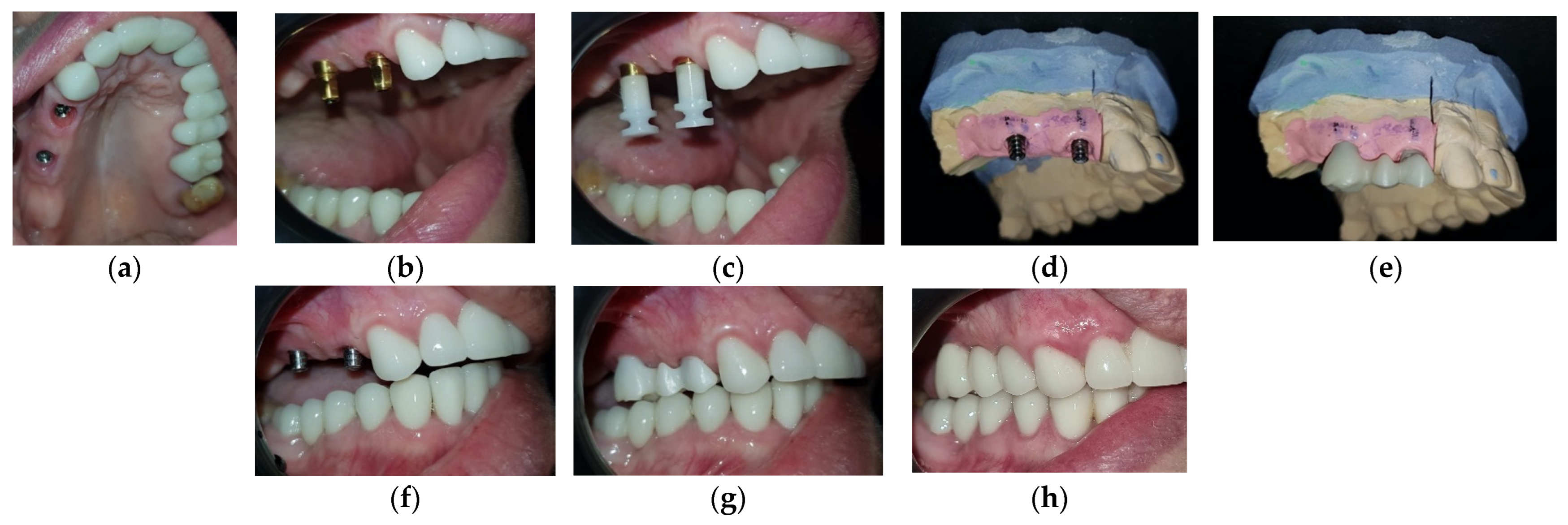
Full-Mouth Rehabilitation of a Patient with Gummy Smile—Multidisciplinary Approach: Case Report
Abstract
:1. Introduction
2. Case Report
3. Discussion
- The patient’s systemic health and her expectations;
- The evaluation of the face and smile line;
- The lip thickness and size;
- The size and shape of the teeth;
- The gingival biotype and the width of keratinized gingiva;
- The thickness and contour of the alveolar bone [17].
- Lack of periodical CBCT evaluation (at three months, six months, and one year)
- Lack of periodical periodontal evaluation using periodontal probing.
4. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Acknowledgments
Conflicts of Interest
References
- Izraelewicz-Djebali, E.; Chabre, C. Gummy smile: Orthodontic or surgical treatment? J. Dentofac. Anom. Orthod. 2015, 8, 102. [Google Scholar] [CrossRef]
- Armitage, G.C. Development of a Classification System for Periodontal Diseases and Conditions. Ann. Periodontol. 1999, 4, 1–6. [Google Scholar] [CrossRef] [PubMed]
- Pandurić, D.G.; Blašković, M.; Brozović, J.; Sušić, M. Surgical Treatment of Excessive Gingival Display Using Lip Repositioning Technique and Laser Gingivectomy as an Alternative to Orthognathic Surgery. J. Oral. Maxillofac. Surg. 2014, 72, 404.e1–404.e11. [Google Scholar] [CrossRef] [PubMed]
- Allen, E.P. Use of mucogingival surgical procedures to enhance esthetics. Dent. Clin. North Am. 1988, 32, 307–330. [Google Scholar] [CrossRef] [PubMed]
- Abou-Arraj, R.V.; Souccar, N.M. Periodontal treatment of excessive gingival display. Semin. Orthod. 2013, 19, 267–278. [Google Scholar] [CrossRef]
- Tjan, A.H.; Miller, G.D.; The, J.G. Some esthetic factors in a smile. J. Prosthet. Dent. 1984, 51, 24–28. [Google Scholar] [CrossRef]
- Hempton, T.J.; Dominici, J.T. Contemporary crown-lengthening therapy: A review. J. Am. Dent. Assoc. 2010, 141, 647–655. [Google Scholar] [CrossRef]
- Lee, E.A. Aesthetic Crown Lengthening: Contemporary Guidelines for Achieving Ideal Gingival Architecture and Stability. Curr. Oral. Health Rep. 2017, 4, 105–111. [Google Scholar] [CrossRef]
- Batista, E.L., Jr.; Moreira, C.C.; Batista, F.C.; de Oliveira, R.R.; Pereira, K.K. Altered passive eruption diagnosis and treatment: A cone beam computed tomography-based reappraisal of the condition. J. Clin. Periodontal. 2012, 39, 1089–1096. [Google Scholar] [CrossRef]
- Arora, S.A.; Chhina, S.; Kazimm, J.; Goel, A.; Mishra, S.; Nidhi, S. Clinical Crown Lengthening using soft tissue diode laser: A case series. Int. J. Oral. Health Med. Res. 2015, 2, 81–83. [Google Scholar]
- Hennet, P. Piezoelectric Bone Surgery: A Review of the Literature and Potential Applications in Veterinary Oromaxillofacial Surgery. Front. Veter-Sci. 2015, 2, 8. [Google Scholar] [CrossRef] [PubMed]
- Kirmani, M.; Trivedi, H.; Bey, A.; Sharma, V.K. Postoperative Complications of Periodontal Surgery. Int. J. Contemp. Med. Res. 2016, 3, 1285–1286. [Google Scholar]
- Paolantoni, G.; Marenzi, G.; Mignogna, J.; Wang, H.L.; Blasi, A.; Sammartino, G. Comparison of three different crown-lengthening procedures in the maxillary anterior aesthetic regions. Quintessence Int. 2016, 47, 407–416. [Google Scholar]
- Mitrea, M.; Niculescu, S.; Dmor, A.; Al Hage, W.E.; Florea, C.; Săveanu, I.C.; Balcos, C.; Forna, N.C. Esthetic rehabilitation with implants-supported fixed dentures after periodontitis. Rom. J. Oral Rehabil. 2021, 13, 102–113. [Google Scholar]
- Sorrentino, R.; Ruggiero, G.; Toska, E.; Leone, R.; Zarone, F. Clinical Evaluation of Cement-Retained Implant-Supported CAD/CAM Monolithic Zirconia Single Crowns in Posterior Areas: Results of a 6-Year Prospective Clinical Study. Prosthesis 2022, 4, 383–393. [Google Scholar] [CrossRef]
- Moura, D.; Lima, E.; Lins, R.; Souza, R.; Martins, A.; Gurgel, B. The treatment of gummy smile: Integrative review of literature. Rev. Clin. Periodontia. Implantol. Oral Rehabil. 2017, 10, 26–28. [Google Scholar] [CrossRef] [Green Version]
- Narayan, S.; Narayan, T.V.; Jacob, P.C. Correction of gummy smile: A report of two cases. J. Indian Soc. Periodontol. 2011, 15, 421–424. [Google Scholar] [CrossRef]
- Jurado, C.A.; Parachuru, V.; Tinoco, J.V.; Guzman-Perez, G.; Tsujimoto, A.; Javvadi, R.; Afrashtehfar, K.I. Diagnostic Mock-Up as a Surgical Reduction Guide for Crown Lengthening: Technique Description and Case Report. Medicina 2022, 58, 1360. [Google Scholar] [CrossRef]
- Alhumaidan, A.; Alqahtani, A.; Al-Qarni, F. 3D-Printed Surgical Guide for Crown Lengthening Based on Cone Beam Computed Tomography Measurements: A Clinical Report with 6 Months Follow Up. Appl. Sci. 2020, 10, 5697. [Google Scholar] [CrossRef]
- Clear, A.G. Guidelines for flapless surgery. J. Oral. Maxillofac. Surg. 2007, 65, 20–32. [Google Scholar]
- Fletcher, P. Biologic rationale of aesthetic crown lengthening using innovative proportion gauges. Int. J. Periodontics Restor. Dent. 2011, 31, 523–532. [Google Scholar]
- Robert, L.; McGuire, M. The diagnosis and treatment of the gummy smile. Compend. Contin. Educ. Dent. 1997, 18, 757–762+764; quiz 766. [Google Scholar]
- Herrero, F.; Scott, J.B.; Maropis, P.; Yukna, R.A. Clinical comparison of desired versus actual amount of surgical crown lengthening. J. Periodontal. 1995, 66, 568–571. [Google Scholar] [CrossRef] [PubMed]
- Kois, J.C. The restorative-periodontal interface: Biological parameters. Periodontology 1996, 11, 29–38. [Google Scholar] [CrossRef] [PubMed]
- Bindl, A.; Mörmann, W.H. Marginal and internal fit of all-ceramic CAD/CAM crown-copings on chamfer preparations. J. Oral Rehabil. 2005, 32, 441–447. [Google Scholar] [CrossRef] [PubMed]
- Beuer, F.; Aggstaller, H.; Richter, J.; Edelhoff, D.; Gernet, W. Influence of preparation angle on marginal and internal fit of CAD/CAM-fabricated zirconia crown copings. Quintessence Int. 2009, 40, 243–250. [Google Scholar]
- Komine, F.; Iwai, T.; Kobayashi, K.; Matsumura, H. Marginal and Internal Adaptation of Zirconium Dioxide Ceramic Copings and Crowns with Different Finish Line Designs. Dent. Mater. J. 2007, 26, 659–664. [Google Scholar] [CrossRef] [Green Version]
- Comlekoglu, M.; Dundar, M.; Ozcan, M.; Gungor, M.; Gokce, B.; Artunc, C. Influence of cervical finish line type on the marginal adaptation of zirconia ceramic crowns. Oper. Dent. 2009, 34, 586–592. [Google Scholar] [CrossRef]
- Iwai, T.; Komine, F.; Kobayashi, K.; Saito, A.; Matsumura, H. Influence of convergence angle and cement space on adaptation of zirconium dioxide ceramic copings. Acta Odontol. Scand. 2008, 66, 214–218. [Google Scholar] [CrossRef]
- Dittmer, M.P.; Borchers, L.; Stiesch, M.; Kohorst, P. Stresses and distortions within zirconia-fixed dental prostheses due to the veneering process. Acta Biomater. 2009, 5, 3231–3239. [Google Scholar] [CrossRef]
- Kohorst, P.; Brinkmann, H.; Dittmer, M.P.; Borchers, L.; Stiesch, M. Influence of the veneering process on the marginal fit of zirconia fixed dental prostheses. J. Oral Rehabil. 2010, 37, 283–291. [Google Scholar] [CrossRef] [PubMed]
- Vigolo, P.; Fonzi, F. An In Vitro Evaluation of Fit of Zirconium-Oxide-Based Ceramic Four-Unit Fixed Partial Dentures, Generated with Three Different CAD/CAM Systems, before and after Porcelain Firing Cycles and after Glaze Cycles. J. Prosthodont. 2008, 17, 621–626. [Google Scholar] [CrossRef] [PubMed]
- Gonzalo, E.; Suárez, M.J.; Serrano, B.; Lozano, J.F. A comparison of the marginal vertical discrepancies of zirconium and metal ceramic posterior fixed dental prostheses before and after cementation. J. Prosthet. Dent. 2009, 102, 378–384. [Google Scholar] [CrossRef] [PubMed]
- Tinschert, J.; Natt, G.; Mautsch, W.; Augthun, M.; Spiekermann, H. Fracture resistance of lithium disilicate-, alumina-, and zirconia-based three-unit fixed partial dentures: A laboratory study. Int. J. Prosthodont. 2001, 14, 231–238. [Google Scholar]
- Rosentritt, M.; Behr, M.; Thaller, C.; Rudolph, H.; Feilzer, A. Fracture performance of computer-aided manufactured zirconia and alloy crowns. Quintessence Int. 2009, 40, 655–662. [Google Scholar]
- Derand, T.; Molin, M.; Kvam, K. Bond strength of composite luting cement to zirconia ceramic surfaces. Dent. Mater. 2005, 21, 1158–1162. [Google Scholar] [CrossRef]
- Kitayama, S.; Nikaido, T.; Ikeda, M.; Alireza, S.; Miura, H.; Tagami, J. Internal coating of zirconia restoration with silica-based ceramic improves bonding of resin cement to dental zirconia ceramic. Bio-Medical Mater. Eng. 2010, 20, 77–87. [Google Scholar] [CrossRef]
- Wittneben, J.G.; Joda, T.; Weber, H.P.; Brägger, U. Screw retained vs. cement retained implant-supported fixed dental prosthesis. Periodontology 2017, 73, 141–151. [Google Scholar] [CrossRef]
- Shadid, R.; Sadaqa, N. A Comparison Between Screw- and Cement-Retained Implant Prostheses. A Lit. Review. J. Oral Implant. 2012, 38, 298–307. [Google Scholar] [CrossRef] [Green Version]
- de Brandão, M.L.; Vettore, M.V.; Vidigal Júnior, G.M. Peri-implant bone loss in cement- and screw-retained prostheses: Systematic review and meta-analysis. J. Clin. Periodontol. 2013, 40, 287–295. [Google Scholar] [CrossRef]
- Rosenstiel, S.F.; Land, M.F.; Fujimoto, J. Contemporary Fixed Prosthodontics, 5th ed.; Elsevier Inc.: St Louis, MO, USA, 2016; pp. 334+358–361. [Google Scholar]
- Park, D.U.; Kim, J.Y.; Lee, J.R.; Kim, H.S.; Sim, H.Y.; Lee, H.; Han, Y.S. Screw-and-cement-retained prosthesis versus cement-retained prosthesis: Which is more appropriate for the upper premolar area? J. Dent. Sci. 2022, 17, 1553–1558. [Google Scholar] [CrossRef] [PubMed]
- Dym, H.; Pierre, R. Diagnosis and Treatment Approaches to a "Gummy Smile". Dent. Clin. North Am. 2020, 64, 341–349. [Google Scholar] [CrossRef] [PubMed]
- Nasr, M.W.; Jabbour, S.F.; Sidaoui, J.A.; Haber, R.N.; Kechichian, E.G. Botulinum Toxin for the Treatment of Excessive Gingival Display: A Systematic Review. Aesthetic Surg. J. 2015, 36, 82–88. [Google Scholar] [CrossRef] [PubMed]












Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2023 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Jánosi, K.M.; Cerghizan, D.; Berneanu, F.D.; Kovács, A.; Szász, A.; Mureșan, I.; Hănțoiu, L.G.; Albu, A.I. Full-Mouth Rehabilitation of a Patient with Gummy Smile—Multidisciplinary Approach: Case Report. Medicina 2023, 59, 197. https://doi.org/10.3390/medicina59020197
Jánosi KM, Cerghizan D, Berneanu FD, Kovács A, Szász A, Mureșan I, Hănțoiu LG, Albu AI. Full-Mouth Rehabilitation of a Patient with Gummy Smile—Multidisciplinary Approach: Case Report. Medicina. 2023; 59(2):197. https://doi.org/10.3390/medicina59020197
Chicago/Turabian StyleJánosi, Kinga Mária, Diana Cerghizan, Florentin Daniel Berneanu, Alpár Kovács, Andrea Szász, Izabella Mureșan, Liana Georgiana Hănțoiu, and Aurița Ioana Albu. 2023. "Full-Mouth Rehabilitation of a Patient with Gummy Smile—Multidisciplinary Approach: Case Report" Medicina 59, no. 2: 197. https://doi.org/10.3390/medicina59020197
APA StyleJánosi, K. M., Cerghizan, D., Berneanu, F. D., Kovács, A., Szász, A., Mureșan, I., Hănțoiu, L. G., & Albu, A. I. (2023). Full-Mouth Rehabilitation of a Patient with Gummy Smile—Multidisciplinary Approach: Case Report. Medicina, 59(2), 197. https://doi.org/10.3390/medicina59020197





