Sociodemographic Determinants in Breast Cancer Screening among Uninsured Women of West Texas
Abstract
:1. Introduction
2. Materials and Methods
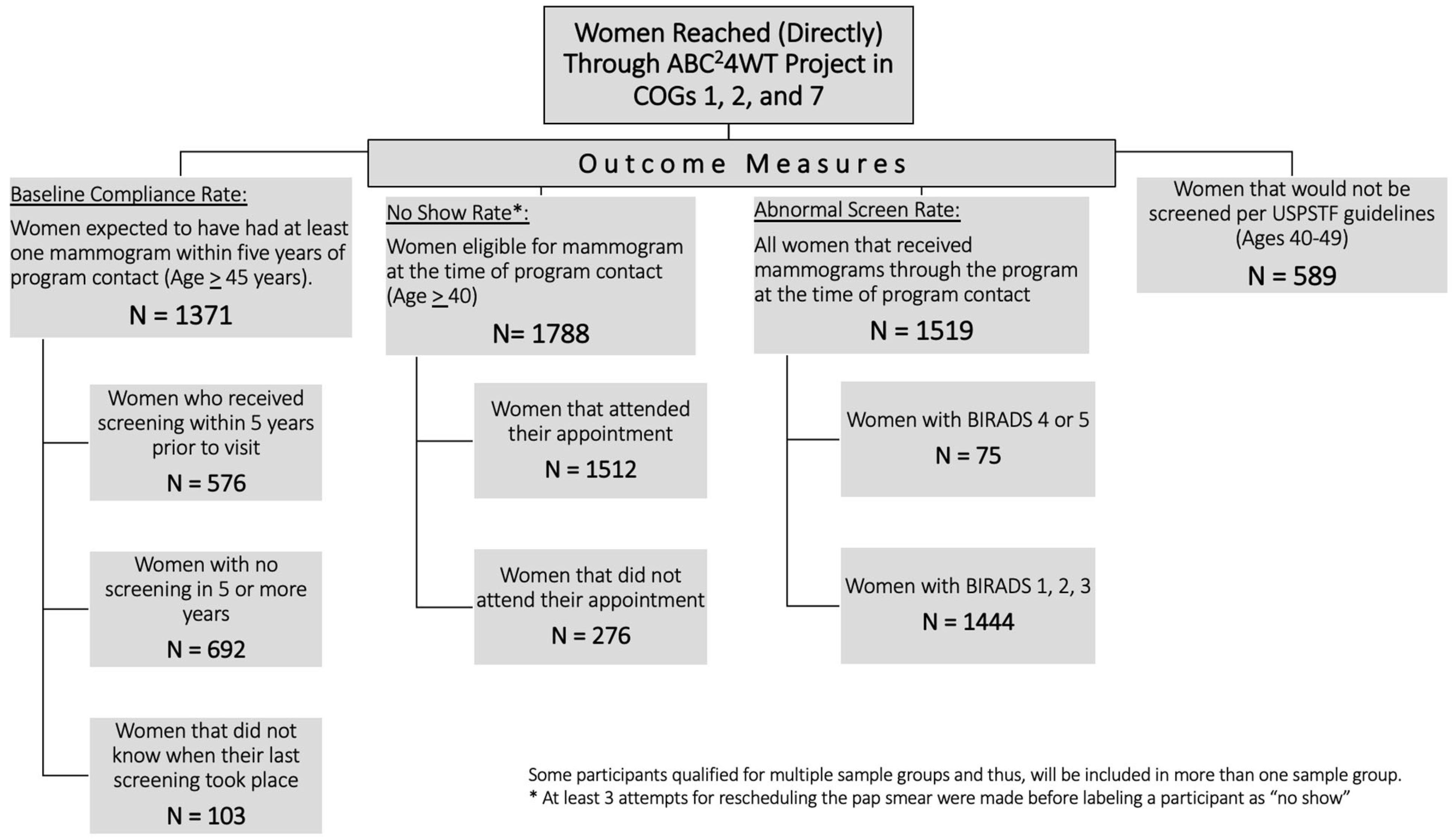
3. Results
3.1. Demographics
3.2. Baseline Non-Compliance Rate
3.3. “No-Show” Rate
3.4. Abnormal Mammograms
3.5. Women Who Would Not Have Been Screened per USPSTF (U.S. Preventative Task Force) Guidelines (Ages 40–49)
4. Discussion
5. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Conflicts of Interest
Abbreviations
| ABC4WT | Access to Breast Cancer Care for West Texas |
| AOR | Adjusted odds ratio; BI-RADS, Breast Imaging Reporting and Data System |
| BI-RADS | Breast Imaging Reporting and Data System |
| BRFSS | Behavioral Risk Factor Surveillance Survey |
| CI | Confidence interval |
| COG | Council of Government |
| CPRIT | Cancer Prevention and Research Institute of Texas |
| SD | Standard deviation |
| SPSS | Statistical Package for the Social Sciences |
| OR | Odds ratio |
| USPSTF | U.S. Preventative Services Task Force |
References
- Female Breast Cancer. Available online: http://seer.cancer.gov/statfacts/html/breast.html (accessed on 1 July 2022).
- Texas Cancer Registry SEER*Stat Database, 1995–2017 Incidence, Texas statewide, Created December 2019, Based on NPCR-CSS Submission, Cut-Off 11/7/2019. Available online: www.dshs.texas.gov/tcr (accessed on 30 September 2021).
- Registry, T.C. Age-Adjusted Cancer Mortality Rates by Council of Government in Texas, Female Breast, 2013–2018. 2021. Available online: http://cancer-rates.info/tx (accessed on 30 September 2021).
- Ahmad, A. Breast Cancer Statistics: Recent Trends. Adv. Exp. Med. Biol. 2019, 1152, 1–7. [Google Scholar] [CrossRef] [PubMed]
- Elmore, J.G. Review: Mammography screening reduces breast cancer mortality in women at average risk. Ann. Intern. Med. 2016, 164, JC26. [Google Scholar] [CrossRef] [PubMed]
- Gong, G.; Belasco, E.; A Hargrave, K.; Lyford, C.P.; Philips, B.U., Jr. Determinants of delayed detection of cancers in Texas Counties in the United States of America. Int. J. Equity Health 2012, 11, 29. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Roetzheim, R.G.; Pal, N.; Tennant, C.; Voti, L.; Ayanian, J.Z.; Schwabe, A.; Krischer, J.P. Effects of Health Insurance and Race on Early Detection of Cancer. J. Natl. Cancer Inst. 1999, 91, 1409–1415. [Google Scholar] [CrossRef] [Green Version]
- Leung, J.; McKenzie, S.; Martin, J.; McLaughlin, D. Effect of rurality on screening for breast cancer: A systematic review and meta-analysis comparing mammography. Rural Remote Health 2014, 14, 2730. [Google Scholar] [CrossRef]
- Halpern, M.T.; Ward, E.M.; Pavluck, A.L.; Schrag, N.M.; Bian, J.; Chen, A.Y. Association of insurance status and ethnicity with cancer stage at diagnosis for 12 cancer sites: A retrospective analysis. Lancet Oncol. 2008, 9, 222–231. [Google Scholar] [CrossRef]
- Yedjou, C.G.; Sims, J.N.; Miele, L.; Noubissi, F.; Lowe, L.; Fonseca, D.D.; Alo, R.A.; Payton, M.; Tchounwou, P.B. Health and Racial Disparity in Breast Cancer. Adv. Exp. Med. Biol. 2019, 1152, 31–49. [Google Scholar] [CrossRef]
- Freeman, H.P.; Chu, K.C. Determinants of Cancer Disparities: Barriers to Cancer Screening, Diagnosis, and Treatment. Surg. Oncol. Clin. North Am. 2005, 14, 655–669. [Google Scholar] [CrossRef]
- Freeman, H.P. Poverty, Culture, and Social Injustice: Determinants of Cancer Disparities. CA Cancer J. Clin. 2004, 54, 72–77. [Google Scholar] [CrossRef]
- Wheeler, S.B.; Reeder-Hayes, K.E.; Carey, L.A. Disparities in Breast Cancer Treatment and Outcomes: Biological, Social, and Health System Determinants and Opportunities for Research. Oncologist 2013, 18, 986–993. [Google Scholar] [CrossRef] [Green Version]
- Coll, P.P.; O’Connor, P.J.; Crabtree, B.F.; Besdine, R.W. Effects of Age, Education, and Physician Advice on Utilization of Screening Mammography. J. Am. Geriatr. Soc. 1989, 37, 957–962. [Google Scholar] [CrossRef]
- Katz, D.; Tengekyon, A.J.; Kahan, N.R.; Calderon-Margalit, R. Patient and physician characteristics affect adherence to screening mammography: A population-based cohort study. PLoS ONE 2018, 13, e0194409. [Google Scholar] [CrossRef] [Green Version]
- Freund, K.M.; Reisinger, S.A.; LeClair, A.M.; Yoon, G.H.; Al-Najar, S.M.; Young, G.S.; González, E.T.; Oliveri, J.M.; Paskett, E.D. Insurance Stability and Cancer Screening Behaviors. Health Equity 2019, 3, 177–182. [Google Scholar] [CrossRef] [Green Version]
- Texas Cancer Information. Available online: https://www.texascancer.info/scripts/mgwns.html (accessed on 9 February 2022).
- Monticciolo, D.L.; Newell, M.S.; Hendrick, R.E.; Helvie, M.A.; Moy, L.; Monsees, B.; Kopans, D.B.; Eby, P.; Sickles, E.A. Breast Cancer Screening for Average-Risk Women: Recommendations from the ACR Commission on Breast Imaging. J. Am. Coll. Radiol. 2017, 14, 1137–1143. [Google Scholar] [CrossRef]
- Office of the Federal Register NAaRA. 21 cfr i—Mammography quality standards act. In Title 42—the Public Health and Welfare; Office of the Federal Register, National Archives and Records Administration: Washington, DC, USA, 2011. [Google Scholar]
- Sickles, E.A.; D’Orsi, C.J.; Bassett, L.W. ACR BI-RADS® Mammography. In ACR BI-RADS® Atlas, Breast Imaging Reporting and Data System; American College of Radiology: Reston, VA, USA, 2013. [Google Scholar]
- Siu, A. Screening for Breast Cancer: U.S. Preventive Services Task Force Recommendation Statement. Ann. Intern. Med. 2016, 164, 279–296. [Google Scholar] [CrossRef] [Green Version]
- Weerakkody, Y.; Yap, J. Breast Imaging-Reporting and Data System (BI-RADS). Reference Article, Radiopaedia.org. Available online: https://radiopaedia.org/articles/breast-imaging-reporting-and-data-system-bi-rads?lang=us (accessed on 23 July 2022).
- Texas Department of Housing and Community Affairs, Urban and Rural Counties. 2020. Available online: https://www.tdhca.state.tx.us/htf/single-family/docs/20-UrbanRuralCounties.pdf (accessed on 9 February 2022).
- Davis, C.; Cadet, T.J.; Moore, M.; Darby, K. A Comparison of Compliance and Noncompliance in Breast Cancer Screening among African American Women. Health Soc. Work 2017, 42, 159–166. [Google Scholar] [CrossRef]
- Tangka, F.K.; Subramanian, S.; Mobley, L.R.; Hoover, S.; Wang, J.; Hall, I.J.; Singh, S.D. Racial and ethnic disparities among state Medicaid programs for breast cancer screening. Prev. Med. 2017, 102, 59–64. [Google Scholar] [CrossRef] [Green Version]
- Crump, S.R.; Mayberry, R.M.; Taylor, B.D.; Barefield, K.P.; Thomas, P.E. Factors related to noncompliance with screening mammogram appointments among low-income African-American women. J. Natl. Med. Assoc. 2000, 92, 237–246. [Google Scholar]
- Doescher, M.P.; Jackson, J.E. Trends in Cervical and Breast Cancer Screening Practices among Women in Rural and Urban Areas of the United States. J. Public Health Manag. Pract. 2009, 15, 200–209. [Google Scholar] [CrossRef] [Green Version]
- Akinlotan, M.; Bolin, J.; Helduser, J.; Ojinnaka, C.; Lichorad, A.; McClellan, D. Cervical Cancer Screening Barriers and Risk Factor Knowledge among Uninsured Women. J. Community Health 2017, 42, 770–778. [Google Scholar] [CrossRef] [Green Version]
- Coronado, G.D.; Thompson, B.; Koepsell, T.D.; Schwartz, S.M.; McLerran, D. Use of Pap test among Hispanics and non-Hispanic whites in a rural setting. Prev. Med. 2004, 38, 713–722. [Google Scholar] [CrossRef]
- Selvin, E.B.K. Breast and Cervical Cancer Screening: Sociodemographic Predictors among White, Black, and Hispanic women. Am. J. Public Health 2003, 93, 618–623. [Google Scholar] [CrossRef]
- Wells, K.J.; Roetzheim, R.G. Health disparities in receipt of screening mammography in Latinas: A critical review of recent literature. Cancer Control 2007, 14, 369–379. [Google Scholar] [CrossRef] [Green Version]
- Hensing, W.L.; Poplack, S.P.; Herman, C.R.; Sutcliffe, S.; Colditz, G.A.; Ademuyiwa, F.O. Racial differences in no-show rates for screening mammography. Cancer 2021, 127, 1857–1863. [Google Scholar] [CrossRef]
- Johnson, N.L.; Head, K.J.; Scott, S.F.; Zimet, G.D. Persistent Disparities in Cervical Cancer Screening Uptake: Knowledge and Sociodemographic Determinants of Papanicolaou and Human Papillomavirus Testing among Women in the United States. Public Health Rep. 2020, 135, 483–491. [Google Scholar] [CrossRef]
- Lehman, C.D.; Arao, R.F.; Sprague, B.L.; Lee, J.M.; Buist, D.S.M.; Kerlikowske, K.; Henderson, L.M.; Onega, T.; Tosteson, A.N.A.; Rauscher, G.H.; et al. National Performance Benchmarks for Modern Screening Digital Mammography: Update from the Breast Cancer Surveillance Consortium. Radiology 2017, 283, 49–58. [Google Scholar] [CrossRef]
- Olaku, O.O.; Taylor, E.A. Cancer in the Medically Underserved Population. Prim. Care: Clin. Off. Pract. 2017, 44, 87–97. [Google Scholar] [CrossRef] [Green Version]
- Thompson, B.; Hohl, S.D.; Molina, Y.; Paskett, E.D.; Fisher, J.L.; Baltic, R.D.; Washington, C.M. Breast Cancer Disparities among Women in Under-served Communities in the USA. Curr. Breast Cancer Rep. 2018, 10, 131–141. [Google Scholar] [CrossRef]
- Miles, R.C. Closing the Gap: Disparities in Breast Cancer Mortality among African American Women. Radiol. Imaging Cancer 2020, 2, e200124. [Google Scholar] [CrossRef]
- Gehlert, S.; Hudson, D.; Sacks, T. A Critical Theoretical Approach to Cancer Disparities: Breast Cancer and the Social Determinants of Health. Front. Public Health 2021, 9, 674736. [Google Scholar] [CrossRef]

| Characteristics | Mammogram Completed (Baseline Compliance) | p-Value | |||||||
|---|---|---|---|---|---|---|---|---|---|
| <5 years | ≥5 or Never | Don’t Know | Total Participants in Subgroup, N (%) | ||||||
| N | % | N | % | N | % | ||||
| Age (Years) | 40–49 | 200 | 39.8% | 265 | 52.7% | 38 | 7.6% | 503 (36.7%) | 0.774 |
| 50–59 | 255 | 43.3% | 289 | 49.1% | 45 | 7.6% | 589 (43.0%) | ||
| 60+ | 121 | 43.4% | 138 | 49.5% | 20 | 7.2% | 279 (20.4%) | ||
| Household Income (USD/month/person) | ≤800 | 350 | 41.8% | 425 | 50.7% | 63 | 7.5% | 838 (64.7%) | 0.853 |
| >800 | 193 | 42.1% | 227 | 49.6% | 38 | 8.3% | 458 (35.3%) | ||
| Settlement | Rural | 86 | 45.5% | 94 | 49.7% | 9 | 4.8% | 189 (13.8%) | 0.467 |
| Urban | 488 | 41.5% | 595 | 50.6% | 93 | 7.9% | 1176 (85.8%) | ||
| Other | 2 | 33.3% | 3 | 50.0% | 1 | 16.7% | 6 (0.4%) | ||
| Race | White | 165 | 41.9% | 200 | 50.8% | 29 | 7.4% | 394 (29.2%) | 0.991 |
| Black | 17 | 38.6% | 23 | 52.3% | 4 | 9.1% | 44 (3.3%) | ||
| Hispanic | 380 | 41.8% | 462 | 50.8% | 68 | 7.5% | 910 (67.5%) | ||
| Texas Region | COG-1 | 236 | 42.7% | 284 | 51.4% | 33 | 6.0% | 553 (40.3%) | 0.063 |
| COG-2 | 274 | 39.8% | 352 | 51.2% | 62 | 9.0% | 688 (50.2%) | ||
| COG-7 | 66 | 50.0% | 56 | 43.1% | 8 | 6.2% | 130 (9.5%) | ||
| Biopsy Results | Non-cancerous | 12 | 30.0% | 22 | 55.0% | 6 | 15.0% | 40 (61.5%) | 0.028 |
| Cancerous | 12 | 48.0% | 13 | 52.0% | 0 | 0.0% | 25 (38.5%) | ||
| Characteristics | “No-Show” for Mammogram Appointments | p-Value | |||
|---|---|---|---|---|---|
| N | % | Total Participants in Subgroup, N (%) | |||
| Age (Years) | 40–49 | 148 | 16.1% | 920 (51.5%) | 0.602 |
| 50–59 | 90 | 15.3% | 589 (32.9%) | ||
| 60+ | 38 | 13.6% | 279 (15.6%) | ||
| Household Income (USD/month/person) | ≤800 | 177 | 15.5% | 1144 (67.4%) | 0.293 |
| >800 | 75 | 13.5% | 554 (32.6%) | ||
| Settlement | Rural | 37 | 15.2% | 244 (13.6%) | 0.571 |
| Urban | 239 | 15.5% | 1538 (86.0%) | ||
| Other | 0 | 0.0% | 6 (0.3%) | ||
| Race | White | 67 | 13.7% | 490 (27.4%) | 0.148 |
| Black | 6 | 9.4% | 64 (3.6%) | ||
| Hispanic | 198 | 16.4% | 1208 (67.6%) | ||
| Texas Region | COG-1 | 179 | 24.2% | 740 (41.4%) | <0.001 |
| COG-2 | 93 | 10.5% | 885 (49.5%) | ||
| COG-7 | 4 | 2.5% | 163 (9.1%) | ||
| Characteristics | Mammogram Outcomes | p-Value | |||||||
|---|---|---|---|---|---|---|---|---|---|
| BI-RADS 1–3 | BI-RADS 4 | BI-RADS 5 | Total Participants in Subgroup, N (%) | ||||||
| N | % | N | % | N | % | ||||
| Age (Years) | <40 | 72 | 91.1% | 3 | 3.8% | 4 | 5.1% | 79 (5.2%) | 0.049 |
| 40–49 | 715 | 96.2% | 21 | 2.8% | 7 | 0.9% | 743 (48.9%) | ||
| 50–59 | 448 | 95.1% | 16 | 3.4% | 7 | 1.5% | 459 (31.0%) | ||
| 60+ | 209 | 92.5% | 10 | 4.4% | 7 | 3.1% | 218 (14.7%) | ||
| Household Income (USD/month/person) | ≤800 | 950 | 95.2% | 30 | 3.0% | 18 | 1.8% | 998 (67.6%) | 0.468 |
| >800 | 453 | 94.8% | 19 | 4.0% | 6 | 1.3% | 478 (32.4%) | ||
| Settlement | Rural | 203 | 95.8% | 5 | 2.4% | 4 | 1.9% | 212 (14.0%) | 0.897 |
| Urban | 1234 | 94.9% | 45 | 3.5% | 21 | 1.6% | 1300 (85.6%) | ||
| Other | 6 | 100.0% | 0 | 0.0% | 0 | 0.0% | 6 (0.4%) | ||
| Race | White | 401 | 94.4% | 13 | 3.1% | 11 | 2.6% | 425 (28.4%) | 0.366 |
| Black | 56 | 94.8% | 3 | 5.2% | 0 | 0.0% | 59 (3.9%) | ||
| Hispanic | 965 | 95.4% | 33 | 3.3% | 14 | 1.4% | 1012 (67.6%) | ||
| Texas Region | COG-1 | 526 | 96.2% | 16 | 2.9% | 5 | 0.9% | 547 (36.0%) | 0.392 |
| COG-2 | 761 | 94.3% | 30 | 3.7% | 16 | 2.0% | 807 (53.1%) | ||
| COG-7 | 157 | 95.2% | 4 | 2.4% | 4 | 2.4% | 165 (10.9%) | ||
| Characteristics | Women Eligible per ACS Guideline AND Ineligible per USPSTF (Women Aged 40–49 Years) | p-Value | |||
|---|---|---|---|---|---|
| N | % | Total Participants in Subgroup, N (%) | |||
| Mammography Outcome | BI-RADS 1, 2, 3 | 715 | 49.5% | 1443 (95.1%) | 0.040 |
| BI-RADS 4 or 5 | 28 | 37.3% | 75 (4.9%) | ||
| Biopsy Result | Non-cancerous | 35 | 51.5% | 68 (66.0%) | 0.026 |
| Cancer | 10 | 28.6% | 35 (34.0%) | ||
| Household Income (USD/month/person) | ≤800 | 644 | 48.7% | 1323 (68.0%) | <0.001 |
| >800 | 232 | 37.2% | 623 (32.0%) | ||
| Settlement | Rural | 136 | 48.4% | 281 (13.6%) | 0.272 |
| Urban | 782 | 44.0% | 1776 (86.0%) | ||
| Other | 2 | 28.6% | 7 (0.3%) | ||
| Race | White | 213 | 36.3% | 587 (28.9%) | <0.001 |
| Black | 35 | 38.0% | 92 (4.5%) | ||
| Hispanic | 661 | 48.9% | 1351 (66.6%) | ||
| Texas Region * | COG-1 | 363 | 41.5% | 874 (42.3%) | <0.001 |
| COG-2 | 493 | 50.3% | 981 (47.5%) | ||
| COG-7 | 64 | 30.5% | 210 (10.2%) | ||
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2022 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Jensen, B.; Khan, H.; Layeequr Rahman, R. Sociodemographic Determinants in Breast Cancer Screening among Uninsured Women of West Texas. Medicina 2022, 58, 1010. https://doi.org/10.3390/medicina58081010
Jensen B, Khan H, Layeequr Rahman R. Sociodemographic Determinants in Breast Cancer Screening among Uninsured Women of West Texas. Medicina. 2022; 58(8):1010. https://doi.org/10.3390/medicina58081010
Chicago/Turabian StyleJensen, Brooke, Hafiz Khan, and Rakhshanda Layeequr Rahman. 2022. "Sociodemographic Determinants in Breast Cancer Screening among Uninsured Women of West Texas" Medicina 58, no. 8: 1010. https://doi.org/10.3390/medicina58081010
APA StyleJensen, B., Khan, H., & Layeequr Rahman, R. (2022). Sociodemographic Determinants in Breast Cancer Screening among Uninsured Women of West Texas. Medicina, 58(8), 1010. https://doi.org/10.3390/medicina58081010





