Abstract
Background and Objectives: The COVID-19 pandemic led to restrictive measures, which aimed to limit the spread of the SARS-CoV-2 virus. These restrictions impacted all areas of life, including the activity of dental offices. For patients with orthodontic appliances, closing the dental offices was a major issue, as most orthodontic treatments last for more than a year and require regular checkups. The aim of this research was to assess the impact that the restrictive measures that were imposed during the COVID-19 pandemic, and, especially, wearing a face mask had on a sample of Romanian teenagers undergoing fixed orthodontic treatment. Material and Methods: The study group consisted of 277 orthodontic patients, with ages between 12 and 17.9 years, from North-Western Romania. They completed a 9-item questionnaire. The control group consisted of 231 participants, with ages between 12 and 17.9 years. They completed an 8-item questionnaire. Results: Most patients from the study group were not worried that wearing a protective face mask would hide their braces (never—49.5%; rarely—26.7%), and their desire to undergo an orthodontic treatment was not affected by the compulsoriness of face mask wearing (never—51.6%; rarely—26%). In contrast to that, in the control group, more than 50% of the participants were worried to some degree that wearing a protective face mask would hide their smile (occasionally—29.9%; frequently—18.2%; very frequently—2.2%). The majority of the participants from the study group did not consider interrupting the orthodontic treatment due to the COVID-19 pandemic (62.5%), and the majority of the participants from the control group did not consider not going to the dentist due to the COVID-19 pandemic (70.6%). Most of the participants from the study group were not happy that they had to wear a face mask, which covered their orthodontic appliances, during the orthodontic treatment (68.6%). The attitude was similar to that of the participants from the control group, who were not happy that they had to wear a face mask, that covered their smile (51.1%). In the study group, most patients did not want face mask wearing to continue to be compulsory, given the fact that their orthodontic appliances were no longer visible (52%). In the control group, the attitude was similar, with 48.1% of the participants not wanting face mask compulsoriness to be maintained. Conclusions: In conclusion, although, most patients would not like to continue wearing a face mask as a mandatory regulation, they were not concerned or negatively affected by wearing a protective face mask, even though face masks hid their braces.
1. Introduction
The identification of a new type of coronavirus at the end of 2019, outlined the scenario that announced the beginning of a major public health crisis worldwide [1]. The disease, a form of severe acute respiratory syndrome, caused by SARS-CoV-2 and called COVID-19, has been described by the World Health Organization as being a viral pneumonia [2]. The symptoms are numerous, and include dry cough, fever, shortness of breath, sore throat, headache, myalgia, fatigue, diarrhea [3], and radiological signs of lung damage [4].
The transmission rate of COVID-19 is high, as it spreads easily from person to person [5]. Coughing, sneezing, or talking can generate aerosols [6], which through close contact with infected people are safe sources of contamination [5]. The virus can enter the body by air and attaches to the mucous membranes of the oral cavity, nose, or eyes [6,7].
As a result of the increase in the number of cases with COVID-19 disease, a pandemic was declared, and worldwide, in an attempt to limit the spread of the virus, quarantine was instated in all countries [8]. Among other restrictions, a safe distance of 1–2 m had to be maintained between people [9]. For dental professionals, this distance was impossible to maintain, as dental work requires close contact with the patient’s oropharyngeal and nasal region, increasing the risk of contamination [9,10]. The activity of dental offices was suspended, which affected all patients [11]. Emergency dental treatments consisting of pain, swelling, bleeding, infections, and trauma were permitted in certain authorized dental offices [12,13].
For patients with orthodontic appliances, closing the dental offices was a major issue, as most orthodontic treatments last for more than a year [12], and require regular checkups [14]. During this period of disruption, treatments could no longer be supervised and were negatively affected, with patients reaching high levels of anxiety caused by the new situation [12].
Face mask wearing became mandatory in many countries as it is considered an important preventive measure during the COVID-19 pandemic [15]. Face masks are considered beneficial since wearing a mask in areas where the advised social distance cannot be properly maintained lowers the spread of virus-loaded droplets [16]. As they cover the nose and mouth of the patients, and the area around them [17], protective face masks also cover the fixed orthodontic appliances bonded on the buccal surface of the teeth, which are visible in smile and speech. For some patients this aspect could potentially cause frustration, since the desire for orthodontic treatment among teenagers has been proven to be high [18], and patients are usually satisfied with their facial aspect during the orthodontic treatment [19]. The question was raised whether the necessity to cover the orthodontic appliance with a face mask could cause teenagers to be less interested in undergoing a necessary orthodontic treatment, especially because often braces are perceived as being an elective luxury and a symbol of status, wealth, and style [20], or whether it could nurture a disobedience towards the mandatory wearing of face masks.
The aim of this research was to assess the attitude that a sample of Romanian teenagers undergoing orthodontic treatment with fixed appliances, during the COVID-19 pandemic, had regarding wearing protective face masks, considering the fact that they covered the orthodontic appliances. Their attitude towards the suspension of dental activity, as orthodontic patients, was investigated as well.
2. Materials and Methods
2.1. Ethical Considerations
The study was conducted in accordance with the 1964 Declaration of Helsinki and its later amendments and was approved by the Research Ethics Committee of the University of Oradea (No. 23/25.02.2021). Before filling in the questionnaires, all parents, caregivers, and participants gave their consent for taking part in this study.
2.2. Sample Size Calculation
Sample size estimation was made using GPower 3.1.9.7 software. By the design of the study, it was considered that the measured items (in Likert scale format) would be mostly compared between genders, using Mann–Whitney U tests (for items with 5 answers) or contingency tables (for items with 3 answers), and the ideal allocation ratio of the genders should be 1:1. Therefore, it was estimated using a medium effect size of d = 0.5, with a minimum power of 0.8 and an α = 0.05, that the minimum sample size should be of 74 patients in each group for Mann–Whitney U tests (a total of 168). For contingency tables, considering a medium effect size of w = 0.3 with Df = 2, a minimum power of 0.8 and an α = 0.05, the minimum total sample size should be equal to 108. Using these values, an estimation was made that a minimum of 74 patients in each gender (with a total of 168 patients) should exist in the study for a minimum power of 0.8 for most tests.
2.3. Participants and Data Collection
The study design was a cross-sectional survey. It was carried out in the period between November 2020 and February 2022. A pilot study was not conducted prior to this research. During the period in which this study was conducted, restrictive measures regarding the mandatory wearing of face masks and social distancing were active.
For the study group, the authors designed a questionnaire consisting of 9 items. For the control group, only 8 items were used, since Item 9 referred strictly to orthodontic patients. The questionnaires were printed on paper and applied in two private orthodontic practices from the city of Oradea, North-Western Romania, which offer treatments to patients who come from families with various incomes (from low to high). They were distributed to adolescents, aged between 12 and 17.9 years. In the study group, the respondents were orthodontic patients, undergoing an orthodontic treatment with fixed appliances. In the control group, the respondents were non-orthodontic patients, who came to the office for a clinical examination. Before filling in the questionnaire, all patients and their parents (or caregivers) were informed that they were being applied for research purposes, and that by filling in the questionnaires, they confirmed their willingness to participate anonymously in this study. The names of the participants were not mentioned on the survey form, and the authors did not know how patients answered. Patients had the possibility to withdraw from the research with no consequences, and no financial incentives were promised to the respondents. No time limit was imposed. The language used for the questionnaires was Romanian.
A Likert-type scale was used for Items 1, 2, 3, 4, and 8. The options included were “never”, “rarely”, “occasionally”, “frequently”, and “very frequently”. For Items 5, 6, 7, and 9, participants had to choose from three options, these being “no”, “yes”, and “maybe”. Items are translated and detailed in Table 1.

Table 1.
Items.
For the study group, the inclusion criteria were that the participants had to be patients wearing a metallic or ceramic fixed orthodontic appliance (bonded on the buccal surface of teeth, and visible in smile and speech), with ages between 12 and 17.9 years, and to live in Romania. The control group consisted of participants who were not wearing and did not wear orthodontic appliances (fixed or removable), with ages between 12 and 17.9 years, and were living in Romania. Patients who were in the contention phase of the orthodontic treatment, as well as questionnaires that were incomplete or incorrectly completed were excluded from this study. Incorrectly completed questionnaires were those where the patients offered more than one answer for the same item.
2.4. Statistical Analysis
Statistical analysis was performed by using IBM SPSS software, version 25 (IBM, Chicago, IL, USA). Quantitative variables were tested for distribution using the Shapiro–Wilk test and were expressed as mean values with standard deviations or medians with interpercentile intervals. The independent quantitative variables with a non-parametric distribution were tested with the Mann–Whitney U or Kruskal–Wallis H tests, and all correlations between them were verified with Spearman’s rho correlation coefficient. Qualitative variables were expressed as absolute numbers or percentages and were tested with Fisher’s exact test.
3. Results
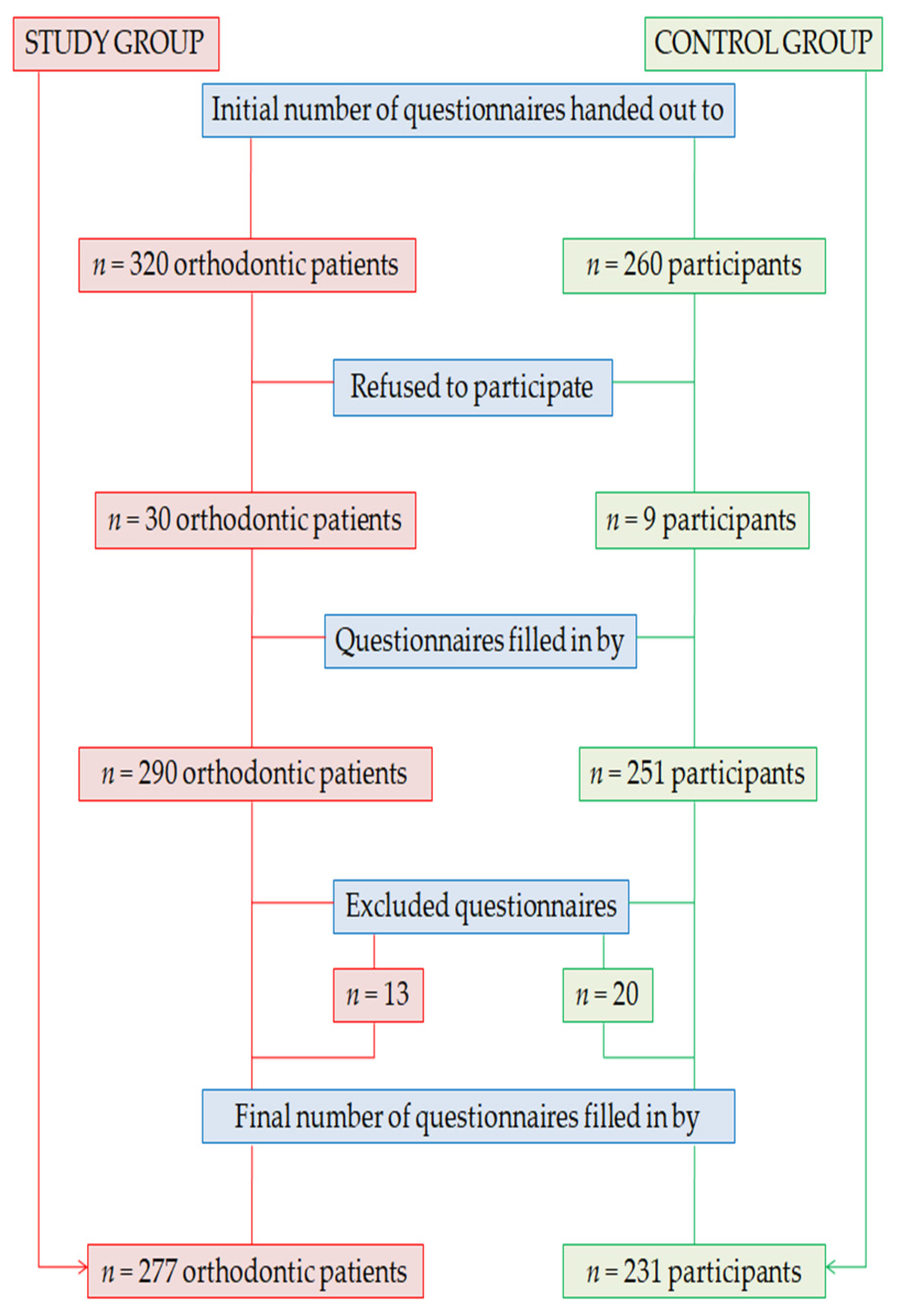
In the study group, the questionnaires were handed out to 320 orthodontic patients, but only 290 agreed to take part in this research and filled in the survey forms. After applying the exclusion criteria, 277 valid questionnaires remained in the study. In the control group, the questionnaires were handed out to 260 participants, but only 251 agreed to take part in this research and filled in the survey forms. After applying the exclusion criteria, 231 valid questionnaires remained in the study (Figure 1).
Figure 1.
Study flowchart.
3.1. Socio-Demographic Data
The study group consisted of 173 (62.5%) girls and 104 (37.5%) boys. Regarding the living environment of the participants, 93 (33.6%) came from a rural environment, while 184 (66.5%) came from an urban environment. The mean age of the respondents was 14.91 ± 1.49 years, with a median of 15 years, and a range between 12 and 17.9 years.
The control group consisted of 134 (58%) girls and 97 (42%) boys. Regarding the living environment of the participants, 92 (39.8%) came from a rural environment, while 139 (60.2%) came from an urban environment. The mean age of the respondents was 14.77 ± 1.64 years, with a median of 15 years and a range between 12 and 17.9 years.
Data in Table 2 shows the comparison of participants’ ages in relation to the living environment. According to the Shapiro–Wilk test, in the study sample, age distribution was non-parametric in both groups, and the Mann–Whitney U test showed that age differences were significant. Participants living in an urban environment had a higher age than those living in a rural environment. In the control sample the age difference was not significant between the groups.

Table 2.
Comparison of participants’ ages in relation to the living environment.
The Mann–Whitney U test showed that the age of the participants was not statistically significant between the study group and the control group (p = 0.346). The living environment of the participants was, also, not statistically significant between the study group and the control group (p = 0.165).
3.2. Attitude towards Protective Face Mask Wearing and Treatment Interruption
Data in Table 3 shows the distribution of the patients according to the answers given for all 9 items (study group) and 8 items (control group). In the study group, most patients were not worried that wearing a protective face mask would hide their braces (Item 1), and their desire to undergo an orthodontic treatment was not affected by the compulsoriness of face mask wearing (Item 2). The majority of the participants did not consider interrupting the orthodontic treatment due to the COVID-19 pandemic (Item 5), but most of them were not happy that they had to wear a face mask, which covered their orthodontic appliances, during the orthodontic treatment (Item 6), and did not want face mask wearing to continue to be compulsory, given the fact that their orthodontic appliances were no longer visible (Item 7). In the control group, more than half of the participants were worried to some degree (occasionally, frequently, very frequently) that wearing a protective face mask would hide their smile (Item 1) and were affected by the compulsoriness of face mask wearing (Item 2). The majority of the participants did not consider not going to the dentist due to the COVID-19 pandemic (Item 5).

Table 3.
Distribution of the patients according to the answers provided.
3.3. Correlational Results
In the study group, statistically significant correlations were found between respondents’ age and answers provided for Items 1, 3 and 8. As such, patients with higher ages were less concerned about the fact that wearing a protective face mask would hide their braces and were less affected by the suspension of dental offices’ activity, as patients undergoing an orthodontic treatment with fixed appliances. However, younger patients were less stressed about wearing a protective face mask that hid the orthodontic appliances (Table 4). In the control group, there were no statistically significant correlations identified between respondents’ age and answers provided for Items 1, 3, and 8.

Table 4.
Correlations between age and Items 1, 3, and 8.
In the study group, patients’ gender influenced the answers received for Items 6 and 7. As such, boys were unhappier with wearing a protective face mask during the orthodontic treatment, while indecisive patients were more frequently girls. Boys were, also, less eager to continue wearing a face mask as a mandatory regulation, considering the fact that face masks covered the braces. The answers received for Items 5, 7, and 9 were significantly influenced by participants’ living environment. Patients living in an urban environment were less prone to considering interrupting the orthodontic treatment as a result of the COVID-19 pandemic, and were more eager to maintain the compulsoriness of face mask wearing, even though face masks covered the orthodontic appliances. Patients living in a rural environment were more frequently indecisive about interrupting the orthodontic treatment during the COVID-19 pandemic, were less eager to maintain the compulsoriness of face mask wearing during the orthodontic treatment, and were more frequently indecisive about interrupting the orthodontic treatment while wearing a face mask (Table 5). In the control group, only the answers received for Item 7 were influenced by patients’ gender. As such, girls were unhappier than boys about the fact that they have to wear a protective face mask that would cover their smile. The answers received for Item 5 were significantly influenced by participants’ living environment. As such, patients living in a rural environment were more frequently indecisive than patients living in an urban environment about not going to the dentist due to the COVID-19 pandemic (Table 5).

Table 5.
Patients’ distribution according to gender, living environment, and answers provided for different items.
Other significant correlations were found between answers provided for some items. As such, in the study group, participants who were more concerned that wearing a face mask would hide their orthodontic appliance (Item 1) considered that the compulsoriness of face mask wearing affected their desire to undergo an orthodontic treatment, because face masks covered their braces (Item 2) (p < 0.001, R = 0.300), and were more affected by the suspension of dental offices’ activity, as patients undergoing an orthodontic treatment with fixed orthodontic appliances (Item 3) (p = 0.001, R = 0.194).
Patients who did not want protective face masks to continue being mandatory, given the fact that they covered the braces (Item 7) were more frequently indecisive about their willingness to continue the orthodontic treatment while wearing a protective face mask (Item 9) (Table 6).

Table 6.
Patients’ distribution according to answers provided for Items 7 and 9.
3.4. Comparative Results
Comparisons were made between participants considering their age, gender, and living environment. Although significant differences were found for some items in relation to age and gender, no significant differences were found in relation to the living environment. Regarding age, in the study group, significant differences were found for Item 9. A comparison of age in relation to patients’ desire to continue the orthodontic treatment while wearing a face mask was made. Age distribution was non-parametric in most groups according to the Shapiro–Wilk test (p < 0.05). The differences between groups were statistically significant according to the Kruskal–Wallis H test (p = 0.002), and post-hoc tests showed that indecisive patients had a lower age than patients who said they do not want to continue the orthodontic treatment while wearing a face mask, given the fact that the orthodontic appliances were no longer visible (p = 0.044) or than patients who said they want to continue the orthodontic treatment while wearing a face mask, despite the fact that the orthodontic appliances were no longer visible (p = 0.001).
Regarding patients’ gender, in the study group significant differences were identified for Items 2 and 4. The results obtained showed that boys’ desires to undergo orthodontic treatment were less affected by the compulsoriness of a face mask that covers the braces, in comparison with girls, and they were less worried about the possibility of the orthodontic treatment suspension than girls (Table 7). In the control group, significant differences were identified for Item 4. The results were similar to the study group. Girls were more worried that they would not be able to go to the dentist due to the COVID-19 pandemic (Table 7).

Table 7.
Comparison of answers provided for Items 2 and 4 in relation to gender.
Other significant differences were found between answers provided for some items. In the study group, significant differences were identified between Items 1 and 9, Items 2 and 5, Items 3 and 5, and Items 3 and 7. In the control group, significant differences were identified between Items 3 and 5 and Items 3 and 7. They are detailed in Table 8, which shows the results of the Kruskal–Wallis H test and Shapiro–Wilk test.

Table 8.
Comparisons between various items.
Table 9 and Table 10 show the comparisons of answers provided for Item 1 to Item 8, according to the analyzed groups (study group and control group). Statistically significant differences were identified for most items. As such, participants undergoing an orthodontic treatment with fixed appliances (study group) were less affected by the compulsoriness of face mask wearing, in comparison to the participants from the control group (Item 2) and were worried that they would not be able to continue the orthodontic treatment (Item 4). In comparison with the study group, participants from the control group were more worried about the fact that they had to wear a protective face mask (Item 1) and were more stressed that they had to wear a protective face mask (Item 8).

Table 9.
Comparison of answers provided for Items 1, 2, 3, 4, and 8 according to the analyzed groups.

Table 10.
Comparison of answers provided for Items 5, 6, and 7 according to the analyzed groups.
4. Discussion
The COVID-19 pandemic has had a strong impact on the global healthcare system, affecting both the economy of health systems [21] and the way patients have accessed healthcare services. During the pandemic, the use of healthcare fell by about a third among patients [22]. Dental practices have also been affected by the restrictions imposed during the pandemic. Restrictive measures maintained for a longer period of time could lead to financial distress, the most affected being dental practices with high operational costs [23]. Withholding dental care led to the progression of undiagnosed and untreated oral diseases [24], and orthodontic treatments were suspended during the lockdown period, with orthodontists being unable to sustain ongoing treatments. In Romania, a state of lockdown was established for a period of two months, between March 16 and May 16, 2020 [25].
It is important to determine patients’ attitudes towards restrictive measures and, especially, towards wearing a protective mask, during the orthodontic treatment, keeping in mind that face masks cover the orthodontic appliances. For this purpose, we designed a short questionnaire, comprising only 9 items (8 items for the control group), to which patients can easily answer in the waiting room, before completing their regular checkup. The use of questionnaires is an accessible method for collecting data from patients, in order to conduct a statistical study [26]. Although most research in the field of dentistry investigating different attitudes during the COVID-19 pandemic is based on questionnaires applied on online platforms [27,28], websites [29], e-mail addresses of dentists [30] or patients, or both online and on paper [31], in the present study the paper printed version of the questionnaire was used for a better selection of patients and for an easier application of the inclusion and exclusion criteria. Additionally, by completing the questionnaires in the dental office after a longer period of wearing a face mask, patients were given clarifications about any questions they could not comprehend. However, completing the questionnaires in the dental office could make participants feel obligated to respond in a manner that would positively represent an orthodontic treatment. In order to reduce this possibility, patients were encouraged to answer freely and honestly, and were assured that the questionnaires will remain anonymous.
Although there are other studies that have examined the impact of the pandemic on orthodontic patients, they have attempted to determine the challenges that patients had and the solutions proposed by them [1]. Our study focused mainly on finding out information about the patients’ attitudes towards wearing a protective mask during the orthodontic treatment. We selected adolescent patients because, generally, they are the main population group receiving orthodontic treatment [32]. The protective mask covers the middle and lower third of the face, thus covering the teeth in smile and speech. In this way, the orthodontic appliance is no longer visible. In our study, although the desire of most patients to undergo the orthodontic treatment was not negatively affected by wearing a face mask, even though face masks covered their braces, most patients were not happy to wear a face mask while wearing the orthodontic appliance. In our view, a potential reason for the unhappiness caused by face mask wearing during the orthodontic treatment could be that adolescent patients, for the most part, want to have the orthodontic appliance visible in smile and speech, since they can be viewed as a fashion statement [20]. A type of fixed braces called “fashion braces” has been developed, with the unique purpose of imitating an orthodontic treatment, but having no therapeutic effect [20]. In other studies, however, there is a preference of young patients for less visible appliances, such as clear aligners [33], while adult patients prefer aesthetic orthodontic appliances [34]. It would be beneficial to find out if face mask wearing could increase patients’ preferences towards less esthetic orthodontic appliances, given the fact that they would not be visible while wearing the protective face mask. Nonetheless, teenagers require further support and stimulation for continuing to respect the COVID-19 mandatory regulations. They should be involved in educational programs that help other people understand the benefits of face mask wearing during the COVID-19 pandemic.
Most teenagers in this study did not consider that it would be necessary to interrupt the treatment due to the COVID-19 pandemic. The lack of concern about the fact that wearing a protective face mask would cover the orthodontic appliance increased with the age of the respondents, so that patients with higher ages were less concerned about the fact that wearing a mask would cover the orthodontic appliances (p = 0.001, R = −0.204). This suggests that younger patients were more eager to have their orthodontic appliance visible. Generally, people are not concerned about wearing a protective face mask, and although there is an impression that the anti-mask sentiment is widespread [35], most studies show that people are willing to follow the authorities’ recommendations and wear a face mask [35].
Regarding the living environment of the respondents and their attitude towards wearing a protective mask, it can be emphasized that patients living in an urban environment were more eager to maintain the compulsoriness of face mask wearing, even though the face mask covered the orthodontic appliances, while patients living in a rural environment were less eager to maintain the compulsoriness of face mask wearing (p = 0.005). This may be due to the fact that the rural population engages less in preventive health behaviors than the urban population [36,37], as other studies suggested.
Regarding the sample size estimation, it is important to highlight the fact that when the sample size was estimated, an ideal gender allocation ratio of 1:1 was taken into consideration. The main goal was to determine the minimum number of questionnaires that had to be completed for each gender. However, more questionnaires than initially planned were distributed, and we did not want to lose the information obtained through these forms. We do not consider that the final distribution of patients could influence the obtained results.
The COVID-19 pandemic and the restrictions connected to it have changed the lives of patients [38]. Despite some inconveniences caused by wearing protective masks [39], wearing protective face masks should be encouraged, because they offer a high protection against the spread of the SARS-CoV-2 virus [40]. Protective face masks, along with proper ventilation, social distancing [41], and vaccination, are the safest methods to combat the COVID-19 pandemic [42].
The limitations of this study are related, first of all, to the number of items. It would be useful to extend the questionnaires and add more items, investigating the attitudes toward orthodontic appliances, oral health, self-esteem, and the main purpose for wearing orthodontic appliances. Extending the questionnaire to the adult population would be beneficial, since it would offer an even more comprehensive view of face mask wearing during the orthodontic treatment. The application of online questionnaires could allow a multicenter, national approach of this topic. In this way, data could be collected from several orthodontic practices from across Romania. However, given the restrictive circumstances in which this survey was conducted, during the COVID-19 pandemic, we consider it to be a solid starting point for future research. Even though mask policies are temporary, the COVID-19 pandemic is still actively causing infections [43], meaning that face masks may remain useful for an indefinite amount of time. Moreover, there are still areas at risk of impactful spillover, which could be the starting point of future pandemics [44]. Under these conditions, face masks could become the new normal.
5. Conclusions
Adolescents wearing fixed orthodontic appliances had a generally positive attitude towards protective face masks, despite the fact that they covered their orthodontic appliances, most of them not being bothered by the fact that face mask wearing was mandatory and not being concerned that they must wear a protective mask that would cover their orthodontic appliances. Usually, boys were less affected by the compulsoriness of face mask wearing, during the orthodontic treatment, in comparison with girls, and they were less worried about the possibility of orthodontic treatment suspension than girls. Wearing a face mask remains one of the key measures in the prevention of the SARS-CoV-2 virus spread and should be encouraged. Non-orthodontic patients were more worried about the fact that they had to wear a protective face mask and more stressed about this issue.
Author Contributions
Conceptualization, J.O.C. and A.E.M.; methodology, J.O.C., L.L.V. and A.E.M.; software, R.D.; validation, J.O.C., G.C. and R.D.; formal analysis, L.L.V. and R.D.; investigation, J.O.C. and G.C.; resources, L.L.V. and R.D.; data curation, A.E.M.; writing—original draft preparation, J.O.C.; writing—review and editing, L.L.V. and A.E.M.; visualization, R.D. and G.C.; supervision, M.B.; project administration, G.C. and R.D.; funding acquisition, J.O.C. and G.C. All authors have read and agreed to the published version of the manuscript.
Funding
This research was funded through the Project 123008, entitled “SmartDoct—High quality programs for doctoral students and postdoctoral researchers from the University of Oradea for growth of the relevance of research and innovation in the context of regional economy”, project financed through the Human Capital Operation Program 2014–2020.
Institutional Review Board Statement
The study was conducted according to the guidelines of the Declaration of Helsinki and approved by the Ethics Committee of the University of Oradea (No. 23/25.02.2021).
Informed Consent Statement
Informed consent was obtained from all subjects involved in the study.
Data Availability Statement
The data presented in this study are available on request from the corresponding authors. The data are not publicly available due to privacy reasons.
Conflicts of Interest
The authors declare no conflict of interest.
References
- Bustati, N.; Rajeh, N. The impact of COVID-19 pandemic on patients receiving orthodontic treatment: An online questionnaire cross-sectional study. J. World Fed. Orthod. 2020, 9, 159–163. [Google Scholar] [CrossRef] [PubMed]
- Bahramian, H.; Gharib, B.; Baghalian, A. COVID-19 Considerations in Pediatric Dentistry. JDR Clin. Trans. Res. 2020, 5, 307–311. [Google Scholar] [CrossRef] [PubMed]
- Yüce, M.; Filiztekin, E.; Özkaya, K.G. COVID-19 diagnosis—A review of current methods. Biosens. Bioelectron. 2021, 172, 112752. [Google Scholar] [CrossRef] [PubMed]
- Lei, S.; Jiang, F.; Su, W.; Chen, C.; Chen, J.; Mei, W.; Zhan, L.Y.; Jia, Y.; Zhang, L.; Liu, D.; et al. Clinical characteristics and outcomes of patients undergoing surgeries during the incubation period of COVID-19 infection. E. Clin. Med. 2020, 21, 100331. [Google Scholar] [CrossRef]
- Huang, C.; Wang, Y.; Li, X.; Ren, L.; Zhao, J.; Hu, Y.; Zhang, L.; Fan, G.; Xu, J.; Gu, X.; et al. Clinical features of patients infected with 2019 novel coronavirus in Wuhan, China. Lancet 2020, 395, 497–506. [Google Scholar] [CrossRef] [Green Version]
- Malekshoar, M.; Javanshir, B. Challenges, limitations, and solutions for orthodontists during the coronavirus pandemic: A review. Am. J. Orthod. Dentofac. Orthop. 2021, 159, e59–e71. [Google Scholar] [CrossRef]
- Belser, J.A.; Rota, P.A.; Tumpey, T.M. Ocular tropism of respiratory viruses. Microbiol. Mol. Biol. Rev. 2013, 77, 144–156. [Google Scholar] [CrossRef] [Green Version]
- Kharroubi, S.; Saleh, F. Are Lockdown Measures Effective Against COVID-19? Front. Public Health 2020, 8, 549692. [Google Scholar] [CrossRef]
- Turkistani, K.A. Precautions and recommendations for orthodontic settings during the COVID-19 outbreak: A review. Am. J. Orthod. Dentofac. Orthop. 2020, 158, 175–181. [Google Scholar] [CrossRef]
- Derruau, S.; Bouchet, J.; Nassif, A.; Baudet, A.; Yasukawa, K.; Lorimier, S.; Prêcheur, I.; Bloch-Zupan, A.; Pellat, B.; Chardin, H.; et al. On Behalf Of Task Force Covid-Collège National des EnseignantS En Biologie Orale Cnesbo-France. COVID-19 and Dentistry in 72 Questions: An Overview of the Literature. J. Clin. Med. 2021, 10, 779. [Google Scholar] [CrossRef]
- Peloso, R.M.; Pini, N.I.P.; Sundfeld Neto, D.; Mori, A.A.; Oliveira, R.C.G.; Valarelli, F.P.; Freitas, K.M.S. How does the quarantine resulting from COVID-19 impact dental appointments and patient anxiety levels? Braz. Oral Res. 2020, 34, e84. [Google Scholar] [CrossRef] [PubMed]
- Alharbi, A.; Alharbi, S.; Alqaidi, S. Guidelines for dental care provision during the COVID-19 pandemic. Saudi Dent. J. 2020, 32, 181–186. [Google Scholar] [CrossRef] [PubMed]
- Suri, S.; Vandersluis, Y.R.; Kochhar, A.S.; Bhasin, R.; Abdallah, M.N. Clinical orthodontic management during the COVID-19 pandemic. Angle Orthod. 2020, 90, 473–484. [Google Scholar] [CrossRef] [PubMed]
- Umeh, O.D.; Utomi, I.L.; Isiekwe, I.G.; Aladenika, E.T. Impact of the coronavirus disease 2019 pandemic on orthodontic patients and their attitude to orthodontic treatment. Am. J. Orthod. Dentofac. Orthop. 2021, 159, e399–e409. [Google Scholar] [CrossRef] [PubMed]
- Zhao, X.; Knobel, P. Face mask wearing during the COVID-19 pandemic: Comparing perceptions in China and three European countries. Transl. Behav. Med. 2021, 11, 1199–1204. [Google Scholar] [CrossRef]
- Matuschek, C.; Moll, F.; Fangerau, H.; Fischer, J.C.; Zänker, K.; van Griensven, M.; Schneider, M.; Kindgen-Milles, D.; Knoefel, W.T.; Lichtenberg, A.; et al. Face masks: Benefits and risks during the COVID-19 crisis. Eur. J. Med. Res. 2020, 25, 32. [Google Scholar] [CrossRef]
- Kisielinski, K.; Giboni, P.; Prescher, A.; Klosterhalfen, B.; Graessel, D.; Funken, S.; Kempski, O.; Hirsch, O. Is a Mask That Covers the Mouth and Nose Free from Undesirable Side Effects in Everyday Use and Free of Potential Hazards? Int. J. Environ. Res. Public Health 2021, 18, 4344. [Google Scholar] [CrossRef]
- Feldens, C.A.; Nakamura, E.K.; Tessarollo, F.R.; Closs, L.Q. Desire for orthodontic treatment and associated factors among adolescents in Southern Brazil. Angle Orthod. 2015, 85, 224–232. [Google Scholar] [CrossRef] [Green Version]
- Mihailescu, A.; Labunet, A.; Muntean, A.; Kui, A.; Campian, R.S. Psycho-social impact of orthodontic treatment in Romanian teenagers and young adults. Clujul Med. 2018, 91, 336–341. [Google Scholar] [CrossRef] [Green Version]
- Hakami, Z.; Chung, H.S.; Moafa, S.; Nasser, H.; Sowadi, H.; Saheb, S.; Bokhari, A.M.; Anderson, N.K. Impact of fashion braces on oral health related quality of life: A web-based cross-sectional study. BMC Oral Health 2020, 20, 236. [Google Scholar] [CrossRef]
- Kaye, A.D.; Okeagu, C.N.; Pham, A.D.; Silva, R.A.; Hurley, J.J.; Arron, B.L.; Sarfraz, N.; Lee, H.N.; Ghali, G.E.; Gamble, J.W.; et al. Economic impact of COVID-19 pandemic on healthcare facilities and systems: International perspectives. Best Pract. Res. Clin. Anaesthesiol. 2021, 35, 293–306. [Google Scholar] [CrossRef] [PubMed]
- Moynihan, R.; Sanders, S.; Michaleff, Z.A.; Scott, A.M.; Clark, J.; To, E.J.; Jones, M.; Kitchene, E.; Fox, M.; Johansson, M.; et al. Impact of COVID-19 pandemic on utilisation of healthcare services: A systematic review. BMJ Open 2021, 11, e045343. [Google Scholar] [CrossRef] [PubMed]
- Schwendicke, F.; Krois, J.; Gomez, J. Impact of SARS-CoV2 (Covid-19) on dental practices: Economic analysis. J. Dent. 2020, 99, 103387. [Google Scholar] [CrossRef] [PubMed]
- Coulthard, P.; Thomson, P.; Dave, M.; Coulthard, F.P.; Seoudi, N.; Hill, M. The COVID-19 pandemic and dentistry: The clinical, legal and economic consequences—Part 2: Consequences of withholding dental care. Br. Dent. J. 2020, 229, 801–805. [Google Scholar] [CrossRef]
- Vancea, F.; Apostol, M.Ş. Changes in mental health during the COVID-19 crisis in Romania: A repeated cross-section study based on the measurement of subjective perceptions and experiences. Sci. Prog. 2021, 104, 368504211025873. [Google Scholar] [CrossRef]
- Sekulic, D.; Ostojic, D.; Decelis, A.; Castro-Piñero, J.; Jezdimirovic, T.; Drid, P.; Ostojic, L.; Gilic, B. The Impact of Scholastic Factors on Physical Activity Levels during the COVID-19 Lockdown: A Prospective Study on Adolescents from Bosnia and Herzegovina. Children 2021, 8, 877. [Google Scholar] [CrossRef]
- Carvalho, J.C.; Declerck, D.; Jacquet, W.; Bottenberg, P. Dentist Related Factors Associated with Implementation of COVID-19 Protective Measures: A National Survey. Int. J. Environ. Res. Public Health 2021, 18, 8381. [Google Scholar] [CrossRef]
- Cotrin, P.; Peloso, R.M.; Oliveira, R.C.; de Oliveira, R.C.G.; Pini, N.I.P.; Valarelli, F.P.; Freitas, K.M.S. Impact of coronavirus pandemic in appointments and anxiety/concerns of patients regarding orthodontic treatment. Orthod. Craniofac. Res. 2020, 23, 455–461. [Google Scholar] [CrossRef]
- Xiong, X.; Wu, Y.; Fang, X.; Sun, W.; Ding, Q.; Yi, Y.; Huang, Y.; Gong, J.; Liu, J.; Wang, J. Mental distress in orthodontic patients during the coronavirus disease 2019 pandemic. Am. J. Orthod. Dentofac. Orthop. 2020, 158, 824–833.e1. [Google Scholar] [CrossRef]
- Schmidt, J.; Waldova, E.; Balkova, S.; Suchanek, J.; Smucler, R. Impact of COVID-19 on Czech Dentistry: A Nationwide Cross-Sectional Preliminary Study among Dentists in the Czech Republic. Int. J. Environ. Res. Public Health 2021, 18, 9121. [Google Scholar] [CrossRef]
- Habib, M.A.; Dayyab, F.M.; Iliyasu, G.; Habib, A.G. Knowledge, attitude and practice survey of COVID-19 pandemic in Northern Nigeria. PLoS ONE 2021, 16, e0245176. [Google Scholar] [CrossRef] [PubMed]
- Vaida, L.; Corega, C.; Roșeanu, G. Letter to Editor. J. Cogn. Behav. Psychother 2009, 9, 131–133. [Google Scholar] [CrossRef]
- Alansari, R.A. Youth Perception of Different Orthodontic Appliances. Patient Prefer. Adherence 2020, 14, 1011–1019. [Google Scholar] [CrossRef] [PubMed]
- Alansari, R.A.; Faydhi, D.A.; Ashour, B.S.; Alsaggaf, D.H.; Shuman, M.T.; Ghoneim, S.H.; Linjawi, A.I.; Marghalani, H.Y.; Dause, R.R. Adult Perceptions of Different Orthodontic Appliances. Patient Prefer. Adherence 2019, 13, 2119–2128. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Taylor, S.; Asmundson, G.J.G. Negative attitudes about facemasks during the COVID-19 pandemic: The dual importance of perceived ineffectiveness and psychological reactance. PLoS ONE 2021, 16, e0246317. [Google Scholar] [CrossRef]
- Chen, X.; Chen, H. Differences in preventive behaviors of COVID-19 between urban and rural residents: Lessons learned from a cross-sectional study in China. Int. J. Environ. Res. Public Health 2020, 17, 4437. [Google Scholar] [CrossRef]
- Zhang, B.; Li, Z.; Jiang, L. The Intentions to Wear Face Masks and the Differences in Preventive Behaviors between Urban and Rural Areas during COVID-19: An Analysis Based on the Technology Acceptance Model. Int. J. Environ. Res. Public Health 2021, 18, 9988. [Google Scholar] [CrossRef]
- Stavridou, A.; Kapsali, E.; Panagouli, E.; Thirios, A.; Polychronis, K.; Bacopoulou, F.; Psaltopoulou, T.; Tsolia, M.; Sergentanis, T.N.; Tsitsika, A. Obesity in Children and Adolescents during COVID-19 Pandemic. Children 2021, 8, 135. [Google Scholar] [CrossRef]
- Techasatian, L.; Lebsing, S.; Uppala, R.; Thaowandee, W.; Chaiyarit, J.; Supakunpinyo, C.; Panombualert, S.; Mairiang, D.; Saengnipanthkul, S.; Wichajarn, K.; et al. The Effects of the Face Mask on the Skin Underneath: A Prospective Survey During the COVID-19 Pandemic. J. Prim. Care Community Health 2020, 11, 2150132720966167. [Google Scholar] [CrossRef]
- Howard, J.; Huang, A.; Li, Z.; Tufekci, Z.; Zdimal, V.; van der Westhuizen, H.M.; von Delft, A.; Price, A.; Fridman, L.; Tang, L.H.; et al. An evidence review of face masks against COVID-19. Proc. Natl. Acad. Sci. USA 2021, 118, e2014564118. [Google Scholar] [CrossRef]
- Cheng, Y.; Ma, N.; Witt, C.; Rapp, S.; Wild, P.S.; Andreae, M.O.; Pöschl, U.; Su, H. Face masks effectively limit the probability of SARS-CoV-2 transmission. Science 2021, eabg6296. [Google Scholar] [CrossRef] [PubMed]
- Fischer, A. SARS-CoV-2 vaccines, where do we stand? C. R. Biol. 2021, 344, 43–55. [Google Scholar] [CrossRef] [PubMed]
- Ashraf, O.; Virani, A.; Cheema, T. COVID-19: An Update on the Epidemiological, Clinical, Preventive, and Therapeutic Management of 2019 Novel Coronavirus Disease. Crit. Care Nurs. Q. 2021, 44, 128–137. [Google Scholar] [CrossRef] [PubMed]
- Walsh, M.G.; Sawleshwarkar, S.; Hossain, S.; Mor, S.M. Whence the next pandemic? The intersecting global geography of the animal-human interface, poor health systems and air transit centrality reveals conduits for high-impact spillover. One Health 2020, 11, 100177. [Google Scholar] [CrossRef] [PubMed]
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2022 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).