Combined Anterior Cruciate Ligament and Anterolateral Ligament Reconstruction Using a Single Achilles Tendon Allograft: A Technical Note
Abstract
:1. Introduction
2. Surgical Technique
2.1. Patient Setup
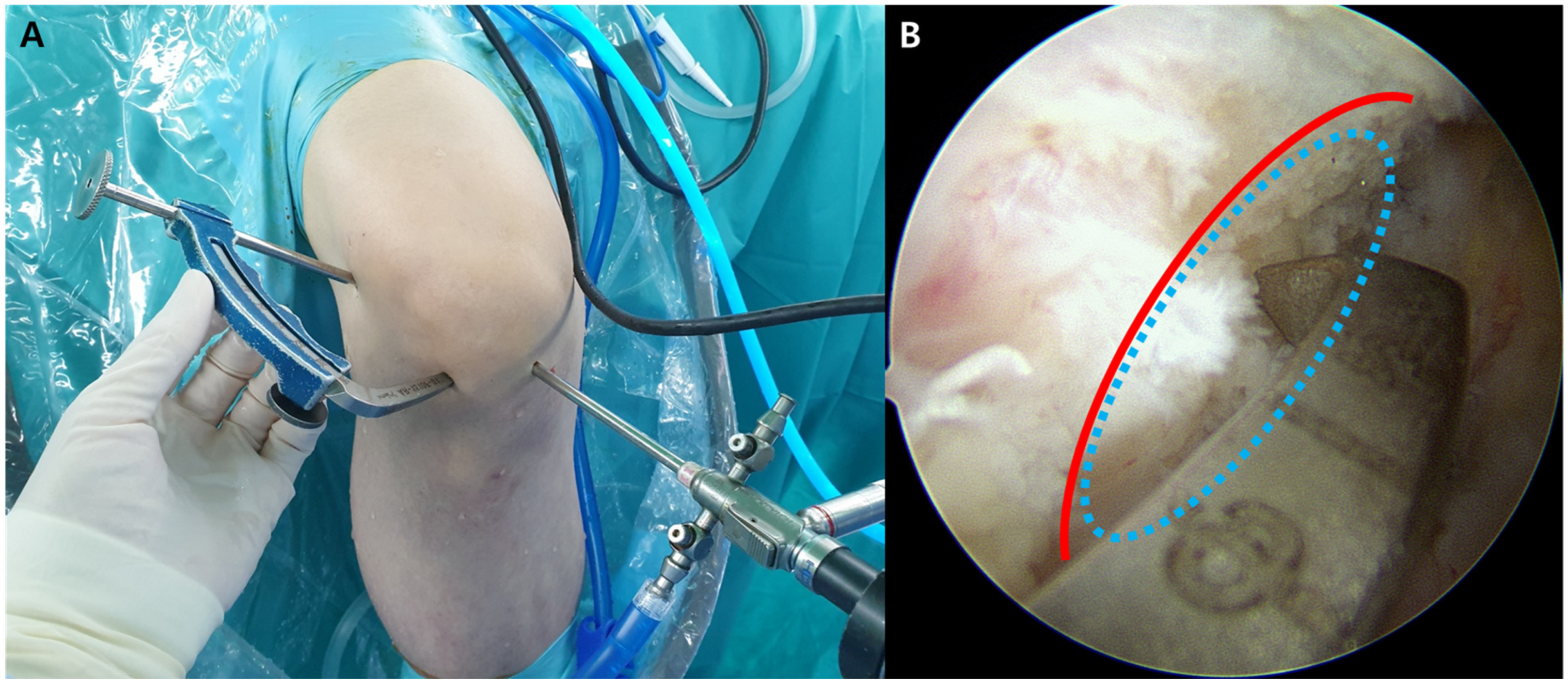
2.2. Arthroscopic Examination and Tibial and Femoral Tunnel Preparation for ACLR
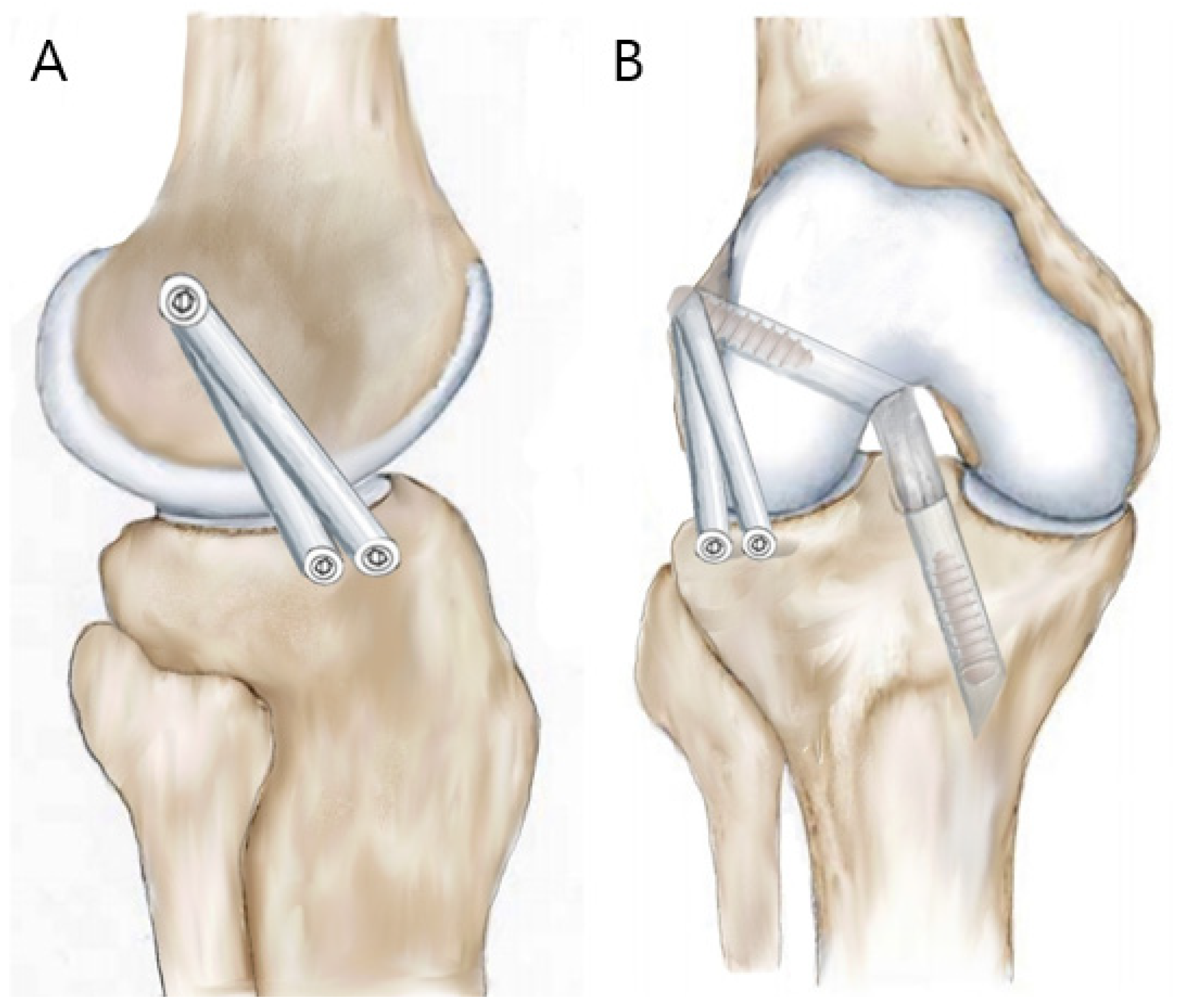
2.3. Preparation of Two Tibial Bony Sockets for ALLR
2.4. Graft Preparation
2.5. Graft Passage and Fixation for the Combined ACL and ALL Reconstruction
3. Discussion
4. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Conflicts of Interest
References
- McCulloch, P.C.; Lattermann, C.; Boland, A.L.; Bach, B.R. An illustrated history of anterior cruciate ligament surgery. J. Knee Surg. 2007, 20, 95–104. [Google Scholar] [CrossRef] [PubMed]
- Chambat, P.; Guier, C.; Sonnery-Cottet, B.; Fayard, J.M.; Thaunat, M. The evolution of ACL reconstruction over the last fifty years. Int. Orthop. 2013, 37, 181–186. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Ardern, C.L.; Webster, K.E.; Taylor, N.F.; Feller, J.A. Return to sport following anterior cruciate ligament reconstruction surgery: A systematic review and meta-analysis of the state of play. Br. J. Sports Med. 2011, 45, 596–606. [Google Scholar] [CrossRef] [PubMed]
- Hettrich, C.M.; Dunn, W.R.; Reinke, E.K.; Group, M.; Spindler, K.P. The rate of subsequent surgery and predictors after ante-rior cruciate ligament reconstruction: Two-and 6-year follow-up results from a multicenter cohort. Am. J. Sports Med. 2013, 41, 1534–1540. [Google Scholar] [CrossRef] [PubMed]
- Hussein, M.; van Eck, C.F.; Cretnik, A.; Dinevski, D.; Fu, F.H. Individualized anterior cruciate ligament surgery: A prospec-tive study comparing anatomic single-and double-bundle reconstruction. Am. J. Sports Med. 2012, 40, 1781–1788. [Google Scholar] [CrossRef] [PubMed]
- Lind, M.; Menhert, F.; Pedersen, A.B. Incidence and outcome after revision anterior cruciate ligament reconstruction: Results from the Danish registry for knee ligament reconstructions. Am. J. Sports Med. 2012, 40, 1551–1557. [Google Scholar] [CrossRef]
- Ariel de Lima, D.; de Lima, L.L.; de Souza, N.G.R.; de Moraes Perez, R.A.; Sobrado, M.F.; Guimarães, T.M.; Helito, C.P. Clinical outcomes of combined anterior cruciate ligament and anterolateral ligament reconstruction: A systematic review and meta-analysis. Knee Surg. Relat. Res. 2021, 33, 33. [Google Scholar] [CrossRef]
- Claes, S.; Vereecke, E.; Maes, M.; Victor, J.; Verdonk, P.; Bellemans, J. Anatomy of the anterolateral ligament of the knee. J. Anat. 2013, 223, 321–328. [Google Scholar] [CrossRef]
- Dodds, A.L.; Halewood, C.; Gupte, C.M.; Williams, A.; Amis, A.A. The anterolateral ligament: Anatomy, length changes and association with the Segond fracture. Bone Jt. J. 2014, 96, 325–331. [Google Scholar] [CrossRef]
- Kennedy, M.I.; Claes, S.; Fuso, F.A.F.; Williams, B.T.; Goldsmith, M.T.; Turnbull, T.L.; Wijdicks, C.A.; LaPrade, R.F. The An-terolateral Ligament. Am. J. Sports Med. 2015, 43, 1606–1615. [Google Scholar] [CrossRef]
- Thein, R.; Boorman-Padgett, J.; Stone, K.; Wickiewicz, T.L.; Imhauser, C.W.; Pearle, A.D. Biomechanical Assessment of the Anterolateral Ligament of the Knee: A Secondary Restraint in Simulated Tests of the Pivot Shift and of Anterior Stability. J. Bone Jt. Surg Am. 2016, 98, 937–943. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Tavlo, M.; Eljaja, S.; Jensen, J.T.; Siersma, V.D.; Krogsgaard, M.R. The role of the anterolateral ligament in ACL insufficient and reconstructed knees on rotatory stability: A biomechanical study on human cadavers. Scand. J. Med. Sci. Sports 2016, 26, 960–966. [Google Scholar] [CrossRef] [PubMed]
- Spencer, L.; Burkhart, T.A.; Tran, M.N.; Rezansoff, A.J.; Deo, S.; Caterine, S.; Getgood, A.M. Biomechanical Analysis of Simu-lated Clinical Testing and Reconstruction of the Anterolateral Ligament of the Knee. Am. J. Sports Med. 2015, 43, 2189–2197. [Google Scholar] [CrossRef] [PubMed]
- Inderhaug, E.; Stephen, J.M.; Williams, A.; Amis, A.A. Biomechanical comparison of anterolateral procedures combined with anterior cruciate ligament reconstruction. Am. J. Sports Med. 2017, 45, 347–354. [Google Scholar] [CrossRef] [PubMed]
- Hardy, A.; Casabianca, L.; Hardy, E.; Grimaud, O.; Meyer, A. Combined reconstruction of the anterior cruciate ligament associated with anterolateral tenodesis effectively controls the acceleration of the tibia during the pivot shift. Knee Surg. Sports Traumatol. Arthrosc. 2017, 25, 1117–1124. [Google Scholar] [CrossRef] [PubMed]
- Bonanzinga, T.; Signorelli, C.; Grassi, A.; Lopomo, N.; Jain, M.; Mosca, M.; Iacono, F.; Marcacci, M.; Zaffagnini, S. Kinematics of ACL and anterolateral ligament. Part II: Anterolateral and anterior cruciate ligament reconstruction. Knee Surg. Sports Traumatol. Arthrosc. 2017, 25, 1062–1067. [Google Scholar] [CrossRef]
- Nitri, M.; Rasmussen, M.T.; Williams, B.T.; Moulton, S.G.; Cruz, R.S.; Dornan, G.J.; Goldsmith, M.T.; LaPrade, R.F. An In Vitro Robotic Assessment of the Anterolateral Ligament, Part 2: Anterolateral Ligament Reconstruction Combined with Anterior Cruciate Ligament Reconstruction. Am. J. Sports Med. 2016, 44, 593–601. [Google Scholar] [CrossRef]
- Helito, C.P.; Bonadio, M.B.; Gobbi, R.G.; da Mota E Albuquerque, R.F.; Pécora, J.R.; Camanho, G.L.; Demange, M.K. Com-bined Intra- and Extra-articular Reconstruction of the Anterior Cruciate Ligament: The Reconstruction of the Knee Anterol-ateral Ligament. Arthrosc Tech. 2015, 4, e239–e244. [Google Scholar] [CrossRef]
- Sonnery-Cottet, B.; Barbosa, N.C.; Tuteja, S.; Daggett, M.; Kajetanek, C.; Thaunat, M. Minimally invasive anterolateral liga-ment reconstruction in the setting of anterior cruciate ligament injury. Arthrosc. Tech. 2016, 5, e211–e215. [Google Scholar] [CrossRef]
- Smith, J.O.; Yasen, S.K.; Lord, B.; Wilson, A.J. Combined anterolateral ligament and anatomic anterior cruciate ligament reconstruction of the knee. Knee Surg. Sports Traumatol. Arthrosc. 2015, 23, 3151–3156. [Google Scholar] [CrossRef]
- Maestro Fernández, A.; Pipa Muñiz, I.; Rodríguez García, N. Two-Stage Anterior Cruciate Ligament Reconstruction Revision Surgery for Severe Bone Defects with Anterolateral Ligament Reconstruction Technique. Arthrosc. Tech. 2020, 9, e327–e337. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Sonnery-Cottet, B.; Thaunat, M.; Freychet, B.; Pupim, B.H.; Murphy, C.G.; Claes, S. Outcome of a Combined Anterior Cruciate Ligament and Anterolateral Ligament Reconstruction Technique with a Minimum 2-Year Follow-up. Am. J. Sports Med. 2015, 43, 1598–1605. [Google Scholar] [CrossRef] [PubMed]
- Zein, A.M.N.; Elshafie, M.; Elsaid, A.N.S.; Elrefai, M.A.E. Combined Anatomic Anterior Cruciate Ligament and Double Bundle Anterolateral Ligament Reconstruction. Arthrosc. Tech. 2017, 6, e1229–e1238. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Rosenstiel, N.; Praz, C.; Ouanezar, H.; Saithna, A.; Fournier, Y.; Hager, J.P.; Thaunat, M.; Sonnery-Cottet, B. Combined Anterior Cruciate and Anterolateral Ligament Reconstruction in the Professional Athlete: Clinical Outcomes from the Scientific Anterior Cruciate Ligament Network International Study Group in a Series of 70 Patients with a Minimum Follow-Up of 2 Years. Arthroscopy 2019, 35, 885–892. [Google Scholar] [PubMed] [Green Version]
- Runer, A.; Birkmaier, S.; Pamminger, M.; Reider, S.; Herbst, E.; Künzel, K.H.; Brenner, E.; Fink, C. The anterolateral ligament of the knee: A dissection study. Knee 2016, 23, 8–12. [Google Scholar] [CrossRef] [PubMed]
- Salmon, L.J.; Russell, V.J.; Refshauge, K.; Kader, D.; Connolly, C.; Linklater, J.; Pinczewski, L.A. Long-term outcome of endoscopic anterior cruciate ligament reconstruction with patellar tendon autograft: Minimum 13-year review. Am. J. Sports Med. 2006, 34, 721–732. [Google Scholar] [CrossRef]
- Pinczewski, L.A.; Lyman, J.; Salmon, L.J.; Russell, V.J.; Roe, J.; Linklater, J. A 10-year comparison of anterior cruciate ligament reconstructions with hamstring tendon and patellar tendon autograft: A controlled, prospective trial. Am. J. Sports Med. 2007, 35, 564–574. [Google Scholar] [CrossRef]
- Marrale, J.; Morrissey, M.C.; Haddad, F.S. A literature review of autograft and allograft anterior cruciate ligament reconstruction. Knee Surg. Sports Traumatol. Arthrosc. 2007, 15, 690–704. [Google Scholar] [CrossRef]
- Mistry, H.; Metcalfe, A.; Colquitt, J.; Loveman, E.; Smith, N.A.; Royle, P.; Waugh, N. Autograft or allograft for reconstruction of anterior cruciate ligament: A health economics perspective. Knee Surg. Sports Traumatol. Arthrosc. 2019, 27, 1782–1790. [Google Scholar] [CrossRef] [Green Version]
- Kim, S.G.; Kim, S.H.; Kim, J.G.; Jang, K.M.; Lim, H.C.; Bae, J.H. Hamstring autograft maturation is superior to tibialis allograft following anatomic single-bundle anterior cruciate ligament reconstruction. Knee Surg. Sports Traumatol. Arthrosc. 2018, 26, 1281–1287. [Google Scholar] [CrossRef]
- Yoo, S.H.; Song, E.K.; Shin, Y.R.; Kim, S.K.; Seon, J.K. Comparison of clinical outcomes and second-look arthroscopic findings after ACL reconstruction using a hamstring autograft or a tibialis allograft. Knee Surg. Sports Traumatol. Arthrosc. 2017, 25, 1290–1297. [Google Scholar] [CrossRef] [PubMed]


Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2022 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Lee, C.-S.; Han, S.-B.; Jang, K.-M. Combined Anterior Cruciate Ligament and Anterolateral Ligament Reconstruction Using a Single Achilles Tendon Allograft: A Technical Note. Medicina 2022, 58, 929. https://doi.org/10.3390/medicina58070929
Lee C-S, Han S-B, Jang K-M. Combined Anterior Cruciate Ligament and Anterolateral Ligament Reconstruction Using a Single Achilles Tendon Allograft: A Technical Note. Medicina. 2022; 58(7):929. https://doi.org/10.3390/medicina58070929
Chicago/Turabian StyleLee, Chul-Soo, Seung-Beom Han, and Ki-Mo Jang. 2022. "Combined Anterior Cruciate Ligament and Anterolateral Ligament Reconstruction Using a Single Achilles Tendon Allograft: A Technical Note" Medicina 58, no. 7: 929. https://doi.org/10.3390/medicina58070929






