25–47) | hUCB-MSC | pre | 1 Y | final | pre | 1 Y | final | pre | 1 Y | final | ||||||
| 32.5 ± 8.3 | 55.8 ± 14.3 | 61.2 ± 17.2 | 39.3 ± 12.2 | 17.2 ± 12.7 | 13.9 ± 14.1 | 7.0 ± 1.6 | 2.5 ± 1.7 | 2.0 ± 2.1 | |||||||||
| song (2) 2020 [18] | 3 Y | hUCB-MSC | pre | 1 Y | 2 Y | 3 Y | pre | 1 Y | 2 Y | 3 Y | pre | 1 Y | 2 Y | 3 Y | |||
| trochlear lesion | 29.3 ± 7.3 | 56.7 ± 9.7 | 61.6 ± 10.7 | 64.7 ± 11 | 44.8 ± 10.3 | 13.8 ± 7.5 | 10.7 ± 6.9 | 8.4 ± 6.4 | 7.8 ± 1.2 | 2.6 ± 1.7 | 2.1 ± 1.5 | 1.6 ± 1.4 | |||||
| no trochlear lesion | 28.5 ± 7.6 | 56.7 ± 9.7 | 61.4 ± 9.5 | 65.3 ± 11.4 | 43.1 ± 11.1 | 13.2 ± 8.2 | 11.3 ± 8.5 | 8.4 ± 6.8 | 7.3 ± 1.3 | 2.3 ± 1.6 | 2.0 ± 1.7 | 1.4 ± 1.6 | |||||
| song (3) 2020 [21] | 26.7 ± 1.8 (24–31) | hUCB-MSC | pre | 1 Y | 2 Y | pre | 1 Y | 2 Y | pre | 1 Y | 2 Y | ||||||
| 24.3 ± 11.1 | 58.9 ± 10.3 | 68.5 ± 12.7 | 57.3 ± 11.4 | 15.6 ± 9.6 | 10.2 ± 7.9 | 76.4 ± 16.6 | 20.4 ± 15.1 | 12.8 ± 11.7 | |||||||||
| Lee 2021 [22] | pre | final | |||||||||||||||
| 20.7 ± 6.1 M | BMAC | N/A | 43.9 ± 12.7 | 23.4 ± 11.6 | N/A | ||||||||||||
| 15.6 ± 2.8 M | hUCB-MSC | N/A | 45.2 ± 8.8 | 19.5 ± 15.8 | N/A | ||||||||||||
| Ryu 2022 [20] | pre | final | pre | final | |||||||||||||
| 2 Y | BMAC | 44.17 ± 12.5 | 80.27 ± 9.48 | N/A | 5.2 ± 1.1 | 0.92 ± 0.98 | |||||||||||
| hUCB-MSC | 42.02 ± 13.63 | 81.35 ± 11.07 | N/A | 5.0 ± 1.2 | 0.85 ± 0.86 | ||||||||||||
| Study | Follow-up | Treatment and Subgroup | IKDC | WOMAC | VAS | ||||||||||||
| Lim 2021 [17] | pre | 48 weeks | 3 Y | 4 Y | 5 Y | pre | 48 weeks | 3 Y | 4 Y | 5 Y | pre | 48 weeks | 3 Y | 4 Y | 5 Y | ||
| 5 Y | microfracture | 41.8 ± 13.4 | 53.5 (48.5 to 58.5) | 49.0 (43.3 to 54.7) | 48.9 (42.1 to 55.7) | 47.1 (41.1 to 53.2) | 40.4 ± 14.8 | 26.2 (21.1 to 31.2) | 34.5 (27.2 to 41.8) | 35.8 (27.6 to 44.1) | 36.2 (28.6 to 43.8) | 44.6 ± 12.9 | 24.1 (18.3 to 29.9) | 41.1 (32.2 to 50.0) | 43.3 (34.7 to 51.8) | 43.5 (35.3 to 51.6) | |
| hUCB-MSC | 42.7 ± 13.9 | 53.4 (49.0 to 57.8) | 57.4 (50.8 to 64.1) | 53.7 (48.2 to 59.3) | 54.7 (48.7 to 60.7) | 37.4 ± 15.1 | 24.7 (20.5 to 28.9) | 25.4 (19.9 to 31.0) | 28.6 (22.4 to 34.9) | 26.9 (20.4 to 33.5) | 44.0 ± 12.5 | 24.2 (17.5 to 31.0) | 30.9 (23.6 to 38.2) | 35.7 (29.2 to 42.3) | 29.1 (22.4 to 35.8) | ||
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2022 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Lee, D.H.; Kim, S.A.; Song, J.-S.; Shetty, A.A.; Kim, B.-H.; Kim, S.J. Cartilage Regeneration Using Human Umbilical Cord Blood Derived Mesenchymal Stem Cells: A Systematic Review and Meta-Analysis. Medicina 2022, 58, 1801. https://doi.org/10.3390/medicina58121801
Lee DH, Kim SA, Song J-S, Shetty AA, Kim B-H, Kim SJ. Cartilage Regeneration Using Human Umbilical Cord Blood Derived Mesenchymal Stem Cells: A Systematic Review and Meta-Analysis. Medicina. 2022; 58(12):1801. https://doi.org/10.3390/medicina58121801
Chicago/Turabian StyleLee, Dong Hwan, Seon Ae Kim, Jun-Seob Song, Asode Ananthram Shetty, Bo-Hyoung Kim, and Seok Jung Kim. 2022. "Cartilage Regeneration Using Human Umbilical Cord Blood Derived Mesenchymal Stem Cells: A Systematic Review and Meta-Analysis" Medicina 58, no. 12: 1801. https://doi.org/10.3390/medicina58121801
APA StyleLee, D. H., Kim, S. A., Song, J.-S., Shetty, A. A., Kim, B.-H., & Kim, S. J. (2022). Cartilage Regeneration Using Human Umbilical Cord Blood Derived Mesenchymal Stem Cells: A Systematic Review and Meta-Analysis. Medicina, 58(12), 1801. https://doi.org/10.3390/medicina58121801







