The Role of Patient Position in the Surgical Treatment of Supracondylar Fractures of the Humerus: Comparison of Prone and Supine Position
Abstract
:1. Introduction
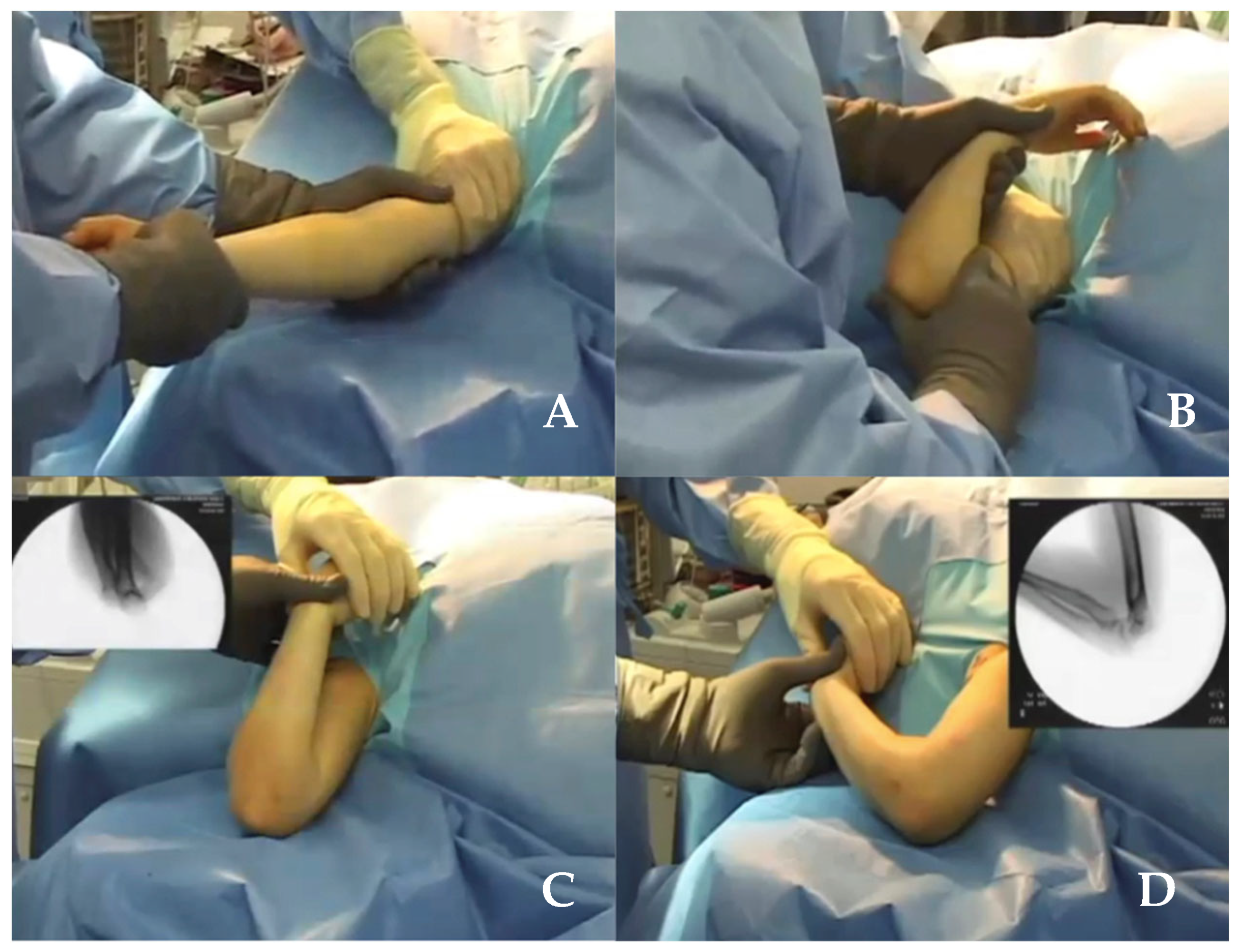
2. Materials and Methods
2.1. Search Strategy
2.2. Inclusion and Exclusion Criteria
2.3. Quality Evaluation Using the MINORS Checklist
2.4. Data Extraction
2.5. Statistical Analysis
3. Results
3.1. Search Results
3.2. Basic Characteristics of Included Studies
3.3. Surgical Treatment
3.4. Effect of Prone or Supine Position on Clinical and Radiographic Outcome
3.5. Effect of Prone or Supine Position on Surgical Outcome
3.6. Anaesthesia Time
4. Discussion
5. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Conflicts of Interest
References
- Babal, J.C.; Mehlman, C.T.; Klein, G. Nerve Injuries Associated with Pediatric Supracondylar Humeral Fractures: A Meta-Analysis. J. Pediatr. Orthop. 2010, 30, 253–263. [Google Scholar] [CrossRef] [Green Version]
- Pavone, V.; Vescio, A.; Riccioli, M.; Culmone, A.; Cosentino, P.; Caponnetto, M.; Dimartino, S.; Testa, G. Is Supine Position Superior to Prone Position in the Surgical Pinning of Supracondylar Humerus Fracture in Children? JFMK 2020, 5, 57. [Google Scholar] [CrossRef]
- Zorrilla, S.; de Neira, J.; Prada-Cañizares, A.; Marti-Ciruelos, R.; Pretell-Mazzini, J. Supracondylar Humeral Fractures in Children: Current Concepts for Management and Prognosis. Int. Orthop. (SICOT) 2015, 39, 2287–2296. [Google Scholar] [CrossRef]
- Dabis, J.; Daly, K. Supracondylar Fractures of the Humerus in Children: Review of Management and Controversies. Orthop. Muscular Syst. 2016, 05, 01. [Google Scholar] [CrossRef]
- Alton, T.B.; Werner, S.E.; Gee, A.O. Classifications in Brief: The Gartland Classification of Supracondylar Humerus Fractures. Clin. Orthop. Relat. Res. 2015, 473, 738–741. [Google Scholar] [CrossRef] [Green Version]
- Abzug, J.M.; Herman, M.J. Management of Supracondylar Humerus Fractures in Children: Current Concepts. J. Am. Acad. Orthop. Surg. 2012, 20, 69–77. [Google Scholar] [CrossRef]
- Venkatadass, K.; Balachandar, G.; Rajasekaran, S. Is Prone Position Ideal for Manipulation and Pinning of Displaced Pediatric Extension-Type Supracondylar Fractures of Humerus?: A Randomized Control Trial. J. Pediatr. Orthop. 2015, 35, 672–676. [Google Scholar] [CrossRef]
- Feldman, D. Supine Position Is Ideal for Manipulation and Pinning of All Types of Supracondylar Fractures Compared with the Prone Position. J. Bone Jt. Surg. Am. 2015, 97, 1372. [Google Scholar] [CrossRef]
- De Pellegrin, M.; Fracassetti, D.; Moharamzadeh, D.; Origo, C.; Catena, N. Advantages and Disadvantages of the Prone Position in the Surgical Treatment of Supracondylar Humerus Fractures in Children. A Literature Review. Injury 2018, 49, S37–S42. [Google Scholar] [CrossRef]
- Jayakumar, P.; Ramachandran, M. Elbow Injuries in Children. In European Surgical Orthopaedics and Traumatology; Bentley, G., Ed.; Springer: Berlin/Heidelberg, Germany, 2014; pp. 4710–4722. [Google Scholar]
- Rasool, M.N. Ulnar Nerve Injury after K-Wire Fixation of Supracondylar Humerus Fractures in Children. J. Pediatr. Orthop. 1998, 18, 686–690. [Google Scholar] [CrossRef]
- Vaquero-Picado, A.; González-Morán, G.; Moraleda, L. Management of Supracondylar Fractures of the Humerus in Children. Effort Open Rev. 2018, 3, 526–540. [Google Scholar] [CrossRef]
- Moher, D.; Liberati, A.; Tetzlaff, J.; Altman, D.G.; The PRISMA Group. Preferred Reporting Items for Systematic Reviews and Meta-Analyses: The PRISMA Statement. PLoS Med. 2009, 6, e1000097. [Google Scholar] [CrossRef] [Green Version]
- Slim, K.; Nini, E.; Forestier, D.; Kwiatkowski, F.; Panis, Y.; Chipponi, J. Methodological Index for Non-Randomized Studies (MINORS): Development and Validation of a New Instrument: Methodological Index for Non-Randomized Studies. ANZ J. Surg. 2003, 73, 712–716. [Google Scholar] [CrossRef]
- Havlas, V.; Trc, T.; Gaheer, R.; Schejbalova, A. Manipulation of Pediatric Supracondylar Fractures of Humerus in Prone Position under General Anesthesia. J. Pediatr. Orthop. 2008, 28, 660–664. [Google Scholar] [CrossRef]
- Kao, H.-K.; Yang, W.-E.; Li, W.-C.; Chang, C.-H. Treatment of Gartland Type III Pediatric Supracondylar Humerus Fractures with the Kapandji Technique in the Prone Position. J. Orthop. Trauma 2014, 28, 354–359. [Google Scholar] [CrossRef]
- Kao, H.-K.; Lee, W.-C.; Yang, W.-E.; Chang, C.-H. Treatment of Displaced Flexion-Type Pediatric Supracondylar Humeral Fractures in the Prone Position. J. Orthop. Surg. 2017, 25, 2309499016684412. [Google Scholar] [CrossRef] [Green Version]
- Reitman, R.D.; Waters, P.; Millis, M. Open reduction and internal fixation for supracondylar humerus fractures in children. J. Pediatr. Orthop. 2001, 21, 157–161. [Google Scholar]
- Bălănescu, R.; Ulici, A.; Rosca, D.; Topor, L.; Barbu, M. Neurovascular Abnormalities in Gartland III Supracondylar Fractures in Children. Chirurgia 2013, 108, 241–244. [Google Scholar]
- Pescatori, E.; Memeo, A.; Brivio, A.; Trapletti, A.; Camurri, S.; Pedretti, L.; Albisetti, W. Supracondylar Humerus Fractures in Children: A Comparison of Experiences. J. Pediatr. Orthop. B 2012, 21, 505–513. [Google Scholar] [CrossRef]
- Guler, O.; Mutlu, S.; Isyar, M.; Mutlu, H.; Cerci, H.; Mahirogullari, M. Prone versus Supine Position during Surgery for Supracondylar Humeral Fractures. J. Orthop. Surg. 2016, 24, 167–169. [Google Scholar] [CrossRef]
- Turgut, A. A New Method to Correct Rotational Malalignment for Closed Reduction and Percutaneous Pinning in Pediatric Supracondylar Humeral Fractures. Acta. Orthop. Traumatol. Turc. 2014, 48, 611–614. [Google Scholar] [CrossRef]
- Fowler, T.P.; Marsh, J.L. Reduction and Pinning of Pediatric Supracondylar Humerus Fractures in the Prone Position. J. Orthop. Trauma 2006, 20, 277–281. [Google Scholar] [CrossRef]
- Herzog, M.A.; Oliver, S.M.; Ringler, J.R.; Jones, C.B.; Sietsema, D.L. Mid-America Orthopaedic Association Physician in Training Award: Surgical Technique: Pediatric Supracondylar Humerus Fractures: A Technique to Aid Closed Reduction. Clin. Orthop. Relat. Res. 2013, 471, 1419–1426. [Google Scholar] [CrossRef] [Green Version]
- Bhuyan, B.K. Close Reduction and Percutaneous Pinning in Displaced Supracondylar Humerus Fractures in Children. J. Clin. Orthop. Trauma 2012, 3, 89–93. [Google Scholar] [CrossRef] [Green Version]
- Flynn, J.C.; Matthews, J.G.; Benoit, R.L. Blind Pinning of Displaced Supracondylar Fractures of the Humerus in Children. Sixteen Years’ Experience with Long-Term Follow-Up. J. Bone Jt. Surg. Am. 1974, 56, 263–272. [Google Scholar]
- Williamson, D.M.; Coates, C.J.; Miller, R.K.; Cole, W.G. Normal Characteristics of the Baumann (Humerocapitellar) Angle: An Aid in Assessment of Supracondylar Fractures. J. Pediatr. Orthop. 1992, 12, 636–639. [Google Scholar]
- De Pellegrin, M.; Brivio, A.; Pescatori, E.; Tessari, L. Frattura sovracondiloidea di omero in età infantile. Osteosintesi percutanea in posizione prona. G. Ital. Di Ortop. E Traumatol. 2008, 34, 199–204. [Google Scholar]
- Pretell Mazzini, J.; Rodriguez Martin, J.; Andres Esteban, E.M. Surgical Approaches for Open Reduction and Pinning in Severely Displaced Supracondylar Humerus Fractures in Children: A Systematic Review. J. Child. Orthop. 2010, 4, 143–152. [Google Scholar] [CrossRef]


| Methodological Items for Non-Randomized Studies | Score † |
|---|---|
|
| Author | Type of Study | Number of Patients (Sex Ratio): | Age (Years) | Follow-Up (Months) | Position | Type of Fracture According to Gartland Classification | Clinical Evaluation and Results | Radiographic Evaluation and Results | Open Reduction Required | Complications | Limits |
|---|---|---|---|---|---|---|---|---|---|---|---|
| Vojtech Havlas et al. [15] (2008) | Rtc | 455 (261 M/194 F) | 7.5 | 3 ± 6 | Prone | II–III | Loss of reduction: 3.5% (n = 16). Not analyzed the second procedure | Loss of reduction: 3.5% (n = 16) Pin tract infections 1.3% (n = 6). | Retrospective study. Short follow-up. | ||
| Hsuan-Kai Kao et al. [16] (2014) | Rtc | 34 (22 M/12 F) | 5.2 | 17.4 | Prone | III | Flynn’s criteria: excellent 31, good 2, poor 1 | Baumann’s angle 5.1 6 3.9°. Humerocapitellar angle 9 6 10° (range 0–55°) | 0 out of 34 | Loss of reduction: 5.8% (n = 2) | Retrospective case series study no comparative radiographs of the noninjured elbow no control group treated with other procedures |
| K. Venkatadass et al. [7] (2015) | Ct | 26 (20 M/6 F) | 6.8 | 12 | Prone | III | Flynn’s Criteria (Cosmetical Factors: Excellent 14/Good 4/Fair 2/Poor 1) Functional Factor (Excellent 9/Good 8/Fair 3/Poor3) | Baumann’s angle 18.46° (7 outliers in prone group) | 0 out of 26. Closed reduction not achieved in 2/26 in prone position. | Compartment syndrome with median nerve palsy 3.84% (n = 1) Cubitus varus 7% (n = 2) Poor ROM 10% (n = 3) | Small sample size |
| Hsuan-Kai Kao et al. [17] (2017) | Rtc | 10 (7 M/3 F) | 9.5 | 17.8 | Prone | III | Flynn’s criteria excellent in 9 patients/poor in 1 patient | Baumann’s angle 3.5 + 1.9 (range: 0–7) Humerocapitellar angle 7.9 + 7.4 (range: 1–24) | 2/10 caused by ulnar preoperatory deficiency | Small sample size Retrospective case series no comparative radiographs of the noninjured elbow no control group | |
| R. Bãlãnescu et al. [19] (2013) | prospective | 40 | 3 | Supine | III | Clinical evaluation after 1 year: elbow flexion +130/140 degrees; elbow extension 0/+ 5 degrees | Radiographic evaluation after 1 year postoperatively: excellent or very good results in 38 patients (95%) | 0/40 | 24 h after surgery: The capillary pulse was found difficult to record using a pulse oximeter in 5 (12.5%) patients (meaning that it displayed values varying >20%) Capillary refill time reduced by >50% in 1 patient (0.02%) Paraesthesia in 4 patients (10%) Finger function affected in 1 patient. 3 months postoperatively: elbow flexion <90 degrees in 3 patients (7%) | Retrospective study Small sample size, no multicentric study. No long-term follow-up. | |
| Ezio Pescatori et al. [20] (2012) | Rtc | 34 (19 M/15 F) | 6.1 | 46 | Supine | III | Flynn’s criteria (Functional: 32 excellent, 2 good, 0 acceptable) (Cosmetic: Humerus–ulnar–carpal angle 30 excellent, 1 good,1 acceptable) | 1 out of 34 | Cubitus varus 5.88% (n = 2) | Retrospective study Small sample size. | |
| Olcay Guler et al. [21] (2016) | Rtc | 27 (15 M/12 F) | 6.9 ± 1.5 | 22.8 ± 9.9 | Prone | III | Flynn’s criteria (very good: good 23:4) | Baumann’s angle 73.1° ± 3.5°. Lateral radiocapitaller angle 41.7° ± 4.2°. | - | Retrospective study Small sample size. | |
| Ali Turgut et al. [22] (2014) | Rtc | 19 | (Mean age: 7 y and 6 m, range: 3 y and 2 m to 12 y and 10 m) | 13.3 | Supine | III | Elbow flexion-extension range of motion 146° (range: 130° to 160°). Carrying angle decreased in 7 elbows, increased in 6 and remained the same in 6. | 0 out of 19 | Retrospective study Small sample size. | ||
| M. De Pellegrin et al. [9] (2008) | Rtc | 45 (32 M/13 F) | 6.5 | Prone | III | Flynn’s criteria (Excellent 44/good 1) Cubital angle (44 excellent/1 deviation varus of 6° and hyperextension of 10° (good result) | - | Retrospective study Small sample size. | |||
| T. P. Fowler et al. [23] (2006) | Rtc | 19 | until fracture healing | Prone | (14 Gartland type III/5 Gartland type II) | 2 out of 19 | Ulnar nerve hypermobility with a propensity to displace anteriorly with elbow flexion >50% of children aged 6 to 10 years | Retrospective study Small sample size. | |||
| Vito Pavone et al. [2] (2020) | Rtc | 25 | 5.9 ± 2.3 | 59.9 ± 12.8 | Prone | III | Flynn’s criteria excellent cosmetic outcome in 23 subjects (92.0%) and good in 2 (8.0%). Functional factor was satisfactory in 100% of patients. MEPS 97.8 ± 3.3 (range 91–100) Final follow-up, the range of motion gave a flexion range of about 113.6° ± 11.2° (range 94°–137°), extension of 2.9° ± 2.2° (range 0°–10°), and supination to pronation of about 86.2° ± 2.2° (range 84°–90°). | Baumann’s angle 5.1° ± 1.1° (range 2.8°–6.6°) | - | Mild hyperextension 4% (n = 1) Local infection 8% (n = 2) | Retrospective study Small sample size. Lack of objective measurements. |
| Herzog M. et al. [24] (2013) | Rtc | 106 (30 M/23 F) | 6.1 | 1 | Supine | II–III | ROM | Baumann’s angle. Humeral capitellar angle. | 8 out of 106 | Vascular injury 1.88% (n = 1) Nerve injury 15% (n = 8) | Retrospective study Small sample size. Lack of objective measurements. |
| Basant Kumar Bhuyan M.S [25] (2012) | Prospective | 277 | 6 | 54 | Supine | II–III | Flynn’s criteria (excellent 202/good 68/fair 5, poor 2). Carrying angle 10.65°. | Baumann’s angle. Humeral capitellar angle. | 6 out of 257 | Pin tract infection 11.55% (n = 32) Ulnar nerve injury 9.38% (n = 26) | Small sample size no multicentric study. |
| PRONE | SUPINE |
|---|---|
| Local infection 0.8%(n = 2) | Local infection 6% (n = 32) |
| Cubitus varus 0.3% (n = 2) | Cubitus varus 1.1% (n = 2) |
| Poor ROM 1% (n = 8) Paraesthesia 0.8% (n = 6) | Poor ROM 1.1% (n = 6) Vascular injury 1.88% (n = 1) Nerve injury 7.6% (n = 39) |
| Compartment syndrome with median nerve palsy 0.15% (n = 1) |
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2023 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Sapienza, M.; Testa, G.; Vescio, A.; Panvini, F.M.C.; Caldaci, A.; Parisi, S.C.; Pavone, V.; Canavese, F. The Role of Patient Position in the Surgical Treatment of Supracondylar Fractures of the Humerus: Comparison of Prone and Supine Position. Medicina 2023, 59, 374. https://doi.org/10.3390/medicina59020374
Sapienza M, Testa G, Vescio A, Panvini FMC, Caldaci A, Parisi SC, Pavone V, Canavese F. The Role of Patient Position in the Surgical Treatment of Supracondylar Fractures of the Humerus: Comparison of Prone and Supine Position. Medicina. 2023; 59(2):374. https://doi.org/10.3390/medicina59020374
Chicago/Turabian StyleSapienza, Marco, Gianluca Testa, Andrea Vescio, Flora Maria Chiara Panvini, Alessia Caldaci, Stefania Claudia Parisi, Vito Pavone, and Federico Canavese. 2023. "The Role of Patient Position in the Surgical Treatment of Supracondylar Fractures of the Humerus: Comparison of Prone and Supine Position" Medicina 59, no. 2: 374. https://doi.org/10.3390/medicina59020374
APA StyleSapienza, M., Testa, G., Vescio, A., Panvini, F. M. C., Caldaci, A., Parisi, S. C., Pavone, V., & Canavese, F. (2023). The Role of Patient Position in the Surgical Treatment of Supracondylar Fractures of the Humerus: Comparison of Prone and Supine Position. Medicina, 59(2), 374. https://doi.org/10.3390/medicina59020374









