Predictive Factors for Nasogastric Tube Removal in Post-Stroke Patients
Abstract
:1. Introduction
2. Materials and Methods
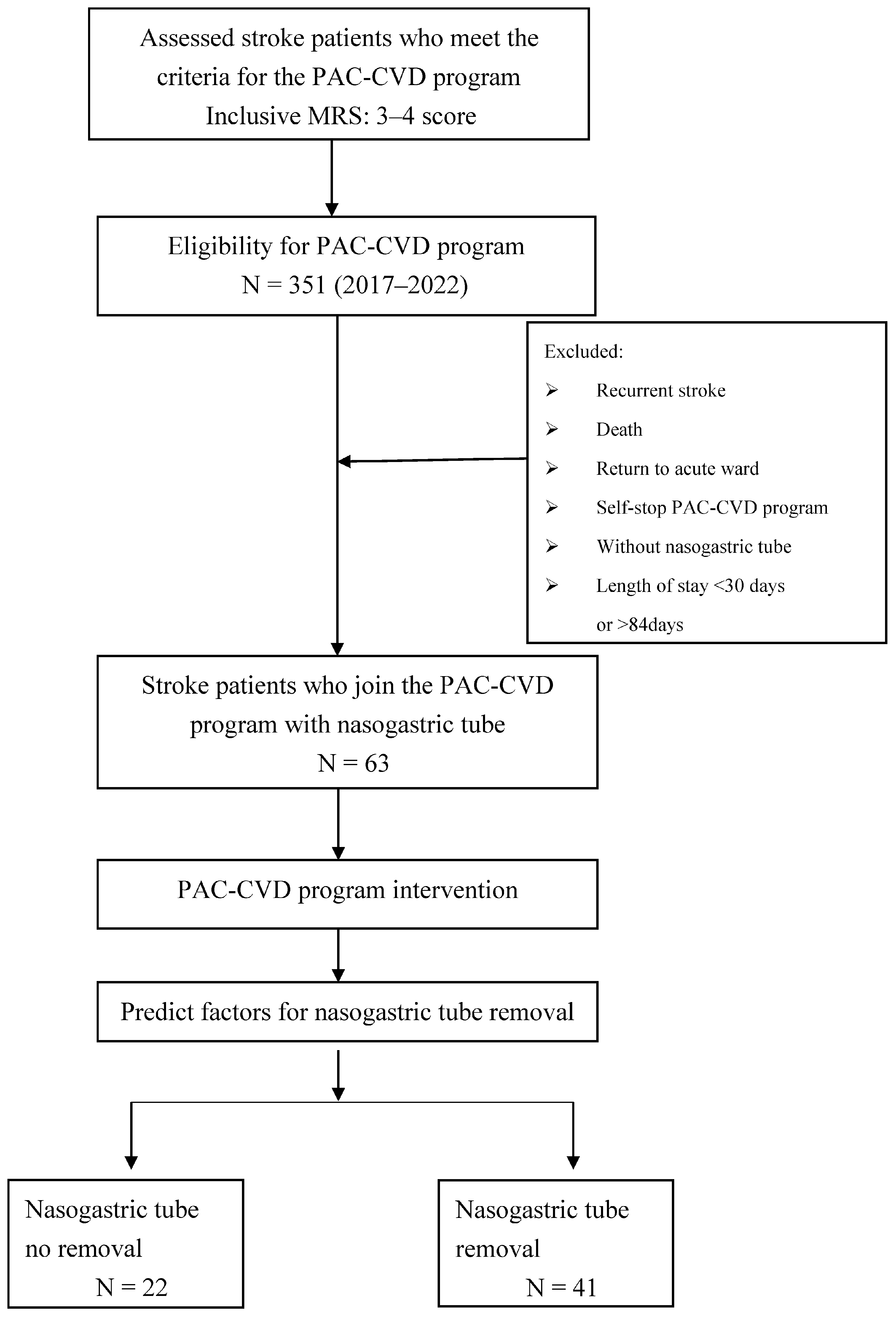
2.1. Patient Recruitment
2.2. Study Methods
2.3. Data Analysis
2.4. Ethical Considerations
3. Results
4. Discussion
Limitations
5. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Acknowledgments
Conflicts of Interest
References
- Health Promotion Administration, MOHW. Available online: https://www.hpa.gov.tw/Pages/List.aspx?nodeid=213 (accessed on 21 March 2022).
- Winstein, C.J.; Stein, J.; Arena, R.; Bates, B.; Cherney, L.R.; Cramer, S.C.; Deruyter, F.; Eng, J.J.; Fisher, B.; Harvey, R.L.; et al. Guidelines for adult stroke rehabilitation and recovery: A guideline for healthcare professionals from the American Heart Association/American Stroke Association. Stroke 2016, 47, e98–e169. [Google Scholar] [CrossRef] [PubMed]
- Han, D.S. The demonstration on improving the quality of post-acute care in Taiwan National Health Insurance. New Taipei J. Nurs. 2015, 17, 1–9. [Google Scholar]
- Hsieh, C.Y.; Tsao, W.C.; Lin, R.T.; Chao, A.C. Three years of the nationwide post-acute stroke care program in Taiwan. J. Chin. Med. Assoc. 2018, 81, 87–88. [Google Scholar] [CrossRef] [PubMed]
- Lai, M.W.; Yang, C.H.; Sung, P.Y.; Tsai, S.W. Intravascular laser irradiation of blood improves functional independence in subacute post-stroke patients: A retrospective observational study from a post-stroke acute care center in Taiwan. Photobiomodul. Photomed. Laser Surg. 2022, 40, 691–697. [Google Scholar] [CrossRef]
- Liao, W.L.; Chang, C.W.; Sung, P.Y.; Hsu, W.N.; Lai, M.W.; Tsai, S.W. The Berg Balance Scale at Admission Can Predict Community Ambulation at Discharge in Patients with Stroke. Medicina 2021, 57, 556. [Google Scholar] [CrossRef] [PubMed]
- Chien, S.H.; Sung, P.Y.; Liao, W.L.; Tsai, S.W. A functional recovery profile for patients with stroke following post-acute rehabilitation care in Taiwan. J. Formos. Med. Assoc. 2020, 119, 254–259. [Google Scholar] [CrossRef]
- Beavan, J. Update on management options for dysphagia after acute stroke. Br. J. Neurosci. Nurs. 2015, 11, 10–19. [Google Scholar] [CrossRef]
- Satou, Y.; Oguro, H.; Murakami, Y.; Onoda, K.; Mitaki, S.; Hamada, C.; Mizuhara, R.; Yamaguchi, S. Gastroesophageal reflux during enteral feeding in stroke patients: A 24-hour esophageal pH-monitoring study. J. Stroke Cerebrovasc. Dis. 2013, 22, 185–189. [Google Scholar] [CrossRef]
- Wang, Z.Y.; Chen, J.M.; Ni, G.X. Effect of an indwelling gastric tube on swallowing function in elderly post-stroke dysphagia patients with long-term nasal feeding. BMC Neurol. 2019, 19, 83. [Google Scholar] [CrossRef]
- Yamada, T.; Motomura, Y.; Hiraoka, E.; Miyagaki, A.; Sato, J. Nasogastric tubes can cause intramural hematoma of the esophagus. Am. J. Case Rep. 2019, 20, 224–227. [Google Scholar] [CrossRef]
- Ho, C.H.; Lin, W.C.; Hsu, Y.F.; Lee, I.H.; Hung, Y.C. One-Year Risk of Pneumonia and Mortality in Patients with Poststroke Dysphagia: A Nationwide Population-Based Study. J. Stroke Cerebrovasc. Dis. 2018, 27, 1311–1317. [Google Scholar] [CrossRef] [PubMed]
- Mahoney, F.I.; Barthel, D.W. Functional evaluation: The Barthel index. Md. State Med. J. 1965, 14, 61–65. [Google Scholar] [PubMed]
- Crary, M.A.; Mann, G.D.; Groher, M.E. Initial psychometric assessment of a functional oral intake scale for dysphagia in stroke patients. Arch. Phys. Med. Rehabil. 2005, 86, 1516–1520. [Google Scholar] [CrossRef] [PubMed]
- Rubenstein, L.Z.; Harker, J.O.; Salvà, A.; Guigoz, Y.; Vellas, B. Screening for undernutrition in geriatric practice: Developing the short-form mini-nutritional assessment (MNA-SF). J. Gerontol. A Biol. Sci. Med. Sci. 2001, 56, M366–M372. [Google Scholar] [CrossRef]
- EuroQol Group. EuroQol—A new facility for the measurement of health-related quality of life. Health Policy 1990, 16, 199–208. [Google Scholar] [CrossRef]
- Gladstone, D.J.; Danells, C.J.; Black, S.E. The Fugl-Meyer assessment of motor recovery after stroke: A critical review of its measurement properties. Neurorehabil. Neural Repair 2002, 16, 232–240. [Google Scholar] [CrossRef]
- Folstein, M.F.; Folstein, S.E.; McHugh, P.R. “Mini-mental state”. A practical method for grading the cognitive state of patients for the clinician. J. Psychiatr. Res. 1975, 12, 189–198. [Google Scholar] [CrossRef]
- Chung, Y.M.; Lee, S.E.; Chang, M.H.; Hsu, T.C. The concise Chinese aphasia test and its application. J. Speech Lang. Hear. Assoc. 1998, 13, 119–137. [Google Scholar]
- Elite Learning. The Original Barthel index of ADLs. Available online: https://www.elitecme.com/resource-center/rehabilitation-therapy/the-original-barthel-index-of-adls/ (accessed on 10 December 2022).
- Tombaugh, T.N.; McIntyre, N.J. The mini-mental state examination: A comprehensive review. J. Am. Geriatr. Soc. 1992, 40, 922–935. [Google Scholar] [CrossRef]
- Ickenstein, G.W.; Kelly, P.J.; Furie, K.L.; Ambrosi, D.; Rallis, N.; Goldstein, R.; Horick, N.; Stein, J. Predictors of feeding gastrostomy tube removal in stroke patients with dysphagia. J. Stroke Cerebrovasc. Dis. 2003, 12, 169–174. [Google Scholar] [CrossRef]
- Lee, J.H.; Kim, S.B.; Lee, K.W.; Lee, S.J.; Park, J.G.; Ri, J.W. Associating factors regarding nasogastric tube removal in patients with Dysphagia after stroke. Ann. Rehabil. Med. 2014, 38, 6–12. [Google Scholar] [CrossRef] [PubMed]
- Oto, T.; Kandori, Y.; Ohta, T.; Domen, K.; Koyama, T. Predicting the chance of weaning dysphagic stroke patients from enteral nutrition: A multivariate logistic modelling study. Eur. J. Phys. Rehabil. Med. 2009, 45, 355–362. [Google Scholar] [PubMed]
- Fernández-Pombo, A.; Seijo-Raposo, I.M.; López-Osorio, N.; Cantón-Blanco, A.; González-Rodríguez, M.; Arias-Rivas, S.; Rodríguez-Yáñez, M.; Santamaría-Nieto, A.; Díaz-Ortega, C.; Gómez-Vázquez, E.; et al. Lesion location and other predictive factors of dysphagia and its complications in acute stroke. Clin. Nutr. ESPEN 2019, 33, 178–182. [Google Scholar] [CrossRef] [PubMed]
- Hackett, M.L.; Pickles, K. Part I: Frequency of depression after stroke: An updated systematic review and meta-analysis of observational studies. Int. J. Stroke 2014, 9, 1017–1025. [Google Scholar] [CrossRef] [PubMed]
- Lincoln, N.B.; Brinkmann, N.; Cunningham, S.; Dejaeger, E.; De Weerdt, W.; Jenni, W.; Mahdzir, A.; Putman, K.; Schupp, W.; Schuback, B.; et al. Anxiety and depression after stroke: A 5-year follow-up. Disabil. Rehabil. 2013, 35, 140–145. [Google Scholar] [CrossRef]
- Maureen, W.; Heather, H.; Jamie, H.; Mark, S. Stroke and Nutrition Fact Sheet 2017. Available online: http://www.neuropt.org/docs/default-source/stroke-sig-docs/info-brief_stroke-sig_nutritionafter-stroke_10-17.pdf?sfvrsn=fbcc5743_2 (accessed on 30 January 2023).
- Chen, Y.; Chang, H.-P.; Tu, H.-J. Role of dietitian in post-acute care of stroke patients. Taipei City Med. J. 2019, 16, 173–179. [Google Scholar]
| All | Nasogastric Tube Removed | |||
|---|---|---|---|---|
| No | Yes | |||
| Variable | No. (%) Mean (SD) (n = 63) | No. (%) Mean (SD) (n = 22) | No. (%) Mean (SD) (n = 41) | p Value |
| Sex: | 0.697 | |||
| (1) Female | 28 (44.4) | 9 (40.9) | 19 (46.3) | |
| (2) Male | 35 (55.6) | 13 (59.1) | 22 (53.7) | |
| Age | 68.8 ± 14.9 | 73.9 ± 13.5 | 66.1 ± 15.1 | 0.040 |
| Stroke type: | 0.382 * | |||
| (1) Hemorrhage | 16 (25.4) | 4 (18.2) | 12 (29.3) | |
| (2) Ischemic | 47 (74.6) | 18 (81.8) | 29 (70.7) | |
| Length of stay | 60.6 ± 21.9 | 62.7 ± 23.5 | 59.5 ± 21.3 | 0.343 |
| Evaluation index: | ||||
| 1. BI (0–100) | 19.7 ± 15.9 | 13.6 ± 12.9 | 22.9 ± 16.6 | 0.028 |
| 2. FOIS (1–7) | 1.8 ± 1.3 | 1.3 ± 0.5 | 2.1 ± 1.5 | 0.005 |
| 3. MNA (0–30) | 10.8 ± 4.9 | 11.1 ± 4.8 | 10.7 ± 4.9 | 0.675 |
| 4. EQ-5D: | ||||
| (1) Mobility (1–3) | 2.3 ± 0.5 | 2.4 ± 0.5 | 2.2 ± 0.4 | 0.115 |
| (2) Anxiety/depression (1–3) | 1.8 ± 0.5 | 1.8 ± 0.4 | 1.8 ± 0.5 | 0.742 |
| 5. FMA: | ||||
| (1) Modified sensation (0–44) | 24 ± 16.4 | 19.9 ± 16.3 | 26.2 ± 16.2 | 0.145 |
| (2) Motor (0–66) | 25.8 ± 23.5 | 21.7 ± 21.1 | 28 ± 24.6 | 0.216 |
| 6. MMSE (0–30) | 14.0 ± 10.1 | 9.7 ± 10.4 | 16.3 ± 9.3 | 0.011 |
| 7. CCAT (1–12) | 7.3 ± 3.8 | 5.7 ± 4.3 | 8.2 ± 3.3 | 0.025 |
| All Nasogastric Tube Removal | |||||
|---|---|---|---|---|---|
| No | Yes | ||||
| Variable | Scores | No. (%) (n = 63) | No. (%) (n = 22) | No. (%) (n = 41) | p Value |
| BI groupings: | 0.050 | ||||
| (1) Total dependence | 0–20 | 42 (66.7) | 19 (86.4) | 23 (56.1) | |
| (2) Severe dependence | 21–60 | 20 (31.7) | 3 (13.6) | 17 (41.5) | |
| (3) Moderate dependence | 61–90 | 1 (1.6) | 0 | 1 (2.4) | |
| (4) Slight dependence | 91–99 | 0 | 0 | 0 | |
| (5) Total independence | 100 | 0 | 0 | 0 | |
| MMSE groupings: | 0.089 | ||||
| (1) Severe cognitive impairment | 0–17 | 34 (54.0) | 14 (63.6) | 20 (48.8) | |
| (2) Mild cognitive impairment | 18–23 | 13 (20.6) | 6 (27.3) | 7 (17.1) | |
| (3) Cognitively intact | 24–30 | 16 (25.4) | 2 (9.1) | 14 (34.1) | |
| Variables | Crude OR | p Value | Adjusted OR (95% CI) † | p Value |
|---|---|---|---|---|
| Sex (male vs. female) | 0.80 | 0.679 | ||
| Age | 0.96 | 0.053 | ||
| Stroke type (I vs. H) | 0.54 | 0.339 | ||
| Length of stay | 0.99 | 0.574 | ||
| Evaluation index | ||||
| 1. BI: | 1.05 | 0.034 | ||
| (1) Total dependence | Ref. | Ref. | ||
| (2) Severe/moderate dependence | 4.96 | 0.022 | 4.55 (1.10–18.90) | 0.037 |
| 2. FOIS | 3.38 | 0.019 | 3.07 (1.10–8.54) | 0.032 |
| 3. MNA | 0.98 | 0.729 | ||
| 4. EQ-5D: | ||||
| (1) Mobility | 0.41 | 0.117 | ||
| (2) Anxiety/depression | 1.25 | 0.669 | ||
| 5. FMA: | ||||
| (1) Modified sensation | 1.02 | 0.146 | ||
| (2) Motor | 1.01 | 0.304 | ||
| 6. MMSE: | 1.07 | 0.015 | ||
| (1) Severe cognitive impairment | Ref. | |||
| (2) Mild cognitive impairment | 0.82 | 0.758 | ||
| (3) Cognitively intact | 4.90 | 0.056 | ||
| 7. CCAT | 1.19 | |||
| Nasogastric Tube Removal | |||
|---|---|---|---|
| Variables | No Mean (SD) (n = 22) | Yes Mean (SD) (n = 41) | p Value |
| 1. BI (0–100) diff. | 20.7 ± 19.9 | 44.5 ± 17.1 | <0.001 |
| 2. FOIS (1–7) diff. | 1.1 ± 1.5 | 4.2 ± 1.7 | <0.001 |
| 3. MNA (0.0–30.0) diff. | 1.1 ± 2.3 | 2.2 ± 2.4 | 0.027 |
| 4. EQ-5D: | |||
| (1) Mobility (1–3) diff. | −0.2 ± 0.6 | −0.4 ± 0.5 | 0.127 |
| (2) Anxiety/depression (1–3) diff. | −0.2 ± 0.5 | −0.6 ± 0.6 | 0.018 |
| 5. FMA: | |||
| (1) Modified sensation (0–44) diff. | 8.9 ± 12.9 | 5.9 ± 8.8 | 0.417 |
| (2) Motor (0–66) diff. | 12.8 ± 16.7 | 14 ± 12.6 | 0.572 |
| 6. MMSE (0–30) diff. | 4.3 ± 4.6 | 4.7 ± 4.3 | 0.434 |
| 7. CCAT (1–12) diff. | 0.5 ± 2.9 | 1.4 ± 1.5 | 0.275 |
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2023 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Chuang, S.-T.; Yen, Y.-H.; Hsu, H.; Lai, M.-W.; Hung, Y.-F.; Tsai, S.-W. Predictive Factors for Nasogastric Tube Removal in Post-Stroke Patients. Medicina 2023, 59, 368. https://doi.org/10.3390/medicina59020368
Chuang S-T, Yen Y-H, Hsu H, Lai M-W, Hung Y-F, Tsai S-W. Predictive Factors for Nasogastric Tube Removal in Post-Stroke Patients. Medicina. 2023; 59(2):368. https://doi.org/10.3390/medicina59020368
Chicago/Turabian StyleChuang, Shu-Ting, Ya-Hui Yen, Honda Hsu, Ming-Wei Lai, Yu-Fang Hung, and Sen-Wei Tsai. 2023. "Predictive Factors for Nasogastric Tube Removal in Post-Stroke Patients" Medicina 59, no. 2: 368. https://doi.org/10.3390/medicina59020368
APA StyleChuang, S.-T., Yen, Y.-H., Hsu, H., Lai, M.-W., Hung, Y.-F., & Tsai, S.-W. (2023). Predictive Factors for Nasogastric Tube Removal in Post-Stroke Patients. Medicina, 59(2), 368. https://doi.org/10.3390/medicina59020368






