A Real-World Cost-Effectiveness Study Evaluating Imaging Strategies for the Diagnostic Workup of Renal Colic in the Emergency Department
Abstract
:1. Introduction
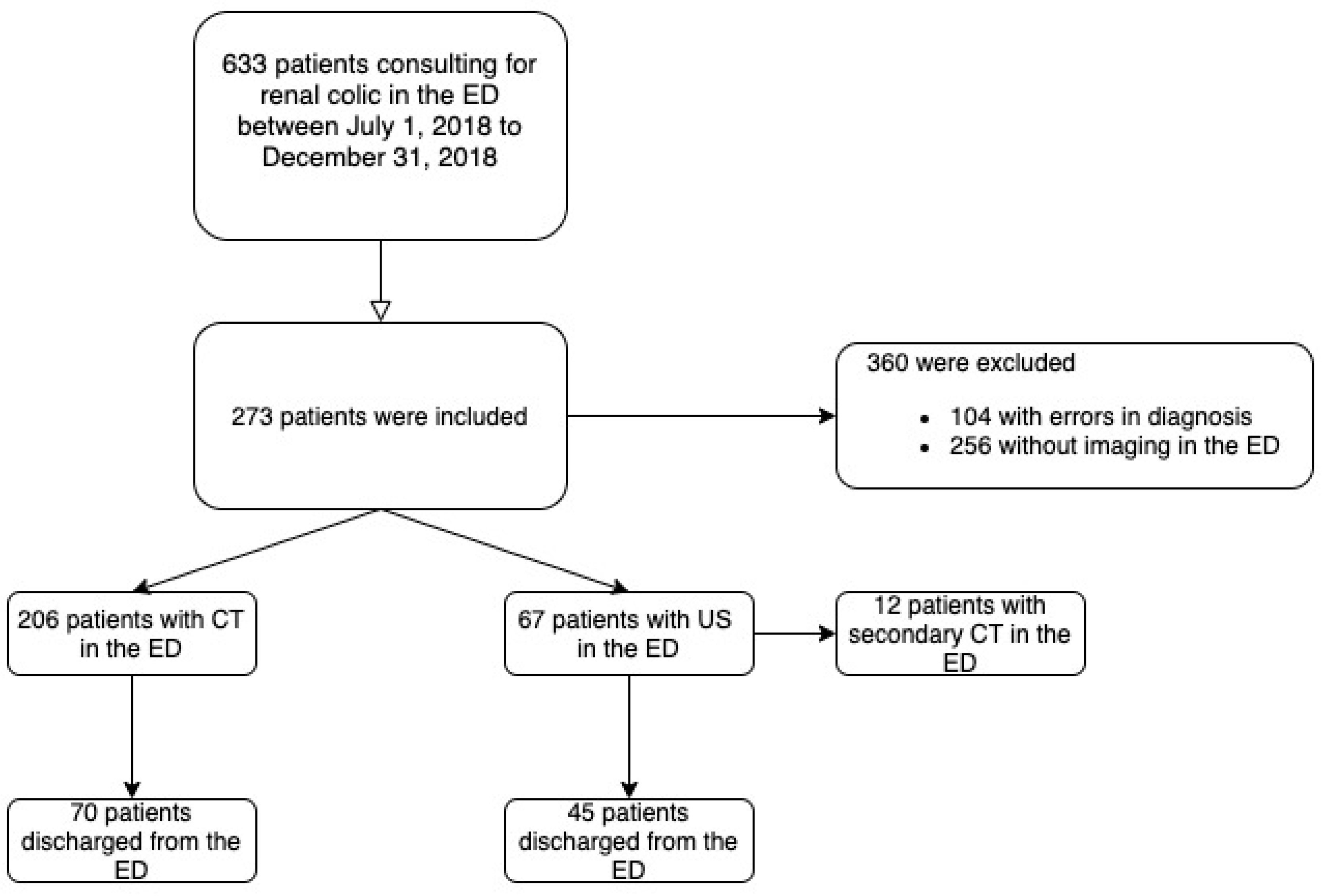
2. Materials and Methods
2.1. Study Population, Setting and Location
2.2. Comparators
2.3. Perspective
2.4. Time Horizon
2.5. Discount Rate
2.6. Measure of Effectiveness
2.7. Measurement and Valuation of Resources and Costs
- -
- Number and unit costs of US and CT performed in the ED;
- -
- Costs of initial hospitalization and readmissions related to initial renal colic during the 60-day follow up period.
2.8. Currency, Price Date, and Conversion
2.9. Selection, Measurement and Valuation of Effectiveness
Primary Endpoint
- Time to imaging, measured as the time from admission to the time of first imaging, as recorded in the ED electronic health record;
- Proportion of patients who underwent a second imaging in the ED;
- Care pathway after ED workup as a proportion of admissions (by medical service type, including intensive care unit [ICU] and short-stay unit);
- Proportion of rehospitalizations during follow-up from local hospital claims databases;
- Proportion of patients with imaging during 60-day follow-up recorded in medical file.
2.10. Rationale and Description of Model
2.11. Analytics and Assumptions
2.12. Characterizing Uncertainty
2.13. Characterizing Heterogeneity
2.14. Ethics Approval, Data and Safety Monitoring
3. Results
3.1. Study Parameters
3.1.1. Effectiveness
3.1.2. Secondary Endpoints
3.2. Incremental Costs and Outcomes
3.2.1. Costs
3.2.2. Group Comparisons
3.3. Characterizing Uncertainty
3.4. Characterizing Heterogeneity
4. Discussion
Limitations and Strengths
5. Conclusions
Supplementary Materials
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Acknowledgments
Conflicts of Interest
Abbreviations
| CT | computed tomography |
| ED | emergency departments |
| US | ultrasound |
| LOS | length of stay |
| ICER | incremental cost effectiveness ratio |
References
- Chewcharat, A.; Curhan, G. Trends in the prevalence of kidney stones in the United States from 2007 to 2016. Urolithiasis 2021, 49, 27–39. [Google Scholar] [CrossRef] [PubMed]
- Scales, C.D., Jr.; Smith, A.C.; Hanley, J.M.; Saigal, C.S. Urologic Diseases in America Project. Prevalence of kidney stones in the United States. Eur. Urol. 2012, 62, 160–165. [Google Scholar] [CrossRef] [Green Version]
- Schoenfeld, E.M.; Pekow, P.S.; Shieh, M.S.; Scales, C.D., Jr.; Lagu, T.; Lindenauer, P.K. The diagnosis and management of patients with renal colic across a sample of US hospitals: High CT utilization despite low rates of admission and inpatient urologic intervention. PLoS ONE 2017, 12, e0169160. [Google Scholar] [CrossRef]
- Ghani, K.R.; Roghmann, F.; Sammon, J.D.; Trudeau, V.; Sukumar, S.; Rahbar, H.; Kumar, R.; Karakiewicz, P.I.; Peabody, J.O.; Menon, M.; et al. Emergency department visits in the United States for upper urinary tract stones: Trends in hospitalization and charges. J. Urol. 2014, 191, 90–96. [Google Scholar] [CrossRef]
- Saigal, C.S.; Joyce, G.; Timilsina, A.R. Urologic Diseases in America Project. Direct and indirect costs of nephrolithiasis in an employed population: Opportunity for disease management? Kidney Int. 2005, 68, 1808–1814. [Google Scholar] [CrossRef] [Green Version]
- Agency for Healthcare Research and Quality. Acute Onset Flank Pain—Suspicion of Stone Disease, ACR Appropriateness Criteria. Available online: http://www.guideline.gov/content.aspx?id=15759 (accessed on 30 December 2022).
- Westphalen, A.C.; Hsia, R.Y.; Maselli, J.H.; Wang, R.; Gonzales, R. Radiological imaging of patients with suspected urinary tract stones: National trends, diagnoses, and predictors. Acad. Emerg. Med. 2011, 18, 699–707. [Google Scholar] [CrossRef] [PubMed]
- Rodger, F.; Roditi, G.; Aboumarzouk, O.M. Diagnostic Accuracy of Low and Ultra-Low Dose CT for Identification of Urinary Tract Stones: A Systematic Review. Urol. Int. 2018, 100, 375–385. [Google Scholar] [CrossRef] [PubMed]
- Xiang, H.; Chan, M.; Brown, V.; Huo, Y.R.; Chan, L.; Ridley, L. Systematic review and meta-analysis of the diagnostic accuracy of low-dose computed tomography of the kidneys, ureters and bladder for urolithiasis. J. Med. Imaging Radiat. Oncol. 2017, 6, 582–590. [Google Scholar] [CrossRef]
- Doty, E.; DiGiacomo, S.; Gunn, B.; Westafer, L.; Schoenfeld, E. What are the clinical effects of the different emergency department imaging options for suspected renal colic? A scoping review. J. Am. Coll. Emerg. Physicians Open 2021, 16, e12446. [Google Scholar] [CrossRef]
- Mills, L.; Morley, E.J.; Soucy, Z.; Vilke, G.M.; Lam, S.H.F. Ultrasound for the Diagnosis and Management of Suspected Urolithiasis in the Emergency Department. J. Emerg. Med. 2018, 54, 215–220. [Google Scholar] [CrossRef] [PubMed]
- Moore, C.L.; Carpenter, C.R.; Heilbrun, M.E. Imaging in Suspected Renal Colic: Systematic Review of the Literature and Multispecialty Consensus. Ann. Emerg. Med. 2019, 74, 391–399. [Google Scholar] [CrossRef] [Green Version]
- Référentiel de Coûts MCO 2018. Available online: http://www.scansante.fr/r%C3%A9f%C3%A9rentiel-de-co%C3%BBts-mco-2018 (accessed on 30 December 2022).
- ATIH. Tarifs MCO et HAD. 2021. Available online: http://www.atih.sante.fr/tarifs-mco-et-had (accessed on 30 December 2022).
- ATIH. Tarification de Référence. 2021. Available online: http://www.atih.sante.fr/tarification-de-reference (accessed on 30 December 2022).
- Van Buuren, S.; Groothuis-Oudshoorn, K. Mice: Multivariate Imputation by Chained Equations in R. J. Stat. Soft. 2011, 45, 1–67. [Google Scholar] [CrossRef] [Green Version]
- Toulouse, E.; Masseguin, C.; Lafont, B.; McGurk, G.; Harbonn, A.; ARoberts, J.; Granier, S.; Dupeyron, A.; Bazin, J.E. French legal approach to clinical research. Anaesth. Crit. Care Pain Med. 2018, 37, 607–614. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Coursey, C.A.; Casalino, D.D.; Remer, E.M.; Arellano, R.S.; Bishoff, J.T.; Dighe, M.; Fulgham, P.; Goldfarb, S.; Israel, G.M.; Lazarus, E.; et al. ACR appropriateness criteria acute onset flank pain—Suspicion of stone disease. Ultrasound Q. 2012, 28, 227–233. [Google Scholar] [CrossRef]
- Fulgham, P.F.; Assimos, D.G.; Pearle, M.S.; Preminger, G.M. Clinical effectiveness protocols for imaging in the management of ureteral calculous disease: AUA technology assessment. J. Urol. 2013, 189, 1203–1213. [Google Scholar] [CrossRef] [PubMed]
- Sierzenski, P.R.; Linton, O.W.; Amis, E.S., Jr.; Courtney, D.M.; Larson, P.A.; Mahesh, M.; Novelline, R.A.; Frush, D.P.; Mettler, F.A.; Timins, J.K.; et al. Applications of justification and optimization in medical imaging: Examples of clinical guidance for computed tomography use in emergency medicine. Ann. Emerg. Med. 2014, 63, 25–32. [Google Scholar] [CrossRef]
- Himelfarb, J.; Lakhani, A.; Shelton, D. Appropriate use of CT for patients presenting with suspected renal colic: A quality improvement study. BMJ Open Qual. 2019, 8, e000470. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Boudi, Z.; Lauque, D.; Alsabri, M.; Östlundh, L.; Oneyji, C.; Khalemsky, A.; Lojo Rial, C.; WLiu, S.; ACamargo, C., Jr.; Aburawi, E.; et al. Association between boarding in the emergency department and in-hospital mortality: A systematic review. PLoS ONE 2020, 15, e0231253. [Google Scholar] [CrossRef] [Green Version]
- Sprivulis, P.C.; Da Silva, J.A.; Jacobs, I.G.; Frazer, A.R.; Jelinek, G.A. The association between hospital overcrowding and mortality among patients admitted via Western Australian emergency departments. Med. J. Aust. 2006, 184, 208–212. [Google Scholar] [CrossRef] [PubMed]
- Singer, A.J.; Thode HCJr Viccellio, P.; Pines, J.M. The association between length of emergency department boarding and mortality. Acad. Emerg. Med. 2011, 18, 1324–1329. [Google Scholar] [CrossRef] [PubMed]
- Jo, S.; Kim, K.; Lee, J.H.; Kim, Y.J.; Suh, G.J.; Jin, Y.H. Emergency department crowding is associated with 28-day mortality in community-acquired pneumonia patients. J. Infect. 2012, 64, 268–275. [Google Scholar] [CrossRef] [PubMed]
- Goldhill, D.R.; McNarry, A.F.; Hadjianastassiou, V.G.; Tekkis, P.P. The longer patients are in hospital before Intensive Care admission the higher their mortality. Intensive Care Med. 2004, 30, 1908–1913. [Google Scholar] [CrossRef] [PubMed]
- Carr, B.G.; Kaye, A.J.; Wiebe, D.J.; Gracias, V.H.; Schwab, C.W.; Reilly, P.M. Emergency department length of stay: A major risk factor for pneumonia in intubated blunt trauma patients. J. Trauma 2007, 63, 9–12. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Smith-Bindman, R.; Aubin, C.; Bailitz, J.; Bengiamin, R.N.; Camargo, C.A., Jr.; Corbo, J.; Dean, A.J.; Goldstein, R.B.; Griffey, R.T.; Jay, G.D.; et al. Ultrasonography versus computed tomography for suspected nephrolithiasis. N. Engl. J. Med. 2014, 371, 1100–1110. [Google Scholar] [CrossRef] [Green Version]
- Blecher, G.; Meek, R.; Egerton-Warburton, D.; McCahy, P. Introduction of a new imaging guideline for suspected renal colic in the ED reduces CT urography utilisation. Emerg. Med. J. 2017, 34, 749–754. [Google Scholar] [CrossRef] [PubMed]
- Kim, S.G.; Jo, I.J.; Kim, T.; Park, J.H.; Shin, T.G.; Sim, M.S.; Cha, W.C.; Yoon, H. Usefulness of protocolized point-of-care ultrasonography for patients with acute renal colic who visited emergency department: A randomized controlled study. Med. Kaunas 2019, 55, 717. [Google Scholar] [CrossRef] [Green Version]
- Caldwell, N.; Srebotnjak, T.; Wang, T.; Hsia, R. “How much will I get charged for this?” Patient charges for top ten diagnoses in the emergency department. PLoS ONE 2013, 8, e55491. [Google Scholar] [CrossRef] [PubMed]
- Eaton, S.H.; Cashy, J.; Pearl, J.A.; Stein, D.M.; Perry, K.; Nadler, R.B. Admission rates and costs associated with emergency presentation of urolithiasis: Analysis of the Nationwide Emergency Department Sample 2006–2009. J. Endourol. 2013, 27, 1535–1538. [Google Scholar] [CrossRef] [Green Version]
- Elder, J.W.; Delgado, M.K.; Chung, B.I.; Pirrotta, E.A.; Wang, N.E. Variation in the intensity of care for patients with uncomplicated renal colic presenting to U.S. emergency departments. J. Emerg. Med. 2016, 51, 628–635. [Google Scholar] [CrossRef]
- Melnikow, J.; Xing, G.; Cox, G.; Leigh, P.; Mills, L.; Miglioretti, D.L.; Moghadassi, M.; Smith-Bindman, R. Cost analysis of the STONE randomized trial: Can health care costs be reduced one test at a time? Med. Care 2016, 54, 337–342. [Google Scholar] [CrossRef]
- Lindqvist, K.; Hellström, M.; Holmberg, G.; Peeker, R.; Grenabo, L. Immediate versus deferred radiological investigation after acute renal colic: A prospective randomized study. Scand. J. Urol. Nephrol. 2006, 40, 119–124. [Google Scholar] [CrossRef]
- Rob, S.; Bryant, T.; Wilson, I.; Somani, B.K. Ultra-low-dose, low-dose, and standard-dose CT of the kidney, ureters, and bladder: Is there a difference? Results from a systematic review of the literature. Clin. Radiol. 2017, 72, 11–15. [Google Scholar] [CrossRef] [PubMed]
- Schoenfeld, E.M.; Houghton, C.; Patel, P.M.; Merwin, L.W.; Poronsky, K.P.; Caroll, A.L.; Sánchez Santana, C.; Breslin, M.; Scales, C.D.; Lindenauer, P.K.; et al. Shared Decision Making in Patients with Suspected Uncomplicated Ureterolithiasis: A Decision Aid Development Study. Acad. Emerg. Med. 2020, 27, 554–565. [Google Scholar] [CrossRef] [PubMed]


| Characteristics | US N = 67 | CT N = 206 | p | |
|---|---|---|---|---|
| Age (M, SD) | 47.4 (±17.1) | 46.5 (±15.4) | 0.69 | |
| Gender | ||||
| Men (N, %) | 48 (72) | 145 (70) | 0.84 | |
| Women (N, %) | 19 (28) | 145 (70) | ||
| Medical history | ||||
| Nephrolithiasis (N, %) | 28 (42) | 66 (32) | 0.14 | |
| Renal malformation (N, %) | 2 (3) | 7 (3.4) | 0.25 | |
| Clinical presentation | ||||
| Heart rate (M, SD) | 78.6 (±13.5) | 77 (±15.1) | 0.42 | |
| Systolic blood pressure (mmHg) (M, SD) | 140 (±19) | 140 (±19.8) | 1 | |
| Pain numerical scale * (Median, Q25-75) | 8 [6; 10] | 8 [6.7; 10] | 0.76 | |
| Body temperature (M, SD) | 36.9 (±0.7) | 36.7 (±0.6) | 0.06 | |
| Laboratory tests | ||||
| Leukocytes (M, SD) | 10.4 (±4) | 10.6 (±3.4) | 0.72 | |
| Cockcroft estimated glomerular filtration rate (µmol/L) (M, SD) | 94.5 (±23.8) | 88.4 (±23.6) | 0.02 | |
| CRP (M, SD) | 8.1 (±16.2) | 13.9 (±39.9) | 0.04 | |
| Hydronephrosis ** (M,SD) | 11.7 (±9.1) | 16.2 (±6.7) | <0.01 | |
| Time to imaging in the ED * (Median, Q25-75) | 4.5 [3.4; 5.9] | 4.8 [3.7; 6.8] | 0.23 | |
| Another imaging in the ED | 12 (18) | 0 (0) | <0.01 | |
| Length of stay in the ED * (M, SD) | 8.8 (±4.5) | 8.6 (±3.7) | 0.32 | |
| Care pathway after ED | ||||
| Discharge from the ED (N, %) | 45 (67) | 70 (34) | <0.01 | |
| Hospitalization in the short time stay unit (N, %) | 19 (28) | 92 (45) | 0.02 | |
| Hospitalization in urology unit (N, %) | 3 (5) | 44 (21) | <0.01 | |
| Length of hospitalization ‡ (Median, Q25-75) | 1 [1;1] | 1 [1;1] | 1 | |
| Another unplanned imaging during follow-up at 60 days | 14 (20.8) | 14 (6.8) | <0.01 | |
| Death at 60 days (N, %) | 0 (0) | 0 (0) | 1 | |
| Costs Expressed as Mean (SD) | US N = 67 | CT N = 206 |
|---|---|---|
| Imaging | €43.7 (±49.6) | €29.6 (±38.2) |
| Consultation in the ED | €33.4 (±39.8) | €30.3 (±38.9) |
| Hospitalization | €649 (±781) | €660 (±826) |
| Reconsultation in the ED | €4.5 (±25.7) | €1.5 (±14.7) |
| Rehospitalization | €428 (±1809) | €235 (±1153) |
| Total cost | €1159 (±1987) | €956 (±1462) |
| Strategy [95% CI] | LOS in the ED | Cost Per Patient | Difference of LOS in the ED | Difference of Cost |
|---|---|---|---|---|
| US | 8.9 [8.1; 9.4] | €1159 [745; 1247] | NA | NA |
| CT | 8.7 [7.9; 9.9] | €961 [779; 1680] | 0.139 [−1.1; 1.5] | € − 199 [−745; 285] |
| Determinant of Analysis | Difference of Cost | Difference of_Efficacy |
|---|---|---|
| Base case | € − 199 | 0.2 |
| Imaging | € − 253 | 0.2 |
| Outpatient visit | € − 219 | 0.2 |
| Hospitalization | € − 918 | 0.2 |
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2023 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Kepka, S.; Zarca, K.; Ohana, M.; Hoffmann, A.; Muller, J.; Le Borgne, P.; Andrès, E.; Bilbault, P.; Durand Zaleski, I. A Real-World Cost-Effectiveness Study Evaluating Imaging Strategies for the Diagnostic Workup of Renal Colic in the Emergency Department. Medicina 2023, 59, 475. https://doi.org/10.3390/medicina59030475
Kepka S, Zarca K, Ohana M, Hoffmann A, Muller J, Le Borgne P, Andrès E, Bilbault P, Durand Zaleski I. A Real-World Cost-Effectiveness Study Evaluating Imaging Strategies for the Diagnostic Workup of Renal Colic in the Emergency Department. Medicina. 2023; 59(3):475. https://doi.org/10.3390/medicina59030475
Chicago/Turabian StyleKepka, Sabrina, Kevin Zarca, Mickaël Ohana, Anne Hoffmann, Joris Muller, Pierrick Le Borgne, Emmanuel Andrès, Pascal Bilbault, and Isabelle Durand Zaleski. 2023. "A Real-World Cost-Effectiveness Study Evaluating Imaging Strategies for the Diagnostic Workup of Renal Colic in the Emergency Department" Medicina 59, no. 3: 475. https://doi.org/10.3390/medicina59030475






