Influence of the Operator`s Experience, Working Time, and Working Position on the Quality of the Margin Width: In Vitro Study
Abstract
1. Introduction
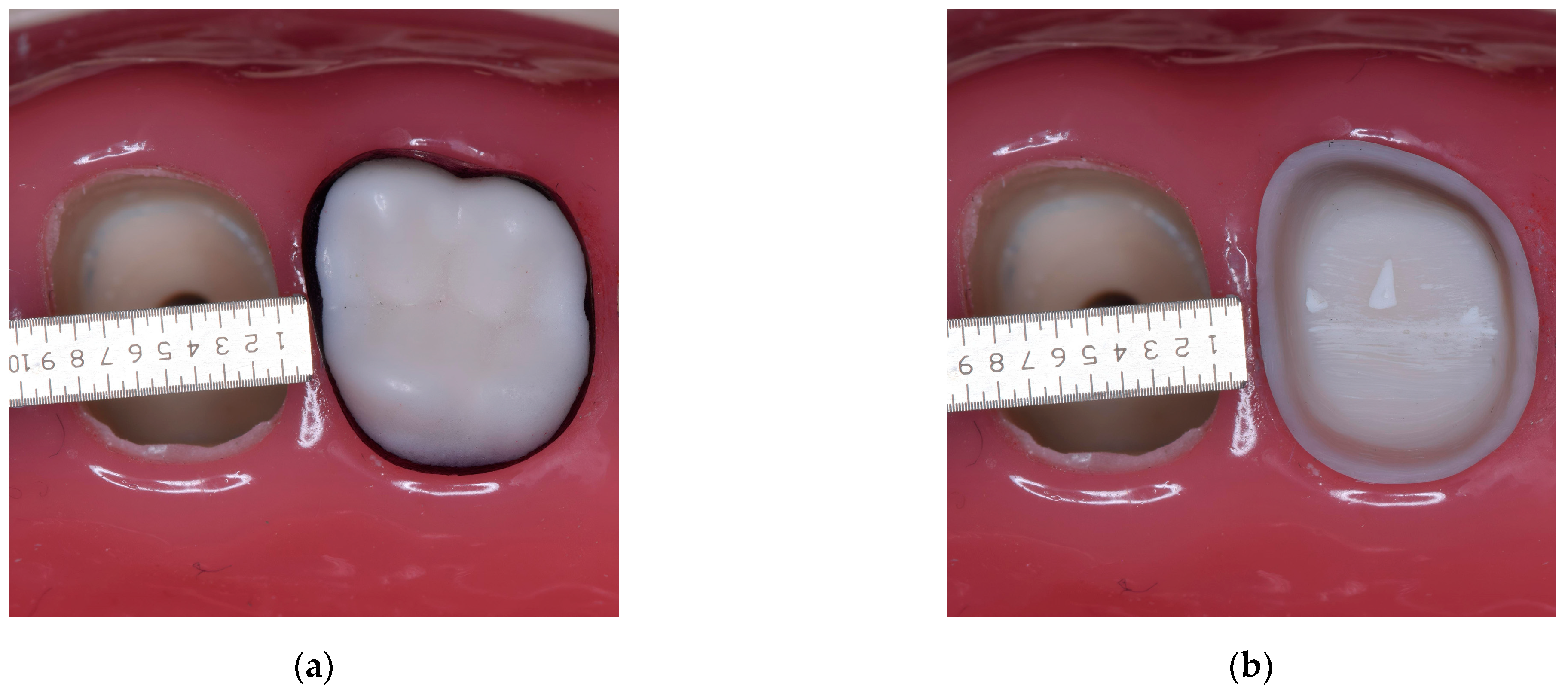
2. Materials and Methods
3. Results
4. Discussion
- In vivo conditions could not be reproduced perfectly. Even the best simulators cannot reproduce the intraoral conditions perfectly (visibility, muscle and tongue tonicity, saliva, and the patient’s movements).
- The low number of participants—a higher number could give different results depending on skill and experience.
- The use of one type of tooth for the preparation—different types of teeth from different regions could lead to different results and improve the complexity of the study.
- Subjective human assessment of the measurements. Using total digital working methods (scanning and digital analysis) can improve the accuracy of the measurements.
5. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Acknowledgments
Conflicts of Interest
References
- Seymour, K.G.; Cherukara, G.P.; Samarawickrama, D.Y.; Zou, L. Consistency of labial finish line preparation for metal ceramic crowns: An investigation of a new bur. J. Prosthodont. 2008, 17, 14–19. [Google Scholar] [CrossRef]
- Sirajuddin, S.; Narasappa, K.M.; Gundapaneni, V.; Chungkham, S.; Walikar, A.S. Iatrogenic damage to periodontium by restorative treatment procedures: An overview. Open Dent. J. 2015, 9, 217–222. [Google Scholar] [CrossRef]
- Sarda, A.S.; Bedia, S.V. Influence of manufacturing technique on marginal fit of cobalt chromium restorations: An in-vitro study. Indian J. Dent. Res. 2021, 32, 495–499. [Google Scholar] [CrossRef]
- McLean, J.W.; Von, F. The estimation of cement film thickness by an in vivo technique. Br. Dent. J. 1971, 131, 107–111. [Google Scholar] [CrossRef]
- Aminian, A.; Brunton, P.A. A comparison of the depths produced using three different tooth preparation techniques. J. Prosthet. Dent. 2003, 89, 19–22. [Google Scholar] [CrossRef]
- Tsitrou, E.A.; Northeast, S.E.; van Noort, R. Evaluation of the marginal fit of three margin designs of resin composite crowns using CAD/CAM. J. Dent. 2007, 35, 68–73. [Google Scholar] [CrossRef]
- Beuer, F.; Edelhoff, D.; Gernet, W.; Naumann, M. Effect of preparation angles on the precision of zirconia crown copings fabricated by CAD/CAM system. Dent. Mater. J. 2008, 27, 814–820. [Google Scholar] [CrossRef]
- Valderhaug, J. Periodontal conditions and carious lesions following the insertion of fixed prostheses: A 10-year follow up study. Int. Dent. J. 1980, 39, 296. [Google Scholar]
- Valderhaug, J.; Birkeland, J.M. Periodontal conditions in patients 5 years following insertion of fixed prostheses. J. Oral Rehabil. 1976, 3, 237. [Google Scholar] [CrossRef] [PubMed]
- Newsome, P.; Owen, S. Improving your margins. J. Aesthetic Dent. Today 2009, 3, 6–12. [Google Scholar]
- Goodacre, C.J.; Compagni, W.V.; Aquilino, S.A. Tooth preparations for complete crowns: An art form based on scientific principles. J. Prosthet. Dent. 2011, 85, 363–376. [Google Scholar] [CrossRef] [PubMed]
- Won, I.J.; Kwon, K.R.; Pae, A.R.; Choi, D.G. An influence of operator’s posture on the shape of prepared tooth surfaces for fixed partial denture. J. Korean Acad. Prosthodont. 2011, 49, 38–48. [Google Scholar] [CrossRef]
- Lee, S.J.; Choi, D.G. The influence of home position (HP) and random position (RP) on the shape of prepared tooth surfaces-upper left 1st molar for full cast crown. J. Dent. Rehabil. Appl. Sci. 2001, 17, 257–274. [Google Scholar]
- Kasem, A.T.; Sakrana, A.A.; Ellayeh, M.; Özcan, M. Evaluation of zirconia and zirconia-reinforced glass ceramic systems fabricated for minimal invasive preparations using a novel standardization method. J. Esthet. Restor. Dent. 2020, 32, 560–568. [Google Scholar] [CrossRef] [PubMed]
- Nakamura, K.; Harada, A.; Inagaki, R.; Kanno, T.; Niwano, Y.; Milleding, P.; Örtengren, U. Fracture resistance of monolithic zirconia molar crowns with reduced thickness. Acta Odontol. Scand. 2015, 73, 602–608. [Google Scholar] [CrossRef] [PubMed]
- Cerghizan, D.; Crăciun, A.; Albu, A.; Baloș, M.; Jánosi, K.M. In vitro study about the abutment axial wall’s convergence. Acta Stomatol. Marisiensis 2020, 3, 269–274. [Google Scholar] [CrossRef]
- Minyé, H.M.; Gilbert, G.H.; Litaker, M.S.; Mungia, R.; Meyerowitz, C.; Louis, D.R.; Slootsky, A.; Gordan, V.V.; McCracken, M.S.; National Dental PBRN Collaborative Group. Preparation techniques used to make single-unit crowns: Findings from the national dental practice-based research network. J. Prosthodont. 2018, 27, 813–820. [Google Scholar] [CrossRef]
- Jubhari, E.H.; Lesal, E. Finish line for full coverage crown: A systematic review. J. Dentomaxillofac. Sci. 2021, 6, 1–4. [Google Scholar] [CrossRef]
- Sadid-Zadeh, R.; Sahraoui, H.; Lawson, B.; Cox, R. Assessment of tooth preparations submitted to dental laboratories for fabrication of monolithic zirconia crowns. Dent. J. 2021, 9, 112. [Google Scholar] [CrossRef] [PubMed]
- Shankar, S.; Gounder, R.; Ganapathy, D. Standards of teeth preparation for anterior all-ceramic crowns in private dental practice. Drug Invent. Today 2020, 14, 484–487. [Google Scholar]
- Haddad, C.; Azzi, K. Influence of the type and thickness of cervical margins on the strength of posterior monolithic zirconia crowns: A review. Eur. J. Gen. Dent. 2022, 11, 073–080. [Google Scholar] [CrossRef]
- Beuer, F.; Aggstaller, H.; Edelhoff, D.; Gernet, W. Effect of preparation design on the fracture resistance of zirconia crown copings. Dent. Mater. J. 2008, 27, 362–367. [Google Scholar] [CrossRef]
- Sadan, A.; Blatz, M.B.; Lang, B. Clinical considerations for densely sintered alumina and zirconia restorations: Part 1. Int. J. Periodontics Restor. Dent. 2005, 25, 213–219. [Google Scholar]
- Alzahrani, A.M.; Beyari, A.M.; Emam, Z.N. The influence of the cervical finish line designs on the fracture resistance of CAD/CAM monolithic zirconia crowns: An in vitro study. Int. J. Health Sci. Res. 2018, 8, 101–110. [Google Scholar]
- Jalalian, E.; Rostami, R.; Atashkar, B. Comparison of chamfer and deep chamfer preparation designs on the fracture resistance of zirconia core restorations. J. Dent. Res. Dent. Clin. Dent. Prospects 2011, 5, 41–45. [Google Scholar] [CrossRef]
- Siegel, S.C.; von Fraunhofer, J.A. Dental burs what bur for which application? A survey of dental schools. J. Prosthodont. 1999, 8, 258–263. [Google Scholar] [CrossRef] [PubMed]
- Hooper, S.M.; Huggett, R.; Foster, L.V. Teaching veneer and crown margins in UK dental schools. Dent. Update 1993, 20, 192–193, 195–196. [Google Scholar]
- Boening, K.W.; Kaestner, K.I.; Luthardt, R.G.; Walter, M.H. Burs with guide pins for standardized tooth preparation. Quintessence Int. 2001, 32, 191–197. [Google Scholar]
- Mansueto, M.A.; Abdulkarim, H.A.; Thabet, W.R.; Haney, S.J. The chamfer finish line: Preclinical student performance using different bur designs. J. Dent. Educ. 2010, 74, 612–617. [Google Scholar] [CrossRef]
- Măroiu, A.-C.; Sinescu, C.; Duma, V.-F.; Topală, F.; Jivănescu, A.; Popovici, P.M.; Tudor, A.; Romînu, M. Micro-CT and microscopy study of internal and marginal gap to tooth surface of crenelated versus conventional dental indirect veneers. Medicina 2021, 57, 772. [Google Scholar] [CrossRef]
- Siegel, S.C.; von Fraunhofer, J.A. Dental cutting with diamond burs: Heavy-handed or light-touch? J. Prosthodont. 1999, 8, 3–9. [Google Scholar] [CrossRef]
- Rotella, M.; Ercoli, C.; Funkenbusch, P.D.; Russell, S.; Feng, C. Performance of single-use and multiuse diamond rotary cutting instruments with turbine and electric handpieces. J. Prosthet. Dent. 2014, 111, 56–63. [Google Scholar] [CrossRef]
- Mihali, S.G.; Lolos, D.; Popa, G.; Tudor, A.; Bratu, D.C. Retrospective long-term clinical outcome of feldspathic ceramic veneers. Materials 2022, 15, 2150. [Google Scholar] [CrossRef]
- Rammelsberg, P.; Eickemeyer, G.; Erdelt, K.; Pospiech, P. Fracture resistance of posterior metal-free polymer crowns. J. Prosthet. Dent. 2000, 84, 303–308. [Google Scholar] [CrossRef]
- Pan, C.-Y.; Lan, T.-H.; Liu, P.-H.; Fu, W.-R. Comparison of different cervical finish lines of all-ceramic crowns on primary molars in finite element analysis. Materials 2020, 13, 1094. [Google Scholar] [CrossRef]
- Tiu, J.; Lin, T.; Al-Amleh, B.; Waddell, J.N. Convergence angles and margin widths of tooth preparations by New Zealand dental students. J. Prosthet. Dent. 2016, 116, 74–79. [Google Scholar] [CrossRef]
- Denry, I.; Kelly, J.R. State of the art of zirconia for dental applications. Dent. Mater. 2008, 24, 299–307. [Google Scholar] [CrossRef]
- Hey, J.; Schweyen, R.; Kupfer, P.; Beuer, F. Influence of preparation design on the quality of tooth preparation in preclinical dental education. J. Dent. Sci. 2017, 12, 21–26. [Google Scholar] [CrossRef] [PubMed]
- Xu, X.; Xie, Q.; Zhou, Y.; Wu, L.; Cao, Y. Effect of a standardized training with digital evaluation on the improvement of prosthodontic faculty’s performance in crown preparation: A pre-post design. J. Prosthodont. 2020, 29, 766–771. [Google Scholar] [CrossRef] [PubMed]
- LeBlanc, V.R.; Urbankova, A.; Hadavi, F.; Lichtenthal, R.M. A preliminary study in using virtual reality to train dental students. J. Dent. Educ. 2004, 68, 378–383. [Google Scholar] [CrossRef] [PubMed]
- Stoilov, M.; Trebess, L.; Klemmer, M.; Stark, H.; Enkling, N.; Kraus, D. Comparison of digital self-assessment systems and faculty feedback for tooth preparation in a preclinical simulation. Int. J. Environ. Res. Public Health 2021, 18, 13218. [Google Scholar] [CrossRef] [PubMed]
- San Diego, J.P.; Newton, T.J.; Sagoo, A.K.; Aston, T.-A.; Banerjee, A.; Quinn, B.F.A.; Cox, M.J. Learning clinical skills using haptic vs. phantom head dental chair simulators in removal of artificial caries: Cluster-randomized trials with two cohorts’ cavity preparation. Dent. J. 2022, 10, 198. [Google Scholar] [CrossRef] [PubMed]
- Valenti, M.; Schmitz, J.H.; Cortellini, D.; Valenti, A.; Canale, A. A diagnostically and digitally driven tooth preparation protocol by using a patient monitoring tool with an intraoral scanner. J. Prosthet. Dent. 2021, 129, 7–13. [Google Scholar] [CrossRef]
- Liu, C.X.; Gao, J.; Zhao, Y.W.; Fan, L.; Jia, L.M.; Hu, N.; Mei, Z.Y.; Dong, B.; Zhang, Q.Q.; Yu, H.Y. Precise tooth preparation technique guided by 3D printing guide plate with quantitative hole. West China J. Stomatol. 2020, 38, 350–355. [Google Scholar]
- Eichenberger, M.; Biner, N.; Amato, M.; Lussi, A.; Perrin, P. Effect of magnification on the precision of tooth preparation in dentistry. Oper. Dent. 2018, 43, 501–507. [Google Scholar] [CrossRef]
- Yu, H. Digital Guided Micro Prosthodontics; Springer: Singapore, 2022; pp. 43–57. [Google Scholar]
- Carpentier, M.; Aubeux, D.; Armengol, V.; Pérez, F.; Prud’homme, T.; Gaudin, A. The effect of magnification loupes on spontaneous posture change of dental students during preclinical restorative training. J. Dent. Educ. 2019, 83, 407–415. [Google Scholar] [CrossRef]
- Aldosari, M.A. Dental magnification loupes: An update of the evidence. J. Contemp. Dent. Pract. 2021, 22, 310–315. [Google Scholar] [CrossRef]
- Güth, J.F.; Wallbach, J.; Stimmelmayr, M.; Gernet, W.; Beuer, F.; Edelhoff, D. Computer-aided evaluation of preparations for CAD/CAM-fabricated all-ceramic crowns. Clin. Oral Investig. 2013, 17, 1389–1395. [Google Scholar] [CrossRef] [PubMed]






| Position | Mean | Standard Deviation | Minimum | Maximum | ||
|---|---|---|---|---|---|---|
| 1 Day | t 1 | Sitting | 0.4175 | 0.1062006 | 0.3000 | 0.6000 |
| Supine | 0.4375 | 0.1410927 | 0.2500 | 0.6600 | ||
| T 1 | Sitting | 0.57625 | 9.999107E-02 | 0.4400 | 0.7000 | |
| Supine | 0.565 | 0.1393864 | 0.3200 | 0.7300 | ||
| t 2 | Sitting | 0.765 | 0.2173214 | 0.4000 | 0.9700 | |
| Supine | 0.90875 | 0.3267344 | 0.5000 | 1.550 | ||
| T 2 | Sitting | 0.6625 | 0.1263499 | 0.5500 | 0.8400 | |
| Supine | 0.6675 | 8.172253E-02 | 0.5200 | 0.8100 | ||
| 2 Day | t 1 | Sitting | 0.4675 | 8.972179E-02 | 0.3600 | 0.5800 |
| Supine | 0.41125 | 0.1664278 | 0.1500 | 0.6400 | ||
| T 1 | Sitting | 0.6175 | 0.2141928 | 0.3200 | 0.9400 | |
| Supine | 0.63625 | 0.1340509 | 0.4200 | 0.8000 | ||
| t 2 | Sitting | 0.68125 | 0.2269322 | 0.3500 | 0.9700 | |
| Supine | 0.745 | 0.3009034 | 0.3100 | 1.200 | ||
| T 2 | Sitting | 0.7025 | 0.1248714 | 0.4800 | 0.8700 | |
| Supine | 0.78375 | 0.1863896 | 0.4300 | 0.9600 | ||
| 3 Day | t 1 | Sitting | 0.425 | 0.155747 | 0.2500 | 0.7000 |
| Supine | 0.495 | 0.1247855 | 0.3400 | 0.6900 | ||
| T 1 | Sitting | 0.50125 | 0.1341042 | 0.2600 | 0.6500 | |
| Supine | 0.5225 | 0.1492601 | 0.2300 | 0.6800 | ||
| t 2 | Sitting | 0.83625 | 0.277434 | 0.3500 | 1.210 | |
| Supine | 0.855 | 0.2514529 | 0.5300 | 1.240 | ||
| T 2 | Sitting | 0.8825 | 0.1805349 | 0.6000 | 1.170 | |
| Supine | 0.79375 | 0.1204678 | 0.6200 | 0.9400 | ||
| 4 Day | t 1 | Sitting | 0.46625 | 0.1100568 | 0.2400 | 0.5800 |
| Supine | 0.385 | 0.1404076 | 0.1200 | 0.5200 | ||
| T 1 | Sitting | 0.65875 | 0.1582437 | 0.4300 | 0.9800 | |
| Supine | 0.525 | 7.111359E-02 | 0.4600 | 0.6600 | ||
| t 2 | Sitting | 0.81 | 0.2532644 | 0.5300 | 1.310 | |
| Supine | 1.09 | 0.2751104 | 0.7800 | 1.500 | ||
| T 2 | Sitting | 0.89875 | 0.1462324 | 0.7200 | 1.170 | |
| Supine | 0.725 | 0.1457983 | 0.5000 | 0.9200 | ||
| 5 Day | t 1 | Sitting | 0.52125 | 0.2118246 | 0.1900 | 0.7900 |
| Supine | 0.48125 | 0.1988134 | 0.1500 | 0.7600 | ||
| T 1 | Sitting | 0.5375 | 0.1239528 | 0.4100 | 0.7800 | |
| Supine | 0.45875 | 0.122991 | 0.3100 | 0.6800 | ||
| t 2 | Sitting | 0.83125 | 0.2511367 | 0.5300 | 1.220 | |
| Supine | 0.8825 | 0.3702027 | 0.4100 | 1.550 | ||
| T 2 | Sitting | 0.94625 | 0.2178425 | 0.3100 | 0.6800 | |
| Supine | 0.9 | 0.2200649 | 0.5700 | 1.210 |
| Participants | Width of the Chamfer (Mean Values) | Differences |
|---|---|---|
| t 1 | 0.450000 | - |
| t 2 | 0.840500 | + |
| T 1 | 0.559125 | + |
| T 2 | 0.79625 | + |
| Day | Operator | Position | Operator | Position | Difference |
|---|---|---|---|---|---|
| 1 | t 1 | Sitting | t 2 | Supine | −0.4913 *** |
| t 1 | Supine | t 2 | Supine | −0.4713 ** | |
| 3 | t 1 | Sitting | T 2 | Sitting | −0.4575 ** |
| t 1 | Sitting | t 2 | Supine | −0.4300 ** | |
| t 1 | Sitting | t 2 | Sitting | −0.4113 * | |
| T 1 | Sitting | T 2 | Sitting | −0.3813 * | |
| t 1 | Supine | T 2 | Sitting | −0.3875 * | |
| 4 | t 1 | Sitting | t 2 | Supine | −0.6238 *** |
| t 1 | Supine | T 2 | Sitting | −0.5138 *** | |
| t 1 | Supine | t 2 | Supine | −0.7050 *** | |
| T 1 | Supine | t 2 | Supine | −0.5650 *** | |
| t 1 | Sitting | T 2 | Sitting | −0.4325 ** | |
| t 1 | Supine | t 2 | Sitting | −0.4250 ** | |
| T 1 | Sitting | t 2F | Supine | −0.4313 ** | |
| 5 | t 1 | Sitting | T 2 | Sitting | −0.4250 ** |
| t 1 | Sitting | T 2 | Supine | −0.3788 * | |
| t 1 | Supine | T 2 | Sitting | −0.4650 ** | |
| t 1 | Supine | T 2 | Supine | −0.4188 * | |
| t 1 | Supine | t 2 | Supine | −0.4013 * | |
| T 1 | Sitting | T 2 | Sitting | −0.4088 * | |
| T 1 | Supine | T 2 | Sitting | −0.4875 *** | |
| T 1 | Supine | T 2 | Supine | −0.4413 ** | |
| T1 | Supine | t 2 | Supine | −0.4238 ** |
| Day | Position | Operator | p Value |
|---|---|---|---|
| 1 | Sitting | t1 | 0.063994 |
| t2 | 0.010706 | ||
| T1 | 0.067921 | ||
| T2 | 0.008313 | ||
| Supine | t1 | 0.250468 | |
| t2 | 0.009490 | ||
| T1 | 0.228685 | ||
| T2 | 0.000665 | ||
| 2 | Sitting | t1 | 0.339675 |
| t2 | 0.058413 | ||
| T1 | 0.164699 | ||
| T2 | 0.002523 | ||
| Supine | t1 | 0.175214 | |
| t2 | 0.054753 | ||
| T1 | 0.023827 | ||
| T2 | 0.003541 | ||
| 3 | Sitting | t1 | 0.215394 |
| t2 | 0.011014 | ||
| T1 | 0.979703 | ||
| T2 | 0.000546 | ||
| Supine | t1 | 0.912950 | |
| t2 | 0.005235 | ||
| T1 | 0.682645 | ||
| T2 | 0.000232 | ||
| 4 | Sitting | t1 | 0.414484 |
| t2 | 0.010518 | ||
| T1 | 0.025135 | ||
| T2 | 0.000115 | ||
| Supine | t1 | 0.053662 | |
| t2 | 0.000508 | ||
| T1 | 0.353181 | ||
| T2 | 0.003294 | ||
| 5 | Sitting | t1 | 0.784815 |
| t2 | 0.007352 | ||
| T1 | 0.420487 | ||
| T2 | 0.000668 | ||
| Supine | t1 | 0.797351 | |
| t2 | 0.022264 | ||
| T1 | 0.374402 | ||
| T2 | 0.001337 |
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2023 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Jánosi, K.M.; Cerghizan, D.; Rétyi, Z.; Kovács, A.; Szász, A.; Mureșan, I.; Albu, A.I.; Hănțoiu, L.G. Influence of the Operator`s Experience, Working Time, and Working Position on the Quality of the Margin Width: In Vitro Study. Medicina 2023, 59, 244. https://doi.org/10.3390/medicina59020244
Jánosi KM, Cerghizan D, Rétyi Z, Kovács A, Szász A, Mureșan I, Albu AI, Hănțoiu LG. Influence of the Operator`s Experience, Working Time, and Working Position on the Quality of the Margin Width: In Vitro Study. Medicina. 2023; 59(2):244. https://doi.org/10.3390/medicina59020244
Chicago/Turabian StyleJánosi, Kinga Mária, Diana Cerghizan, Zsigmond Rétyi, Alpár Kovács, Andrea Szász, Izabella Mureșan, Aurița Ioana Albu, and Liana Georgiana Hănțoiu. 2023. "Influence of the Operator`s Experience, Working Time, and Working Position on the Quality of the Margin Width: In Vitro Study" Medicina 59, no. 2: 244. https://doi.org/10.3390/medicina59020244
APA StyleJánosi, K. M., Cerghizan, D., Rétyi, Z., Kovács, A., Szász, A., Mureșan, I., Albu, A. I., & Hănțoiu, L. G. (2023). Influence of the Operator`s Experience, Working Time, and Working Position on the Quality of the Margin Width: In Vitro Study. Medicina, 59(2), 244. https://doi.org/10.3390/medicina59020244








