Clinical Application of the Computed-Tomography-Based Three-Dimensional Models in the Surgical Planning and Intraoperative Navigation of Ureteropelvic Junction Obstruction Complicated with Renal Calculi
Abstract
:1. Introduction
2. Methods and Materials
2.1. Patient Selection and Management
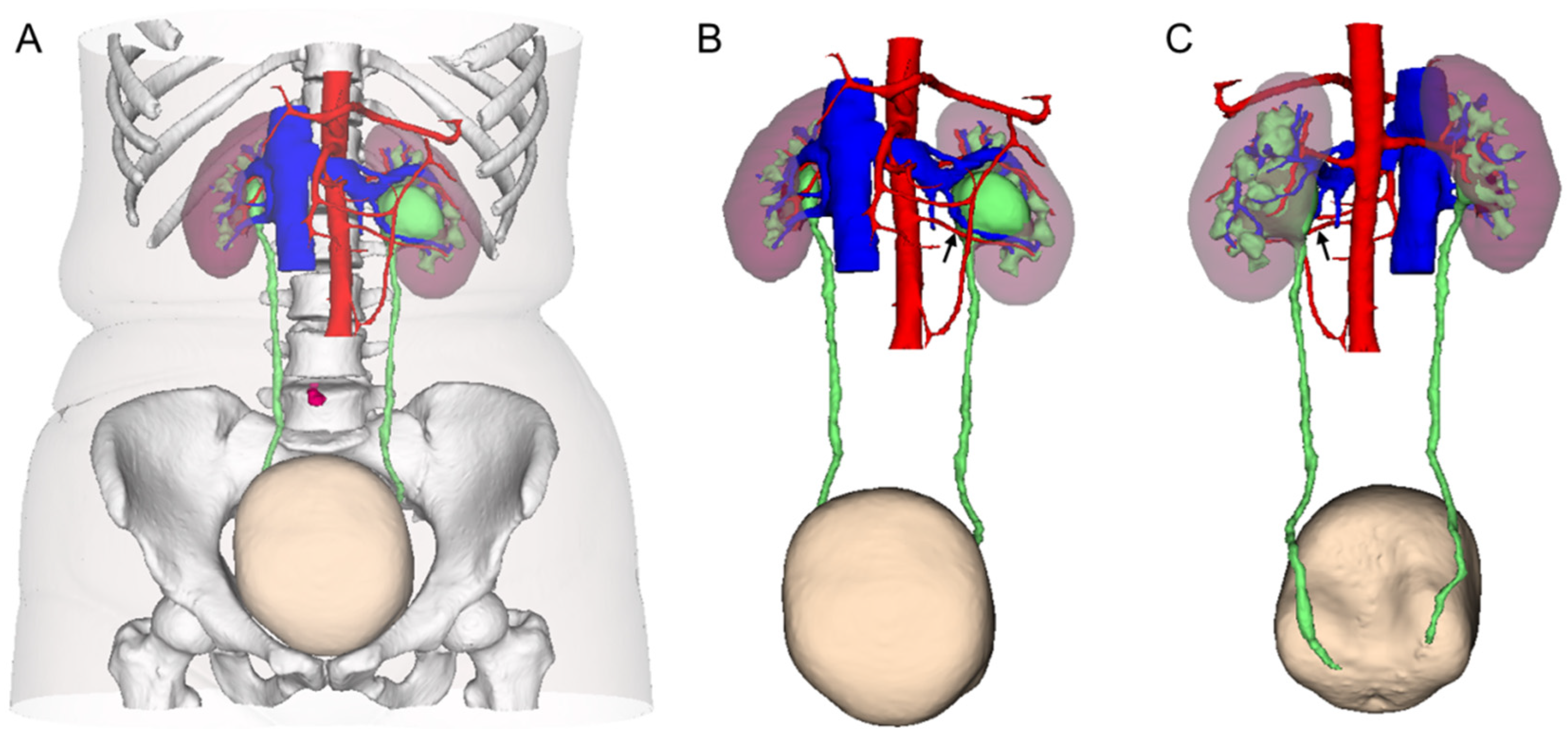
2.2. 3D CT Reconstruction and Stone Evaluation
2.3. Patient Grouping and Surgical Planning
2.4. Surgical Techniques
2.5. Statistical Analysis
3. Results
3.1. Characteristics of Patients and Renal Calculi
3.2. Perioperative and Follow-Up Data
4. Discussion
5. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Conflicts of Interest
Abbreviations
| 3D CT | Three-dimensional computed tomography |
| UPJ | Ureteropelvic junction |
| UPJO | Ureteropelvic junction obstruction |
| LP | Laparoscopic pyeloplasty |
| TLP | Traditional laparoscopic pyeloplasty |
| RALP | Robot-assisted laparoscopic pyeloplasty |
| PCNL | Percutaneous nephrolithotomy |
| eGFR | Estimated glomerular filtration rate |
References
- Scarcella, S.; Tiroli, M.; Torino, G.; Mariscoli, F.; Cobellis, G.; Galosi, A.B. Combined treatment of ureteropelvic junction obstruction and renal calculi with robot-assisted laparoscopic pyeloplasty and laser lithotripsy in children: Case report and non-systematic review of the literature. Int. J. Med. Robot. 2021, 17, e2246. [Google Scholar] [CrossRef] [PubMed]
- Kouriefs, C.; Georgiades, F.; Grange, P. Stones First! A Gas Pyelo-nephroscopy Strategy for Laparoscopic Pyeloplasty and Renal Stone Extraction. Urology 2017, 109, 206–209. [Google Scholar] [CrossRef] [PubMed]
- Stasinou, T.; Bourdoumis, A.; Masood, J. Forming a stone in pelviureteric junction obstruction: Cause or effect? Int. Braz. J. Urol. 2017, 43, 13–19. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Skolarikos, A.; Dellis, A.; Knoll, T. Ureteropelvic obstruction and renal stones: Etiology and treatment. Urolithiasis 2015, 43, 5–12. [Google Scholar] [CrossRef] [PubMed]
- Li, H.; Chen, Y.; Liu, C.; Li, B.; Xu, K.; Bao, S. Construction of a three-dimensional model of renal stones: Comprehensive planning for percutaneous nephrolithotomy and assistance in surgery. World J. Urol. 2013, 31, 1587–1592. [Google Scholar] [CrossRef]
- Porpiglia, F.; Fiori, C.; Checcucci, E.; Amparore, D.; Bertolo, R. Hyperaccuracy Three-dimensional Reconstruction Is Able to Maximize the Efficacy of Selective Clamping During Robot-assisted Partial Nephrectomy for Complex Renal Masses. Eur. Urol. 2018, 74, 651–660. [Google Scholar] [CrossRef]
- Zhang, L.; Fang, D.; Li, X.; Yao, L.; Xiong, G.; He, Z.; Zhou, L. Transperitoneal Subcostal Access for Urologic Laparoscopy: Experience of a Large Chinese Center. BioMed Res. Int. 2016, 2016, 4062390. [Google Scholar] [CrossRef]
- Yang, K.; Yao, L.; Li, X.; Zhang, C.; Wang, T.; Zhang, L.; Fang, D.; He, Z.; Zhou, L. A modified suture technique for transperitoneal laparoscopic dismembered pyeloplasty of pelviureteric junction obstruction. Urology 2015, 85, 263–267. [Google Scholar] [CrossRef]
- Hong, P.; Ding, G.P.; Zhu, D.D.; Yang, K.L.; Pan, J.H.; Li, X.S.; Chen, Z.P.; Zhang, L.; Tang, Q.; Hao, H.; et al. Head-to-Head Comparison of Modified Laparoscopic Pyeloplasty and Robot-Assisted Pyeloplasty for Ureteropelvic Junction Obstruction in China. Urol. Int. 2018, 101, 337–344. [Google Scholar] [CrossRef]
- Shin, T.; Ukimura, O.; Gill, I.S. Three-dimensional Printed Model of Prostate Anatomy and Targeted Biopsy-proven Index Tumor to Facilitate Nerve-sparing Prostatectomy. Eur. Urol. 2016, 69, 377–379. [Google Scholar] [CrossRef]
- Bertolo, R.; Autorino, R.; Fiori, C.; Amparore, D.; Checcucci, E.; Mottrie, A.; Porter, J.; Haber, G.P.; Derweesh, I.; Porpiglia, F. Expanding the Indications of Robotic Partial Nephrectomy for Highly Complex Renal Tumors: Urologists’ Perception of the Impact of Hyperaccuracy Three-Dimensional Reconstruction. J. Laparoendosc. Adv. Surg. Tech. A 2019, 29, 233–239. [Google Scholar] [CrossRef] [PubMed]
- Yang, C.; Zhou, J.; Lu, Z.X.; Hao, Z.; Wang, J.; Zhang, L.; Liang, C. Simultaneous treatment of ureteropelvic junction obstruction complicated by renal calculi with robotic laparoscopic surgery and flexible cystoscope. World J. Urol. 2019, 37, 2217–2223. [Google Scholar] [CrossRef] [PubMed]
- Brehmer, M.; Beckman, M.O.; Magnusson, A. Three-dimensional computed tomography planning improves percutaneous stone surgery. Scand. J. Urol. 2014, 48, 316–323. [Google Scholar] [CrossRef] [PubMed]
- Pradere, B.; Doizi, S.; Proietti, S.; Brachlow, J.; Traxer, O. Evaluation of Guidelines for Surgical Management of Urolithiasis. J. Urol. 2018, 199, 1267–1271. [Google Scholar] [CrossRef] [PubMed]
- Abdrabuh, A.M.; Salih, E.M.; Aboelnasr, M.; Galal, H.; El-Emam, A.; El-Zayat, T. Endopyelotomy versus redo pyeoloplasty for management of failed pyeloplasty in children: A single center experience. J. Pediatr. Surg. 2018, 53, 2250–2255. [Google Scholar] [CrossRef] [PubMed]
- Kadihasanoglu, M.; Yucetas, U.; Karabay, E.; Sonmezay, E. Comparison of the outcomes of laparoscopic pyeloplasty with and without concomitant pyelolithotomy. Int. Braz. J. Urol. 2019, 45, 965–973. [Google Scholar] [CrossRef] [Green Version]
- Yin, Z.; Wei, Y.B.; Liang, B.L.; Zhou, K.Q.; Gao, Y.L.; Yan, B.; Wang, Z.; Yang, J.R. Initial experiences with laparoscopy and flexible ureteroscopy combination pyeloplasty in management of ectopic pelvic kidney with stone and ureter-pelvic junction obstruction. Urolithiasis 2015, 43, 255–260. [Google Scholar] [CrossRef]
- Hong, P.; Li, Z.; Zhu, D.; Zhuang, L.; Yang, K.; Hao, H.; Li, X.; Zhou, L. A Simple Modification for the Usage of Flexible Cystoscope in Modified Laparoscopic Pyeloplasty for Ureteropelvic Junction Obstruction with Renal Calculi: A Flexible Guiding Tube. Urol. Int. 2019, 102, 262–268. [Google Scholar] [CrossRef]
- Zheng, J.; Yan, J.; Zhou, Z.; Chen, Z.; Li, X.; Pan, J.; Li, W. Concomitant treatment of ureteropelvic junction obstruction and renal calculi with robotic laparoscopic surgery and rigid nephroscopy. Urology 2014, 83, 237–242. [Google Scholar] [CrossRef]
- Koh, L.T.; Ng, F.C.; Ng, K.K. Outcomes of long-term follow-up of patients with conservative management of asymptomatic renal calculi. BJU Int. 2012, 109, 622–625. [Google Scholar] [CrossRef]
- Darrad, M.P.; Yallappa, S.; Metcalfe, J.; Subramonian, K. The natural history of asymptomatic calyceal stones. BJU Int. 2018, 122, 263–269. [Google Scholar] [CrossRef] [PubMed]




| Variables | LP | LP with Pyelolithotomy | LP with Endoscopy | Total | p Values |
|---|---|---|---|---|---|
| Number of patients, n | 6 | 11 | 9 | 26 | - |
| Gender, n | 0.526 | ||||
| Male | 3 | 8 | 7 | 18 | |
| Female, | 3 | 3 | 2 | 8 | |
| Age, years | 36.7 ± 14.2 | 27.7 ± 8.9 | 31.9 ± 11.9 | 31.2 ± 11.7 | 0.329 |
| BMI, kg/m2 | 22.9 ± 3.5 | 23.7 ± 2.0 | 25.1 ± 4.6 | 24.1 ± 3.6 | 0.455 |
| Side of UPJO and stones, no. of patients, n | 0.450 | ||||
| Right | 2 | 2 | 2 | 6 | |
| Left | 4 | 7 | 7 | 18 | |
| Bilateral | 0 | 0 | 2 | 2 | |
| eGFR, mL/min | 102.3 ± 18.1 | 112.6 ± 22.9 | 110.7 ± 16.7 | 107.7 ± 15.0 | 0.590 |
| No. of crossing vessel, n | 2 | 2 | 1 | 5 | 0.494 |
| Affected renal parenchymal volume, mL | 149.2 ± 52.8 | 190.7 ± 65.4 | 156.6 ± 43.1 | 166.6 ± 54.3 | 0.360 |
| Affected renal hydronephrosis volume, mL | 81.0 ± 26.3 | 193.8 ± 121.3 | 126.6 ± 92.4 | 138.7 ± 144.2 | 0.413 |
| Hydronephrosis degree, no. of patients, n | 0.310 | ||||
| Mild | 4 | 7 | 3 | 14 | |
| Moderate or severe | 2 | 4 | 6 | 12 | |
| Stones, no. of patients, n | 0.384 | ||||
| Single | 4 | 4 | 3 | 11 | |
| Multiple | 2 | 7 | 6 | 15 | |
| Distribution of stones, no. of patients, n | 0.499 | ||||
| Upper calyces | 0 | 1 | 2 | 3 | |
| Middle or lower calyces | 6 | 10 | 7 | 23 | |
| Involved renal calyces, no. of patients, n | 0.041 * | ||||
| ≤2, | 6 | 9 | 4 | 19 | |
| >3 | 0 | 2 | 5 | 7 | |
| Maximum cross-sectional area, mm2 | 51.50 ± 29.44 | 176.30 ± 89.58 | 347.59 ± 113.98 | 206.79 ± 89.51 | 0.036 * |
| Variables | LP | LP with Pyelolithotomy | LP with Endoscopy | Total | p Values |
|---|---|---|---|---|---|
| Options of pyeloplasty, no. of patients, n | 0.119 | ||||
| Traditional laparoscopic | 2 | 4 | 7 | 13 | |
| Robot-assisted laparoscopic | 4 | 7 | 2 | 13 | |
| Operative time, min, | 150.2 ± 62.3 | 153.4 ± 47.2 | 136.1 ± 37.9 | 146.6 ± 46.7 | 0.716 |
| Estimated blood loss, mL | 25.8 ± 26.5 | 49.1 ± 57.3 | 32.7 ± 33.2 | 38.1 ± 43.6 | 0.540 |
| Intraoperative stone clearance rate, % | 0 | 100% (11/11) | 77.8% (7/9) | - | - |
| Pararenal draining time, day | 6.0 ± 5.4 | 3.4 ± 1.2 | 3.9 ± 1.2 | 4.2 ± 3.2 | 0.270 |
| Length of hospital stay after operation, day | 6.7 ± 6.1 | 4.2 ± 1.6 | 4.3 ± 1.0 | 4.8 ± 3.1 | 0.246 |
| Perioperative complications (>grade 2), n | 0 | 0 | 1 | 1 | - |
| Follow-up time, month | 18.4 ± 6.7 | 20.1 ± 5.9 | 21.6 ± 6.3 | 19.4 ± 6.4 | 0.648 |
| Success rate of UPJO, n/N (%) | 5/6 (83.3) | 11/11 (100) | 9/9 (100) | 25/26 (96.2) | 0.193 |
| Success rate of renal calculi, n/N (%) | 4/6 (83.3) | 10/11 (90.9) | 7/9 (77.8) | 21/26 (80.8) | 0.592 |
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2022 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Xiong, S.; Zheng, M.; Liu, C.; Yang, K.; Li, Z.; Zhang, L.; Tian, Y.; Zhou, L.; Li, X. Clinical Application of the Computed-Tomography-Based Three-Dimensional Models in the Surgical Planning and Intraoperative Navigation of Ureteropelvic Junction Obstruction Complicated with Renal Calculi. Medicina 2022, 58, 1769. https://doi.org/10.3390/medicina58121769
Xiong S, Zheng M, Liu C, Yang K, Li Z, Zhang L, Tian Y, Zhou L, Li X. Clinical Application of the Computed-Tomography-Based Three-Dimensional Models in the Surgical Planning and Intraoperative Navigation of Ureteropelvic Junction Obstruction Complicated with Renal Calculi. Medicina. 2022; 58(12):1769. https://doi.org/10.3390/medicina58121769
Chicago/Turabian StyleXiong, Shengwei, Mengmeng Zheng, Chunlin Liu, Kunlin Yang, Zhihua Li, Lei Zhang, Ye Tian, Liqun Zhou, and Xuesong Li. 2022. "Clinical Application of the Computed-Tomography-Based Three-Dimensional Models in the Surgical Planning and Intraoperative Navigation of Ureteropelvic Junction Obstruction Complicated with Renal Calculi" Medicina 58, no. 12: 1769. https://doi.org/10.3390/medicina58121769





