Laboratory Findings in Children with Excess Body Weight in Romania
Abstract
1. Introduction
2. Methods
3. Results
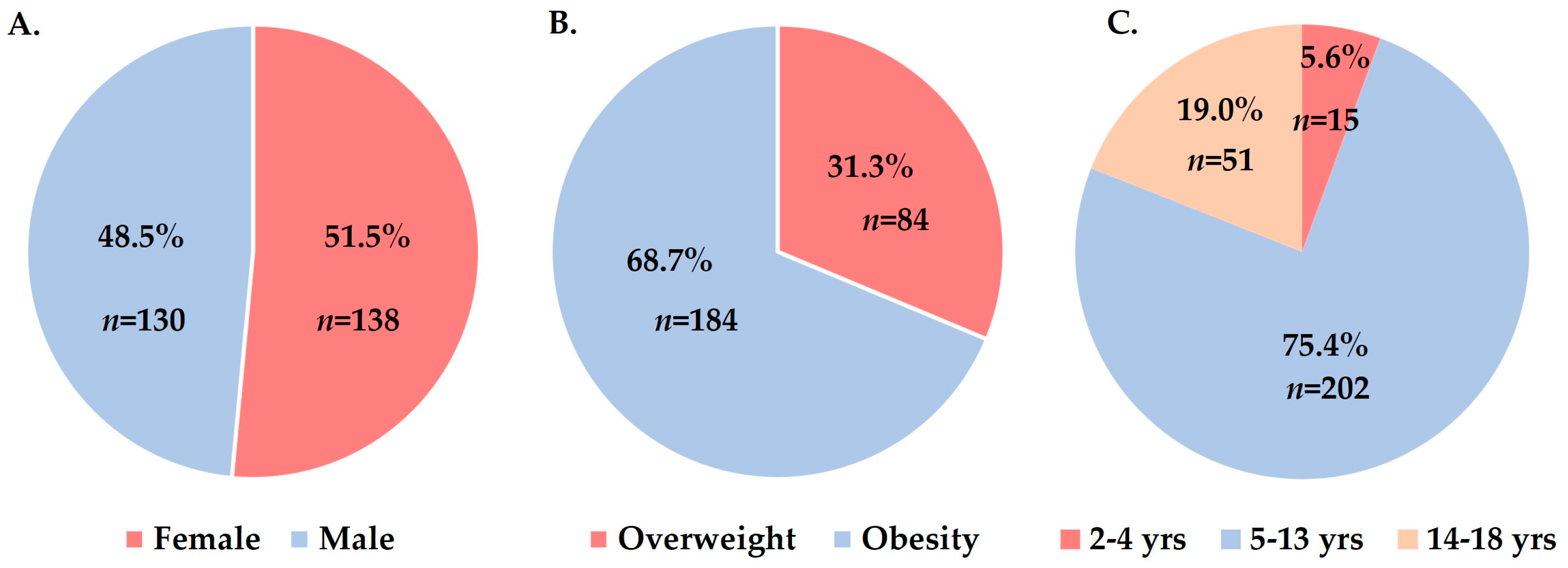
3.1. General Data Analysis
3.2. Analysis of Data According to Sex and Age Group
3.3. Data Analysis: Overweight vs. Obesity
4. Discussion
5. Conclusions
Supplementary Materials
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Conflicts of Interest
References
- Di Cesare, M.; Sorić, M.; Bovet, P.; Miranda, J.J.; Bhutta, Z.; Stevens, G.A.; Laxmaiah, A.; Kengne, A.-P.; Bentham, J. The epidemiological burden of obesity in childhood: A worldwide epidemic requiring urgent action. BMC Med. 2019, 17, 212. [Google Scholar]
- Jha, S.; Mehendale, A.M. Increased Incidence of Obesity in Children and Adolescents Post-COVID-19 Pandemic: A Review Article. Cureus 2022, 14, e29348. [Google Scholar]
- Palermi, S.; Vecchiato, M.; Pennella, S.; Marasca, A.; Spinelli, A.; De Luca, M.; De Martino, L.; Fernando, F.; Sirico, F.; Biffi, A. The Impact of the COVID-19 Pandemic on Childhood Obesity and Lifestyle-A Report from Italy. Pediatr. Rep. 2022, 14, 410–418. [Google Scholar] [CrossRef]
- Valenzise, M.; D’Amico, F.; Cucinotta, U.; Lugarà, C.; Zirilli, G.; Zema, A.; Wasniewska, M.; Pajno, G.B. The lockdown effects on a pediatric obese population in the COVID-19 era. Ital. J. Pediatr. 2021, 47, 209. [Google Scholar] [CrossRef]
- Centers for Disease Control and Prevention. Childhood Obesity Facts 2022. Available online: https://www.cdc.gov/obesity/data/childhood.html (accessed on 20 December 2022).
- Europe WHO. Childhood Obesity in European Region Remains High: New WHO Report Presents Latest Country Data 2022. Available online: https://www.who.int/europe/news/item/08-11-2022-childhood-obesity-in-european-region-remains-high--new-who-report-presents-latest-country-data (accessed on 20 December 2022.).
- Sahoo, K.; Sahoo, B.; Choudhury, A.K.; Sofi, N.Y.; Kumar, R.; Bhadoria, A.S. Childhood obesity: Causes and consequences. J. Fam. Med. Prim. Care 2015, 4, 187–192. [Google Scholar]
- Fang, K.; Mu, M.; Liu, K.; He, Y. Screen time and childhood overweight/obesity: A systematic review and meta-analysis. Child Care Health Dev. 2019, 45, 744–753. [Google Scholar]
- Loos, R.J.F.; Yeo, G.S.H. The genetics of obesity: From discovery to biology. Nat. Rev. Genet. 2022, 23, 120–133. [Google Scholar] [CrossRef]
- Miron, V.D.; Bar, G.; Filimon, C.; Gaidamut, V.A.; Craiu, M. Monitoring of Excess Body Weight in Children in the Emergency Department of a Tertiary Pediatric Hospital in Bucharest, Romania. Maedica 2021, 16, 389–393. [Google Scholar] [CrossRef]
- Barbu, C.G.; Teleman, M.D.; Albu, A.I.; Sirbu, A.E.; Martin, S.C.; Bancescu, A.; Fica, S.V. Obesity and eating behaviors in school children and adolescents -data from a cross sectional study from Bucharest, Romania. BMC Public Health 2015, 15, 206. [Google Scholar] [CrossRef]
- Simmonds, M.; Llewellyn, A.; Owen, C.G.; Woolacott, N. Predicting adult obesity from childhood obesity: A systematic review and meta-analysis. Obes. Rev. 2016, 17, 95–107. [Google Scholar] [CrossRef]
- Centers for Disease Control and Prevention. BMI Percentile Calculator for Child and Teen 2022. Available online: https://www.cdc.gov/healthyweight/bmi/calculator.html (accessed on 14 December 2022).
- Ghaben, A.L.; Scherer, P.E. Adipogenesis and metabolic health. Nat. Rev. Mol. Cell Biol. 2019, 20, 242–258. [Google Scholar]
- Uribe-Querol, E.; Rosales, C. Neutrophils Actively Contribute to Obesity-Associated Inflammation and Pathological Complications. Cells 2022, 11, 1883. [Google Scholar]
- Herishanu, Y.; Rogowski, O.; Polliack, A.; Marilus, R. Leukocytosis in obese individuals: Possible link in patients with unexplained persistent neutrophilia. Eur. J. Haematol. 2006, 76, 516–520. [Google Scholar] [CrossRef]
- Weir, A.B.; Lewis, J.B., Jr.; Arteta-Bulos, R. Chronic idiopathic neutrophilia: Experience and recommendations. South Med. J. 2011, 104, 99–504. [Google Scholar] [CrossRef]
- Kim, J.A.; Park, H.S. White blood cell count and abdominal fat distribution in female obese adolescents. Metabolism 2008, 57, 1375–1379. [Google Scholar] [CrossRef]
- Dixon, J.B.; O’Brien, P.E. Obesity and the white blood cell count: Changes with sustained weight loss. Obes. Surg. 2006, 16, 251–257. [Google Scholar]
- Ohshita, K.; Yamane, K.; Hanafusa, M.; Mori, H.; Mito, K.; Okubo, M.; Hara, H.; Kohno, N. Elevated White Blood Cell Count in Subjects with Impaired Glucose Tolerance. Diabetes Care 2004, 27, 491–496. [Google Scholar] [CrossRef]
- Marginean, C.O.; Melit, L.E.; Ghiga, D.V.; Marginean, M.O. Early Inflammatory Status Related to Pediatric Obesity. Front. Pediatr. 2019, 7, 241. [Google Scholar]
- Samocha-Bonet, D.; Justo, D.; Rogowski, O.; Saar, N.; Abu-Abeid, S.; Shenkerman, G.; Shapira, I.; Berliner, S.; Tomer, A. Platelet Counts and Platelet Activation Markers in Obese Subjects. Mediat. Inflamm. 2008, 2008, 834153. [Google Scholar]
- Marquardt, L.; Ruf, A.; Mansmann, U.; Winter, R.; Schuler, M.; Buggle, F.; Mayer, H.; Grau, A.J. Course of Platelet Activation Markers After Ischemic Stroke. Stroke 2002, 33, 2570–2574. [Google Scholar]
- Jeong, H.R.; Lee, H.S.; Shim, Y.S.; Hwang, J.S. Positive Associations between Body Mass Index and Hematological Parameters, Including RBCs, WBCs, and Platelet Counts, in Korean Children and Adolescents. Children 2022, 9, 109. [Google Scholar]
- Ausk, K.J.; Ioannou, G.N. Is obesity associated with anemia of chronic disease? A population-based study. Obesity 2008, 16, 2356–2361. [Google Scholar]
- Pinhas-Hamiel, O.; Newfield, R.S.; Koren, I.; Agmon, A.; Lilos, P.; Phillip, M. Greater prevalence of iron deficiency in overweight and obese children and adolescents. Int. J. Obes. Relat. Metab. Disord. 2003, 27, 416–418. [Google Scholar] [CrossRef]
- de Dios, O.; Gavela-Pérez, T.; Aguado-Roncero, P.; Pérez-Tejerizo, G.; Ricote, M.; González, N.; Garcés, C.; Soriano-Guillén, L. C-reactive protein expression in adipose tissue of children with acute appendicitis. Pediatr. Res. 2018, 84, 564–567. [Google Scholar]
- Rumińska, M.; Witkowska-Sędek, E.; Artemniak-Wojtowicz, D.; Krajewska, M.; Majcher, A.; Sobol, M.; Pyrżak, B. Changes in leukocyte profile and C-reactive protein concentration in overweight and obese adolescents after reduction of body weight. Central Eur. J. Immunol. 2019, 44, 307–315. [Google Scholar] [CrossRef]
- Shin, S.H.; Lee, Y.J.; Lee, Y.A.; Kim, J.H.; Lee, S.Y.; Shin, C.H. High-Sensitivity C-Reactive Protein Is Associated with Prediabetes and Adiposity in Korean Youth. Metab. Syndr. Relat. Disord. 2020, 18, 47–55. [Google Scholar] [CrossRef]
- Pérez-Segura, P.; de Dios, O.; Herrero, L.; Vales-Villamarín, C.; Aragón-Gómez, I.; Gavela-Pérez, T.; Garcés, C.; Soriano-Guillén, L. Children with type 1 diabetes have elevated high-sensitivity C-reactive protein compared with a control group. BMJ Open Diabetes Res. Care 2020, 8, e001424. [Google Scholar] [CrossRef]
- Cayres, S.U.; Werneck, A.O.; Urban, J.B.; Turi-Lynch, B.C.; Barbosa, M.F.; Fernandes, R.A. Sports participation is inversely associated with C-reactive protein levels in adolescents: ABCD Growth Study. Scand J. Med. Sci. Sports 2019, 29, 1000–1005. [Google Scholar] [CrossRef]
- Fang, X.; Zuo, J.; Zhou, J.; Cai, J.; Chen, C.; Xiang, E.; Li, H.; Cheng, X.; Chen, P. Childhood obesity leads to adult type 2 diabetes and coronary artery diseases: A 2-sample mendelian randomization study. Medicine 2019, 98, e16825. [Google Scholar]
- Sadeghian, M.; Vafadar, M.; Torabi, A.; Torabi, S.; Fazel, M. Prevalence of fatty liver and its related factors in children. J. Fam. Med. Prim. Care 2022, 11, 5604–5608. [Google Scholar]
- Duan, Y.; Luo, J.; Pan, X.; Wei, J.; Xiao, X.; Li, J.; Luo, M. Association between inflammatory markers and non-alcoholic fatty liver disease in obese children. Front. Public Health 2022, 10, 991393. [Google Scholar] [CrossRef]
- Putri, R.R.; Casswall, T.; Hagman, E. Prevalence of increased transaminases and its association with sex, age, and metabolic parameters in children and adolescents with obesity-a nationwide cross-sectional cohort study. BMC Pediatr. 2021, 21, 271. [Google Scholar]
- Feldstein, A.E.; Patton-Ku, D.; Boutelle, K.N. Obesity, nutrition, and liver disease in children. Clin. Liver Dis. 2014, 18, 219–231. [Google Scholar]
- Rospleszcz, S.; Dermyshi, D.; Muller-Peltzer, K.; Strauch, K.; Bamberg, F.; Peters, A. Association of serum uric acid with visceral, subcutaneous and hepatic fat quantified by magnetic resonance imaging. Sci. Rep. 2020, 10, 442. [Google Scholar] [CrossRef]
- Li, F.; Chen, S.; Qiu, X.; Wu, J.; Tan, M.; Wang, M. Serum Uric Acid Levels and Metabolic Indices in an Obese Population: A Cross-Sectional Study. Diabetes Metab. Syndr. Obes. 2021, 14, 627–635. [Google Scholar]
- Kwiterovich, P.O., Jr. Recognition and management of dyslipidemia in children and adolescents. J. Clin. Endocrinol. Metab. 2008, 93, 4200–4209. [Google Scholar]
- Cook, S.; Kavey, R.E. Dyslipidemia and pediatric obesity. Pediatr. Clin. N. Am. 2011, 58, 1363–1373. [Google Scholar] [CrossRef]
- Brzezinski, M.; Metelska, P.; Mysliwiec, M.; Szlagatys-Sidorkiewicz, A. Lipid disorders in children living with overweight and obesity- large cohort study from Poland. Lipids Health Dis. 2020, 19, 47. [Google Scholar] [CrossRef]
- Radaelli, G.; Sausen, G.; Cesa, C.C.; Portal, V.L.; Pellanda, L.C. Secondary Dyslipidemia In Obese Children-Is There Evidence For Pharmacological Treatment? Arq. Bras Cardiol. 2018, 111, 356–361. [Google Scholar]
- Ruminska, M.; Witkowska-Sedek, E.; Majcher, A.; Pyrzak, B. Thyroid Function in Obese Children and Adolescents and Its Association with Anthropometric and Metabolic Parameters. Adv. Exp. Med. Biol. 2016, 912, 33–41. [Google Scholar]
- Ghergherehchi, R.; Hazhir, N. Thyroid hormonal status among children with obesity. Ther. Adv. Endocrinol. Metab. 2015, 6, 51–55. [Google Scholar] [CrossRef]
- Nogueira-de-Almeida, C.A.; Del Ciampo, L.A.; Ferraz, I.S.; Del Ciampo, I.R.L.; Contini, A.A.; Ued, F.D.V. COVID-19 and obesity in childhood and adolescence: A clinical review. J. Pediatr. 2020, 96, 546–558. [Google Scholar] [CrossRef]
- Thompson, D.L.; Jungk, J.; Hancock, E.; Smelser, C.; Landen, M.; Nichols, M.; Selvage, D.; Baumbach, J.; Sewell, M. Risk factors for 2009 pandemic influenza A (H1N1)-related hospitalization and death among racial/ethnic groups in New Mexico. Am. J. Public Health 2011, 101, 1776–1784. [Google Scholar]
- Hsu, P.C.; Chen, S.J. Obesity and risk of urinary tract infection in young children presenting with fever. Medicine 2018, 97, e13006. [Google Scholar]
- Miron, V.D.; Toma, A.R.; Filimon, C.; Bar, G.; Craiu, M. Optional Vaccines in Children-Knowledge, Attitudes, and Practices in Romanian Parents. Vaccines 2022, 10, 404. [Google Scholar]
- Clarke, M.; Mathew, S.M.; Giles, L.C.; Pena, A.S.; Barr, I.G.; Richmond, P.C.; Marshall, H.S. A Prospective Study Investigating the Impact of Obesity on the Immune Response to the Quadrivalent Influenza Vaccine in Children and Adolescents. Vaccines 2022, 10, 699. [Google Scholar] [CrossRef]

| Lab Analysis | Results | Unit Lab | |
|---|---|---|---|
| WBC | increased, n (%) | 2 (0.7) | |
| value, median (IQR) | 8.82 (6.08, 10.0) | ×103/μL | |
| Neutrophils | increased, n (%) | 34 (12.7) | |
| value, median (IQR) | 5.08 (3.53, 6.01) | ×103/μL | |
| Hemoglobin | decreased, n (%) | 41 (15.3) | |
| value, median (IQR) | 12.8 (12.4, 13.0) | g/mL | |
| Platelets | increased, n (%) | 24 (9.0) | |
| value, median (IQR) | 347 (323, 389) | ×103 μL | |
| Blood glucose | increased, n (%) | 9 (3.4) | |
| value, median (IQR) | 85 (79, 89) | mg/dL | |
| AST | increased, n (%) | 23 (8.6) | |
| value, median (IQR) | 28 (23, 32) | U/L | |
| ALT | increased, n (%) | 20 (7.5) | |
| value, median (IQR) | 27 (21, 34) | U/L | |
| ALP | increased, n (%) | 36 (13.4) | |
| value, median (IQR) | 303 (235, 352) | mg/dL | |
| Urea | increased, n (%) | 27 (10.0) | |
| value, median (IQR) | 23 (17, 31) | mg/dL | |
| Creatinine | increased, n (%) | 0 (0.0) | |
| value, median (IQR) | 0.5 (0.5, 0.6) | mg/dL | |
| Uric acid | increased, n (%) | 95 (35.4) | |
| value, median (IQR) | 4.7 (4.1, 5.3) | mg/dL | |
| Cholesterol | increased, n (%) | 48 (17.9) | |
| value, median (IQR) | 141 (126, 176) | mg/dL | |
| LDL | increased, n (%) | 134 (50.0) | |
| value, median (IQR) | 90 (69, 112) | mg/dL | |
| HDL | decreased, n (%) | 158 (58.9) | |
| value, median (IQR) | 47 (41, 54) | mg/dL | |
| Triglycerides | increased, n (%) | 34 (12.7) | |
| value, median (IQR) | 92 (64, 129) | mg/dL | |
| TSH | increased, n (%) | 55 (20.5) | |
| value, median (IQR) | 2.74 (2.34, 5.54) | μIU/dL | |
| T4 | decreased, n (%) | 36 (13.4) | |
| value, median (IQR) | 1.06 (0.84, 1.13) | ng/dL | |
| CRP | increased, n (%) | 44 (16.4) | |
| value, median (IQR) | 0.22 (0.06, 0.33) | mg/dL | |
| ESR | increased, n (%) | 61 (22.8) | |
| value, median (IQR) | 10 (8, 14) | mm/h | |
| Age Group | Sex | p-Value | Type of Excess Body Weight | p-Value | ||
|---|---|---|---|---|---|---|
| Female, N = 138, n (%) | Male, N = 130, n (%) | Overweight N = 84, n (%) | Obesity, N = 202, n (%) | |||
| 2–5 years | 10 (7.2) | 5 (3.8) | 0.226 | 2 (2.4) | 13 (6.4) | 0.245 |
| 5–14 years | 97 (70.3) | 105 (80.8) | 0.046 * | 62 (73.8) | 140 (69.3) | 0.446 |
| 14–18 years | 31 (22.5) | 20 (15.4) | 0.139 | 20 (23.8) | 31 (15.3) | 0.088 |
| Lab Analysis | Sex | p-Value | Age Group | p-Value | |||
|---|---|---|---|---|---|---|---|
| Female, N = 138, n (%) | Male, N = 130, n (%) | 2–5 yrs N = 15, n (%) | 5–14 yrs, N = 202, n (%) | 14–18 yrs, N = 51, n (%) | |||
| WBC increase | 1 (0.7) | 1 (0.7) | NA | 1 (6.7) | 1 (0.5) | 0 (0.0) | NA |
| Neutrophils increase | 21 (15.2) | 13 (10.0) | 0.198 | 4 (26.7) | 19 (9.4) | 11 (21.6) | 0.075 |
| Anemia | 22 (15.9) | 19 (14.6) | 0.764 | 0 (0.0) | 30 (14.9) | 11 (21.6) | 0.117 |
| Platelets increase | 13 (9.4) | 11 (8.5) | 0.777 | 3 (20.0) | 17 (8.4) | 4 (7.8) | 0.302 |
| High blood glucose | 3 (2.2) | 6 (4.6) | 0.286 | 0 (0.0) | 8 (4.0) | 1 (2.0) | 0.588 |
| AST increase | 9 (6.5) | 14 (10.8) | 0.214 | 4 (26.7) | 15 (7.4) | 4 (7.8) | 0.203 |
| ALT increase | 7 (5.1) | 13 (10.0) | 0.125 | 2 (13.3) | 10 (5.0) | 8 (15.7) | 0.689 |
| ALP increase | 16 (12.0) | 20 (15.4) | 0.362 | 0 (0.0) | 30 (14.9) | 6 (11.8) | 0.765 |
| Urea increase | 10 (7.2) | 17 (13.1) | 0.113 | 2 (13.3) | 21 (10.4) | 4 (7.8) | 0.759 |
| Uric acid increase | 42 (30.4) | 53 (40.8) | 0.077 | 1 (6.7) | 60 (29.7) | 34 (66.7) ‡ | <0.001 |
| High cholesterol | 27 (19.6) | 21 (16.2) | 0.466 | 1 (6.7) | 36 (17.8) | 11 (21.6) | 0.526 |
| High LDL | 70 (50.7) | 64 (49.2) | 0.806 | 5 (33.3) | 106 (52.5) | 23 (45.1) | 0.315 |
| Low HDL | 74 (53.6) | 84 (64.6) | 0.067 | 9 (60.0) | 115 (56.9) | 34 (66.7) | 0.549 |
| High TG | 18 (13.0) | 16 (12.3) | 0.862 | 1 (6.7) | 26 (12.9) | 7 (13.7) | 0.926 |
| TSH increase | 28 (20.3) | 27 (20.8) | 0.920 | 1 (6.7) | 41 (20.3) | 13 (25.5) | 0.378 |
| Low T4 level | 28 (20.3) ‡ | 8 (6.2) | <0.001 | 0 (0.0) | 26 (12.9) | 10 (19.6) | 0.535 |
| CRP increase | 25 (18.1) | 19 (14.6) | 0.438 | 3 (20.0) | 33 (29.2) | 8 (15.7) | 0.877 |
| ESR increase | 40 (29.0) ‡ | 21 (16.2) | 0.012 | 0 (0.0) | 48 (23.8) | 13 (25.5) | 0.541 |
| Lab Analysis | Overweight, N = 84, n (%) | Obesity, N = 184, n (%) | p-Value |
|---|---|---|---|
| WBC increase | 0 (0.0) | 0.0 (1.1) | N/A |
| Neutrophils increase | 8 (9.5) | 26 (14.1) | 0.450 |
| Anemia | 10 (11.9) | 31 (16.8) | 0.297 |
| Platelets increase | 5 (6.0) | 19 (10.3) | 0.245 |
| High blood glucose | 2 (2.4) | 7 (3.8) | 0.639 |
| AST increase | 6 (7.1) | 17 (9.2) | 0.571 |
| ALT increase | 4 (4.8) | 16 (8.7) | 0.256 |
| ALP increase | 6 (7.1) | 30 (16.3) ‡ | 0.041 |
| Urea increase | 10 (11.9) | 17 (9.2) | 0.502 |
| Uric acid increase | 13 (15.5) | 82 (44.6) ‡ | <0.001 |
| High cholesterol | 13 (15.5) | 35 (19.0) | 0.483 |
| High LDL | 33 (39.3) | 101 (54.9) ‡ | 0.017 |
| Low HDL | 39 (46.2) | 119 (64.7) ‡ | 0.004 |
| High TG | 7 (8.3) | 27 (14.7) | 0.148 |
| TSH increase | 15 (17.9) | 40 (21.7) | 0.466 |
| Low T4 level | 10 (11.9) | 26 (14.1) | 0.617 |
| CRP increase | 7 (8.3) | 37 (20.1) ‡ | 0.015 |
| ESR increase | 19 (22.6) | 42 (22.8) | 0.935 |
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2023 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Pascu, B.M.; Miron, V.D.; Matei, E.R.; Craiu, M. Laboratory Findings in Children with Excess Body Weight in Romania. Medicina 2023, 59, 319. https://doi.org/10.3390/medicina59020319
Pascu BM, Miron VD, Matei ER, Craiu M. Laboratory Findings in Children with Excess Body Weight in Romania. Medicina. 2023; 59(2):319. https://doi.org/10.3390/medicina59020319
Chicago/Turabian StylePascu, Bogdan Mihai, Victor Daniel Miron, Emanuela Rachel Matei, and Mihai Craiu. 2023. "Laboratory Findings in Children with Excess Body Weight in Romania" Medicina 59, no. 2: 319. https://doi.org/10.3390/medicina59020319
APA StylePascu, B. M., Miron, V. D., Matei, E. R., & Craiu, M. (2023). Laboratory Findings in Children with Excess Body Weight in Romania. Medicina, 59(2), 319. https://doi.org/10.3390/medicina59020319







