The Course and Surgical Treatment of Acute Appendicitis during the First and Second Wave of the COVID-19 Pandemic: A Retrospective Analysis in University Affiliated Hospital in Latvia
Abstract
:1. Introduction
2. Materials and Methods
2.1. Emergency Department Pathway for Patients with Acute Appendicitis
2.2. Statistical Analysis
3. Results
3.1. Patient Demographics
3.2. Diagnostic Procedures
3.3. Surgical Approach and Time until Treatment
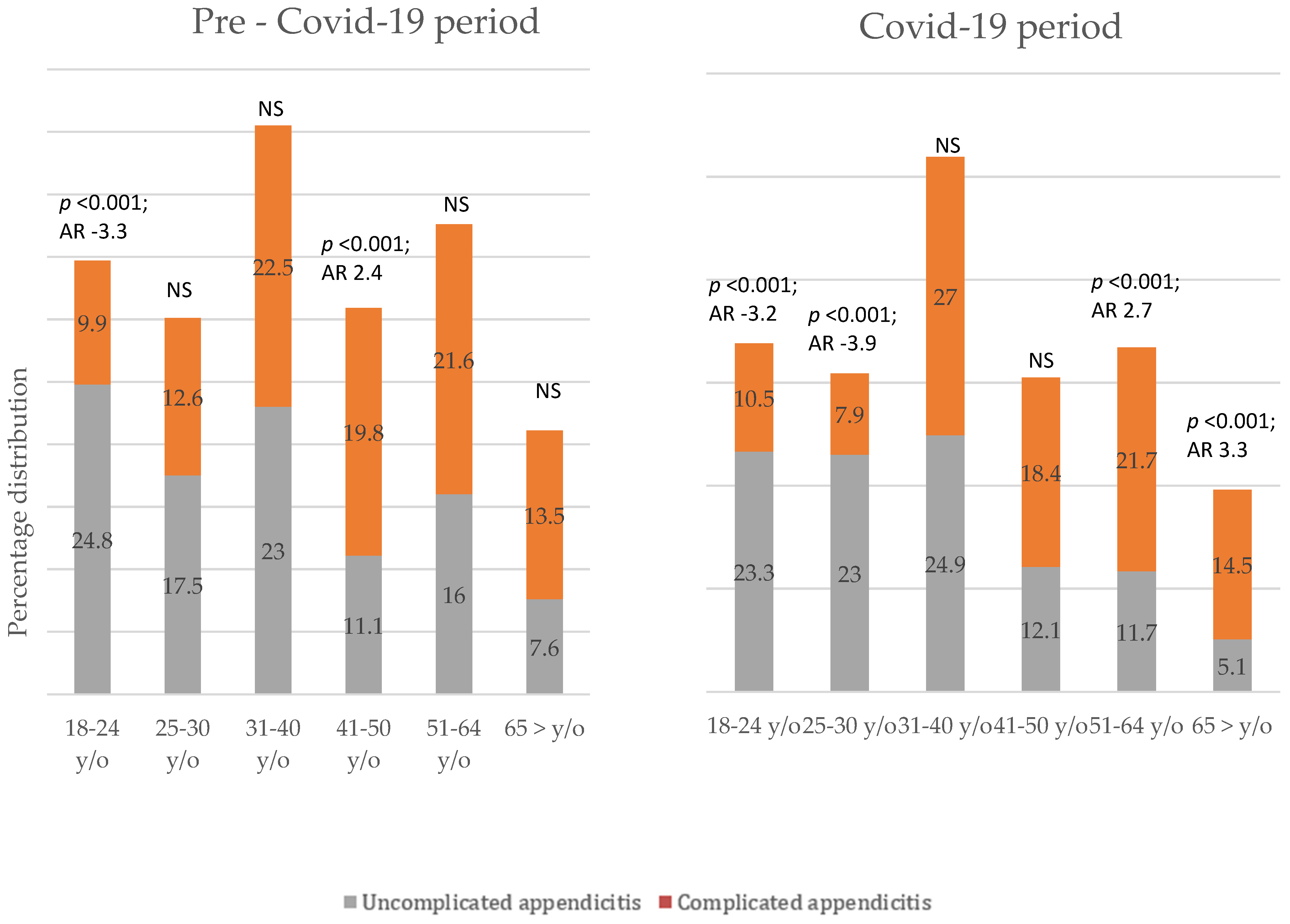
3.4. Severity of Acute Appendicitis
3.5. Outcomes
4. Discussion
Strengths and Limitations
5. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Conflicts of Interest
References
- Li, Q.; Guan, X.; Wu, P.; Wang, X.; Zhou, L.; Tong, Y.; Ren, R.; Leung, K.S.; Lau, E.H.; Wong, J.Y.; et al. Early Transmission Dynamics in Wuhan, China, of Novel Coronavirus-Infected Pneumonia. N. Engl. J. Med. 2020, 382, 1199–1207. Available online: https://www.ncbi.nlm.nih.gov/pubmed/31995857 (accessed on 7 April 2021). [CrossRef] [PubMed]
- Wuhan City Health Committee (WCHC). Wuhan Municipal Health and Health Commission’s Briefing on the Current Pneumonia Epidemic Situation in Our City 2019. Available online: https://wjw.wuhan.gov.cn/front/web/showDetail/2019123108989 (accessed on 7 April 2021).
- Tan, W.; Zhao, X.; Ma, X.; Wang, W.; Niu, P.; Xu, W.; Gao, G.F.; Wu, G. A Novel Coronavirus Genome Identified in a Cluster of Pneumonia Cases—Wuhan, China 2019−2020. China CDC Wkly. 2020, 2, 61–62. [Google Scholar] [CrossRef] [PubMed]
- Zhu, N.; Zhang, D.; Wang, W.; Li, X.; Yang, B.; Song, J.; Zhao, X.; Huang, B.; Shi, W.; Lu, R.; et al. A Novel Coronavirus from Patients with Pneumonia in China, 2019. N. Engl. J. Med. 2020, 382, 727–733. [Google Scholar] [CrossRef] [PubMed]
- WHO. WHO Director-General’s Remarks at the Media Briefing on 2019-nCoV on 11 February 2020. 2020. Available online: https://www.who.int/director-general/speeches/detail/who-director-general-s-remarks-at-the-media-briefing-on-2019-ncov-on-11-february-2020 (accessed on 7 April 2021).
- EU Fundamental Rights Agency. Coronavirus COVID-19 Outbreak in the EU Fundamental Rights Implications. 2020. Available online: https://fra.europa.eu/sites/default/files/fra_uploads/latvia-report-covid-19-april-2020_en.pdf (accessed on 7 April 2021).
- COVID-19 Statistics in Latvia. Available online: https://www.spkc.gov.lv/lv/covid-19-statistika (accessed on 23 January 2023).
- Humes, D.J.; Simpson, J. Acute Appendicitis. BMJ 2006, 333, 530–534. Available online: https://www.ncbi.nlm.nih.gov/pmc/articles/PMC1562475/ (accessed on 3 November 2019). [CrossRef] [PubMed]
- Papandria, D.; Lardaro, T.; Rhee, D.; Ortega, G.; Gorgy, A.; Makary, M.A.; Abdullah, F. Risk Factors for Conversion from Laparoscopic to Open Surgery: Analysis of 2138 Converted Operations in the American College of Surgeons National Surgical Quality Improvement Program. Am. Surg. 2013, 79, 914–921. Available online: https://pubmed.ncbi.nlm.nih.gov/24069991/ (accessed on 24 August 2022). [CrossRef] [PubMed]
- Flum, D.R. Acute Appendicitis—Appendectomy or the “Antibiotics First” Strategy. N. Engl. J. Med. 2015, 372, 1937–1943. [Google Scholar] [CrossRef] [PubMed]
- Moletta, L.; Pierobon, E.S.; Capovilla, G.; Costantini, M.; Salvador, R.; Merigliano, S.; Valmasoni, M. International guidelines and recommendations for surgery during COVID-19 pandemic: A Systematic Review. Int. J. Surg. 2020, 79, 180–188. [Google Scholar] [CrossRef] [PubMed]
- Collard, M.; Lakkis, Z.; Loriau, J.; Mege, D.; Sabbagh, C.; Lefevre, J.; Maggiori, L. Antibiotics alone as an alternative to appendectomy for uncomplicated acute appendicitis in adults: Changes in treatment modalities related to the COVID-19 health crisis. J. Visc. Surg. 2020, 157, S33–S42. [Google Scholar] [CrossRef] [PubMed]
- Macrotrends. Riga, Latvia Metro Area Population 1950–2022. Available online: http://www.macrotrends.net/cities/21778/riga/population (accessed on 24 August 2022).
- Gomes, C.A.; Sartelli, M.; Di Saverio, S.; Ansaloni, L.; Catena, F.; Coccolini, F.; Inaba, K.; Demetriades, D.; Gomes, F.C.; Gomes, C.C. Acute appendicitis: Proposal of a new comprehensive grading system based on clinical, imaging and laparoscopic findings. World J. Emerg. Surg. 2015, 10, 1–6. [Google Scholar] [CrossRef] [PubMed]
- STROBE—Strengthening the Reporting of Observational Studies in Epidemiology. Available online: www.strobe-statement.org (accessed on 7 April 2021).
- Rausei, S.; Ferrara, F.; Zurleni, T.; Frattini, F.; Chiara, O.; Pietrabissa, A.; Sarro, G. Dramatic decrease of surgical emergencies during COVID-19 outbreak. J. Trauma: Inj. Infect. Crit. Care 2020, 89, 1085–1091. [Google Scholar] [CrossRef] [PubMed]
- Maneck, M.; Günster, C.; Meyer, H.-J.; Heidecke, C.-D.; Rolle, U. Influence of COVID-19 Confinement Measures on Appendectomies in Germany—A Claims Data Analysis of 9797 Patients. Langenbeck’s Arch. Surg. 2020, 406, 385–391. Available online: https://pubmed.ncbi.nlm.nih.gov/33277682/ (accessed on 24 August 2022). [CrossRef] [PubMed]
- Köhler, F.; Acar, L.; Berg, A.V.D.; Flemming, S.; Kastner, C.; Müller, S.; Diers, J.; Germer, C.-T.; Lock, J.F.; L’Hoest, H.; et al. Impact of the COVID-19 Pandemic on Appendicitis Treatment in Germany—A Population-Based Analysis. Langenbeck’s Arch. Surg. 2021, 406, 377–383. Available online: https://pubmed.ncbi.nlm.nih.gov/33420517/ (accessed on 24 August 2022). [CrossRef] [PubMed]
- Kibbe, M.R. Surgery and COVID-19. JAMA 2020, 324, 1151. [Google Scholar] [CrossRef] [PubMed]
- Yousman, L.C.; Khunte, A.; Hsiang, W.; Jain, S.; Forman, H.; Wiznia, D. Urgent care center wait times increase for COVID-19 results in August 2020, with rapid testing availability limited. BMC Heal. Serv. Res. 2021, 21, 1–5. [Google Scholar]
- Orthopoulos, G.; Santone, E.; Izzo, F.; Tirabassi, M.; Pérez-Caraballo, A.M.; Corriveau, N.; Jabbour, N. Increasing incidence of complicated appendicitis during COVID-19 pandemic. Am. J. Surg. 2021, 221, 1056–1060. [Google Scholar] [CrossRef] [PubMed]
- Puche-Sanz, I.; Sabio-Bonilla, A.; Sánchez-Conde, V.; Jiménez-Domínguez, A.C.; Tamayo-Gómez, A.; Vila-Braña, P.; Vázquez-Alonso, F.; Rivas, J.G.; Gómez-Gómez, E.; Campos-Juanatey, F.; et al. Emergency Surgery during COVID-19 Pandemia. Arch. Esp. Urol. 2020, 73, 353–359. Available online: https://pubmed.ncbi.nlm.nih.gov/32538804/ (accessed on 24 August 2022). [PubMed]

| Variables | Patients during Pre-COVID-19 n = 454 | Patients during COVID-19 n = 409 | p Value |
|---|---|---|---|
| n (%) | n (%) | ||
| Age, median (IQR) | 35 (51–26) | 35 (49–27) | NS |
| Age groups | |||
| 18–24 | 96 (21.15) | 76 (18.58) | NS |
| 24–30 | 74 (16.30) | 71 (17.36) | NS |
| 31–40 | 104 (22.91) | 105 (25.67) | NS |
| 41–50 | 60 (13.22) | 59 (14.43) | NS |
| 50–64 | 79 (17.40) | 63 (15.40) | NS |
| >65 | 41 (9.03) | 35 (8.56) | NS |
| Gender | |||
| Male | 218 (48) | 201 (49.1) | NS |
| Female | 236 (52) | 208 (50.9) | NS |
| Severity of appendicitis | |||
| Uncomplicated appendicitis | 343 (75.6) | 257 (62.8) | <0.001 |
| Complicated appendicitis | 111 (24.4) | 152 (37.2) | <0.001 |
| Patients during Pre-COVID-19 n = 454 | Patients during COVID-19 n = 409 | p Value | |
|---|---|---|---|
| n (%) | n (%) | ||
| US | 324 (71.4) | 275 (67.2) | NS |
| CT | 15 (3.3) | 19 (4.6) | NS |
| US and CT | 115 (25.3) | 115 (28.1) | NS |
| Time | Patients during Pre-COVID-19 n = 454 | Patients during COVID-19 n = 409 | p Value |
|---|---|---|---|
| n (%) | n (%) | ||
| Patients that had only US | |||
| <6 h | 162 (50) | 149 (54.2) | NS |
| 6–24 h | 151 (46.6) | 118 (42.9) | NS |
| >24 h | 11 (3.4) | 8 (2.9) | NS |
| Patients that had only CT scan | |||
| <6 h | 7 (46.7) | 10 (52.6) | NS |
| 6–24 h | 6 (40) | 7 (36.8) | NS |
| >24 h | 2 (13.3) | 2 (10.5) | NS |
| Patients that had US and CT scan | |||
| <6 h | 38 (33.0) | 38 (33) | NS |
| 6–24 h | 60 (52.2) | 63 (54.8) | NS |
| >24 h | 17 (14.8) | 14 (12.2) | NS |
| Variable | Patients during Pre-COVID-19 n = 454 | Patients during COVID-19 n = 409 | p Value |
|---|---|---|---|
| n (%) | n (%) | ||
| Overall hospital stay (days), median (IQR) | 4 (5–3) | 3 (5–3) | NS |
| Overall hospital stay | |||
| <3 days | 214 (47.10) | 207 (50.6) | NS |
| 4–6 days | 191 (42.10) | 166 (40.6) | NS |
| >7 days | 49 (10.80) | 36 (8.8) | NS |
| Admission to ICU (number of patients) | 10 (2.2) | 13 (3.2) | NS |
| Mortality | 1 (0.2) | 0 (0) | NS |
| Pre-COVID-19 Period | COVID-19 Period | |||
|---|---|---|---|---|
| R | p Value | R | p Value | |
| All patients | ||||
| Overall hospital stay | 0.312 | <0.001 | 0.348 | <0.001 |
| Uncomplicated appendicitis | ||||
| Overall hospital stay | 0.191 | <0.001 | 0.185 | 0.003 |
| Local peritonitis | ||||
| Overall hospital stay | 0.405 | <0.001 | 0.396 | <0.001 |
| Generalized peritonitis | ||||
| Overall hospital stays | 0.48 | 0.06 | 0.497 | 0.012 |
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2023 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Lescinska, A.M.; Sondore, E.; Ptasnuka, M.; Mukans, M.; Plaudis, H. The Course and Surgical Treatment of Acute Appendicitis during the First and Second Wave of the COVID-19 Pandemic: A Retrospective Analysis in University Affiliated Hospital in Latvia. Medicina 2023, 59, 295. https://doi.org/10.3390/medicina59020295
Lescinska AM, Sondore E, Ptasnuka M, Mukans M, Plaudis H. The Course and Surgical Treatment of Acute Appendicitis during the First and Second Wave of the COVID-19 Pandemic: A Retrospective Analysis in University Affiliated Hospital in Latvia. Medicina. 2023; 59(2):295. https://doi.org/10.3390/medicina59020295
Chicago/Turabian StyleLescinska, Anna Marija, Elza Sondore, Margarita Ptasnuka, Maksims Mukans, and Haralds Plaudis. 2023. "The Course and Surgical Treatment of Acute Appendicitis during the First and Second Wave of the COVID-19 Pandemic: A Retrospective Analysis in University Affiliated Hospital in Latvia" Medicina 59, no. 2: 295. https://doi.org/10.3390/medicina59020295







