Relationship between the Accuracy of the Acetabular Cup Angle and BMI in Posterolateral Total Hip Arthroplasty with CT-Based Navigation
Abstract
:1. Introduction
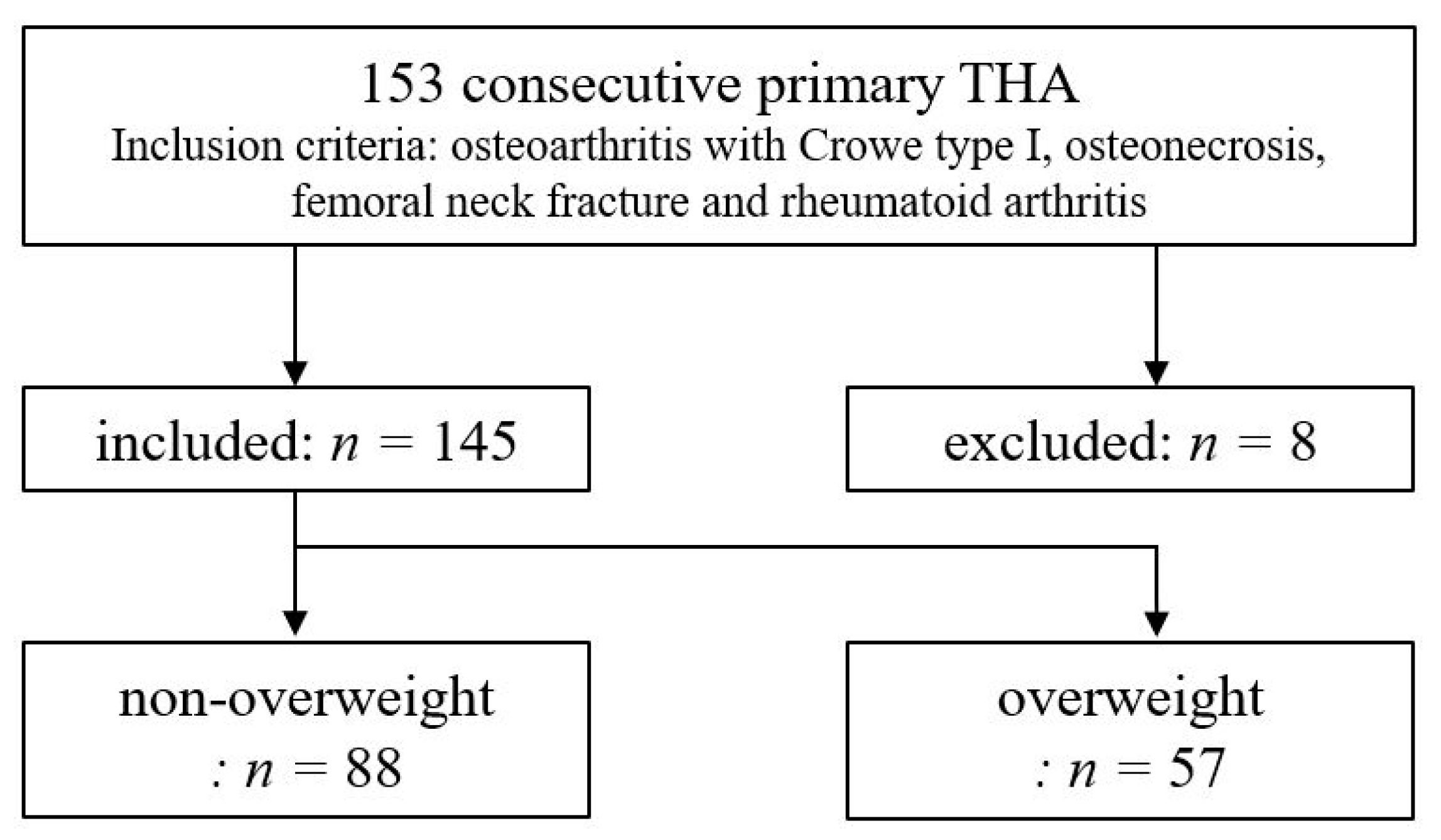
2. Materials and Methods
2.1. Participants
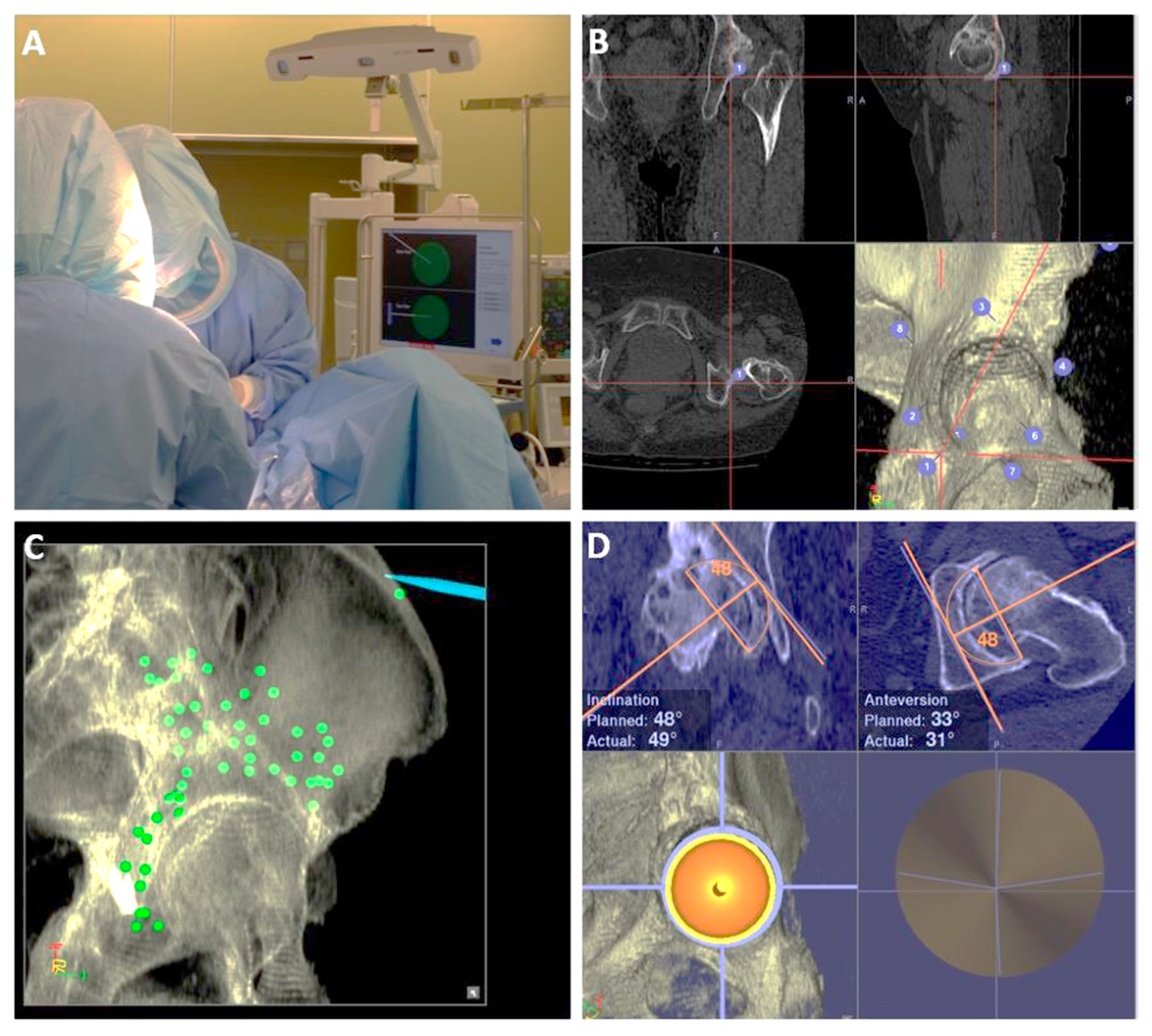
2.2. Preoperative Planning
2.3. Surgical Procedure with CT-Navi
2.4. Postoperative Evaluation
2.5. Data Analysis
3. Results
4. Discussion
5. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Conflicts of Interest
References
- Jamari, J.; Ammarullah, M.I.; Santoso, G.; Sugiharto, S.; Supriyono, T.; Prakoso, A.T.; Basri, H.; van der Heide, E. Computational Contact Pressure Prediction of CoCrMo, SS 316L and Ti6Al4V Femoral Head against UHMWPE Acetabular Cup under Gait Cycle. J. Funct. Biomater. 2022, 13, 64. [Google Scholar] [CrossRef] [PubMed]
- Merola, M.; Affatato, S. Materials for Hip Prostheses: A Review of Wear and Loading Considerations. Materials 2019, 12, 495. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Lass, R.; Olischar, B.; Kubista, B.; Waldhoer, T.; Giurea, A.; Windhager, R. Total Hip Arthroplasty Using Imageless Computer-Assisted Navigation-2-Year Follow-Up of a Prospective Randomized Study. J. Clin. Med. 2020, 9, 1620. [Google Scholar] [CrossRef] [PubMed]
- Brady, A.W.; Tatka, J.; Fagotti, L.; Kemler, B.R.; Fossum, B.W. Accuracy and Reliability of Software Navigation for Acetabular Component Placement in THA: An In Vitro Validation Study. Medicina 2022, 58, 663. [Google Scholar] [CrossRef]
- Lewinnek, G.E.; Lewis, J.L.; Tarr, R.; Compere, C.L.; Zimmerman, J.R. Dislocations after total hip-replacement arthroplasties. J. Bone Jt. Surg. Am. 1978, 60, 217–220. [Google Scholar] [CrossRef]
- Abdel, M.P.; von Roth, P.; Jennings, M.T.; Hanssen, A.D.; Pagnano, M.W. What Safe Zone? The Vast Majority of Dislocated THAs Are Within the Lewinnek Safe Zone for Acetabular Component Position. Clin. Orthop. Relat. Res. 2016, 474, 386–391. [Google Scholar] [CrossRef] [Green Version]
- Widmer, K.H.; Zurfluh, B. Compliant positioning of total hip components for optimal range of motion. J. Orthop. Res. 2004, 22, 815–821. [Google Scholar] [CrossRef]
- Yoshimine, F. The safe-zones for combined cup and neck anteversions that fulfill the essential range of motion and their optimum combination in total hip replacements. J. Biomech. 2006, 39, 1315–1323. [Google Scholar] [CrossRef]
- Barrack, R.L.; Krempec, J.A.; Clohisy, J.C.; McDonald, D.J.; Ricci, W.M.; Ruh, E.L.; Nunley, R.M. Accuracy of acetabular component position in hip arthroplasty. J. Bone Jt. Surg. Am. 2013, 95, 1760–1768. [Google Scholar] [CrossRef] [Green Version]
- Tsukada, S.; Wakui, M. Decreased accuracy of acetabular cup placement for imageless navigation in obese patients. J. Orthop. Sci. 2010, 15, 758–763. [Google Scholar] [CrossRef]
- Imai, N.; Takubo, R.; Suzuki, H.; Shimada, H.; Miyasaka, D.; Tsuchiya, K.; Endo, N. Accuracy of acetabular cup placement using CT-based navigation in total hip arthroplasty: Comparison between obese and non-obese patients. J. Orthop. Sci. 2019, 24, 482–487. [Google Scholar] [CrossRef] [PubMed]
- Takada, R.; Jinno, T.; Miyatake, K.; Hirao, M.; Yagishita, K.; Yoshii, T.; Okawa, A. Supine versus lateral position for accurate positioning of acetabular cup in total hip arthroplasty using the modified Watson-Jones approach: A randomized single-blind controlled trial. Orthop. Traumatol. Surg. Res. 2019, 105, 915–922. [Google Scholar] [CrossRef] [PubMed]
- Crowe, J.F.; Mani, V.J.; Ranawat, C.S. Total hip replacement in congenital dislocation and dysplasia of the hip. J. Bone Jt. Surg. Am. Vol. 1979, 61, 15–23. [Google Scholar] [CrossRef] [Green Version]
- Arai, N.; Nakamura, S.; Matsushita, T.; Suzuki, S. Minimal radiation dose computed tomography for measurement of cup orientation in total hip arthroplasty. J. Arthroplast. 2010, 25, 263–267. [Google Scholar] [CrossRef]
- Kamenaga, T.; Hayashi, S.; Hashimoto, S.; Fukuda, K.; Takayama, K.; Tsubosaka, M.; Takashima, Y.; Niikura, T.; Kuroda, R.; Matsumoto, T. Pelvic morphology medial to the femoral head center predicts anterior coverage and range of motion after curved periacetabular osteotomy. J. Orthop. Res. Off. Publ. Orthop. Res. Soc. 2020, 38, 2031–2039. [Google Scholar] [CrossRef]
- Mukaka, M.M. Statistics corner: A guide to appropriate use of correlation coefficient in medical research. Malawi Med. J. 2012, 24, 69–71. [Google Scholar]
- Asai, Y.; Tsutsui, S.; Oka, H.; Yoshimura, N.; Hashizume, H.; Yamada, H.; Akune, T.; Muraki, S.; Matsudaira, K.; Kawaguchi, H.; et al. Sagittal spino-pelvic alignment in adults: The Wakayama Spine Study. PLoS ONE 2017, 12, e0178697. [Google Scholar] [CrossRef]
- Kennedy, J.G.; Rogers, W.B.; Soffe, K.E.; Sullivan, R.J.; Griffen, D.G.; Sheehan, L.J. Effect of acetabular component orientation on recurrent dislocation, pelvic osteolysis, polyethylene wear, and component migration. J. Arthroplast. 1998, 13, 530–534. [Google Scholar] [CrossRef]
- Leslie, I.J.; Williams, S.; Isaac, G.; Ingham, E.; Fisher, J. High cup angle and microseparation increase the wear of hip surface replacements. Clin. Orthop. Relat. Res. 2009, 467, 2259–2265. [Google Scholar] [CrossRef] [Green Version]
- Little, N.J.; Busch, C.A.; Gallagher, J.A.; Rorabeck, C.H.; Bourne, R.B. Acetabular polyethylene wear and acetabular inclination and femoral offset. Clin. Orthop. Relat. Res. 2009, 467, 2895–2900. [Google Scholar] [CrossRef] [Green Version]
- Sugano, N.; Takao, M.; Sakai, T.; Nishii, T.; Miki, H. Does CT-based navigation improve the long-term survival in ceramic-on-ceramic THA? Clin. Orthop. Relat. Res. 2012, 470, 3054–3059. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Iwana, D.; Nakamura, N.; Miki, H.; Kitada, M.; Hananouchi, T.; Sugano, N. Accuracy of angle and position of the cup using computed tomography-based navigation systems in total hip arthroplasty. Comput. Aided Surg. 2013, 18, 187–194. [Google Scholar] [CrossRef] [PubMed]
- Tsutsui, T.; Goto, T.; Wada, K.; Takasago, T.; Hamada, D.; Sairyo, K. Efficacy of a computed tomography-based navigation system for placement of the acetabular component in total hip arthroplasty for developmental dysplasia of the hip. J. Orthop. Surg. 2017, 25, 2309499017727954. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Kalteis, T.; Handel, M.; Bathis, H.; Perlick, L.; Tingart, M.; Grifka, J. Imageless navigation for insertion of the acetabular component in total hip arthroplasty: Is it as accurate as CT-based navigation? J. Bone Jt. Surg. Br. 2006, 88, 163–167. [Google Scholar] [CrossRef] [PubMed]
- Goodnough, L.H.; Finlay, A.K.; Huddleston, J.I., 3rd; Goodman, S.B.; Maloney, W.J.; Amanatullah, D.F. Obesity Is Independently Associated With Early Aseptic Loosening in Primary Total Hip Arthroplasty. J. Arthroplast. 2018, 33, 882–886. [Google Scholar] [CrossRef]
- Triantafyllopoulos, G.K.; Soranoglou, V.G.; Memtsoudis, S.G.; Sculco, T.P.; Poultsides, L.A. Rate and Risk Factors for Periprosthetic Joint Infection among 36,494 Primary Total Hip Arthroplasties. J. Arthroplast. 2018, 33, 1166–1170. [Google Scholar] [CrossRef]
- Purcell, R.L.; Parks, N.L.; Cody, J.P.; Hamilton, W.G. Comparison of Wound Complications and Deep Infections with Direct Anterior and Posterior Approaches in Obese Hip Arthroplasty Patients. J. Arthroplast. 2018, 33, 220–223. [Google Scholar] [CrossRef]
- Russo, M.W.; Macdonell, J.R.; Paulus, M.C.; Keller, J.M.; Zawadsky, M.W. Increased Complications in Obese Patients Undergoing Direct Anterior Total Hip Arthroplasty. J. Arthroplast. 2015, 30, 1384–1387. [Google Scholar] [CrossRef]
- Ramachandran, A.; Chamukuttan, S.; Shetty, S.A.; Arun, N.; Susairaj, P. Obesity in Asia--is it different from rest of the world. Diabetes Metab. Res. Rev. 2012, 28 (Suppl. 2), 47–51. [Google Scholar] [CrossRef]


| Non-Overweight | Overweight | p-Value | |
|---|---|---|---|
| Number of hips | 88 | 57 | |
| Mean BMI | 21.7 | 28.7 | <0.001 * |
| Age (years) | 66.3 ± 11.3 | 60.5 ± 10.5 | 0.002 * |
| Female sex | 70 (80%) | 39 (68%) | 0.13 ** |
| Diagnosis | |||
| OA | 68 (77%) | 45 (79%) | 0.81 ** |
| ON | 17 (19%) | 10 (18%) | 0.91 ** |
| FNF | 2 | 1 | |
| RA | 1 | 1 |
| Non-Overweight | Overweight | p-Value | |
|---|---|---|---|
| RI (°) | 2.8 ± 2.2 | 2.6 ± 2.4 | 0.67 * |
| RA (°) | 2.6 ± 2.3 | 2.4 ± 2.4 | 0.58 * |
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2022 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Ishikura, H.; Nakamura, M.; Nakamura, S.; Tanaka, T.; Kawano, H.; Tanaka, S. Relationship between the Accuracy of the Acetabular Cup Angle and BMI in Posterolateral Total Hip Arthroplasty with CT-Based Navigation. Medicina 2022, 58, 856. https://doi.org/10.3390/medicina58070856
Ishikura H, Nakamura M, Nakamura S, Tanaka T, Kawano H, Tanaka S. Relationship between the Accuracy of the Acetabular Cup Angle and BMI in Posterolateral Total Hip Arthroplasty with CT-Based Navigation. Medicina. 2022; 58(7):856. https://doi.org/10.3390/medicina58070856
Chicago/Turabian StyleIshikura, Hisatoshi, Masaki Nakamura, Shigeru Nakamura, Takeyuki Tanaka, Hirotaka Kawano, and Sakae Tanaka. 2022. "Relationship between the Accuracy of the Acetabular Cup Angle and BMI in Posterolateral Total Hip Arthroplasty with CT-Based Navigation" Medicina 58, no. 7: 856. https://doi.org/10.3390/medicina58070856






