The Impact of COVID-19 Lockdowns in a Sample of Outpatients in a Mental Health Department of a Metropolitan Hospital in Milan
Abstract
:1. Introduction
2. Materials and Methods
2.1. Participants and Procedures
2.2. Survey Instrument
2.3. Statistical Analysis
3. Results
3.1. Participant Characteristics
3.2. Results of the Clinical and Stress Scales
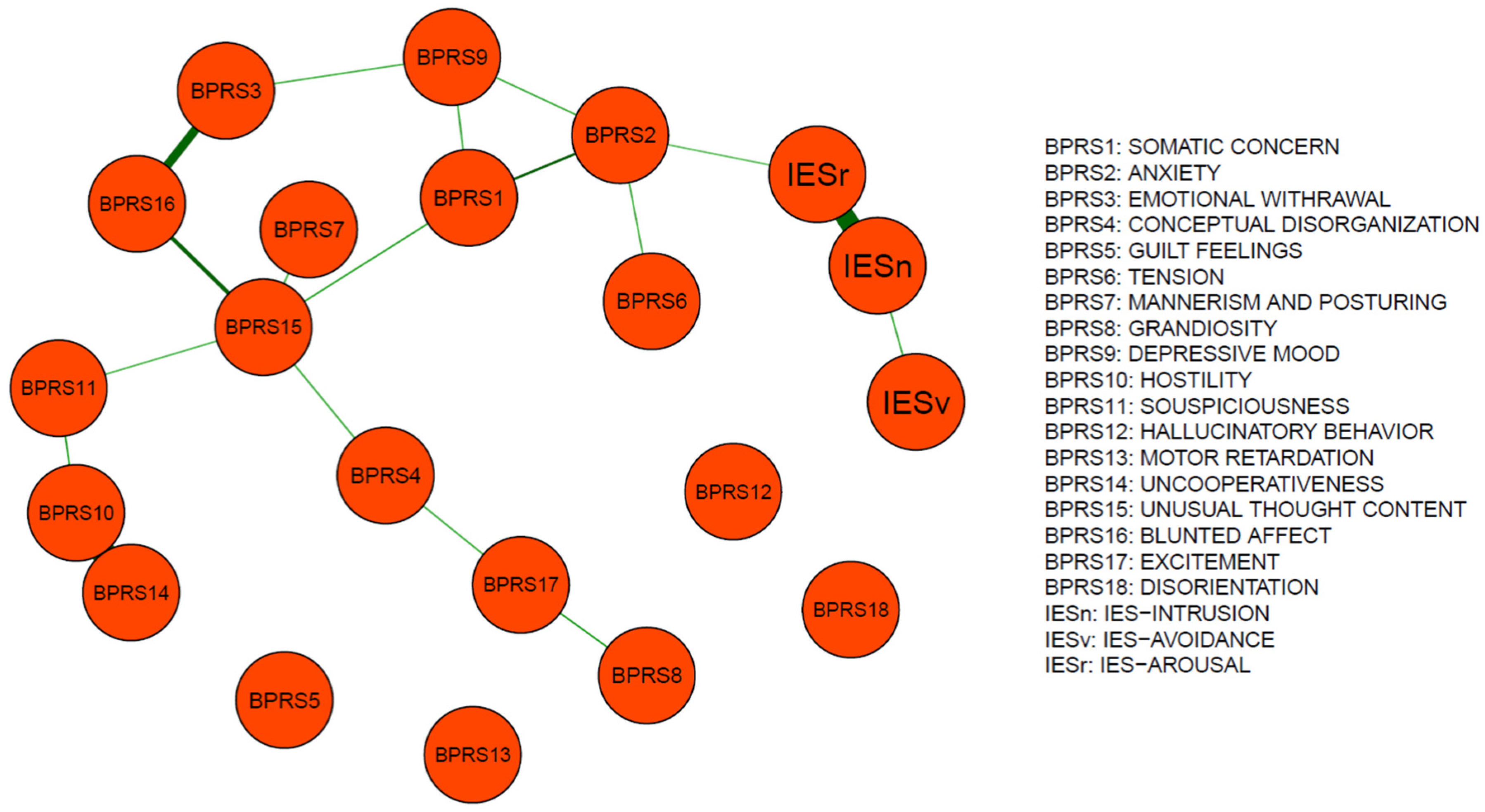
3.3. Network Analysis
4. Discussion
5. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Conflicts of Interest
References
- Luo, M.; Guo, L.; Yu, M.; Jiang, W.; Wang, H. The psychological and mental health impact of coronavirus disease 2019 (COVID-19) on medical staff and general public—A systematic review and meta-analysis. Psychiatry Res. 2020, 291, 113190. [Google Scholar] [CrossRef] [PubMed]
- World Health Organisation. Statement on the Second Meeting of the International Health Regulations (2005) Emergency Committee Regarding the Outbreak of Novel Coronavirus (2019-nCov). 30 January 2020. Available online: https://www.who.int/news/item/30-01-2020-statement-on-the-second-meeting-of-the-international-health-regulations-(2005)-emergency-committee-regarding-the-outbreak-of-novel-coronavirus-(2019-ncov) (accessed on 14 February 2021).
- World Health Organisation. WHO Director-General’s Opening Remarks at the Media Briefing on COVID-19. 11 March 2020. Available online: https://www.who.int/director-general/speeches/detail/who-director-general-s-opening-remarks-at-the-media-briefing-on-covid-19---11-march-2020 (accessed on 14 February 2021).
- Holmes, E.A.; O’Connor, R.C.; Perry, V.H.; Tracey, I.; Wessely, S.; Arseneault, L.; Ballard, C.; Christensen, H.; Cohen Silver, R.; Everall, I.; et al. Multidisciplinary research priorities for the COVID-19 pandemic: A call for action for mental health science. Lancet Psychiatry 2020, 7, 547–560. [Google Scholar] [CrossRef]
- Ballard, M.; Bancroft, E.; Nesbit, J.; Johnson, A.; Holeman, I.; Foth, J.; Rogers, D.; Yang, J.; Nardella, J.; Olsen, H.; et al. Prioritising the role of the community health workers in the COVID-19 response. BMJ Glob. Health 2020, 5, e002550. [Google Scholar] [CrossRef] [PubMed]
- Franklin, P.; Gkiouleka, A. A scoping review of psychosocial risk to health woorkers during the COVID-19 pandemic. Int. J. Environ. Res. Public Health 2021, 18, 2453. [Google Scholar] [CrossRef] [PubMed]
- Ranieri, J.; Guerra, F.; Perilli, E.; Passafiume, D.; Maccarone, D.; Ferri, C.; Di Giacomo, D. Prolonged COVID-19 outbreak and psychological response of nurses in Italian Healthcare System: Cross-sectional study. Front. Psychol. 2021, 12, 608413. [Google Scholar] [CrossRef]
- Mazza, C.; Ricci, E.; Biondi, S.; Colasanti, M.; Ferracuti, S.; Napoli, C.; Roma, P. A Nationwide Survey of Psychological Distress among Italian People during the COVID-19 Pandemic: Immediate Psychological Responses and Associated Factors. Int. J. Environ. Res. Public Health 2020, 17, 3165. [Google Scholar] [CrossRef]
- Moccia, L.; Janiri, D.; Pepe, M.; Dattoli, L.; Molinaro, M.; De Martin, V.; Chieffo, D.; Janiri, L.; Fiorillo, A.; Sani, G.; et al. Affective temperament, attachment style, and the psychological impact of the COVID-19 outbreak: An early report on the Italian general population. Brain Behav. Immun. 2020, 87, 75–79. [Google Scholar] [CrossRef]
- Tommasi, M.; Toro, F.; Arnò, S.; Carrieri, A.; Conte, M.M.; Devastato, M.D.; Picconi, L.; Sergi, M.R.; Saggino, A. Physical and Psychological Impact of the Phase One Lockdown for COVID-19 on Italians. Front. Psychol. 2020, 11, 563722. [Google Scholar] [CrossRef]
- Rossi, R.; Socci, V.; Talevi, D.; Mensi, S.; Niolu, C.; Pacitti, F.; Di Marco, A.; Rossi, A.; Siracusano, A.; Di Lorenzo, G. COVID-19 Pandemic and Lockdown Measures Impact on Mental Health Among the General Population in Italy. Front. Psychiatry 2020, 11, 790. [Google Scholar] [CrossRef]
- Bonichini, S.; Tremolada, M. Quality of life and symptoms of PTSD during the COVID-19 lockdown in Italy. Int. J. Environ. Res. Public Health 2021, 18, 4385. [Google Scholar] [CrossRef]
- Porcellana, M.; Morganti, C.; Boccalari, L.; Limosani, I.; Manzo, V.; Zerbinati, L.; Corradin, M.; Moreno, M.; Percudani, M. The impact of the COVID-19 emergency in a community mental health setting of a metropolitan hospital. J. Psychopathol. 2020, 26, 134–140. [Google Scholar]
- Guy, W. ECDEU Assessment Manual for Psychopharmacology; US Department of Health and Welfare: Washington, DC, USA, 1976; pp. 534–537. [Google Scholar]
- Overall, J.E. The Brief Psychiatric Rating Scale in psychopharmacology research. In Psychological Measurements in Psychopharmacology; Pichot, P., Olivier-Martin, R., Eds.; S. Karger AG: Basel, Switzerland, 1974; pp. 67–78. [Google Scholar]
- Morosini, P.; Rancone, R.; Impallomeni, M.; Marola, V.; Casacchia, M. Presentazione dell’adattamento italiano della Brief Psychiatric Rating Scale. Riv. Riabil. Psichiatr. Psicosoc. 1995, 1, 48–54. [Google Scholar]
- Weiss, D.S.; Marmar, C.R. The impact of event scale-revised. In Assessing Psychological Trauma and PTSD; Wilson, J.P., Keane, T.M., Eds.; Guilford Press: New York, NY, USA, 1997; pp. 399–411. [Google Scholar]
- Pietrantonio, F.; De Gennaro, L.; Di Paolo, M.C.; Solano, L. The Impact of Event Scale: Validation of an Italian version. J. Psychosom. Res. 2003, 55, 389–393. [Google Scholar] [CrossRef]
- Borsboom, D.; Cramer, A.O. Network analysis: An integrative approach to the structure of psychopathology. Annu. Rev. Clin. Psychol. 2013, 9, 91–121. [Google Scholar] [CrossRef]
- Epskamp, S.; Cramer, A.O.J.; Waldorp, L.J.; Schmittmann, V.D.; Borsboom, D. Qgraph: Network Visualizations of Relationships in Psychometric Data. J. Stat. Softw. 2012, 48, 1–18. [Google Scholar] [CrossRef]
- Friedman, J.; Hastie, T.; Tibshirani, R. Sparse inverse covariance estimation with the graphical lasso. Biostatistics 2008, 9, 432–441. [Google Scholar] [CrossRef]
- Moradian, S.; Bauerle, A.; Schweda, A.; Musche, V.; Kohler, H.; Fink, M.; Weismuller, B.; Benecke, A.V.; Dorrie, N.; Skoda, E.M.; et al. Differences and simililarities between the impact of the first and the second COVID-19-lockdown on mental health and safety behaviour in Germany. J. Public Health 2021, 43, 710–713. [Google Scholar] [CrossRef]
- Brooks, S.K.; Webster, R.K.; Smith, L.E.; Woodland, L.; Wessely, S.; Greenberg, N.; Rubin, G.J. The psychological impact of quarantine and how to reduce it: Rapid review of the evidence. Lancet 2020, 395, 912–920. [Google Scholar] [CrossRef]
- Smith, K.; Ostinelli, E.; Cipriani, A. COVID-19 and mental health: A transformational opportunity to apply an evidence-based approach to clinical practice and research. Evid. Based Ment. Health 2020, 23, 45–46. [Google Scholar] [CrossRef]
- Zhu, Y.; Chen, L.; Ji, H.; Xi, M.; Fang, Y.; Li, Y. The risk and prevention of novel coronavirus pneumonia infections among inpatients in psychiatric hospitals. Neurosci. Bull. 2020, 36, 299–302. [Google Scholar] [CrossRef]
- Bedford, J.; Enria, D.; Giesecke, J.; Heymann, D.L.; Ihekweazu, C.; Kobinger, G.; Lane, H.C.; Memish, Z.; Oh, M.D.; Sall, A.A.; et al. WHO Strategic and Technical Advisory Group for Infectious Hazards. COVID-19: Towards controlling of a pandemic. Lancet 2020, 395, 1015–1018. [Google Scholar] [CrossRef]
- Percudani, M.; Corradin, M.; Moreno, M.; Indelicato, A.; Vita, A. Mental health service in Lombardy during COVID-19 outbreak. Psychiatry Res. 2020, 288, 112980. [Google Scholar] [CrossRef] [PubMed]
- Liu, T.B.; Chen, X.Y.; Miao, G.D. Recommendations on diagnostic criteria and prevention of SARS-related mental disorders. J. Clin. Psychol. Med. 2003, 13, 188–191. [Google Scholar]
- Maunder, R.; Hunter, J.; Vincent, L.; Bennett, J.; Peladeau, N.; Leszcz, M.; Sadavoy, J.; Verhaeghe, L.M.; Steinberg, R.; Mazzulli, T. The immediate psychological and occupational impact of the 2003 SARS outbreak in a teaching hospital. CMAJ 2003, 168, 1245–1251. [Google Scholar]
- Bäuerle, A.; Teufel, M.; Musche, V.; Weismüller, B.; Kohler, H.; Hetkamp, M.; Dörrie, N.; Schweda, A.; Skoda, E.M. Increased generalized anxiety, depression and distress during the COVID-19 pandemic: A cross-sectional study in Germany. J. Public Health 2020, 42, 672–678. [Google Scholar] [CrossRef]
- Petzold, M.B.; Bendau, A.; Plag, J.; Pyrkosch, L.; Mascarell Maricic, L.; Betzler, F.; Rogoll, J.; Große, J.; Ströhle, A. Risk, resilience, psychological distress, and anxiety at the beginning of the COVID-19 pandemic in Germany. Brain Behav. 2020, 10, e01745. [Google Scholar] [CrossRef]
- Wu, T.; Jia, X.; Shi, H.; Niu, J.; Yin, X.; Xie, J.; Wang, X. Prevalence of mental health problems during the COVID-19 pandemic: A systematic review and meta-analysis. J. Affect. Disord. 2021, 281, 91–98. [Google Scholar] [CrossRef]
- Ettman, C.K.; Abdalla, S.M.; Cohen, G.H.; Sampson, L.; Vivier, P.M.; Galea, S. Prevalence of Depression Symptoms in US Adults Before and During the COVID-19 Pandemic. JAMA Netw. Open 2020, 3, e2019686. [Google Scholar] [CrossRef]
- Talevi, D.; Socci, V.; Carai, M.; Carnaghi, G.; Faleri, S.; Trebbi, E.; di Bernardo, A.; Capelli, F.; Pacitti, F. Mental health outcomes of the COVID-19 pandemic. Riv. Psichiatr. 2020, 55, 137–144. [Google Scholar] [CrossRef]
- World Health Organisation; Regional Office for Europe. Pandemic Fatigue: Reinvigorating the Public to Prevent COVID-19: Policy, Considerations for the Member States in the WHO European Region; WHO; Regional Office for Europe: Copenhagen, Denmark, 2020. [Google Scholar]
- Compean, E.; Hamner, M. Posttraumatic Stress Disorder with secondary psychotic features (PTSD-SP): Diagnostic and treatment challenges. Prog. Neuropsychopharmacol. Biol. Psychiatry 2019, 88, 265–275. [Google Scholar] [CrossRef]
- Yang, Y.; Li, W.; Zhang, Q.; Zhang, L.; Cheung, T.; Xiang, Y.T. Mental health services for older adults in China during the COVID-19 outbreak. Lancet Psychiatry 2020, 7, e19. [Google Scholar] [CrossRef]
- Starace, F.; Ferrara, M.; on behalf of the Italian Society of Epidemiological Psychiatry (SIEP) Board Members. COVID-19 disease emergency operational instructions for Mental health departments issued by the Italian Society of Epidemiological Psychiatry. Epidemiol. Psychiatr. Sci. 2020, 29, e116. [Google Scholar] [CrossRef] [PubMed] [Green Version]



| April (n = 116) | November (n = 116) | ||||
|---|---|---|---|---|---|
| Age | 50.68 ± 11.59 | 51.39 ± 11.97 | t = −0.47, df = 250, p > 0.05, Cohen’s d = −0.05 | ||
| Civil Status | |||||
| unmarried | 66 | 52.4% | 66 | 52.4% | χ2 = 2.82, df = 3, p > 0.05 |
| married | 35 | 27.8% | 41 | 32.5% | |
| separated/divorced | 23 | 18.3% | 15 | 11.9% | |
| widowed | 2 | 1.6% | 4 | 3.2% | |
| Education | |||||
| primary | 2 | 1.6% | 2 | 1.6% | χ2 = 7.72, df = 3, p > 0.05 |
| middle | 32 | 25.4% | 42 | 33.3% | |
| high school | 63 | 50.0% | 69 | 54.8% | |
| graduate/postgraduate | 29 | 23.0% | 13 | 10.3% | |
| Living Situation | |||||
| alone | 47 | 37.3% | 39 | 31.0% | χ2 = 1.54, df = 3, p > 0.05 |
| partner | 51 | 40.5% | 52 | 41.3% | |
| relatives | 23 | 18.3% | 29 | 23.0% | |
| other | 5 | 4.0% | 6 | 4.8% | |
| Work Status | |||||
| unemployed | 16 | 12.7% | 20 | 15.9% | χ2 = 9.83, df = 3, p < 0.05 |
| employed | 65 | 51.6% | 54 | 42.9% | |
| retired | 7 | 5.6% | 16 | 12.7% | |
| student/housewife | 9 | 7.1% | 2 | 1.6% | |
| invalid | 29 | 23.0% | 34 | 27.0% | |
| Psychiatric Diagnosis | |||||
| schizophrenia | 38 | 30.2% | 43 | 34.1% | χ2 = 7.93, df = 4, p > 0.05 |
| bipolar disorder | 33 | 26.2% | 19 | 15.1% | |
| depressive disorder | 22 | 17.5% | 24 | 19.0% | |
| anxiety disorder | 3 | 2.4% | 10 | 7.9% | |
| personality disorder | 30 | 23.8% | 30 | 23.8% | |
| April | November | Statistics | |
|---|---|---|---|
| CGI-S | 3.38 ± 0.90 | 3.83 ± 0.72 | t = −4.39, df = 250, p < 0.001,Cohen’s d = −0.55 |
| IES-R Intrusion | 11.31 ± 6.24 | 11.89 ± 6.50 | t = −0.71, df = 249, p > 0.05, Cohen’s d = −0.09 |
| IES-R Avoidance | 10.9 ± 6.68 | 10.72 ± 6.02 | t = 0.22, df = 249, p > 0.05, Cohen’s d = 0.02 |
| IES-R Arousal | 9.32 ± 5.37 | 9.18 ± 5.18 | t = 0.21, df = 249, p > 0.05, Cohen’s d = 0.02 |
| IES-R Total score | 31.44 ± 15.44 | 31.7 ± 14.67 | t = −0.14, df = 249, p > 0.05, Cohen’s d = −0.01 |
| PTSD cases | |||
| Cases (IES-R < 33) | 61 52.6% | 58 50.0% | χ2 = 0.15, df = 1, p > 0.05 |
| Cases (IES-R ≥ 33) | 55 47.4% | 58 50.0% | |
| BPRS Total | 37.69 ± 8.36 | 40.84 ± 10.28 | t = −2.65, df = 248, p < 0.01, Cohen’s d = −0.33 |
| Somatic Concern | Anxiety | Emotional Withdrawal | Conceptual Disorganization | Guilt Feelings | Tension | Mannerism And.Posturing | Grandiosity | Depressive Mood | Hostility | Suspiciousness | Hallucinatory Behavior | Motor Retardation | Uncooperativeness | Unusual Thought Content | Blunted Affect | Excitement | Disorientation | IES-INTRUSION | IES-AVOIDANCE | IES-AROUSAL | |
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
| Somatic Concern | 0.34 | 0.29 | 0.29 | ||||||||||||||||||
| Anxiety | 0.34 | 0.25 | 0.25 | 0.2 | |||||||||||||||||
| Emotional Withdrawal | 0.24 | 0.41 | |||||||||||||||||||
| Conceptual Disorganization | 0.27 | 0.25 | |||||||||||||||||||
| Guilt Feelings | |||||||||||||||||||||
| Tension | 0.25 | ||||||||||||||||||||
| Mannerism And Posturing | 0.27 | ||||||||||||||||||||
| Grandiosity | 0.3 | ||||||||||||||||||||
| Depressive Mood | 0.29 | 0.25 | 0.24 | ||||||||||||||||||
| Hostility | 0.32 | 0.58 | |||||||||||||||||||
| Suspiciousness | 0.32 | 0.23 | |||||||||||||||||||
| Hallucinatory Behavior | |||||||||||||||||||||
| Motor Retardation | |||||||||||||||||||||
| Uncooperativeness | 0.58 | ||||||||||||||||||||
| Unusual Thought Content | 0.29 | 0.27 | 0.27 | 0.23 | 0.36 | ||||||||||||||||
| Blunted Affect | 0.41 | 0.36 | |||||||||||||||||||
| Excitement | 0.25 | 0.3 | |||||||||||||||||||
| Disorientation | |||||||||||||||||||||
| IES-INTRUSION | 0.27 | 0.53 | |||||||||||||||||||
| IES-AVOIDANCE | 0.27 | ||||||||||||||||||||
| IES-AROUSAL | 0.2 | 0.53 |
| Somatic Concern | Anxiety | Emotional Withdrawal | Conceptual Disorganization | Guilt Feelings | Tension | Mannerism and Posturing | Grandiosity | Depressive Mood | Hostility | Suspiciousness | Hallucinatory Behavior | Motor Retardation | Uncooperativeness | Unusual Thought Content | Blunted Affect | Excitement | Disorientation | IES-INTRUSION | IES-AVOIDANCE | IES-AROUSAL | |
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
| Somatic Concern | 0.35 | 0.24 | |||||||||||||||||||
| Anxiety | 0.35 | ||||||||||||||||||||
| Emotional Withdrawal | 0.29 | 0.21 | 0.28 | ||||||||||||||||||
| Conceptual Disorganization | 0.29 | 0.23 | 0.4 | ||||||||||||||||||
| Guilt Feelings | |||||||||||||||||||||
| Tension | |||||||||||||||||||||
| Mannerism and Posturing | 0.23 | ||||||||||||||||||||
| Grandiosity | 0.51 | ||||||||||||||||||||
| Depressive Mood | 0.24 | 0.21 | 0.23 | ||||||||||||||||||
| Hostility | 0.42 | 0.3 | |||||||||||||||||||
| Suspiciousness | 0.42 | 0.35 | |||||||||||||||||||
| Hallucinatory Behavior | 0.35 | ||||||||||||||||||||
| Motor Retardation | |||||||||||||||||||||
| Uncooperativeness | 0.3 | ||||||||||||||||||||
| Unusual Thought Content | 0.4 | ||||||||||||||||||||
| Blunted Affect | 0.28 | 0.23 | |||||||||||||||||||
| Excitement | 0.51 | ||||||||||||||||||||
| Disorientation | |||||||||||||||||||||
| IES-INTRUSION | 0.62 | ||||||||||||||||||||
| IES-AVOIDANCE | |||||||||||||||||||||
| IES-AROUSAL | 0.62 |
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2022 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Percudani, M.; Porcellana, M.; Di Bernardo, I.; Limosani, I.; Negri, A.; Zerbinati, L.; Morganti, C. The Impact of COVID-19 Lockdowns in a Sample of Outpatients in a Mental Health Department of a Metropolitan Hospital in Milan. Medicina 2022, 58, 1274. https://doi.org/10.3390/medicina58091274
Percudani M, Porcellana M, Di Bernardo I, Limosani I, Negri A, Zerbinati L, Morganti C. The Impact of COVID-19 Lockdowns in a Sample of Outpatients in a Mental Health Department of a Metropolitan Hospital in Milan. Medicina. 2022; 58(9):1274. https://doi.org/10.3390/medicina58091274
Chicago/Turabian StylePercudani, Mauro, Matteo Porcellana, Ilaria Di Bernardo, Ivan Limosani, Attilio Negri, Luigi Zerbinati, and Carla Morganti. 2022. "The Impact of COVID-19 Lockdowns in a Sample of Outpatients in a Mental Health Department of a Metropolitan Hospital in Milan" Medicina 58, no. 9: 1274. https://doi.org/10.3390/medicina58091274





