Vermiform Appendix within Post-Laparoscopic Incisional Hernia: A Unique Case Report and Literature Review
Abstract
:1. Introduction
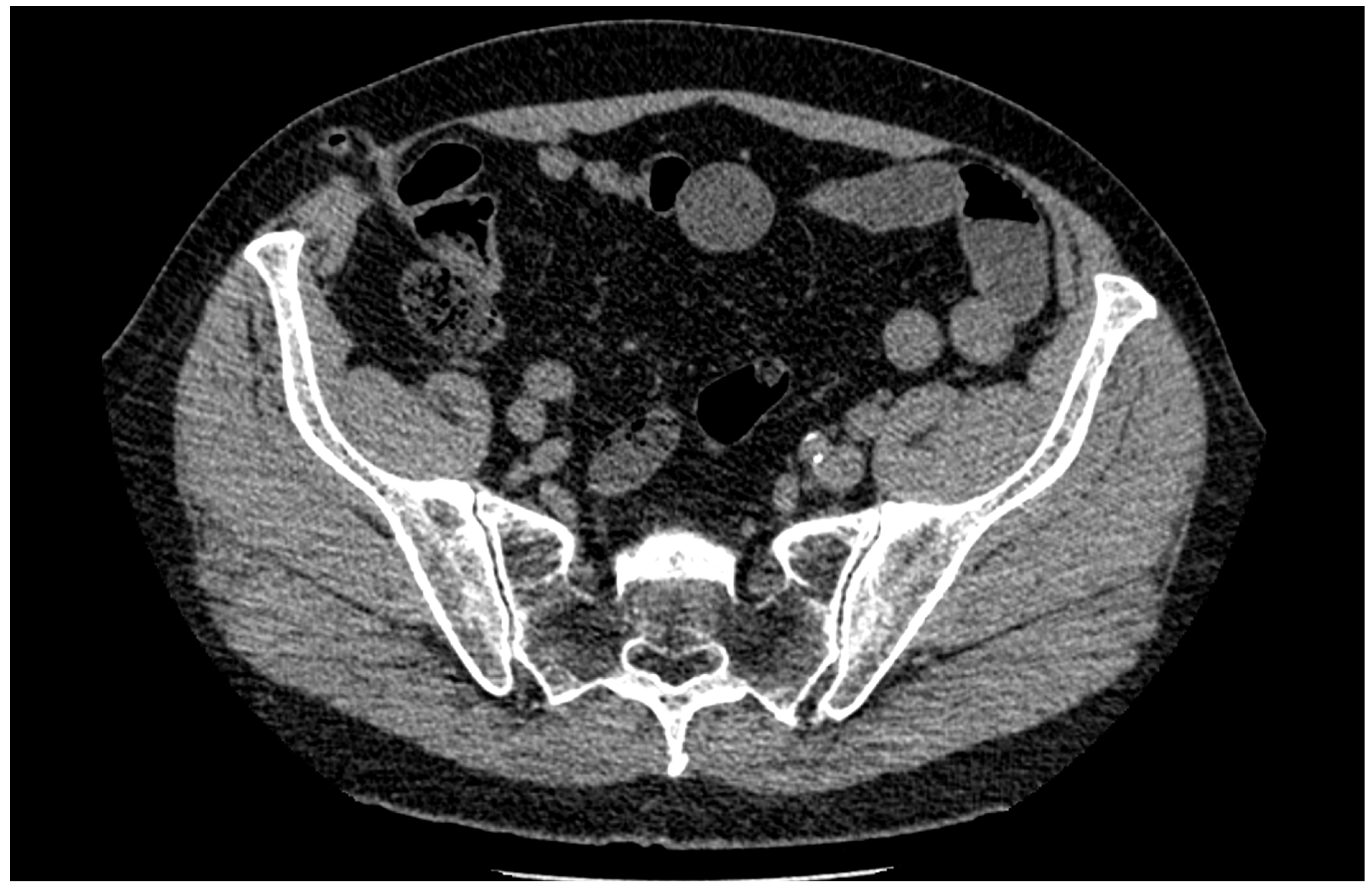
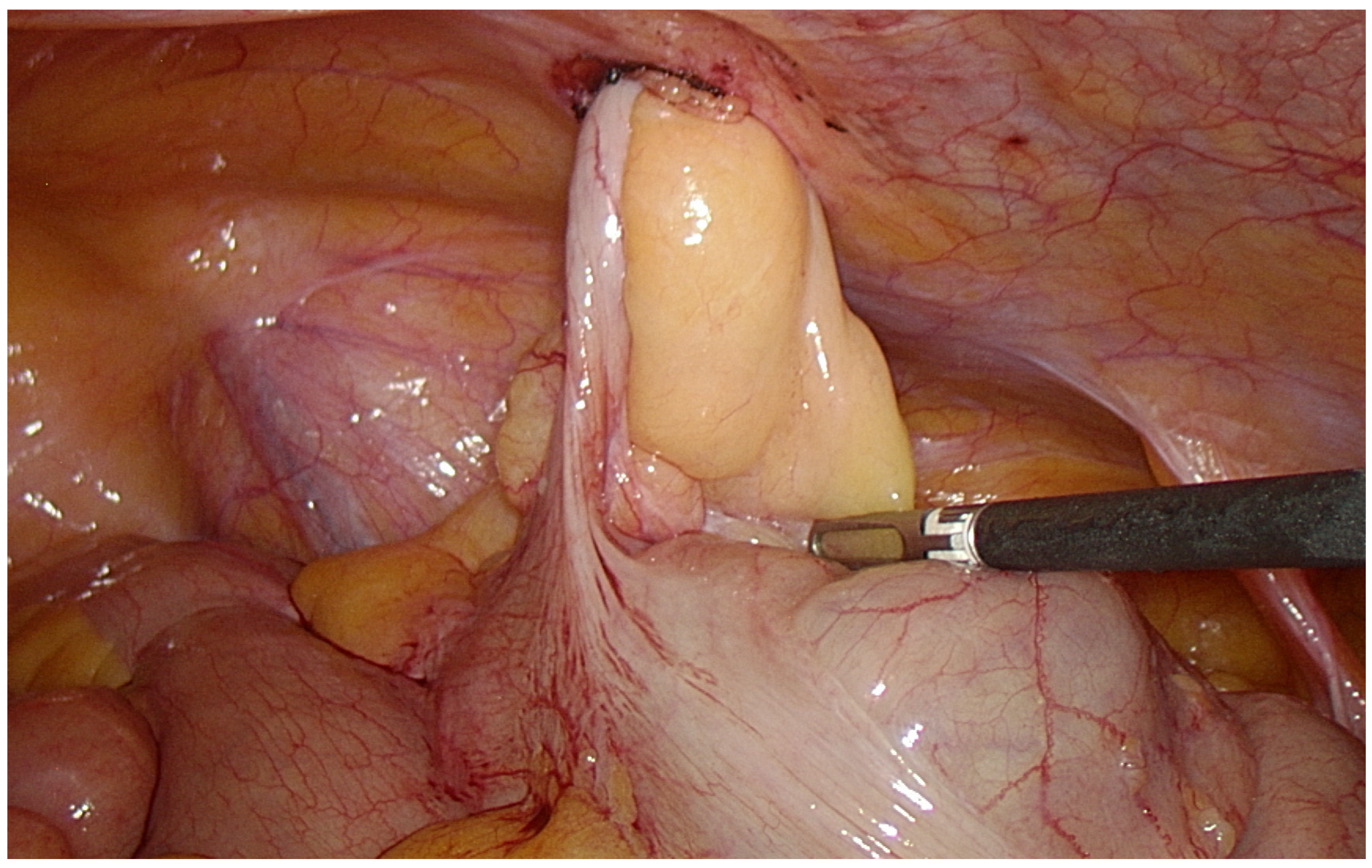
2. Case Report
3. Discussion
4. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Conflicts of Interest
References
- Ciscar, A.; Badia, J.M.; Novell, F.; Bolívar, S.; Mans, E. Incidence and risk factors for trocar-site incisional hernia detected by clinical and ultrasound examination: A prospective observational study. BMC Surg. 2020, 20, 330. [Google Scholar] [CrossRef] [PubMed]
- Issa, M.G. Acute appendicitis within incisional hernia sac: A unique case report. Egypt. J. Radiol. Nucl. Med. 2020, 51, 45. [Google Scholar] [CrossRef] [Green Version]
- Sharma, H.; Gupta, A.; Shekhawat, N.S.; Memon, B.; Memon, M.A. Amyand’s hernia: A report of 18 consecutive patients over a 15-year period. Hernia 2007, 11, 31–35. [Google Scholar] [CrossRef] [PubMed]
- Lam, A.; Black, J.; Parnell, B.; West, C. Appendicitis due to incarceration within a laparoscopic umbilical port-site hernia secondary to a degree of intestinal malrotation. Ann. R. Coll. Surg. Engl. 2019, 101, e119–e121. [Google Scholar] [CrossRef] [PubMed]
- Sugrue, C.; Hogan, A.; Robertson, I.; Mahmood, A.; Khan, W.H.; Barry, K. Incisional hernia appendicitis: A report of two unique cases and literature review. Int. J. Surg. Case Rep. 2012, 4, 256–258. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Menenakos, C.; Tsilimparis, N.; Guenther, N.; Braumann, C. Strangulated Appendix within a Trocar Site Incisional Hernia Following Laparoscopic Low Anterior Rectal Resection. A Case Report. Acta Chir. Belgica 2009, 109, 411–413. [Google Scholar] [CrossRef]
- Erol, T.; Mahmudzada, K. Uncommon case of pseudo inflammed incisional hernia. Ann. Ital. Chir. 2022, 11, S2239253X22037434. [Google Scholar]
- Paudyal, N.; Sah, S. Incisional hernia appendicitis: A unique case report. Int. J. Surg. Case Rep. 2021, 89, 106549. [Google Scholar] [CrossRef]
- Lakhani, D.A.; Dada, J.; Balar, A.B.; Khan, A.U.; Patel, Z.; Markovich, B.; Nguyen, T.P. Appendicitis in an incisional hernia sac following renal transplantation: A case report and brief review of the literature. Radio Case Rep. 2021, 16, 1736–1739. [Google Scholar] [CrossRef]
- Molina, G.A.; Rojas, C.L.; Aguayo, W.G.; Moyon, M.A.; Gálvez, P.; Polanco, E.C.; Novoa, L.P.; Reveló, V. Appendiceal hernia: An extremely rare condition. Annals 2021, 103, e50–e52. [Google Scholar] [CrossRef]
- Kler, A.; Hossain, N.; Singh, S.; Scarpinata, R. Vermiform appendix within incisional hernia. BMJ Case Rep. 2017, bcr2017221216. [Google Scholar] [CrossRef] [PubMed]
- West, C.; Richards, J.; Sujendran, V.; Wheeler, J. Spontaneous evisceration of the appendix through an incisional hernia at rest. BMJ Case Rep. 2016, 2016, bcr2016217585. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Galiñanes, E.L.; Ramaswamy, A. Appendicitis found in an incisional hernia. J. Surg. Case Rep. 2012, 2012, 3. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Dittmar, Y.; Scheuerlein, H.; Götz, M.; Settmacher, U. Adherent appendix vermiformis within an incisional hernia after kidney transplantation mimicking acute appendicitis: Report of a case. Hernia 2012, 16, 359–361. [Google Scholar] [CrossRef] [PubMed]
- Singal, R.; Mittal, A.; Gupta, A.; Gupta, S.; Sahu, P.; Sekhon, M.S. An incarcerated appendix: Report of three cases and a review of the literature. Hernia 2012, 16, 91–97. [Google Scholar] [CrossRef]
- McKay, D.W. Vermiform appendix in right upper quadrant incisional hernia. ANZ J. Surg. 2005, 75, 729–730. [Google Scholar] [CrossRef]
- Bunting, D.M. Port-Site Hernia Following Laparoscopic Cholecystectomy. JSLS J. Soc. Laparoendosc. Surg. 2010, 14, 490–497. [Google Scholar] [CrossRef] [Green Version]
- Lambertz, A.; Stüben, B.O.; Bock, B.; Eickhoff, R.; Kroh, A.; Klink, C.D.; Neumann, U.P.; Krones, C.J. Port-site incisional hernia—A case series of 54 patients. Ann. Med. Surg. 2017, 14, 8–11. [Google Scholar] [CrossRef]
- Jones, M.W.; Lopez, R.A.; Deppen, J.G. Appendicitis. In StatPearls [Internet]; StatPearls Publishing: Treasure Island, FL, USA, 2022. [Google Scholar]
- Pocard, M.; Chasserant, P.; Parc, R. Massive rectal bleeding after appendectomy: Report of 2 further cases and review of the literature. Ann. Chir. 2002, 127, 703–705. [Google Scholar] [CrossRef]
- Wu, T.; Yang, Y.; Wu, Y.; Lu, L.; Dong, S. Complications after appendectomy in patients with treated appendicitis: Results from a retrospective study. Ann. Palliat. Med. 2021, 10, 125462553. [Google Scholar] [CrossRef]
- Zahid, A. The vermiform appendix: Not a useless organ. J. Coll. Physicians Surg. Pak. 2004, 14, 256–258. [Google Scholar] [PubMed]
- Fatehi Hassanabad, A.; Zarzycki, A.N.; Jeon, K.; Deniset, J.F.; Fedak, P.W.M. Post-Operative Adhesions: A Comprehensive Review of Mechanisms. Biomedicines 2021, 9, 867. [Google Scholar] [CrossRef] [PubMed]
- Pereira, C.; Rai, R. Open Versus Laparoscopic Ventral Hernia Repair: A Randomized Clinical Trial. Cureus 2021, 13, e20490. [Google Scholar] [CrossRef] [PubMed]
- Basukala, S.; Tamang, A.; Rawal, S.B.; Malla, S.; Bhusal, U.; Dhakal, S.; Sharma, S. Comparison of outcomes of laparoscopic hernioplasty with and without fascial repair (IPOM-Plus vs IPOM) for ventral hernia: A retrospective cohort study. Ann. Med. Surg. 2022, 80, 104297. [Google Scholar] [CrossRef]
- Shahdhar, M.; Sharma, A. Laparoscopic Ventral Hernia Repair: Extraperitoneal Repair. Annals of Laparoscopic and Endoscopic Surgery. Available online: https://ales.amegroups.com/article/view/4744 (accessed on 28 September 2018).
- Schumacher, O.P.; Peiper, C.; Lörken, M.; Schumpelick, V. Long-term results after Spitzy’s umbilical hernia repair. Chirurg 2003, 74, 50–54. [Google Scholar] [CrossRef]
- Ferrari, G.C.; Miranda, A.; Sansonna, F.; Magistro, C.; Di Lernia, S.; Maggioni, D.; Franzetti, M.; Hernia, R.P. Laparoscopic management of incisional hernias ≥15 cm in diameter. Hernia 2008, 12, 571–576. [Google Scholar] [CrossRef]
- Dehn, T. Incisional Hernia Repair—Laparoscopic or Open Surgery? Ann. R. Coll. Surg. Engl. 2009, 91, 631–636. [Google Scholar] [CrossRef] [Green Version]
- Tonouchi, H.; Ohmori, Y.; Kobayashi, M.; Kusunoki, M. Trocar site hernia. Arch. Surg. 2004, 139, 1248–1256. [Google Scholar] [CrossRef] [Green Version]
- Yamamoto, M.; Minikel, L.; Zaritsky, E. Laparoscopic 5-mm Trocar Site Herniation and Literature Review. JSLS J. Soc. Laparoendosc. Surg. 2011, 15, 122–126. [Google Scholar] [CrossRef] [Green Version]
- Tarnay, C.M.; Glass, K.B.; Munro, M.G. Incision characteristics associated with six laparoscopic trocar-cannula systems: A randomized, observer-blinded comparison. Obs. Gynecol 1999, 94, 89–93. [Google Scholar] [CrossRef]
- Bhoyrul, S.; Mori, T.; Way, L.W. Radially expanding dilatation. A superior method of laparoscopic trocar access. Surg. Endosc. 1996, 10, 775–778. [Google Scholar] [CrossRef] [PubMed]

| No | Authors | Previous Operation | Location of the Hernia | Type of Performed Operation | Normal or Altered Appendix |
|---|---|---|---|---|---|
| 1 | Erol T. et al. [7] | NA | NA | NA | Inflamed |
| 2 | Paudyal N. et al. [8] | Laparotomy with right-sided salpingectomy | Pfannenstiel incision | Open surgery | Inflamed |
| 3 | Lakhani DA. et al. [9] | Left total nephrectomy and renal transplantation | Right lower quadrant incisional hernia | Open surgery | Perforated |
| 4 | Molina G. et al. [10] | Open cholecystectomy | Kocher incision | Open surgery | Inflamed |
| 5 | Lam A. et al. [4] | Laparoscopic sterilization | Umbilical laparoscopic port site incision | Open surgery | Inflamed |
| 6 | Kler A. et al. [11] | Open total hysterectomy | Pfannenstiel incision | Open surgery | Normal |
| 7 | West C. et al. [12] | Open abdominal aortic aneurysm repair | Laparotomy incision | Open surgery | NA |
| 8 | Sugrue C. et al. [5] | Open cholecystectomy | Upper midline incisional hernia | Open surgery | Inflamed |
| 9 | Sugrue C. et al. [5] | Diagnostic laparoscopy and lavage | Five mm port site in the right iliac fossa | Open surgery | Inflamed |
| 10 | Galiñanes EL. et al. [13] | Total abdominal hysterectomy with right-sided oophorectomy | Pfannenstiel incision | Laparoscopic surgery | Inflamed |
| 11 | Dittmar Y. et al. [14] | Kidney transplantation | Right lower quadrant incisional hernia | Laparoscopic surgery | Inflamed |
| 12 | Singal R. et al. [15] | Open surgery of subsequent bone grafting from the right iliac crest | Previous operation incision | Open surgery | Inflamed |
| 13 | Menenakos Ch. et al. [6] | Laparoscopic low anterior rectal resection | Twelve mm trocar site incision in the right iliac fossa | Open surgery | Inflamed |
| 14 | McKay DW. et al. [16] | Open cholecystectomy | Kocher incision | Open surgery | Normal |
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2023 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Marcinkeviciute, K.; Makunaite, G.; Danys, D.; Strupas, K. Vermiform Appendix within Post-Laparoscopic Incisional Hernia: A Unique Case Report and Literature Review. Medicina 2023, 59, 538. https://doi.org/10.3390/medicina59030538
Marcinkeviciute K, Makunaite G, Danys D, Strupas K. Vermiform Appendix within Post-Laparoscopic Incisional Hernia: A Unique Case Report and Literature Review. Medicina. 2023; 59(3):538. https://doi.org/10.3390/medicina59030538
Chicago/Turabian StyleMarcinkeviciute, Kristina, Gabija Makunaite, Donatas Danys, and Kestutis Strupas. 2023. "Vermiform Appendix within Post-Laparoscopic Incisional Hernia: A Unique Case Report and Literature Review" Medicina 59, no. 3: 538. https://doi.org/10.3390/medicina59030538





