Regeneration of Horizontal Bone Defect in Edentulous Maxilla Using the Allogenic Bone-Plate Shell Technique and a Composite Bone Graft—A Case Report
Abstract
:1. Introduction
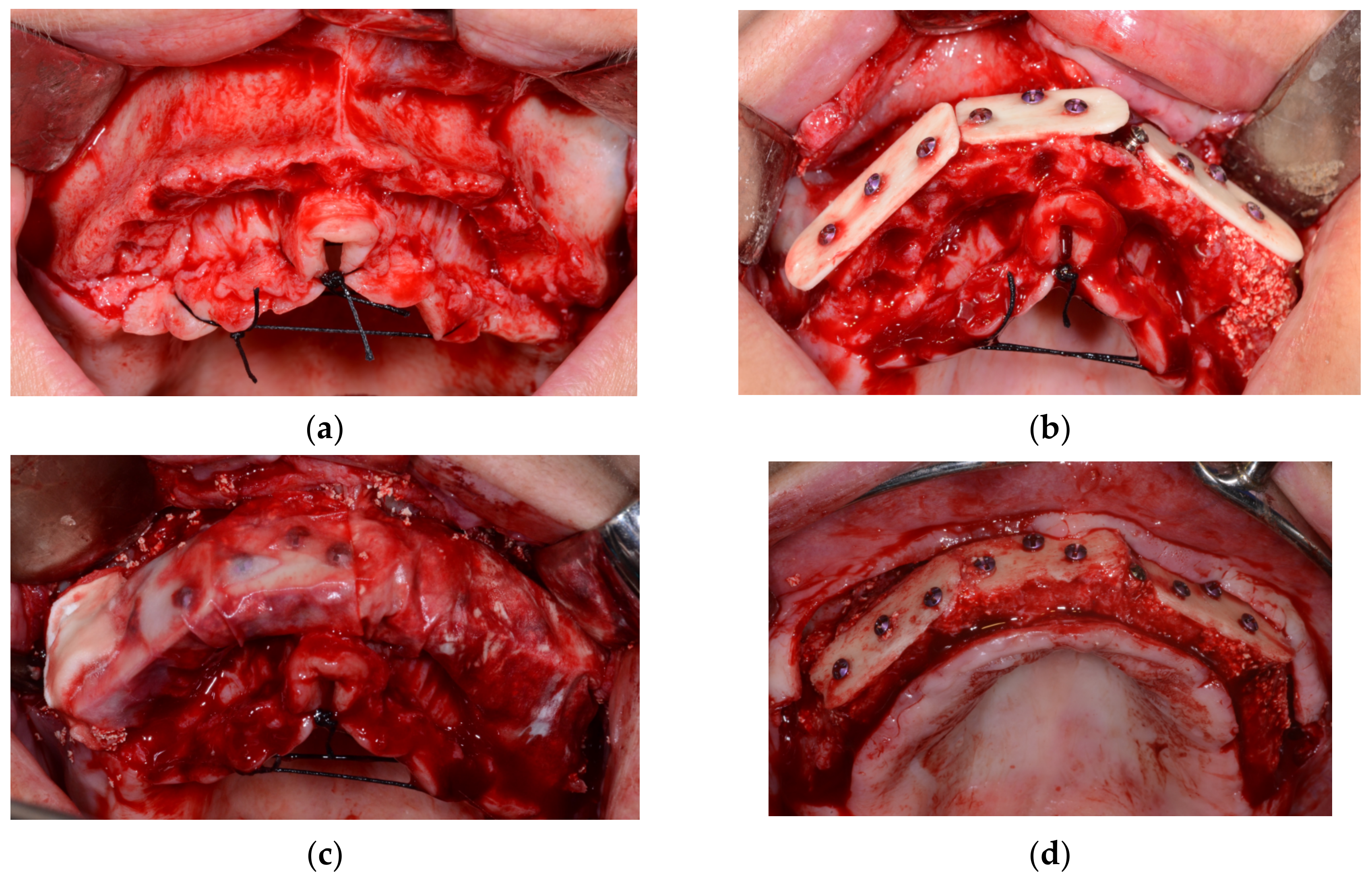
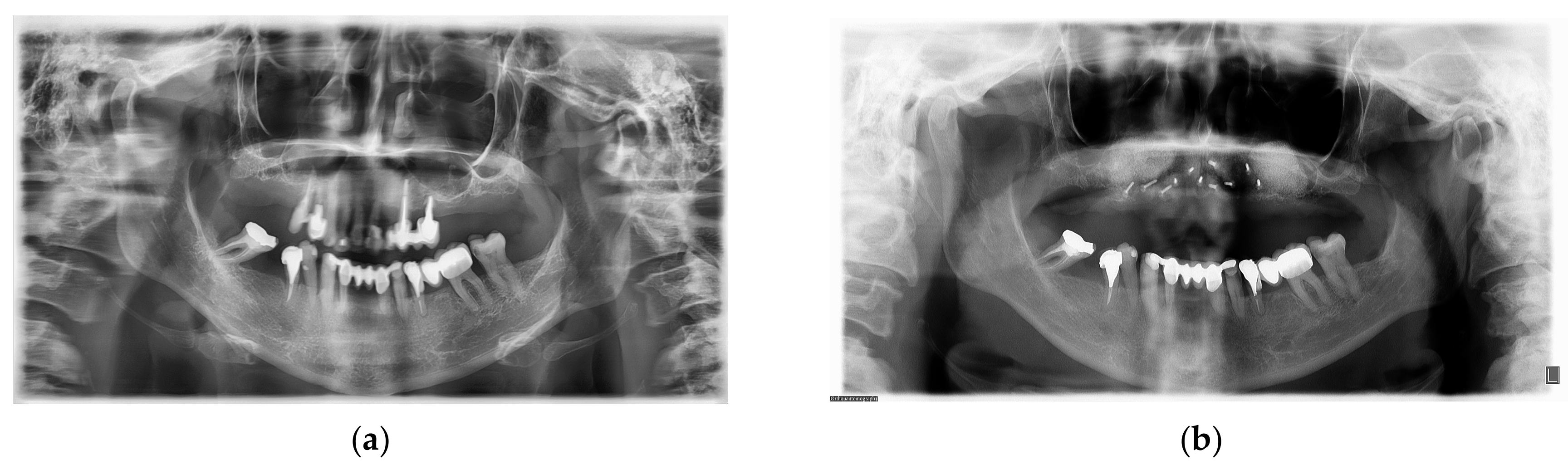
2. Case Report
3. Discussion
4. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Conflicts of Interest
References
- Schropp, L.; Wenzel, A.; Kostopoulos, L.; Karring, T. Bone healing and soft tissue contour changes following single-tooth extraction: A clinical and radiographic 12-month prospective study. Int. J. Periodontics Restor. Dent. 2003, 23, 313–323. [Google Scholar]
- Buser, D.; Martin, W.; Belser, U.C. Optimizing esthetics for implant restorations in the anterior maxilla: Anatomic and surgical considerations. Int. J. Oral. Maxillofac. Implant. 2004, 19, 43–61. [Google Scholar]
- McAllister, B.S.; Haghighat, K. Bone augmentation techniques. J. Periodontol. 2007, 78, 377–396. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Khoury, F.; Ponte, A. The three-dimensional reconstruction of the alveolar crest with mandibular bone block graft: A clinical study. Int. J. Oral. Maxillofac. Implant. 2004, 19, 765–766. [Google Scholar]
- Khoury, F.; Hanser, T. Three-Dimensional Vertical Alveolar Ridge Augmentation in the Posterior Maxilla: A 10-year Clinical Study. Int. J. Oral. Maxillofac. Implant. 2019, 34, 471–480. [Google Scholar] [CrossRef] [PubMed]
- Nefussi, J.R. Biology and physiology of the implant bone site. In Bone Augmentation in Oral Implantology; Khoury, F., Antoun, H., Missika, P., Eds.; Quintessence Books: London, UK, 2007; pp. 1–27. [Google Scholar]
- Tunkel, J.; Würdinger, R.; de Stavola, L. Vertical 3D Bone Reconstruction with Simultaneous Implantation: A Case Series Report. Int. J. Periodontics Restor. Dent. 2018, 38, 413–421. [Google Scholar] [CrossRef] [Green Version]
- Khoury, F.; Hanser, T. Mandibular bone block harvesting from the retromolar region: A 10-year prospective clinical study. Int. J. Oral. Maxillofac. Implant. 2015, 30, 688–697. [Google Scholar] [CrossRef] [Green Version]
- Sakkas, A.; Wilde, F.; Heufelder, M.; Winter, K.; Schramm, A. Autogenous bone grafts in oral implantology-is it still a “gold standard”? A consecutive review of 279 patients with 456 clinical procedures. Int. J. Implant. Dent. 2017, 3, 23. [Google Scholar] [CrossRef]
- Carlsen, A.; Gorst-Rasmussen, A.; Jensen, T. Donor site morbidity associated with autogenous bone harvesting from the ascending mandibular ramus. Implant. Dent. 2013, 22, 503–506. [Google Scholar] [CrossRef]
- Jensen, S.S.; Terheyden, H. Bone augmentation procedures in localized defects in the alveolar ridge: Clinical results with different bone grafts and bone-substitute materials. Int. J. Oral. Maxillofac. Implant. 2009, 24, 218–236. [Google Scholar]
- Hämmerle, C.H.; Jung, R.E.; Yaman, D.; Lang, N.P. Ridge augmentation by applying bioresorbable membranes and deproteinized bovine bone mineral: A report of twelve consecutive cases. Clin. Oral. Implant. Res. 2008, 19, 19–25. [Google Scholar] [CrossRef] [PubMed]
- Chisci, G.; Fredianelli, L. Therapeutic Efficacy of Bromelain in Alveolar Ridge Preservation. Antibiotics 2022, 11, 1542. [Google Scholar] [CrossRef] [PubMed]
- Sassano, P.; Gennaro, P.; Chisci, G.; Gabriele, G.; Aboh, I.V.; Mitro, V.; di Curzio, P. Calvarial onlay graft and submental incision in treatment of atrophic edentulous mandibles: An approach to reduce postoperative complications. J. Craniofac. Surg. 2014, 25, 693–697. [Google Scholar] [CrossRef] [PubMed]
- Valentini, V.; Gennaro, P.; Aboh, I.V.; Longo, G.; Mitro, V.; Ialongo, C. Iliac crest flap: Donor site morbidity. J. Craniofac. Surg. 2009, 20, 1052–1055. [Google Scholar] [CrossRef]
- Starch-Jensen, T.; Deluiz, D.; Tinoco, E.M.B. Horizontal Alveolar Ridge Augmentation with Allogeneic Bone Block Graft Compared with Autogenous Bone Block Graft: A Systematic Review. J. Oral. Maxillofac. Res. 2020, 11, e1. [Google Scholar] [CrossRef]
- Cinar, I.C.; Gultekin, B.A.; Saglanmak, A.; Akay, A.S.; Zboun, M.; Mijiritsky, E. Comparison of Allogeneic Bone Plate and Guided Bone Regeneration Efficiency in Horizontally Deficient Maxillary Alveolar Ridges. Appl. Sci. 2022, 12, 10518. [Google Scholar] [CrossRef]
- Schlee, M.; Rothamel, D. Ridge augmentation using customized allogenic bone blocks: Proof of concept and histological findings. Implant. Dent. 2013, 22, 212–218. [Google Scholar] [CrossRef] [Green Version]
- De Stavola, L.; Tunkel, J. Results of vertical bone augmentation with autogenous bone block grafts and the tunnel technique: A clinical prospective study of 10 consecutively treated patients. Int. J. Periodontics Restor. Dent. 2013, 33, 651–659. [Google Scholar] [CrossRef] [Green Version]
- Alérico, F.A.; Bernardes, S.R.; Fontão, F.N.; Diez, G.F.; Alérico, J.H.; Claudino, M. Prospective tomographic evaluation of autogenous bone resorption harvested from mandibular ramus in atrophic maxilla. J. Craniofac. Surg. 2014, 25, 543–546. [Google Scholar] [CrossRef]
- Lee, H.G.; Kim, Y.D. Volumetric stability of autogenous bone graft with mandibular body bone: Cone-beam computed tomography and three-dimensional reconstruction analysis. J. Korean Assoc. Oral. Maxillofac. Surg. 2015, 41, 232–239. [Google Scholar] [CrossRef] [Green Version]
- Von Arx, T.; Buser, D. Horizontal ridge augmentation using autogenous block grafts and the guided bone regeneration technique with collagen membranes: A clinical study with 42 patients. Clin. Oral. Implant. Res. 2006, 17, 359–366. [Google Scholar] [CrossRef] [PubMed]
- Maiorana, C.; Beretta, M.; Salina, S.; Santoro, F. Reduction of autogenous bone graft resorption by means of bio-oss coverage: A prospective study. Int. J. Periodontics Restor. Dent. 2005, 25, 19–25. [Google Scholar]
- Cordaro, L.; Torsello, F.; Morcavallo, S.; di Torresanto, V.M. Effect of bovine bone and collagen membranes on healing of mandibular bone blocks: A prospective randomized controlled study. Clin. Oral. Implant. Res. 2011, 22, 1145–1150. [Google Scholar] [CrossRef]
- Tunkel, J.; de Stavola, L.; Kloss-Brandstätter, A. Alveolar ridge augmentation using the shell technique with allogeneic and autogenous bone plates in a split-mouth design-A retrospective case report from five patients. Clin. Case Rep. 2020, 9, 947–959. [Google Scholar] [CrossRef] [PubMed]
- Pistilli, R.; Felice, P.; Piatelli, M.; Nisii, A.; Barausse, C.; Esposito, M. Blocks of autogenous bone versus xenografts for the rehabilitation of atrophic jaws with dental implants: Preliminary data from a pilot randomised controlled trial. Eur. J. Oral. Implantol. 2014, 7, 153–171. [Google Scholar] [PubMed]
- Peck, M.T. Alveolar Ridge Augmentation using the Allograft Bone Shell Technique. J. Contemp. Dent Pract. 2015, 16, 768–773. [Google Scholar] [CrossRef]
- Würdinger, R.; Donkiewicz, P. Allogeneic cortical struts and bone granules for challenging alveolar reconstructions: An innovative approach toward an established technique. J. Esthet. Restor. Dent. 2020, 32, 747–756. [Google Scholar] [CrossRef]

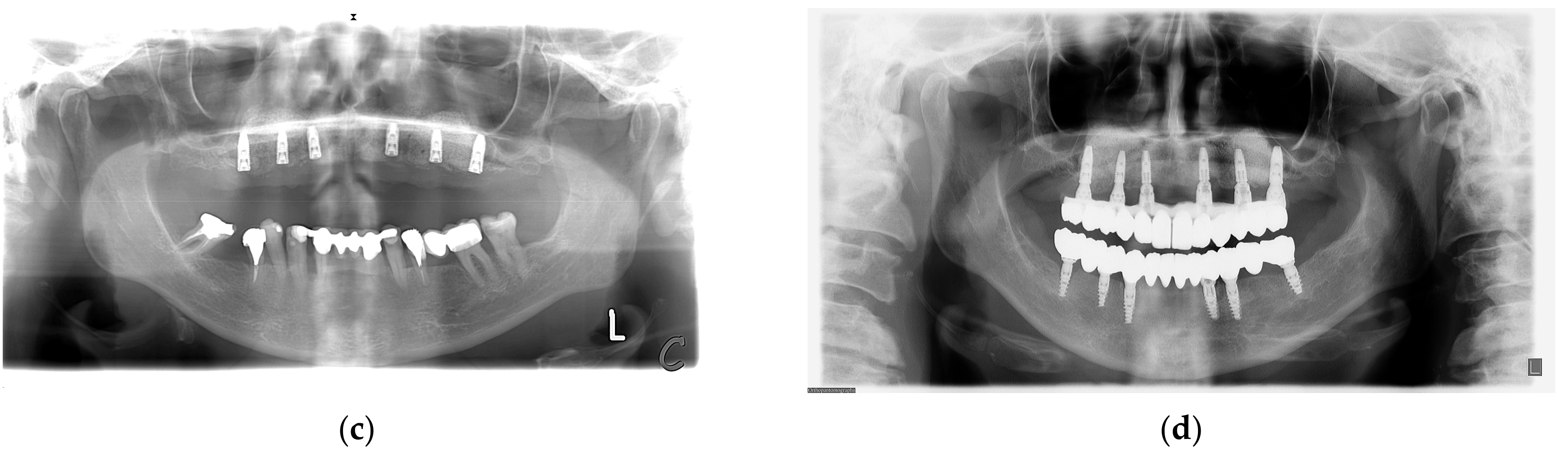
| Measurements in mm | R1 | R2 | R3 | L1 | L2 | L3 | Avg | Avg Change (%) |
|---|---|---|---|---|---|---|---|---|
| Initial situation | 7.06 | 6.3 | 2.72 | 5.85 | 4.2 | 6.74 | 5.48 | |
| Post augmentation (6 months) | 12.04 | 11.71 | 10.64 | 12.11 | 10.72 | 11.27 | 11.42 | 47.9 |
| Follow up (6 years) | 9.47 | 9.97 | 6.03 | 9.72 | 9.47 | 9.13 | 8.97 | −21.4 |
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2023 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Kovac, Z.; Cabov, T.; Blaskovic, M.; Morelato, L. Regeneration of Horizontal Bone Defect in Edentulous Maxilla Using the Allogenic Bone-Plate Shell Technique and a Composite Bone Graft—A Case Report. Medicina 2023, 59, 494. https://doi.org/10.3390/medicina59030494
Kovac Z, Cabov T, Blaskovic M, Morelato L. Regeneration of Horizontal Bone Defect in Edentulous Maxilla Using the Allogenic Bone-Plate Shell Technique and a Composite Bone Graft—A Case Report. Medicina. 2023; 59(3):494. https://doi.org/10.3390/medicina59030494
Chicago/Turabian StyleKovac, Zoran, Tomislav Cabov, Marko Blaskovic, and Luka Morelato. 2023. "Regeneration of Horizontal Bone Defect in Edentulous Maxilla Using the Allogenic Bone-Plate Shell Technique and a Composite Bone Graft—A Case Report" Medicina 59, no. 3: 494. https://doi.org/10.3390/medicina59030494





