Comparative Efficacy of Traditional Corticotomy and Flapless Piezotomy in Facilitating Orthodontic Tooth Movement: A Systematic Review and Meta-Analysis
Abstract
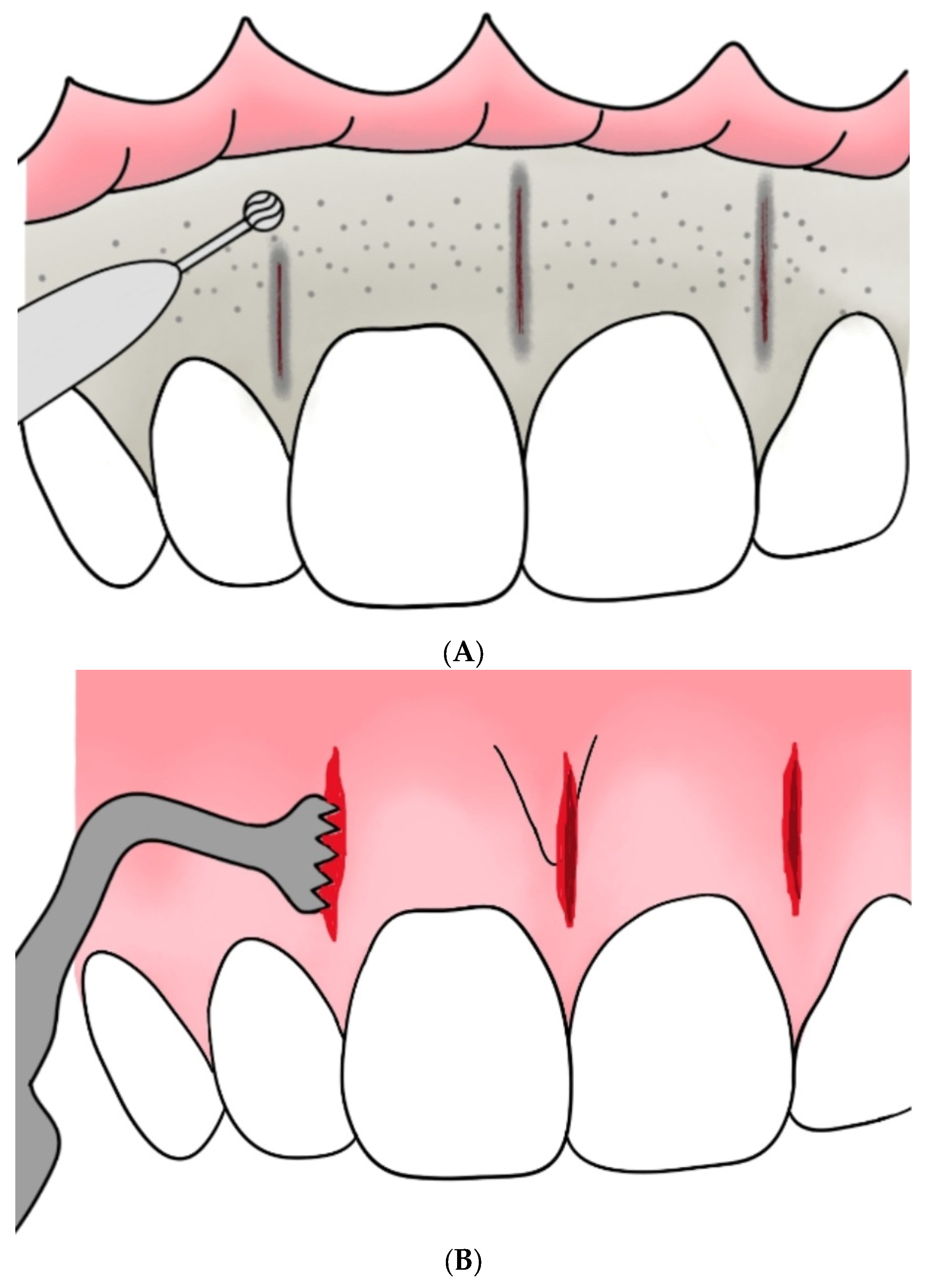
:1. Introduction
2. Materials and Methods
2.1. Protocol and Registration
2.2. Eligibility Criteria
2.3. Information Sources and Search Strategy
2.4. Study Selection and Data Extraction
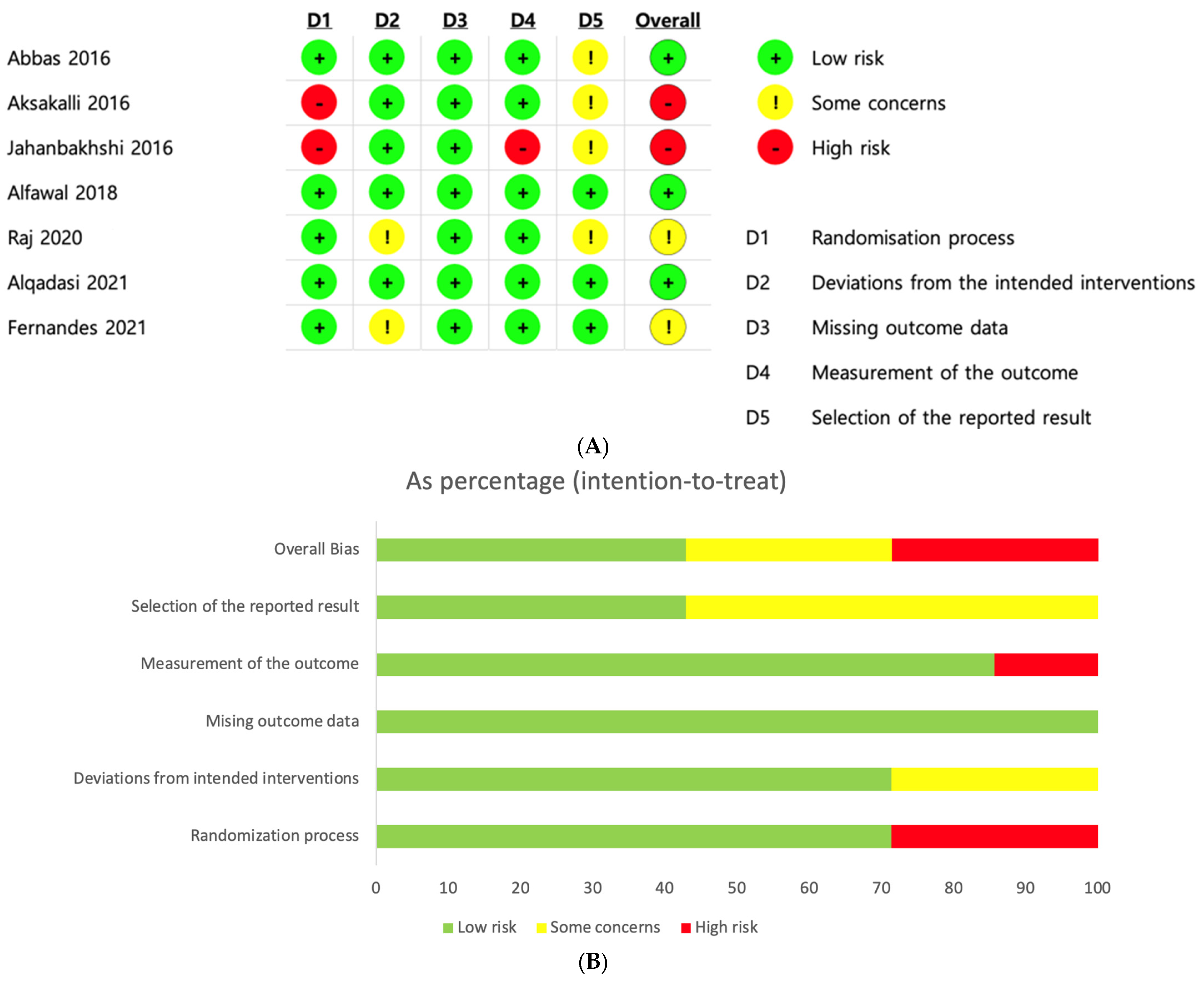
2.5. Risk of Bias Assessment
2.6. Data Synthesis and Analysis
3. Results
3.1. Study Selection
3.2. Risk of Bias Assessment
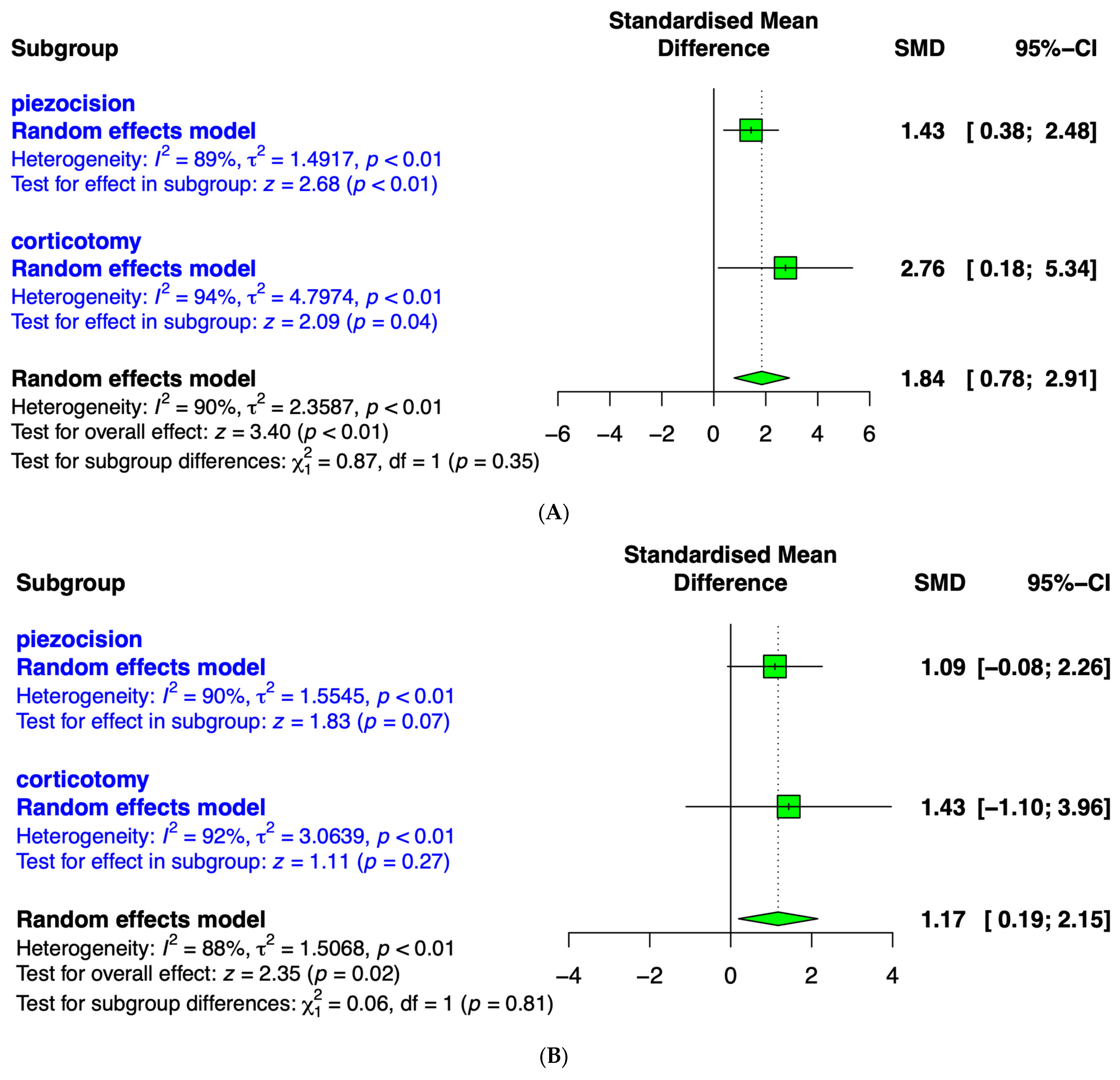
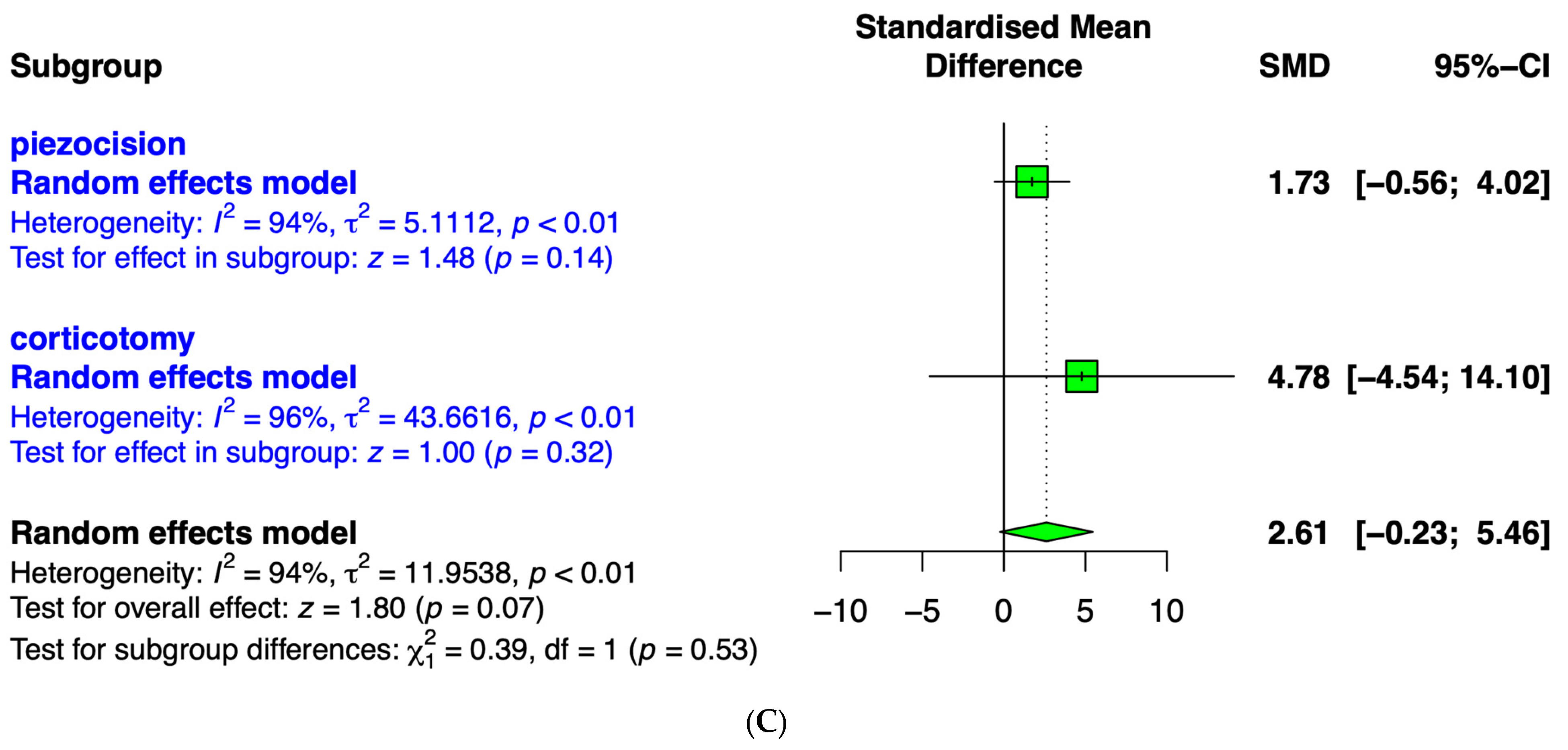
3.3. Meta-Analysis
3.4. Comparison between Piezocision and Corticotomy
3.5. Canine Retraction after 1 Month
3.6. Canine Retraction after 2 Months
3.7. Canine Retraction after 3 Months
4. Discussion
5. Conclusions
Supplementary Materials
Author Contributions
Funding
Data Availability Statement
Conflicts of Interest
References
- Rosvall, M.D.; Fields, H.W.; Ziuchkovski, J.; Rosenstiel, S.F.; Johnston, W.M. Attractiveness, acceptability, and value of orthodontic appliances. Am. J. Orthod. Dentofac. Orthop. 2009, 135, 276.e1–276.e12; discussion 276–277. [Google Scholar] [CrossRef]
- Maini, A. Short-term cosmetic orthodontics for general dental practitioners. Br. Dent. J. 2013, 214, 83–84. [Google Scholar] [CrossRef] [PubMed]
- Bukhari, O.M.; Sohrabi, K.; Tavares, M. Factors affecting patients’ adherence to orthodontic appointments. Am. J. Orthod. Dentofac. Orthop. 2016, 149, 319–324. [Google Scholar] [CrossRef] [PubMed]
- Dindaroğlu, F.; Doğan, S. Root Resorption in Orthodontics. Turk. J. Orthod. 2016, 29, 103–108. [Google Scholar] [CrossRef]
- Aljabaa, A.; Almoammar, K.; Aldrees, A.; Huang, G. Effects of vibrational devices on orthodontic tooth movement: A systematic review. Am. J. Orthod. Dentofac. Orthop. 2018, 154, 768–779. [Google Scholar] [CrossRef]
- Spielmann, T.; Wieslander, L.; Hefti, A.F. Acceleration of orthodontically induced tooth movement through the local application of prostaglandin (PGE1). Schweiz. Monatsschrift Zahnmed. 1989, 99, 162–165. [Google Scholar]
- Sydorak, I.; Dang, M.; Baxter, S.J.; Halcomb, M.; Ma, P.; Kapila, S.; Hatch, N. Microsphere controlled drug delivery for local control of tooth movement. Eur. J. Orthod. 2019, 41, 1–8. [Google Scholar] [CrossRef]
- Chandak, S.; Patil, A.S. Effect of platelet-rich plasma on the rate of orthodontic tooth movement. Am. J. Orthod. Dentofac. Orthop. 2022, 162, e28–e34. [Google Scholar] [CrossRef]
- Gkantidis, N.; Mistakidis, I.; Kouskoura, T.; Pandis, N. Effectiveness of non-conventional methods for accelerated orthodontic tooth movement: A systematic review and meta-analysis. J. Dent. 2014, 42, 1300–1319. [Google Scholar] [CrossRef]
- Cronshaw, M.; Parker, S.; Anagnostaki, E.; Lynch, E. Systematic Review of Orthodontic Treatment Management with Photobiomodulation Therapy. Photobiomodul. Photomed. Laser Surg. 2019, 37, 862–868. [Google Scholar] [CrossRef]
- Olguín Vargas, P.; Yáñez Ocampo, B.R. Corticotomy: Historical perspective. Rev. Odontológica Mex. 2016, 20, 82–92. [Google Scholar] [CrossRef]
- Kole, H. Surgical operations on the alveolar ridge to correct occlusal abnormalities. Oral Surg. Oral Med. Oral Pathol. 1959, 12, 277–288, contd. [Google Scholar] [CrossRef] [PubMed]
- Lee, W. Corticotomy for orthodontic tooth movement. J. Korean Assoc. Oral Maxillofac. Surg. 2018, 44, 251–258. [Google Scholar] [CrossRef] [PubMed]
- Han, J.J.; Yang, H.J.; Hwang, S.J. Enhanced Bone Regeneration by Bone Morphogenetic Protein-2 after Pretreatment with Low-Intensity Pulsed Ultrasound in Distraction Osteogenesis. Tissue Eng. Regen. Med. 2022, 19, 871–886. [Google Scholar] [CrossRef] [PubMed]
- Wilcko, W.M.; Wilcko, T.; Bouquot, J.E.; Ferguson, D.J. Rapid orthodontics with alveolar reshaping: Two case reports of decrowding. Int. J. Periodontics Restor. Dent. 2001, 21, 9–19. [Google Scholar]
- Gil, A.P.S.; Haas, O.L., Jr.; Méndez-Manjón, I.; Masiá-Gridilla, J.; Valls-Ontañón, A.; Hernández-Alfaro, F.; Guijarro-Martínez, R. Alveolar corticotomies for accelerated orthodontics: A systematic review. J. Craniomaxillofac. Surg. 2018, 46, 438–445. [Google Scholar] [CrossRef] [PubMed]
- Patterson, B.M.; Dalci, O.; Darendeliler, M.A.; Papadopoulou, A.K. Corticotomies and Orthodontic Tooth Movement: A Systematic Review. J. Oral Maxillofac. Surg. 2016, 74, 453–473. [Google Scholar] [CrossRef]
- Alfawal, A.M.; Hajeer, M.Y.; Ajaj, M.A.; Hamadah, O.; Brad, B. Effectiveness of minimally invasive surgical procedures in the acceleration of tooth movement: A systematic review and meta-analysis. Prog. Orthod. 2016, 17, 33. [Google Scholar] [CrossRef]
- Cassetta, M.; Di Carlo, S.; Giansanti, M.; Pompa, V.; Pompa, G.; Barbato, E. The impact of osteotomy technique for corticotomy-assisted orthodontic treatment (CAOT) on oral health-related quality of life. Eur. Rev. Med. Pharmacol. Sci. 2012, 16, 1735–1740. [Google Scholar]
- Dibart, S.; Sebaoun, J.D.; Surmenian, J. Piezocision: A minimally invasive, periodontally accelerated orthodontic tooth movement procedure. Compend. Contin. Educ. Dent. 2009, 30, 342–344, 346, 348–350. [Google Scholar]
- Pakhare, V.V.; Khandait, C.H.; Shrivastav, S.S.; Dhadse, P.V.; Baliga, V.S.; Seegavadi, V.D. Piezosurgery®-assisted periodontally accelerated osteogenic orthodontics. J. Indian Soc. Periodontol. 2017, 21, 422–426. [Google Scholar] [CrossRef] [PubMed]
- Tunçer, N.I.; Arman-Özçirpici, A.; Oduncuoglu, B.F.; Göçmen, J.S.; Kantarci, A. Efficiency of piezosurgery technique in miniscrew supported en-masse retraction: A single-centre, randomized controlled trial. Eur. J. Orthod. 2017, 39, 586–594. [Google Scholar] [CrossRef] [PubMed]
- Yi, J.; Xiao, J.; Li, Y.; Li, X.; Zhao, Z. Efficacy of piezocision on accelerating orthodontic tooth movement: A systematic review. Angle Orthod. 2017, 87, 491–498. [Google Scholar] [CrossRef] [PubMed]
- Uribe, F.; Davoody, L.; Mehr, R.; Jayaratne, Y.S.N.; Almas, K.; Sobue, T.; Allareddy, V.; Nanda, R. Efficiency of piezotome-corticision assisted orthodontics in alleviating mandibular anterior crowding-a randomized clinical trial. Eur. J. Orthod. 2017, 39, 595–600. [Google Scholar] [CrossRef] [PubMed]
- Gibreal, O.; Hajeer, M.Y.; Brad, B. Efficacy of piezocision-based flapless corticotomy in the orthodontic correction of severely crowded lower anterior teeth: A randomized controlled trial. Eur. J. Orthod. 2018, 41, 188–195. [Google Scholar] [CrossRef] [PubMed]
- Mheissen, S.; Khan, H.; Samawi, S. Is Piezocision effective in accelerating orthodontic tooth movement: A systematic review and meta-analysis. PLoS ONE 2020, 15, e0231492. [Google Scholar] [CrossRef] [PubMed]
- Page, M.J.; McKenzie, J.E.; Bossuyt, P.M.; Boutron, I.; Hoffmann, T.C.; Mulrow, C.D.; Shamseer, L.; Tetzlaff, J.M.; Akl, E.A.; Brennan, S.E.; et al. The PRISMA 2020 statement: An updated guideline for reporting systematic reviews. Syst. Rev. 2021, 10, 89. [Google Scholar] [CrossRef] [PubMed]
- Abbas, N.H.; Sabet, N.E.; Hassan, I.T. Evaluation of corticotomy-facilitated orthodontics and piezocision in rapid canine retraction. Am. J. Orthod. Dentofacial. Orthop. 2016, 149, 473–480. [Google Scholar] [CrossRef]
- Aksakalli, S.; Calik, B.; Kara, B.; Ezirganli, S. Accelerated tooth movement with piezocision and its periodontal-transversal effects in patients with Class II malocclusion. Angle Orthod. 2016, 86, 59–65. [Google Scholar] [CrossRef]
- Jahanbakhshi, M.R.; Motamedi, A.M.; Feizbakhsh, M.; Mogharehabed, A. The effect of buccal corticotomy on accelerating orthodontic tooth movement of maxillary canine. Dent. Res. J. 2016, 13, 303–308. [Google Scholar] [CrossRef]
- Raj, S.C.; Praharaj, K.; Barik, A.K.; Patnaik, K.; Mahapatra, A.; Mohanty, D.; Katti, N.; Mishra, D.; Panda, S.M. Retraction With and Without Piezocision-Facilitated Orthodontics: A Randomized Controlled Trial. Int. J. Periodontics Restor. Dent. 2020, 40, e19–e26. [Google Scholar] [CrossRef] [PubMed]
- Alqadasi, B.; Xia, H.Y.; Alhammadi, M.S.; Hasan, H.; Aldhorae, K.; Halboub, E. Three-dimensional assessment of accelerating orthodontic tooth movement-micro-osteoperforations vs piezocision: A randomized, parallel-group and split-mouth controlled clinical trial. Orthod. Craniofacial Res. 2021, 24, 335–343. [Google Scholar] [CrossRef] [PubMed]
- Fernandes, L.; Figueiredo, D.S.F.; Oliveira, D.D.; Houara, R.G.; Rody, W.J., Jr.; Gribel, B.F.; Soares, R.V. The effects of corticotomy and piezocision in orthodontic canine retraction: A randomized controlled clinical trial. Prog. Orthod. 2021, 22, 37. [Google Scholar] [CrossRef] [PubMed]
- Alfailany, D.T.; Hajeer, M.Y.; Al-Bitar, M.I.; Alsino, H.I.; Jaber, S.T.; Brad, B.; Darwich, K. Effectiveness of Flapless Cortico-Alveolar Perforations Using Mechanical Drills Versus Traditional Corticotomy on the Retraction of Maxillary Canines in Class II Division 1 Malocclusion: A Three-Arm Randomized Controlled Clinical Trial. Cureus 2023, 15, e44190. [Google Scholar] [CrossRef] [PubMed]
- Mheissen, S.; Khan, H.; Alsafadi, A.S.; Almuzian, M. The effectiveness of surgical adjunctive procedures in the acceleration of orthodontic tooth movement: A systematic review of systematic reviews and meta-analysis. J. Orthod. 2021, 48, 156–171. [Google Scholar] [CrossRef] [PubMed]
- Gopalakrishnan, U.; Madasamy, R.; Mathew, R.; Alsulaimani, F.F.; Sayed, M.; Mugri, M.; Baeshen, H.A.; Bhandi, S.; Testarelli, L.; Mahendra, L.; et al. A split-mouth randomized controlled trial to compare the rate of canine retraction after a soft tissue procedure compared against a corticotomy procedure for accelerated tooth movement. Niger. J. Clin. Pract. 2023, 26, 666–673. [Google Scholar] [CrossRef]
- Addanki, P.; Gooty, J.R.; Palaparthy, R. Clinical and Radiographic Comparative Evaluation of Buccal and Palatal Corticotomy with Buccal Corticotomy in Periodontally Accelerated Osteogenic Orthodontics with Surgical Bur. Contemp. Clin. Dent. 2017, 8, 321–326. [Google Scholar] [CrossRef] [PubMed]
- Yavuz, M.C.; Sunar, O.; Buyuk, S.K.; Kantarcı, A. Comparison of piezocision and discision methods in orthodontic treatment. Prog. Orthod. 2018, 19, 44. [Google Scholar] [CrossRef]
- Wang, C.W.; Yu, S.H.; Mandelaris, G.A.; Wang, H.L. Is periodontal phenotype modification therapy beneficial for patients receiving orthodontic treatment? An American Academy of Periodontology best evidence review. J. Periodontol. 2020, 91, 299–310. [Google Scholar] [CrossRef]
- Lu, Y.; Liu, H.; Liu, J.; Chen, M. Augmented Corticotomy on the Lingual Side in Mandibular Anterior Region Assisting Orthodontics in Protrusive Malocclusion: A Case Report. Medicina 2022, 58, 1181. [Google Scholar] [CrossRef]
- Ma, H.M.; Lyu, H.M.; Xu, L.; Hou, J.X.; Wang, X.X.; Li, W.R.; Li, X.T. Effect of augmented corticotomy-assisted presurgical orthodontic treatment on alveolar bone fenestration and dehiscence in skeletal class III patients. J. Dent. Sci. 2023, 18, 997–1007. [Google Scholar] [CrossRef] [PubMed]
- Nagy, P.; Porzse, V.; Nemeth, F.; Windisch, P.; Palkovics, D. Presentation of a novel surgical technique in periodontally accelerated osteogenic orthodontics. CBCT assessment of the buccal alveolar dimensional changes: A proof-of-concept report of four cases. Quintessence Int. 2023, 54, 358–370. [Google Scholar] [CrossRef] [PubMed]
- Abu Alhaija, E.S.; Al-Areqi, M.M.; AlShami, R.; Al Maaitah, E.F.; Al Wahadni, A. Effect of piezocision-assisted lower second molar protraction on periodontal tissues, alveolar bone height, and lower second molar root resorption. Angle Orthod. 2023, 93, 306–312. [Google Scholar] [CrossRef] [PubMed]
- Ngan, P.W.; Burch, J.G.; Wei, S.H. Grafted and ungrafted labial gingival recession in pediatric orthodontic patients: Effects of retraction and inflammation. Quintessence Int. 1991, 22, 103–111. [Google Scholar] [PubMed]
- Gasparro, R.; Bucci, R.; De Rosa, F.; Sammartino, G.; Bucci, P.; D’Antò, V.; Marenzi, G. Effectiveness of surgical procedures in the acceleration of orthodontic tooth movement: Findings from systematic reviews and meta-analyses. Jpn. Dent. Sci. Rev. 2022, 58, 137–154. [Google Scholar] [CrossRef] [PubMed]
- Go, E.J.; Kim, S.A.; Cho, M.L.; Lee, K.S.; Shetty, A.A.; Kim, S.J. A Combination of Surgical and Chemical Induction in a Rabbit Model for Osteoarthritis of the Knee. Tissue Eng. Regen. Med. 2022, 19, 1377–1388. [Google Scholar] [CrossRef] [PubMed]
- Baloul, S.S.; Gerstenfeld, L.C.; Morgan, E.F.; Carvalho, R.S.; Van Dyke, T.E.; Kantarci, A. Mechanism of action and morphologic changes in the alveolar bone in response to selective alveolar decortication-facilitated tooth movement. Am. J. Orthod. Dentofac. Orthop. 2011, 139, S83–S101. [Google Scholar] [CrossRef] [PubMed]
- Mousa, M.R.; Hajeer, M.Y.; Burhan, A.S.; Heshmeh, O. Adult periodontal comparison after treatment of palatally impacted canines aligned by conventional or accelerated minimally-invasive corticotomy-assisted orthodontic traction: A randomized controlled trial. Int. Orthod. 2023, 21, 100785. [Google Scholar] [CrossRef]
- Zou, M.; Li, C.; Zheng, Z. Remote Corticotomy Accelerates Orthodontic Tooth Movement in a Rat Model. BioMed Res. Int. 2019, 2019, 4934128. [Google Scholar] [CrossRef]
- Matsumura, N.; Li, X.; Uchikawa-Kitaya, E.; Li, N.; Dong, H.; Chen, K.; Yoshizawa, M.; Kagami, H. Tissue Engineering with Compact Bone-Derived Cell Spheroids Enables Bone Formation around Transplanted Tooth. Tissue Eng. Regen. Med. 2022, 19, 377–387. [Google Scholar] [CrossRef]
- Pouliezou, I.; Xenou, A.; Vavetsi, K.; Mitsea, A.; Sifakakis, I. Adverse Effects of Surgically Accelerated Orthodontic Techniques: A Systematic Review. Children 2022, 9, 1835. [Google Scholar] [CrossRef] [PubMed]
- Alfailany, D.T.; Hajeer, M.Y.; Burhan, A.S.; Mahaini, L.; Darwich, K.; Aljabban, O. Evaluation of the Effectiveness of Surgical Interventions Versus Non-surgical Ones When Used in Conjunction With Fixed Appliances to Accelerate Orthodontic Tooth Movement: A Systematic Review. Cureus 2022, 14, e25381. [Google Scholar] [CrossRef] [PubMed]
- Khlef, H.N.; Mousa, M.M.; Ammar, A.M.; Hajeer, M.Y.; Awawdeh, M.A. Evaluation of Patient-Centered Outcomes Associated With the Acceleration of en-Masse Retraction of Upper Anterior Teeth Assisted by Flapless Corticotomy Compared to Traditional Corticotomy: A Two-Arm Randomized Controlled Trial. Cureus 2023, 15, e42273. [Google Scholar] [CrossRef] [PubMed]
- Kabbur, K.J.; Kamaraj, S.; Ramesh, B.; Hemanth, M.; Aravind, M.; Jayanth, N.R. An Assessment and Comparison of Root Resorption With Two Different Corticotomy Techniques During Anterior Teeth Retraction: A Split Mouth Prospective Clinical Study. Cureus 2023, 15, e33431. [Google Scholar] [CrossRef] [PubMed]
- Patterson, B.M.; Dalci, O.; Papadopoulou, A.K.; Madukuri, S.; Mahon, J.; Petocz, P.; Spahr, A.; Darendeliler, M.A. Effect of piezocision on root resorption associated with orthodontic force: A microcomputed tomography study. Am. J. Orthod. Dentofac. Orthop. 2017, 151, 53–62. [Google Scholar] [CrossRef] [PubMed]
- Grawish, M.E.; Grawish, L.M.; Grawish, H.M.; Grawish, M.M.; Holiel, A.A.; Sultan, N.; El-Negoly, S.A. Demineralized Dentin Matrix for Dental and Alveolar Bone Tissues Regeneration: An Innovative Scope Review. Tissue Eng. Regen. Med. 2022, 19, 687–701. [Google Scholar] [CrossRef] [PubMed]
- Papadopoulos, N.; Beindorff, N.; Hoffmann, S.; Jost-Brinkmann, P.G.; Präger, T.M. Impact of piezocision on orthodontic tooth movement. Korean J. Orthod. 2021, 51, 366–374. [Google Scholar] [CrossRef] [PubMed]
- Xu, Y.; Yu, L.; Tong, X.; Wang, Y.; Li, Y.; Pan, J.; Yang, Y.; Liu, Y. Efficacy and safety of piezocision in accelerating maxillary anterior teeth en-masse retraction: Study protocol for a randomized controlled trial. Trials 2022, 23, 476. [Google Scholar] [CrossRef]
- Fujinaka, T.; Kernitsky, J.; Liu, J.; Dibart, S. Piezocision Through Computer-Guided Navigation. Int. J. Periodontics Restor. Dent. 2023. [Google Scholar] [CrossRef]
- Simre, S.S.; Rajanikanth, K. Evaluation of conventional corticotomy with novel piezosurgery in orthodontic treatment – Study protocol for a comparative study. Eur. J. Mol. Clin. Me.d 2020, 7, 2128–2131. [Google Scholar]
- Deepak, C. Corticotomy assisted fixed orthodontic treatment vs non corticotomy assisted fixed orthodontic treatment: A randomized clinical trial study. Indian J. Public Health Res. Dev. 2019, 10, 2873–2875. [Google Scholar] [CrossRef]
- Sonone, T.P.; Nawab, A.; Krishnarai, P.; Nagar, P.; Arya; Mohan, I. The effects of corticotomy and piezocision in orthodontic canine retraction: A randomized controlled clinical trial. J. Pharm. Bioallied Sci. 2022, 14, S757–S764. [Google Scholar] [CrossRef] [PubMed]
- Al-A’athal, H.S.; Al-Nimri, K.; Alhammadi, M.S. Analysis of canine retraction and anchorage loss in different facial types with and without piezocision: A split-mouth-design, randomized clinical trial. Angle Orthod. 2022, 92, 746–754. [Google Scholar] [CrossRef] [PubMed]
- Hawkins, V.M.; Panadopoulou, A.K.; Wong, M.; Pandis, N.; Dalci, O.; Darendeliler, M.A. The effect of piezocision vs non piezocision on maxillary extraction space closure: A split-mouth, randomized controlled clinical trial. Am. J. Orthop. Dentofac. Orthop. 2022, 161, 7–19. [Google Scholar] [CrossRef]
- Farid, K.A.; Eid, A.A.; Kaddah, A.; Elsharaby, F.A. The effect of combined corticotomy and low level laser therapy on the rate of orthodontic tooth movement: Split mouth randomized clinical trial. Laser Ther. 2019, 28, 275–283. [Google Scholar] [CrossRef] [PubMed]
- Alfawal, A.M.H.; Hajeer, M.Y.; Ajaj, M.A.; Hamadah, O.; Brad, B.; Latifeh, Y. Evaluation of patient-centered outcomes associated with the acceleration of canine retraction by using minimally invasive surgical procedures: A randomized clinical controlled trial. Dent. Med. Probl. 2020, 57, 285–293. [Google Scholar] [CrossRef] [PubMed]
- Türker, G.; Yavuz, I.; Gönen, B. Which method is more effective for accelerating canine distalization short term, low-level laser therapy or piezocision? A split-mouth study. J. Orofac. Orthop. 2021, 82, 236–245. [Google Scholar] [CrossRef] [PubMed]
- Simre, S.S.; Rajanikanth, K.; Bhola, N.; Jadhav, A.; Patil, C.; Mishra, A. Comparative assessment of corticotomy facilitated rapid canine retraction using piezo versus bur: A randomized clinical study. J. Oral Biol. Craniofac. Res. 2022, 12, 182–186. [Google Scholar] [CrossRef]
- Qabool, H.; Sukhia, R.H. Assessment of rate of tooth movement and duration of canine retraction using piezocision. Am. J. Orthod. Dentofac. Orthop. 2022, 161, 766. [Google Scholar] [CrossRef]

| Study | Region | Study Design | Comparison | Sample Size, n; Sex; Age | Type and Site of Intervention | Duration | Outcome |
|---|---|---|---|---|---|---|---|
| Abbas 2016 [28] | Egypt | RCT, multi-arm | Corticotomy + OT vs. piezocision + OT; split mouth | 20; not given; 15 to 25 | Piezocision (upper canines); piezocision (full cortical depth and canine root length) mesial and distal to canine root, 150 g force; suture incisions; surgical instrument: piezotome (VarioSurg3; NSK) | 3 mo | RCM, molar anchorage loss, canine rotation and inclination, canine root resorption, periodontal parameter |
| Aksakalli 2016 [29] | Turkey | RCT | Piezocision + OT vs. OT; split mouth | 20; f6, m4; 16.3 | Piezocision (upper canines); piezocision (3 mm depth and 10 mm length) mesial and distal to canine, 150 g force; surgical instrument: piezosurgery knife (BS1) | Until class I canine relationship | Compare the extent of distalization and transversal changes, gingival indices, mobility scores |
| Jahanbakhshi 2016 [30] | Iran | RCT | Buccal corticotomy + OT vs. OT; split mouth | 15; f15; 25 | Buccal corticotomy (distal to canine, mesial to U5, vertical groove length 1 mm × depth 0.5~1 mm, 10 spherical perforation with round 2 bur); 200 g force, simple vertical loop | 4 mo | Compare average velocity of tooth movement (monthly and total) |
| Alfawal 2018 [18] | Syria | RCT, multi-arm | Piezocision + OT vs. laser-assisted flapless corticotomy + OT; split mouth | 36; f24, m12; 18.08 | Piezocision (upper canines); 2 corticotomies (3 mm in depth and 10 mm in length) in the buccal at equal distance from the upper canine and second premolar, 150 g force; surgical instrument: piezosurgery knife (BS1); LAFC (3 mm in depth; 8 mm in length) at equal distance from the upper canine and second premolar, 150 g force; surgical instrument: ER:YAG laser, 200 mJ, 12 Hz, 3 W | 4 mo | RCM, molar anchorage loss |
| Raj 2020 [31] | India | RCT | Piezocision + OT vs. OT Split mouth | 20; f14, m6; 20–25 | Piezocision (upper canine); piezocision (3 mm depth × 10 mm length); surgical instrument: piezosurgery knife (Acteon, BS1); 150 g Force canine retraction | 6 mo | Compare rate of canine extraction, resultant alveolar bone level, root resorption, and periodontal parameter |
| Alqadasi 2021 [32] | China | RCT, paralle-group | Piezoincision vs. convetional; split mouth Micro-osteo perforation vs. convetional; split mouth Piezoincision vs. MOP | 21; f12, m9; 15 to 40 | MOPs (flapless perforation using an automated mini-implant driver, 1.5–2 mm in diameter, 5–7 mm in depth) Piezoincision using piezoelectric instruments (Surgybone; Silfradent) (2 mm below the crest of the alveolar ridge and 3 mm in length and 3–5 mm in depth) | 3 mo | Rate of tooth movement, Root resorption, bone height |
| Fernandes 2021 [33] | Brazil | RCT | Corticitomy + OT vs. piezocision + OT vs. Corticotomy + piezocision; Split mouth | 47; m19, f28; 15~38 | Piezocision (upper canine) (3 mm depth × 5 mm length), (Acteon, BS1); Corticotomy (Vertical groove: mesial and distal of canine root, mesial of second premolar/horizontal groove: above canine apex/spherical cortical perforation with round 2 bur, canine to mesial of second premolar); 1.15 N force canine retraction | 6 mo | Compare cumulative distal movement of canines and molecular analysis of gingival crevicular fluid |
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2023 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Han, S.-H.; Park, W.-J.; Park, J.-B. Comparative Efficacy of Traditional Corticotomy and Flapless Piezotomy in Facilitating Orthodontic Tooth Movement: A Systematic Review and Meta-Analysis. Medicina 2023, 59, 1804. https://doi.org/10.3390/medicina59101804
Han S-H, Park W-J, Park J-B. Comparative Efficacy of Traditional Corticotomy and Flapless Piezotomy in Facilitating Orthodontic Tooth Movement: A Systematic Review and Meta-Analysis. Medicina. 2023; 59(10):1804. https://doi.org/10.3390/medicina59101804
Chicago/Turabian StyleHan, Sung-Hoon, Won-Jong Park, and Jun-Beom Park. 2023. "Comparative Efficacy of Traditional Corticotomy and Flapless Piezotomy in Facilitating Orthodontic Tooth Movement: A Systematic Review and Meta-Analysis" Medicina 59, no. 10: 1804. https://doi.org/10.3390/medicina59101804
APA StyleHan, S.-H., Park, W.-J., & Park, J.-B. (2023). Comparative Efficacy of Traditional Corticotomy and Flapless Piezotomy in Facilitating Orthodontic Tooth Movement: A Systematic Review and Meta-Analysis. Medicina, 59(10), 1804. https://doi.org/10.3390/medicina59101804









