Abstract
Background: Surgical incision pain, rebound pain, and recurrence can manifest themselves in different forms of postoperative pain after full endoscopic lumbar discectomy (FELD). This study aims to evaluate various postoperative pains after FELD and summarize their characteristics. Methods: Data about the demographic characteristics of patients, pain intensity, and functional assessment results were collected from January 2016 to September 2019. Clinical outcomes including Oswestry Disability Index (ODI) and visual analog scale (VAS) scores, were obtained. Results: A total of 206 patients were enrolled. ODI and VAS of the patients significantly decreased after FELD at 12-month follow-up. A total of 193 (93.7%) patients had mild surgical incision pain after FELD and generally a VAS < 4, and it mostly resolved on its own within 3 days. A total of 12 (5.8%) patients experienced rebound pain, which was typically characterized by pain (mainly leg pain with or without back pain), generally occurring within 2 weeks after FELD and lasting < 3 weeks. The pain levels of rebound pain were equal to or less than those of preoperative pain, and generally scored a VAS of < 6. The recurrence rate was 4.4%. Recurrence often occurs within three months after surgery, with the pain level of the recurrence being greater than or equal to the preoperative pain. Conclusions: Different types of postoperative pain have their own unique characteristics and durations, and treatment options are also distinct. Conservative treatment and analgesia may be indicated for rebound pain and surgical incision pain, but recurrence usually requires surgical treatment.
1. Introduction
Full endoscopic lumbar discectomy (FELD) has evolved rapidly in the treatment of degenerative lumbar spine disease [1,2,3,4]. Compared with traditional open surgery, FELD has evident advantages. These include a low volume of blood loss, less trauma, faster recovery, and a shorter length of hospitalization [5,6]. However, some patients still experience pain symptoms for a period of time after FELD [7,8,9]. The manifestations of postoperative pain after FELD are diverse, and the characteristics of pain have different causes [10]. Surgical incision pain, inadequate decompression, epidural hematoma, nerve root injury, and recurrence can manifest themselves in different forms of postoperative pain. In addition, during our clinical experience, we observed that some patients experience pain relief immediately after surgery, but after a few days they may feel mild pain in the back or leg, soreness and weakness in the back, or leg numbness, especially when they get up and stand or walk, but it is usually not too serious. This condition was referred to as rebound pain, and the pathological mechanism of recurrent transient pain after FELD is not yet fully elucidated. As a distinct pain phenomenon, it is not a notion that has gained widespread support. These postoperative pains vary in terms of presentation, appearance, duration, and degree. Some of these postoperative pains are temporary, while others require medication or surgical intervention. Obviously, if the surgeons have a good grasp of these postoperative pain characteristics, it will help them better address the patient’s pain and respond more accurately to the issue.
Thus far, there is no specific research about transient rebound pain. Hence, some studies have retrospectively analyzed the recurrence of transient pain in some patients who underwent FELD. On this basis, the current study aimed to assess various postoperative pains that appears after FELD, and summarizes the characteristics of various postoperative pains. We also sought evaluate the incidence, clinical features, and long-term clinical effects of rebound pain after FELD, to assess the risk factors of rebound pain, and to provide appropriate clinical diagnosis and treatment.
2. Materials and Methods
This is a retrospective study. The current study was approved by the institutional review board of Changhua Christian Hospital (CCH No.190905). After a cautious review of the data, we retrospectively selected 328 consecutive patients who underwent FELD from January 2016 to September 2019. The inclusion criteria were as follows: (1) patients with disc herniation with unilateral radiculopathy, with/without mild stenosis (2) those with single-level symptoms, and (3) those who received failed conservative treatment for more than 3 months. Patients with spinal instability, multilevel symptoms, spondylolisthesis or scoliosis, moderate/severe spinal stenosis, infection, trauma, neoplasm, recurrence, or a history of prior spinal surgery at the index level were excluded from the research.
In addition, based on the presence of recurrent transient pain after FELD, the patients were divided into rebound and non-rebound pain groups.
2.1. Surgical Technique
Using the transforaminal approach, the patients received epidural anesthesia while in the prone position under fluoroscopic guidance to confirm the surgical level. The working channel was inserted over the dilator and along the guide wire after a skin incision was made. An endoscope (SPINENDOS GmbH, München, Germany) was inserted into the working channel. In some cases, foraminoplasty was required to enlarge the working space via the removal of some bony tissues using a reamer, trephine, or high-speed burr. Then, the disc fragments were removed, and an annuloplasty was performed.
2.2. Postoperative Management
Postoperative dehydration and neurotrophic drugs were routinely administered. Patients were monitored for 24 h postoperatively, and they moved freely on the bed. One day after FELD, patients with a waist brace performed back muscle exercises. Simultaneously, we instructed our patients to minimize strenuous activity (strenuous activity refers to those activities that are vigorous, high volume, high frequency, and confrontational, with excessive load on the cardiorespiratory function; under normal circumstances a heart rate of more than 120 beats per minute after exercise is called strenuous exercise. Most anaerobic exercises are strenuous exercises, such as running, soccer, basketball, and high-volume equipment fitness) for 3–4 weeks after surgery and to wear a lumbar brace for at least 4 weeks after surgery.
2.3. Outcome Evaluation
Demographic data, including age, sex, smoking, body mass index (BMI), diagnosis, and surgical level, were collected. In addition, information regarding the operative time and complications was obtained.
Data about patient-reported functional outcomes, including visual analog scale (VAS) scores for back and leg pain and the Oswestry Disability Index (ODI) at each follow-up time, were prospectively collected. Moreover, VAS scores for surgical incision pain were monitored daily until 3 days postoperatively. The rebound pain group underwent weekly monitoring until 1 month and at 3, 6, and 12 (last f/u) months after surgery. The satisfaction rate was assessed based on the modified Macnab criteria (excellent or good outcomes) [11].
After discharge, we regularly conducted telephone follow-ups with patients to collect data on outcomes, including characteristics of pain, the occurrence of rebound pain, functional changes, and treatment efficacy. All of the data were collected by one research assistant.
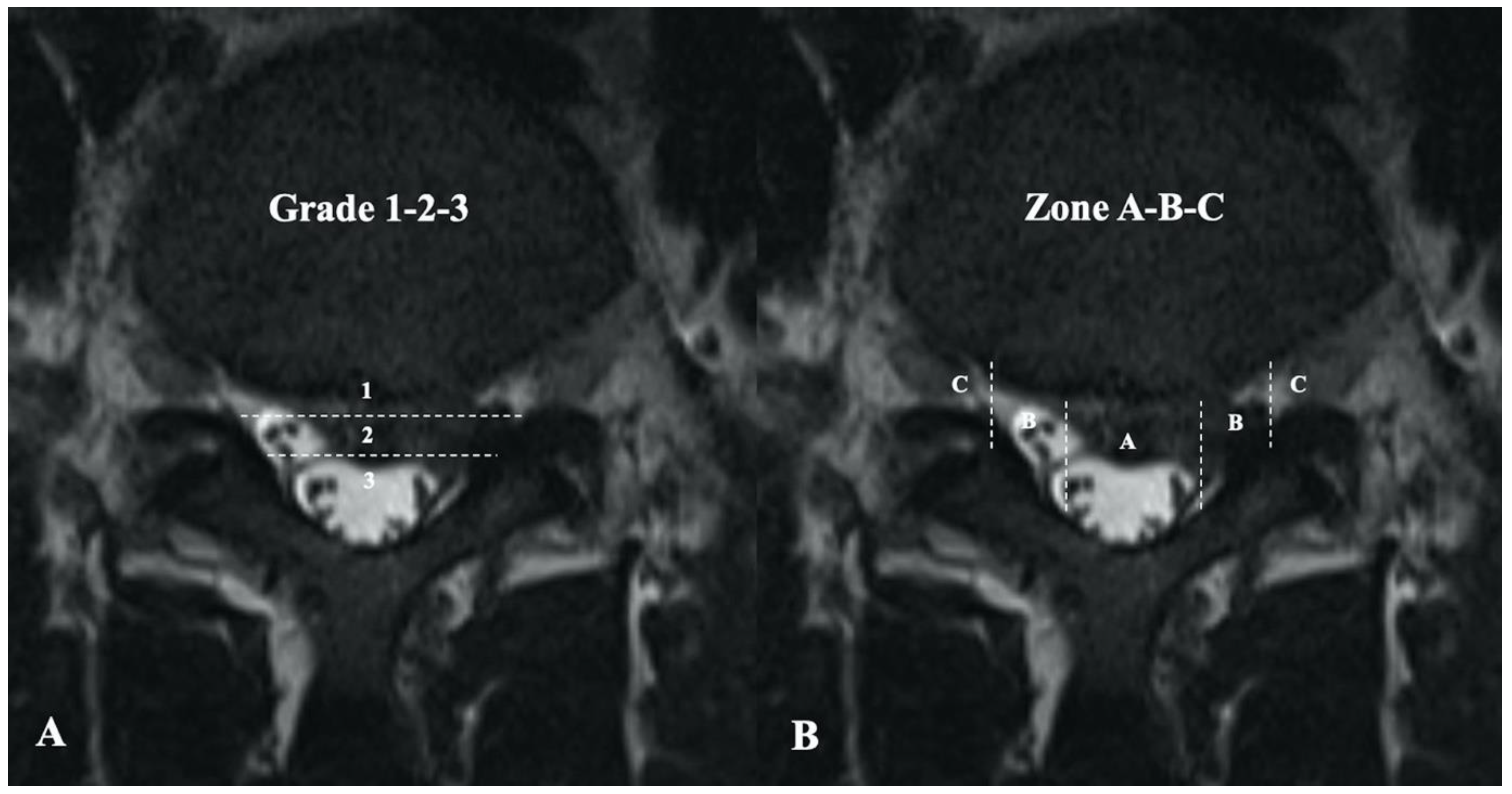
Preoperative magnetic resonance imaging (MRI) was performed to assess for Modic change and Schmorl’s node. The herniated disc size and location were evaluated using the Michigan State University classification (Figure 1) [12]. Lumbar disc degeneration was evaluated according to the Pfirrmann grading system [13]. MRI was again performed 3 months after surgery to observe for residual mass or recurrence. All radiological data were evaluated by two senior spine surgeons who were blinded to the study.
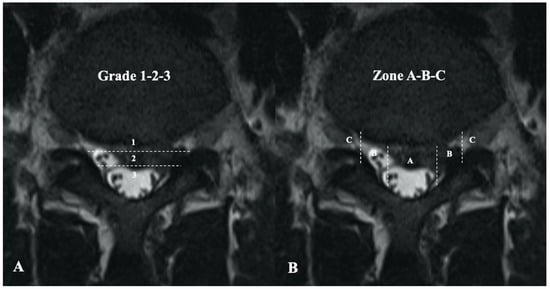
Figure 1.
Michigan State University classification of herniated lumbar discs on magnetic resonance imaging. (A) Grading of disc herniation according to size. Grade 1 lesions have minimal impact and grade 3 have the most significant effect on nerve compression. (B) Zoning of the disc to identify location. Lesions in tighter zones (B and C) had more impact.
2.4. Statistical Analysis
Quantitative variables were expressed as mean ± standard deviation. The two-sample t-test or the Kolmogorov–Smirnov test as well as the x2 test or the Fisher’s exact test were used to analyze continuous and categorical variables, respectively. The logistic regression model was used to assess the risk factors for rebound pain. Statistical analyses were performed using the Statistical Package for the Social Sciences software, version 24.0 (IBM Corp., Armonk, NY, USA). A p-value of <0.05 was considered statistically significant.
3. Results
3.1. General Information
122 patients were lost to follow-up. Finally, a total of 206 patients, including 99 men and 107 women, were enrolled in this study. The mean age and BMI of the participants were 36.7 ± 7.6 (range: 20–57) years and 22.1 ± 2.6 (range: 17.8–30.6) kg/m2, respectively. Moreover, there were 37 (17.9%) smokers, including 12 with lesions at the L3/4 level, 120 at the L4/5 level, and 74 at the L5/S1 level, presented with single-level lumbar disc herniation without stenosis. Only 11 patients exhibited Modic change at the index level, and 8 (3.9%) presented with Schmorl’s node at the index level. According to the Pfirrmann grading system, 63 presented with a grade I lesion, 130 with a grade II lesion, and 13 with a grade III lesion. The average operative time was 40.4 ± 7.0 (range: 25–54) mins.
3.2. Clinical Outcomes
In the current study, 193 out of 206 patients (93.7%) had mild surgical incision pain after FELD, and most of them could relieve the pain by themselves with appropriate analgesic drugs. The mean VAS for surgical incision pain decreased from 3.02 ± 0.68 on postoperative day-1 to 1.48 ± 0.59 on postoperative day-2 and 0.61 ± 0.69 on postoperative day-3. It seems that the surgical incision pain lasts about 3 days after FELD. In addition, most patients have VAS scores of less than 3, and a few patients reach 4.
One year after surgery, the VAS scores for back and leg pain significantly decreased from 5.6 ± 1.8 to 1.3 ± 1.1 and from 6.9 ± 1.5 to 1.2 ± 1.1, respectively (p < 0.05). Further, the ODI scores significantly improved from 49.3 ± 11.5 to 13.8 ± 5.5 (p < 0.05).
Nine patients experienced recurrence, with an incidence rate of 4.4%. According to our study, recurrence often occurred within 3 months after surgery. In most cases, the pain level of recurrence is greater than or equal to the preoperative pain (Table 1). Among them, eight required an additional endoscopic lumbar discectomy, and one underwent open fusion surgery.

Table 1.
Changes in VAS and ODI scores of recurrent pain in patients with time.
3.3. Rebound Pain Group
In total, 12 (5.8%) patients experienced rebound pain. Table 2 and Table 3 depict the demographic data and clinical characteristics of patients (n = 12) with rebound pain. There were three men and nine women, with an average age of 38.4 ± 2.4 (range: 26–46) years. Patients commonly presented with single-level lumbar disc herniation without stenosis (n = 11 [91.7%]), and these included five patients with lesions at the L4/5 and seven at the L5/S1. Rebound pain often occurred within 2 weeks after surgery, and it lasted less than 3 weeks. In most cases, the pain level of rebound pain was less than or equal to the preoperative pain, and a high proportion of patients had VAS scores of <6 (Table 4). According to the modified Macnab criteria, eight and four patients presented with excellent and good outcomes, respectively.

Table 2.
Characteristics of patients in the rebound pain group.

Table 3.
Changes in VAS and ODI scores of rebound pain in patients with time.

Table 4.
Demographic data of the two groups.
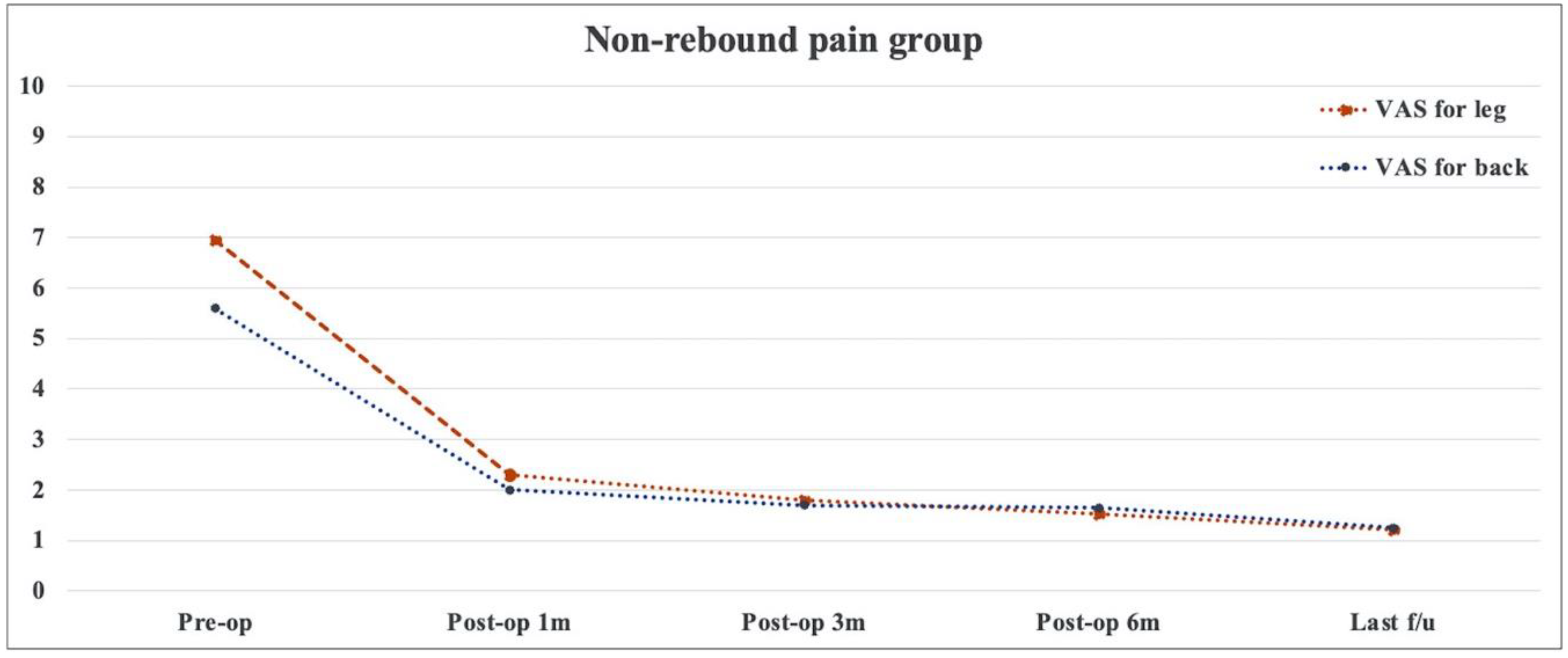
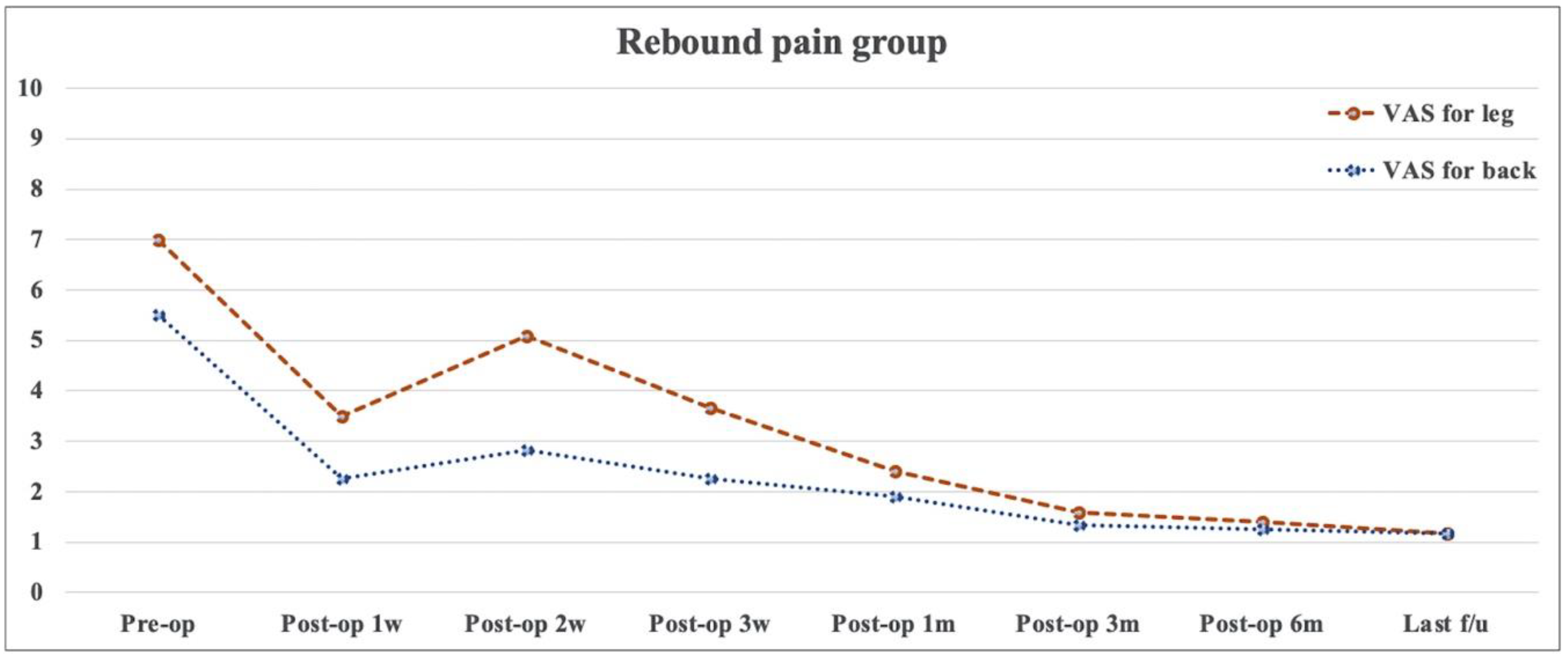
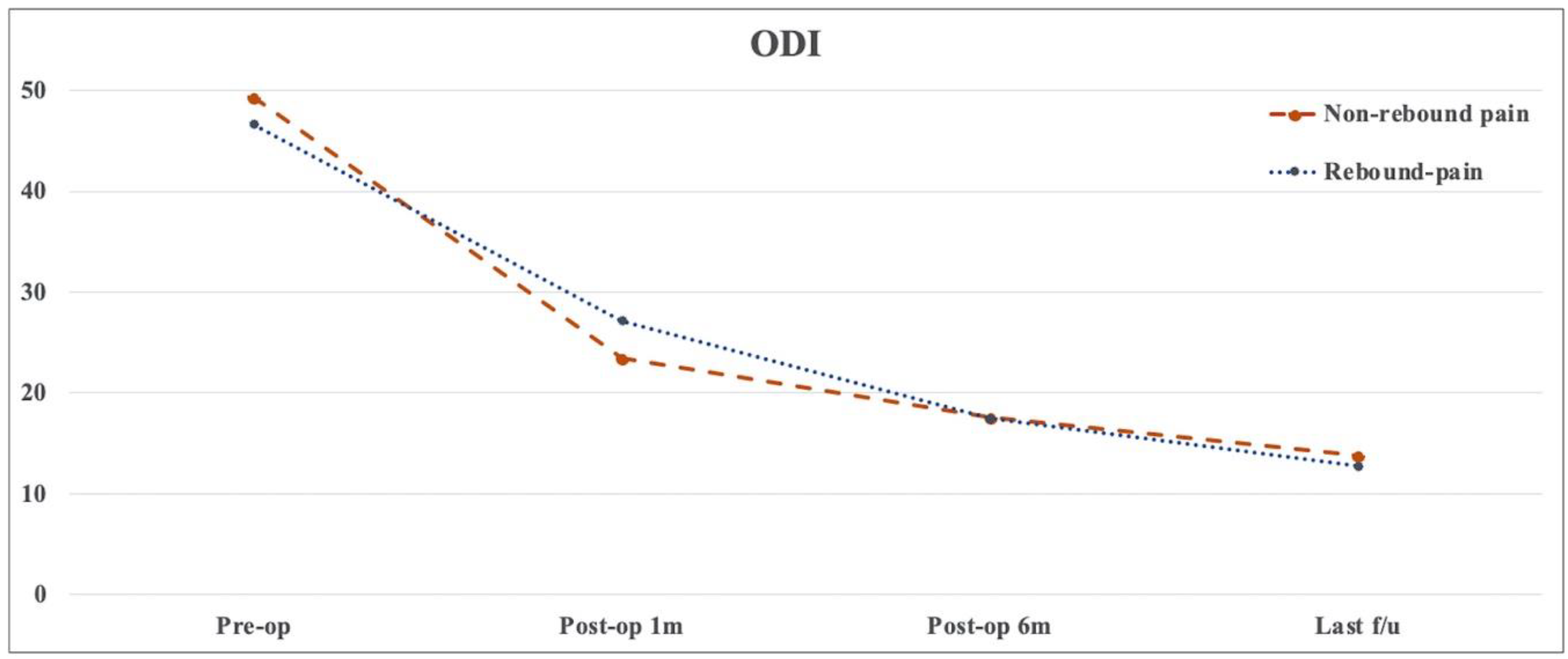
3.4. Subgroup Analysis
There was no significant difference in terms of age, sex, smoking, BMI, diagnosis, surgical level, operative time, and preoperative clinical outcomes between the non-rebound and rebound pain groups (p > 0.05) (Table 4). Table 5 presents the baseline data on disc herniation between the two groups. The herniated disc was commonly located on the 2-B side, followed by the 2-AB side. Results showed no significant differences between the two groups in terms of disc herniation size and location. Changes in pain and functional recovery between the two groups were compared, and results showed no significant differences in early postoperative and short-term efficacy (Figure 2, Figure 3 and Figure 4). In the logistic regression analysis, age, sex, BMI, diagnosis, surgical level and approach, Modic change, disc degeneration, operative time, and the preoperative VAS score and ODI did not significantly affect the development of postoperative rebound pain (p > 0.05) (Table 6).

Table 5.
The size and location of the herniated disc in the two groups (based on MSU classification).
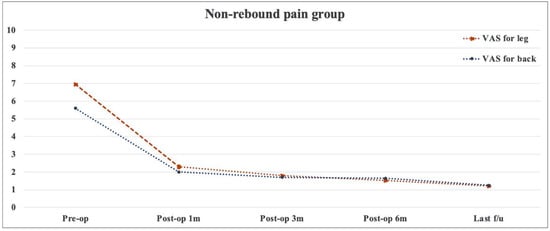
Figure 2.
Changes in visual analog scale scores with time in the non-rebound pain group.
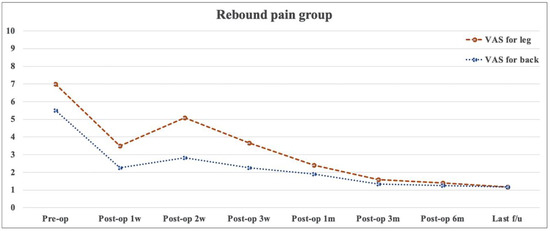
Figure 3.
Changes in visual analog scale scores with time in the rebound pain group.
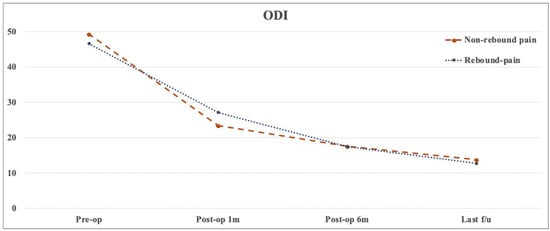
Figure 4.
Changes in the Oswestry disability index scores with time for the non-rebound and rebound pain groups.

Table 6.
Logistic regression analyses for the risk factors of rebound pain.
4. Discussion
At present, with the development of FELD and the accumulation of cases, increasing attention has been directed toward the treatment and prevention of complications. Previous studies have shown that this technique is associated with some complications, including nerve root injury, residual remnants, prominent recurrence, and postoperative transient/persistent pain [14,15]. Postoperative pain after FELD has various manifestations, and the different characteristics are correlated with varying causes. Further, the outcome and prognosis of clinical symptoms differ [16,17]. This study focused on various postoperative pains that occur after FELD and summarized the characteristics of various postoperative pains.
It is common to experience pain at the site of the incision. As the wound heals, the pain will decrease. Most of the pain and soreness will disappear when the wound is completely healed and the sutures or staples are removed. In open surgery, deep tissue soreness and pain usually last for one to two weeks. Similar to our study, most patients (93.7%) had mild surgical incision pain after surgery. However, it mostly resolved on its own within 3 days, which is a benefit of FELD’s lower trauma.
Previously, some experienced spine surgeons considered rebound pain only an empirical finding, and it was even disregarded by several surgeons. To date, there is no relevant study about this unique condition, and standardized diagnostic criteria are not available. The pathogenesis of rebound pain has not been fully elucidated, and it may be correlated with several factors. Although the nerve roots have good activity after adhesion release and decompression via FELD, they remain in an inflammatory edematous state due to surgical trauma and self-repair. Moreover, insufficient blood supply in the local vasculature can further aggravate inflammatory edema [18]. In our opinion, the removal of herniated disc tissues will cause the cavity to be filled with blood clots, and inflammatory edema can occur. Organization and absorption may take time, during which symptoms may aggravate. Furthermore, articular surface and capsule damage during FELD, resulting in facet joint degeneration and instability, may lead to the aggravation of postoperative symptoms.
In the current study, the incidence rate of transient rebound pain is 5.8%. This is not lower than the incidence of various postoperative complications after FELD. Interestingly, rebound pain mostly occurs in the early postoperative period, and the pain is not too severe. We did not identify the precipitating factors of rebound pain based on the survey indexes of age, sex, BMI, diagnosis, surgical level, Modic change, disc degeneration, operative time, and preoperative VAS score and ODI in the logistic regression analysis. Regarding clinical efficacy, our study compared pain intensity and functional assessment results at least during the 1-year follow-up between the rebound and non-rebound pain groups. There were no significant differences between the two groups. Thus, postoperative rebound pain is a short-term symptom, and it has no significant effect on the final efficacy of FELD.
According to previous studies, the prevalence of recurrence after FELD can reach 2.8–11% [11,19,20]. In our study, the recurrence rate was 4.4%, which was within an acceptable range. As for the characteristics of pain, early recurrence pain symptoms are similar to transient rebound pain, and both have a transient pain remission period [21]. The difference is that the patient feels well after FELD and then suddenly suffers the same or more severe pain and numbness as before; this is not postoperative rebound pain but may be a recurrence.
Based on the findings of this study, the characteristics of postoperative pain are summarized as follows: (1) Most patients have mild surgical incision pain after FELD, and it mostly resolves on its own within 3 days, and VAS scores are generally lower than 4. Most of them can relieve pain on their own, and appropriate analgesics can be given when necessary. (2) Postoperative rebound pain has a distinct pathological process of regaining pain after relief, and its pain level is less than or equal to the preoperative pain (a high proportion of patients had VAS scores of <6). Rebound pain is typically characterized by pain (mainly leg pain with or without back pain) and usually occurs within 2 weeks after surgery and lasts <3 weeks. Rebound pain does not require surgical intervention; most of it can be relieved by adequate bed rest, and if necessary, analgesics and physical therapy are used to relieve the pain. Also, rebound pain did not affect long-term surgical outcomes. (3) Recurrence often occurs within 3 months after surgery, and the pain level is greater than or equal to the preoperative pain. Most patients require surgical intervention for recurrence.
In addition, several other complications of postoperative pain, such as residual remnants, hematomas, and nerve root injuries, should also be noted [22,23]. Special caution, particularly for the management of residual remnants and nerve root damage, should be taken if there is no pain during the remission period after surgery. If a residual mass is suspected, an MRI should be performed. In the current study, patients with rebound pain underwent MRI to exclude organic causes such as residual remnants and recurrent disc herniation. In a recent study, 38 (16.9%) patients presented with residual remnants after FELD based on postoperative MRI findings. Among them, three (1.3%) were symptomatic [24]. Therefore, although symptomatic residuals can result in reoperation, the watchful and wait strategy may be a suitable option for patients with asymptomatic residual remnants. Postoperative pain can also manifest as transient postoperative pain when a postoperative hematoma compresses a nerve. Drainage is usually not placed after FELD, and this may lead to the formation of hematomas, which takes a certain period of time. Moreover, it indirectly manifests as postoperative pain during the remission period. Because blood is a fluid, compression may not be limited to the nerve root involved before surgery [25]. If a hematoma develops after surgery, postoperative pain is distributed in multiple areas and is even involved in the development of cauda equina syndrome. In cases of transient rebound pain, multiple nerve root involvement and cauda equina syndrome are not observed. In an iatrogenic nerve injury, there is no pain remission period. This type of complication can commonly be observed during surgery, and pain caused by a nerve injury can develop immediately after surgery without a transient improvement process. Further, symptoms do not significantly improve.
The current study had several limitations. That is, it was retrospective in nature, had a small sample size, and a short-term follow-up duration. Patient data that was lost during the follow-up may affect the results. In addition, there were no power calculations for our samples. Moreover, the definition of rebound pain after FELD is uncertain due to its diverse features, unclear etiology, and limited cases. Therefore, large multicenter prospective studies must be conducted in the future.
5. Conclusions
Different types of postoperative pain have their own unique characteristics and durations. Most patients gave feedback on the pain of the surgical incision, which could be relieved by themselves or by using analgesics appropriately to relieve the pain, and its duration, usually about 3 days. Approximately 5.8% of patients experienced rebound pain, and its level is less than or equal to the preoperative pain, as well as being mitigated by conservative treatment, sufficient bed rest, and analgesics. Rebound pain does not affect the final efficacy of FELD. Recurrence often occurs within three months after FELD, and the pain level is greater than or equal to the preoperative pain. In addition, most cases required surgical intervention. Careful differentiation between the various types of postoperative pain is needed to contribute to better patient relief.
Author Contributions
Writing—original draft, G.-X.L.; Investigation, L.-W.S.; Software, S.-W.J.; Project management and help with manuscript revisions, B.-S.H.; interpreted of data and supervision, G.R.; Writing—review and editing, C.-M.C. All authors have read and agreed to the published version of the manuscript.
Funding
This research was funded by the Natural Science Foundation of Fujian Province, grant number 2021J05282; funded by the “Xiamen Health System Discipline Leaders and their Backup Candidates, Senior Management Talent Training Candidates Training Program (2021)”; funded by Ningxia Jingyuan County Science and Technology Planning Bureau (2022). The funder had no role in the design of the study or collection, analysis, or interpretation of the data, or in the writing of the manuscript.
Institutional Review Board Statement
This retrospective study was approved by the institutional Ethics Committee of the Changhua Christian Hospital (IRB number: CCH No.220306).
Informed Consent Statement
Informed consent was waivered due to the retrospective and non-interventional nature of this analysis.
Data Availability Statement
The datasets are presented within the manuscript.
Acknowledgments
The author (G.X.L.) wishes to acknowledge financial support from the “Xiamen Health High-Level Talent Training Program”.
Conflicts of Interest
The authors declare no conflict of interest.
References
- Hsu, H.T.; Chang, S.J.; Yang, S.S.; Chai, C.L. Learning curve of full-endoscopic lumbar discectomy. Eur. Spine J. 2013, 22, 727–733. [Google Scholar] [CrossRef] [PubMed]
- Lin, G.X.; Park, C.W.; Suen, T.K.; Kotheeranurak, V.; Jun, S.G.; Kim, J.S. Full Endoscopic Technique for High-Grade Up-Migrated Lumbar Disk Herniation via a Translaminar Keyhole Approach: Preliminary Series and Technical Note. J. Neurol. Surg. A Cent. Eur. Neurosurg. 2020, 81, 379–386. [Google Scholar] [CrossRef] [PubMed]
- Wang, Z.; Jian, F.; Wu, H.; Wang, X.; Wang, K.; Duan, W.; Liu, Z.; Chen, Z. Treatment of Upper Lumbar Disc Herniation with a Transforaminal Endoscopic Technique. Front. Surg. 2022, 9, 893122. [Google Scholar] [CrossRef] [PubMed]
- Lin, G.X.; Sun, L.W.; Jhang, S.W.; Ou, S.W.; Chang, K.S.; Tsai, R.Y.; Hu, B.S.; Rui, G.; Chen, C.M. A Pilot Study of Radiculopathy Following Osteoporotic Vertebral Fracture in Elderly Patients: An Algorithmic Approach to Surgical Management. Geriatr. Orthop. Surg. Rehabil. 2021, 12, 21514593211044912. [Google Scholar] [CrossRef] [PubMed]
- Sivakanthan, S.; Hasan, S.; Hofstetter, C. Full-Endoscopic Lumbar Discectomy. Neurosurg. Clin. N. Am. 2020, 31, 1–7. [Google Scholar] [CrossRef] [PubMed]
- Ruetten, S.; Komp, M.; Merk, H.; Godolias, G. Full-endoscopic interlaminar and transforaminal lumbar discectomy versus conventional microsurgical technique: A prospective, randomized, controlled study. Spine 2008, 33, 931–939. [Google Scholar] [CrossRef]
- Ahn, Y.; Lee, S.G.; Son, S.; Keum, H.J. Transforaminal Endoscopic Lumbar Discectomy Versus Open Lumbar Microdiscectomy: A Comparative Cohort Study with a 5-Year Follow-Up. Pain Physician 2019, 22, 295–304. [Google Scholar] [CrossRef]
- Wang, H.; Zhou, T.; Gu, Y.; Yan, Z. Evaluation of efficacy and safety of percutaneous transforaminal endoscopic surgery (PTES) for surgical treatment of calcified lumbar disc herniation: A retrospective cohort study of 101 patients. BMC Musculoskelet. Disord. 2021, 22, 65. [Google Scholar] [CrossRef]
- Rushton, A.; Heneghan, N.R.; Heymans, M.W.; Staal, J.B.; Goodwin, P. Clinical course of pain and disability following primary lumbar discectomy: Systematic review and meta-analysis. Eur. Spine J. 2020, 29, 1660–1670. [Google Scholar] [CrossRef]
- Liang, J.Q.; Chen, C.; Zhao, H. Revision Surgery after Percutaneous Endoscopic Transforaminal Discectomy Compared with Primary Open Surgery for Symptomatic Lumbar Degenerative Disease. Orthop. Surg. 2019, 11, 620–627. [Google Scholar] [CrossRef] [PubMed]
- Zhou, C.; Zhang, G.; Panchal, R.R.; Ren, X.; Xiang, H.; Xuexiao, M.; Chen, X.; Tongtong, G.; Hong, W.; Dixson, A.D. Unique Complications of Percutaneous Endoscopic Lumbar Discectomy and Percutaneous Endoscopic Interlaminar Discectomy. Pain Physician 2018, 21, E105–E112. [Google Scholar] [PubMed]
- Mysliwiec, L.W.; Cholewicki, J.; Winkelpleck, M.D.; Eis, G.P. MSU classification for herniated lumbar discs on MRI: Toward developing objective criteria for surgical selection. Eur. Spine J. 2010, 19, 1087–1093. [Google Scholar] [CrossRef] [PubMed]
- Pfirrmann, C.W.; Metzdorf, A.; Zanetti, M.; Hodler, J.; Boos, N. Magnetic resonance classification of lumbar intervertebral disc degeneration. Spine 2001, 26, 1873–1878. [Google Scholar] [CrossRef]
- Pan, M.; Li, Q.; Li, S.; Mao, H.; Meng, B.; Zhou, F.; Yang, H. Percutaneous Endoscopic Lumbar Discectomy: Indications and Complications. Pain Physician 2020, 23, 49–56. [Google Scholar]
- Chen, X.; Chamoli, U.; Vargas Castillo, J.; Ramakrishna, V.A.S.; Diwan, A.D. Complication rates of different discectomy techniques for symptomatic lumbar disc herniation: A systematic review and meta-analysis. Eur. Spine J. 2020, 29, 1752–1770. [Google Scholar] [CrossRef]
- Li, T.; Zhu, B.; Liu, X. Revision Strategy of Symptomatic Lumbar Adjacent Segment Degeneration: Full Endoscopic Decompression versus Extended Posterior Interbody Fusion. World Neurosurg. 2020, 142, e215–e222. [Google Scholar] [CrossRef]
- Goker, B.; Aydin, S. Endoscopic Surgery for Recurrent Disc Herniation After Microscopic or Endoscopic Lumbar Discectomy. Turk. Neurosurg. 2020, 30, 112–118. [Google Scholar] [CrossRef]
- Otoshi, K.; Kikuchi, S.; Konno, S.; Sekiguchi, M. The reactions of glial cells and endoneurial macrophages in the dorsal root ganglion and their contribution to pain-related behavior after application of nucleus pulposus onto the nerve root in rats. Spine 2010, 35, 264–271. [Google Scholar] [CrossRef]
- Yin, S.; Du, H.; Yang, W.; Duan, C.; Feng, C.; Tao, H. Prevalence of Recurrent Herniation Following Percutaneous Endoscopic Lumbar Discectomy: A Meta-Analysis. Pain Physician 2018, 21, 337–350. [Google Scholar] [PubMed]
- Park, C.H.; Park, E.S.; Lee, S.H.; Lee, K.K.; Kwon, Y.K.; Kang, M.S.; Lee, S.Y.; Shin, Y.H. Risk Factors for Early Recurrence after Transforaminal Endoscopic Lumbar Disc Decompression. Pain Physician 2019, 22, E133–E138. [Google Scholar] [CrossRef]
- Kim, H.S.; You, J.D.; Ju, C.I. Predictive Scoring and Risk Factors of Early Recurrence after Percutaneous Endoscopic Lumbar Discectomy. Biomed. Res. Int. 2019, 2019, 6492675. [Google Scholar] [CrossRef] [PubMed]
- Phan, K.; Xu, J.; Schultz, K.; Alvi, M.A.; Lu, V.M.; Kerezoudis, P.; Maloney, P.R.; Murphy, M.E.; Mobbs, R.J.; Bydon, M. Full-endoscopic versus micro-endoscopic and open discectomy: A systematic review and meta-analysis of outcomes and complications. Clin. Neurol. Neurosurg. 2017, 154, 1–12. [Google Scholar] [CrossRef] [PubMed]
- Choi, K.C.; Lee, J.H.; Kim, J.S.; Sabal, L.A.; Lee, S.; Kim, H.; Lee, S.H. Unsuccessful percutaneous endoscopic lumbar discectomy: A single-center experience of 10,228 cases. Neurosurgery 2015, 76, 372–380. [Google Scholar] [CrossRef] [PubMed]
- Baek, J.; Yang, S.H.; Kim, C.H.; Chung, C.K.; Choi, Y.; Heo, J.H.; Park, S.B.; Hwang, S.H.; Jung, J.M.; Kim, K.T. Postoperative Longitudinal Outcomes in Patients with Residual Disc Fragments after Percutaneous Endoscopic Lumbar Discectomy. Pain Physician 2018, 21, E457–E466. [Google Scholar] [PubMed]
- Kim, J.E.; Choi, D.J.; Kim, M.C.; Park, E.J. Risk Factors of Postoperative Spinal Epidural Hematoma After Biportal Endoscopic Spinal Surgery. World Neurosurg. 2019, 129, e324–e329. [Google Scholar] [CrossRef]
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2022 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).