Efficacy of Listening to Music on Pain Reduction during Colposcopy-Directed Cervical Biopsy: A Randomized, Controlled Trial
Abstract
:1. Introduction
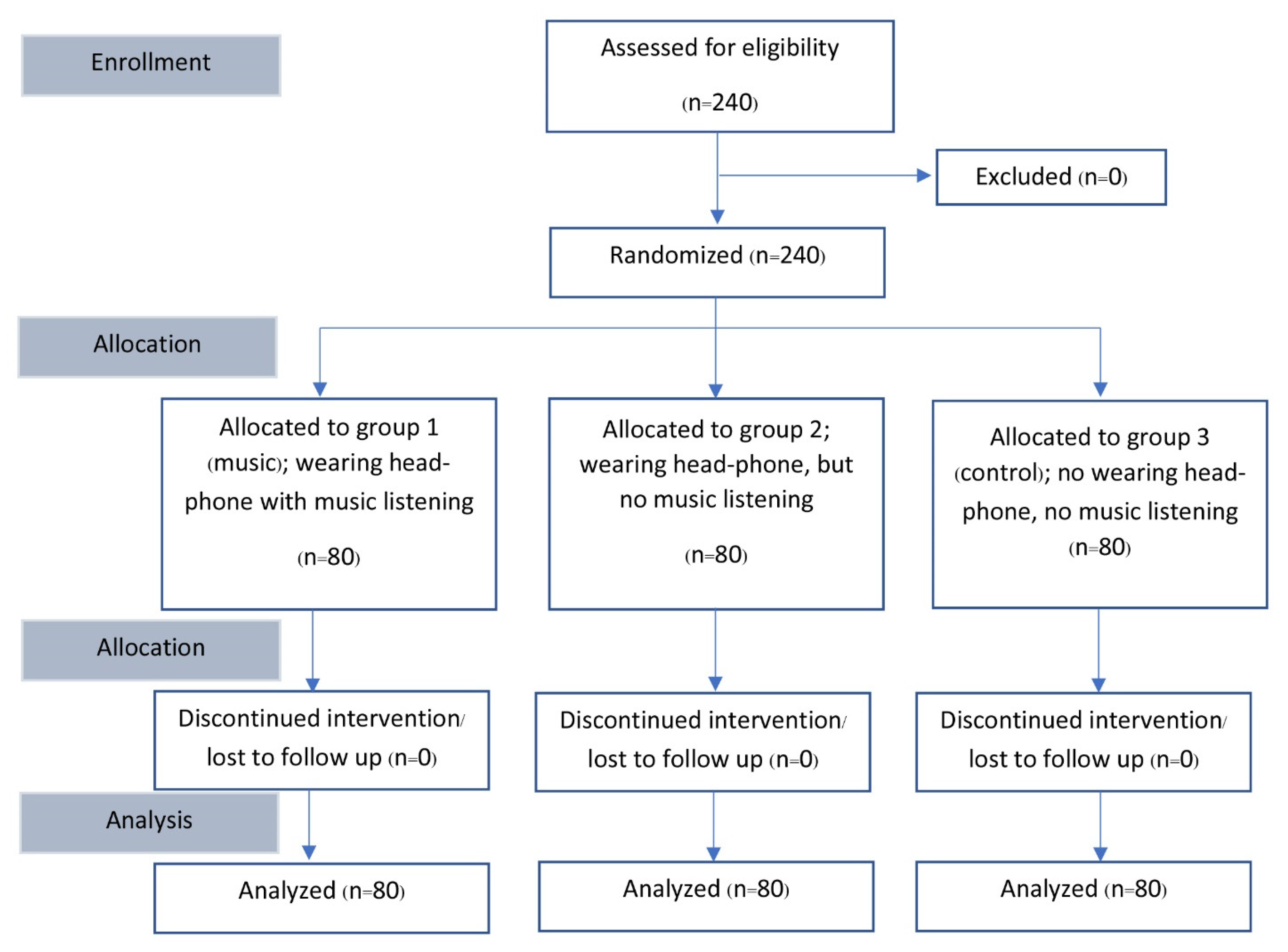
2. Material and Methods
3. Results
4. Discussion
5. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Acknowledgments
Conflicts of Interest
References
- Sung, H.; Ferlay, J.; Siegel, R.L.; Laversanne, M.; Soerjomataram, I.; Jemal, A.; Bray, F. Global cancer statistics 2020: GLOBOCAN estimates of incidence and mortality worldwide for 36 cancers in 185 countries. CA Cancer J. Clin. 2021, 71, 209–249. [Google Scholar] [CrossRef] [PubMed]
- Bray, F.; Ferlay, J.; Soerjomataram, I.; Siegel, R.L.; Torre, L.A.; Jemal, A. Global cancer statistics 2018: GLOBOCAN estimates of incidence and mortality worldwide for 36 cancers in 185 countries. CA Cancer J. Clin. 2018, 68, 394–424. [Google Scholar] [CrossRef] [Green Version]
- Human Papillomavirus and Related Cancers in World. Summary Report 2010. 2010. Available online: http://www.who.int/hpvcentre/en/ (accessed on 1 February 2022).
- Torre, L.A.; Bray, F.; Siegel, R.L.; Ferlay, J.; Lortet-Tieulent, J.; Jemal, A. Global cancer statistics, 2012. CA Cancer J. Clin. 2015, 65, 87–108. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Khan, M.J.; Werner, C.L.; Darragh, T.M.; Guido, R.S.; Mathews, C.; Moscicki, A.B.; Mitchell, M.M.; Schiffman, M.; Wentzensen, N.; Massad, L.S.; et al. ASCCP colposcopy standards: Role of colposcopy, benefits, potential harms, and terminology for colposcopic practice. J. Low. Genit. Tract Dis. 2017, 21, 223–229. [Google Scholar] [CrossRef] [PubMed]
- Cheung, L.C.; Egemen, D.; Chen, X.; Katki, H.A.; Demarco, M.; Wiser, A.L.; Perkins, R.B.; Guido, R.S.; Wentzensen, N.; Schiffman, M. 2019 ASCCP risk-based management consensus guidelines: Methods for risk estimation, recommended management, and validation. J. Low. Genit. Tract Dis. 2020, 24, 90–101. [Google Scholar] [CrossRef] [PubMed]
- Mao, C. Teaching residents humanistic skills in a colposcopy clinic. Acad. Med. 2002, 77, 742. [Google Scholar] [CrossRef] [PubMed]
- Karaman, E.; Kolusarı, A.; Alkış, İ.; Çetin, O. Comparison of topical lidocaine spray with forced coughing in pain relief during colposcopic biopsy procedure: A randomised trial. J. Obstet. Gynaecol. J. Inst. Obstet. Gynaecol. 2019, 39, 534–538. [Google Scholar] [CrossRef] [PubMed]
- Naki, M.M.; Api, O.; Acioglu, H.C.; Uzun, M.G.; Kars, B.; Unal, O. Analgesic efficacy of forced coughing versus local anesthesia during cervical punch biopsy. Gynecol. Obstet. Investig. 2011, 72, 5–9. [Google Scholar] [CrossRef] [PubMed]
- Oyama, I.A.; Wakabayashi, M.T.; Frattarelli, L.C.; Kessel, B. Local anesthetic reduces the pain of colposcopic biopsies: A randomized trial. Am. J. Obstet. Gynecol. 2003, 188, 1164–1165. [Google Scholar] [CrossRef] [PubMed]
- Öz, M.; Korkmaz, E.; Cetinkaya, N.; Bas, S.; Özdal, B.; Meydanl, M.M.; Güngör, T. Comparison of topical lidocaine spray with placebo for pain relief in colposcopic procedures: A randomized, placebo-controlled, double-blind study. J. Low. Genit. Tract Dis. 2015, 19, 212–214. [Google Scholar] [CrossRef] [PubMed]
- Gauba, A.; Ramachandra, M.N.; Saraogi, M.; Geraghty, R.; Hameed, B.Z.; Abumarzouk, O.; Somani, B.K. Music reduces patient-reported pain and anxiety and should be routinely offered during flexible cystoscopy: Outcomes of a systematic review. Arab. J. Urol. 2021, 19, 480–487. [Google Scholar] [CrossRef]
- Hsu, H.F.; Chen, K.M.; Belcastro, F. The effect of music interventions on chronic pain experienced by older adults: A systematic review. J. Nurs. Scholarsh. Off. Publ. Sigma Tau Int. Honor. Soc. Nurs. 2022, 54, 64–71. [Google Scholar] [CrossRef] [PubMed]
- Patiyal, N.; Kalyani, V.; Mishra, R.; Kataria, N.; Sharma, S.; Parashar, A.; Kumari, P. Effect of music therapy on pain, anxiety, and use of opioids among patients underwent orthopedic surgery: A systematic review and meta-analysis. Cureus 2021, 13, e18377. [Google Scholar] [CrossRef] [PubMed]
- Ting, B.; Tsai, C.L.; Hsu, W.T.; Shen, M.L.; Tseng, P.T.; Chen, D.T.; Su, K.P.; Jingling, L. Music intervention for pain control in the pediatric population: A systematic review and meta-analysis. J. Clin. Med. 2022, 11, 991. [Google Scholar] [CrossRef] [PubMed]
- Chan, Y.M.; Lee, P.W.; Ng, T.Y.; Ngan, H.Y.; Wong, L.C. The use of music to reduce anxiety for patients undergoing colposcopy: A randomized trial. Gynecol. Oncol. 2003, 91, 213–217. [Google Scholar] [CrossRef]
- Galaal, K.; Bryant, A.; Deane, K.H.; Al-Khaduri, M.; Lopes, A.D. Interventions for reducing anxiety in women undergoing colposcopy. Cochrane Database Syst. Rev. 2011, 12, CD006013. [Google Scholar]
- Danhauer, S.C.; Rutherford, C.A.; Lovato, J.F.; Asbury, D.Y.; Marler, B.; McQuellon, R.P.; Miller, B.E. Music or guided imagery for women undergoing colposcopy: A randomized controlled study of effects on anxiety, pain level, and patient satisfaction. J. Low. Genit. Tract Dis. 2006, 10, 185. [Google Scholar] [CrossRef]
- Hilal, Z.; Alici, F.; Tempfer, C.B.; Rath, K.; Nar, K.; Rezniczek, G.A. Mozart for reducing patient anxiety during colposcopy: A randomized controlled trial. Obstet. Gynecol. 2018, 132, 1047–1055. [Google Scholar] [CrossRef] [PubMed]
- Mak, N.; Reinders, I.M.A.; Slockers, S.A.; Westen, E.; Maas, J.W.M.; Bongers, M.Y. The effect of music in gynaecological office procedures on pain, anxiety and satisfaction: A randomized controlled trial. Gynecol. Surg. 2017, 14, 14. [Google Scholar] [CrossRef] [PubMed]
- Abdelhakim, A.M.; Samy, A.; Abbas, A.M. Effect of music in reducing patient anxiety during colposcopy: A systematic review and meta-analysis of randomized controlled trials. J. Gynecol. Obstet. Hum. Reprod. 2019, 48, 855–861. [Google Scholar] [CrossRef] [PubMed]
- Norman, G.R.; Streiner, D.L. Biostatistics: The Bare Essentials, 3rd ed.; B.C. Decker: New York, NY, USA, 2008. [Google Scholar]
- Angioli, R.; Nardone, C.D.C.; Plotti, F.; Cafà, E.V.; Dugo, N.; Damiani, P.; Ricciardi, R.; Linciano, F.; Terranova, C. Use of music to reduce anxiety during office hysteroscopy: Prospective randomized trial. J. Minim. Invasive Gynecol. 2014, 21, 454–459. [Google Scholar] [CrossRef] [PubMed]
- Law, H.Y.; Ng, D.Y.T.; Chung, C.D. Use of music in reducing pain during outpatient hysteroscopy: Prospective randomized trial. J. Obstet. Gynaecol. Res. 2021, 47, 904–912. [Google Scholar] [CrossRef] [PubMed]
- Bradshaw, D.H.; Chapman, C.R.; Jacobson, R.C.; Donaldson, G.W. Effects of music engagement on responses to painful stimulation. Clin. J. Pain 2012, 28, 418–427. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Kelly, D.J.; Ahmad, M.; Brull, S.J. Preemptive analgesia I: Physiological pathways and pharmacological modalities. Can. J. Anaesth. 2001, 48, 1000–1010. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Salimpoor, V.N.; Benovoy, M.; Larcher, K.; Dagher, A.; Zatorre, R.J. Anatomically distinct dopamine release during anticipation and experience of peak emotion to music. Nat. Neurosci. 2011, 14, 257–262. [Google Scholar] [CrossRef] [PubMed]
- Valet, M.; Sprenger, T.; Boecker, H.; Willoch, F.; Rummeny, E.; Conrad, B.; Erhard, P.; Tolle, T.R. Distraction modulates connectivity of the cingulo-frontal cortex and the midbrain during pain—An fMRI analysis. Pain 2004, 109, 399–408. [Google Scholar] [CrossRef] [PubMed]
- Lee, J.H. The effects of music on pain: A meta-analysis. J. Music Ther. 2016, 53, 430–477. [Google Scholar] [CrossRef]
- Huang, Q.; Lin, J.; Han, R.; Peng, C.; Huang, A. Using virtual reality exposure therapy in pain management: A systematic review and meta-analysis of randomized controlled trials. Value Health 2022, 25, 288–301. [Google Scholar] [CrossRef]
- Karaman, D.; Taşdemir, N. The effect of using virtual reality during breast biopsy on pain and anxiety: A randomized controlled trial. J. Perianesth. Nurs. 2021, 36, 702–705. [Google Scholar] [CrossRef]
- Noergaard, M.W.; Håkonsen, S.J.; Bjerrum, M.; Pedersen, P.U. The effectiveness of hypnotic analgesia in the management of procedural pain in minimally invasive procedures: A systematic review and meta-analysis. J. Clin. Nurs. 2019, 28, 4207–4224. [Google Scholar] [CrossRef]
- Langlois, P.; Perrochon, A.; David, R.; Rainville, P.; Wood, C.; Vanhaudenhuyse, A.; Pageaux, B.; Ounajim, A.; Lavallière, M.; Debarnot, U.; et al. Hypnosis to manage musculoskeletal and neuropathic chronic pain: A systematic review and meta-analysis. Neurosci. Biobehav. Rev. 2022, 135, 104591. [Google Scholar] [CrossRef] [PubMed]
- Wood, C.; Martiné, G.; Espagne-Dubreuilh, G.; Le Goff, K.; Moens, M.; Goudman, L.; Baron, S.; David, R.; Naïditch, N.; Billot, M.; et al. The added value of intraoperative hypnosis during spinal cord stimulation lead implantation under awake anesthesia in patients presenting with refractory chronic pain. Medicina 2022, 58, 220. [Google Scholar] [CrossRef] [PubMed]

| Characteristics | Headphones with Music (n = 80) | Headphones without Music (n = 80) | Usual Care (n = 80) | p-Value |
|---|---|---|---|---|
| Age (years) | 41.00 (30.00–51.00) | 40.00 (32.00–52.00) | 43.00 (34.50–52.50) | 0.38 |
| Parity | 0.07 | |||
| Nulliparity | 35 (43.8) | 21 (26.3) | 28 (35.0) | |
| Multiparity | 45 (56.3) | 59 (73.8) | 52 (65.0) | |
| Menopause status | 0.98 | |||
| No | 59 (73.8) | 57 (71.3) | 58 (72.5) | |
| Yes | 21 (26.3) | 23 (28.8) | 22 (27.5) | |
| Dysmenorrhea | 0.06 | |||
| No | 43 (53.8) | 49 (61.3) | 59 (73.8) | |
| Mild | 26 (32.5) | 21 (26.3) | 14 (17.5) | |
| Moderate | 6 (7.5) | 8 (10.0) | 7 (8.8) | |
| Severe | 5 (6.3) | 2 (2.5) | 0 (0.0) | |
| HIV | 0.16 | |||
| Negative | 78 (97.5) | 72 (90.0) | 75 (93.8) | |
| Positive | 2 (2.5) | 8 (10.0) | 5 (6.3) | |
| Underlying disease | 0.11 | |||
| No | 63 (78.8) | 56 (70.0) | 59 (73.8) | |
| Yes | 17 (21.3) | 24 (30) | 21 (26.3) | |
| Anxiety score | 0.80 | |||
| No | 22 (27.5) | 14 (17.5) | 15 (18.8) | |
| Mild | 33 (41.3) | 38 (47.5) | 35 (43.8) | |
| Moderate | 15 (18.8) | 18 (22.5) | 18 (22.5) | |
| Severe | 10 (12.5) | 10 (12.5) | 12 (15.0) | |
| HPV test | 0.97 | |||
| Not done | 59 (73.8) | 61 (76.3) | 58 (72.5) | |
| Negative | 4 (5.0) | 5 (6.3) | 4 (5.0) | |
| High-risk HPV-positive | 9 (11.3) | 9 (11.3) | 9 (11.3) | |
| Other 12 HR HPV-positive | 8 (10.0) | 5 (6.3) | 9 (11.3) | |
| Cytology | 0.14 | |||
| Normal | 6 (7.9) | 3 (3.8) | 3 (3.8) | |
| ASCUS | 34 (42.5) | 24 (30.0) | 31 (38.8) | |
| LSIL | 29 (36.3) | 33 (41.3) | 29 (36.3) | |
| HSIL | 6 (7.5) | 14 (17.5) | 10 (12.5) | |
| ASC-H | 2 (2.5) | 3 (3.8) | 7 (8.8) | |
| No cytology | 3 (3.8) | 3 (3.8) | 0 (0.0) | |
| Final histology | 0.01 * | |||
| Normal/inflammation | 47 (58.8) | 40 (50.0) | 39 (48.8) | |
| LSIL | 23 (28.8) | 16 (20.0) | 29 (36.6) | |
| HSIL | 7 (8.8) | 23 (28.8) | 11 (13.8) | |
| Cancer | 3 (3.8) | 1 (1.3) | 1 (1.3) | |
| Number of biopsies | 0.09 | |||
| 1 | 15 (18.8) | 26 (32.5) | 15 (18.8) | |
| 2 | 63 (78.8) | 54 (67.5) | 64 (80.0) | |
| 3 | 2 (2.5) | 0 (0.0) | 1 (1.3) |
| Pain Score | Total (n = 240) | Headphone with Music (n = 80) | Headphones without Music (n = 80) | Usual Care (n = 80) | p-Value |
|---|---|---|---|---|---|
| Baseline | 2.77 (2.50–3.04) | 2.83 (2.37–3.28) | 2.54 (2.08–3.00) | 2.94 (2.45–3.43) | 0.47 |
| Biopsy | 4.25 (3.92–4.58) | 4.21 (3.64–4.78) | 4.24 (3.67–4.81) | 4.30 (3.74–4.86) | 0.98 |
| Biopsy to baseline change | 1.48 (1.13–1.83) | 1.39 (0.69–2.08) | 1.70 (1.13–2.27) | 1.36 (0.81–1.90) | 0.69 |
| Post-procedure | 2.34 (2.09–2.59) | 2.34 (1.91–2.77) | 2.44 (2.00–2.87) | 2.25 (1.82–2.68) | 0.83 |
| Variables | Mean Difference (95%CI) | p-Value |
|---|---|---|
| Biopsy to baseline difference (scores) | ||
| Headphone without music vs. control group | −0.34 (−1.21–0.52) | 0.44 |
| Headphone with music vs. control group | −0.03 (−0.90–0.83) | 0.94 |
| Headphone with music vs. without music | 0.31 (−0.55–1.18) | 0.48 |
| Postprocedure to baseline difference (scores) | ||
| Headphone without music vs. control group | −0.59 (−1.33–0.15) | 0.12 |
| Headphone with music vs. control group | −0.21 (−0.95–0.53) | 0.58 |
| Headphone with music vs. without music | 0.39 (−0.35–1.13) | 0.30 |
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2022 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Pradit, L.; Tantipalakorn, C.; Charoenkwan, K.; Suprasert, P.; Srisomboon, J.; Muangmool, T. Efficacy of Listening to Music on Pain Reduction during Colposcopy-Directed Cervical Biopsy: A Randomized, Controlled Trial. Medicina 2022, 58, 429. https://doi.org/10.3390/medicina58030429
Pradit L, Tantipalakorn C, Charoenkwan K, Suprasert P, Srisomboon J, Muangmool T. Efficacy of Listening to Music on Pain Reduction during Colposcopy-Directed Cervical Biopsy: A Randomized, Controlled Trial. Medicina. 2022; 58(3):429. https://doi.org/10.3390/medicina58030429
Chicago/Turabian StylePradit, Lalita, Charuwan Tantipalakorn, Kittipat Charoenkwan, Prapaporn Suprasert, Jatupol Srisomboon, and Tanarat Muangmool. 2022. "Efficacy of Listening to Music on Pain Reduction during Colposcopy-Directed Cervical Biopsy: A Randomized, Controlled Trial" Medicina 58, no. 3: 429. https://doi.org/10.3390/medicina58030429
APA StylePradit, L., Tantipalakorn, C., Charoenkwan, K., Suprasert, P., Srisomboon, J., & Muangmool, T. (2022). Efficacy of Listening to Music on Pain Reduction during Colposcopy-Directed Cervical Biopsy: A Randomized, Controlled Trial. Medicina, 58(3), 429. https://doi.org/10.3390/medicina58030429







