The Prone Lateral Approach for Lumbar Fusion—A Review of the Literature and Case Series
Abstract
1. Introduction
2. The Prone Lateral Approach
3. Our Initial Institutional Experience
Patient Selection and Data Collection
4. Case Examples
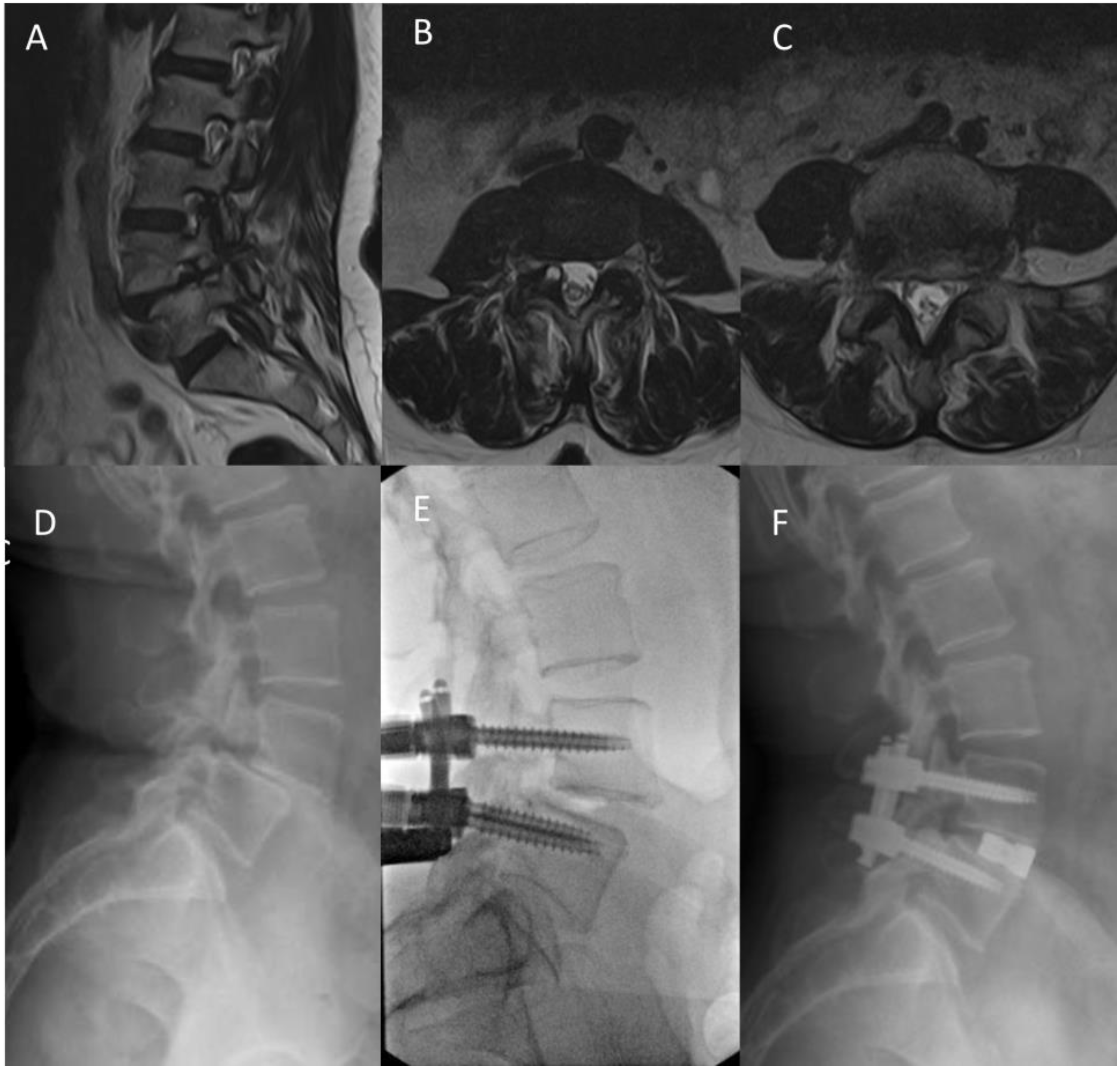
4.1. Case 1
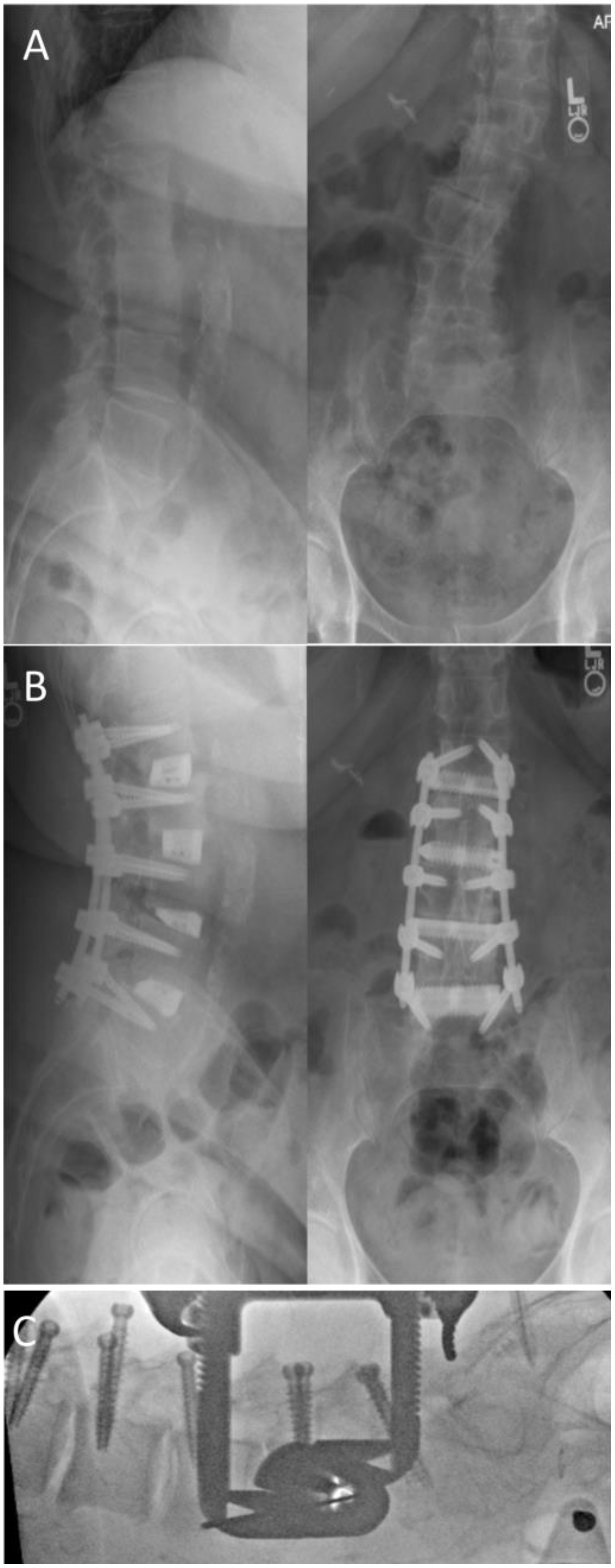
4.2. Case 2
5. Future Directions
6. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Conflicts of Interest
References
- McAfee, P.C.; Phillips, F.M.; Andersson, G.; Buvenenadran, A.; Kim, C.W.; Lauryssen, C.; Isaacs, R.E.; Youssef, J.A.; Brodke, D.S.; Cappuccino, A.; et al. Minimally Invasive Spine Surgery. Spine 2010, 35, S271–S273. Available online: https://journals.lww.com/spinejournal/Fulltext/2010/12151/Minimally_Invasive_Spine_Surgery.1.aspx (accessed on 9 July 2022). [CrossRef] [PubMed]
- Talia, A.J.; Wong, M.L.; Lau, H.C.; Kaye, A.H. Comparison of the different surgical approaches for lumbar interbody fusion. J. Clin. Neurosci. 2015, 22, 243–251. [Google Scholar] [CrossRef] [PubMed]
- Ozgur, B.M.; Aryan, H.E.; Pimenta, L.; Taylor, W.R. Extreme Lateral Interbody Fusion (XLIF): A novel surgical technique for anterior lumbar interbody fusion. Spine J. 2006, 6, 435–443. [Google Scholar] [CrossRef] [PubMed]
- Singh, H.; Mallozzi, S. Role of Lateral Fusion in Deformity Surgery. Int. J. Spine Surg. 2022, 16, S33. [Google Scholar] [CrossRef]
- Pimenta, L.; Fortti, F.; Oliveira, L.; Marchi, L.; Jensen, R.; Coutinho, E.; Amaral, R. Anterior column realignment following lateral interbody fusion for sagittal deformity correction. Eur. J. Orthop. Surg. Traumatol. 2015, 25, 29–33. [Google Scholar] [CrossRef]
- Kono, Y.; Gen, H.; Sakuma, Y.; Koshika, Y. Comparison of Clinical and Radiologic Results of Mini-Open Transforaminal Lumbar Interbody Fusion and Extreme Lateral Interbody Fusion Indirect Decompression for Degenerative Lumbar Spondylolisthesis. Asian Spine J. 2018, 12, 356–364. [Google Scholar] [CrossRef]
- Saadeh, Y.S.; Joseph, J.R.; Smith, B.W.; Kirsch, M.J.; Sabbagh, A.M.; Park, P. Comparison of Segmental Lordosis and Global Spinopelvic Alignment After Single-Level Lateral Lumbar Interbody Fusion or Transforaminal Lumbar Interbody Fusion. World Neurosurg. 2019, 126, e1374–e1378. [Google Scholar] [CrossRef]
- Watkins, R.G.; Hanna, R.; Chang, D.; Watkins, R.G. Sagittal Alignment After Lumbar Interbody Fusion: Comparing Anterior, Lateral, and Transforaminal Approaches. J. Spinal Disord. Tech. 2014, 27, 253–256. [Google Scholar] [CrossRef]
- Isaacs, R.E.; Sembrano, J.; Tohmeh, A.G. Two-Year Comparative Outcomes of MIS Lateral and MIS Transforaminal Interbody Fusion in the Treatment of Degenerative Spondylolisthesis. Part II: Radiographic Findings. Spine 2016, 41, S133–S144. [Google Scholar] [CrossRef]
- Lykissas, M.G.; Aichmair, A.; Hughes, A.P.; Sama, A.A.; Lebl, D.R.; Taher, F.; Du, J.Y.; Cammisa, F.P.; Girardi, F.P. Nerve injury after lateral lumbar interbody fusion: A review of 919 treated levels with identification of risk factors. Spine J. 2014, 14, 749–758. [Google Scholar] [CrossRef]
- Alluri, R.; Mok, J.K.; Vaishnav, A.; Shelby, T.; Sivaganesan, A.; Hah, R.; Qureshi, S.A. Intraoperative Neuromonitoring During Lateral Lumbar Interbody Fusion. Neurospine 2021, 18, 430–436. [Google Scholar] [CrossRef]
- Uribe, J.S.; Deukmedjian, A.R. Visceral, vascular, and wound complications following over 13,000 lateral interbody fusions: A survey study and literature review. Eur. Spine J. 2015, 24, 386–396. [Google Scholar] [CrossRef] [PubMed]
- Guiroy, A.; Carazzo, C.; Camino-Willhuber, G.; Gagliardi, M.; Fernandes-Joaquim, A.; Cabrera, J.P.; Menezes, C.; Asghar, J. Single-Position Surgery versus Lateral-Then-Prone-Position Circumferential Lumbar Interbody Fusion: A Systematic Literature Review. World Neurosurg. 2021, 151, e379–e386. [Google Scholar] [CrossRef] [PubMed]
- Lopez, G.; Sayari, A.J.; Phillips, F. Single-Position Anterior Column Lateral Lumbar Interbody Fusion. Int. J. Spine Surg. 2022, 16, S17. [Google Scholar] [CrossRef] [PubMed]
- Hiyama, A.; Katoh, H.; Sakai, D.; Sato, M.; Tanaka, M.; Watanabe, M. Comparison of radiological changes after single- position versus dual- position for lateral interbody fusion and pedicle screw fixation. BMC Musculoskelet. Disord. 2019, 20, 601. [Google Scholar] [CrossRef]
- Buckland, A.J.; Ashayeri, K.; Leon, C.; Manning, J.; Eisen, L.; Medley, M.; Protopsaltis, T.S.; Thomas, J.A. Single position circumferential fusion improves operative efficiency, reduces complications and length of stay compared with traditional circumferential fusion. Spine J. 2021, 21, 810–820. [Google Scholar] [CrossRef]
- Ziino, C.; Konopka, J.A.; Ajiboye, R.M.; Ledesma, J.B.; Koltsov, J.C.B.; Cheng, I. Single position versus lateral-then-prone positioning for lateral interbody fusion and pedicle screw fixation. J. Spine Surg. 2018, 4, 717–724. [Google Scholar] [CrossRef]
- Ashayeri, K.; Leon, C.; Tigchelaar, S.; Fatemi, P.; Follett, M.; Cheng, I.; Thomas, J.A.; Medley, M.; Braly, B.; Kwon, B.; et al. Single position lateral decubitus anterior lumbar interbody fusion (ALIF) and posterior fusion reduces complications and improves perioperative outcomes compared with traditional anterior-posterior lumbar fusion. Spine J. 2022, 22, 419–428. [Google Scholar] [CrossRef]
- Pimenta, L.; Taylor, W.R.; Stone, L.E.; Wali, A.R.; Santiago-Dieppa, D.R. Prone Transpsoas Technique for Simultaneous Single-Position Access to the Anterior and Posterior Lumbar Spine. Oper. Neurosurg. 2021, 20, E5–E12. Available online: https://journals.lww.com/onsonline/Fulltext/2021/01000/Prone_Transpsoas_Technique_for_Simultaneous.18.aspx (accessed on 21 September 2022). [CrossRef]
- Walker, C.T.; Farber, S.H.; Gandhi, S.; Godzik, J.; Turner, J.D.; Uribe, J.S. Single-Position Prone Lateral Interbody Fusion Improves Segmental Lordosis in Lumbar Spondylolisthesis. World Neurosurg. 2021, 151, e786–e792. [Google Scholar] [CrossRef]
- Pimenta, L.; Pokorny, G.; Amaral, R.; Ditty, B.; Batista, M.; Moriguchi, R.; Melo Filho, F.; Taylor, W.R. Single-Position Prone Transpsoas Lateral Interbody Fusion Including L4L5: Early Postoperative Outcomes. World Neurosurg. 2021, 149, e664–e668. [Google Scholar] [CrossRef] [PubMed]
- Alluri, R.; Clark, N.; Sheha, E.; Shafi, K.; Geiselmann, M.; Kim, H.J.; Qureshi, S.; Dowdell, J. Location of the Femoral Nerve in the Lateral Decubitus Versus Prone Position. Glob. Spine J. 2021, 219256822110491. [Google Scholar] [CrossRef] [PubMed]
- Amaral, R.; Daher, M.T.; Pratali, R.; Arnoni, D.; Pokorny, G.; Rodrigues, R.; Batista, M.; Fortuna, P.P.; Pimenta, L.; Herrero, C.F.P.; et al. The Effect of Patient Position on Psoas Morphology and in Lumbar Lordosis. World Neurosurg. 2021, 153, e131–e140. [Google Scholar] [CrossRef] [PubMed]
- Walker, C.T.; Farber, S.H.; Cole, T.S.; Xu, D.S.; Godzik, J.; Whiting, A.C.; Hartman, C.; Porter, R.W.; Turner, J.D.; Uribe, J. Complications for minimally invasive lateral interbody arthrodesis: A systematic review and meta-analysis comparing prepsoas and transpsoas approaches. J. Neurosurg. Spine 2019, 30, 446–460. [Google Scholar] [CrossRef]
- Lamartina, C.; Berjano, P. Prone single-position extreme lateral interbody fusion (Pro-XLIF): Preliminary results. Eur. Spine J. 2020, 29, 6–13. [Google Scholar] [CrossRef]
- Cummock, M.D.; Vanni, S.; Levi, A.D.; Yu, Y.; Wang, M.Y. An analysis of postoperative thigh symptoms after minimally invasive transpsoas lumbar interbody fusion: Clinical article. J. Neurosurg. Spine 2011, 15, 11–18. [Google Scholar] [CrossRef]
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2023 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Barkay, G.; Wellington, I.; Mallozzi, S.; Singh, H.; Moss, I.L. The Prone Lateral Approach for Lumbar Fusion—A Review of the Literature and Case Series. Medicina 2023, 59, 251. https://doi.org/10.3390/medicina59020251
Barkay G, Wellington I, Mallozzi S, Singh H, Moss IL. The Prone Lateral Approach for Lumbar Fusion—A Review of the Literature and Case Series. Medicina. 2023; 59(2):251. https://doi.org/10.3390/medicina59020251
Chicago/Turabian StyleBarkay, Gal, Ian Wellington, Scott Mallozzi, Hardeep Singh, and Isaac L. Moss. 2023. "The Prone Lateral Approach for Lumbar Fusion—A Review of the Literature and Case Series" Medicina 59, no. 2: 251. https://doi.org/10.3390/medicina59020251
APA StyleBarkay, G., Wellington, I., Mallozzi, S., Singh, H., & Moss, I. L. (2023). The Prone Lateral Approach for Lumbar Fusion—A Review of the Literature and Case Series. Medicina, 59(2), 251. https://doi.org/10.3390/medicina59020251




