Awareness of Placental Pathologic Examination Criteria and Utilization of Pathology Reports among Obstetricians
Abstract
1. Introduction
2. Materials and Methods
2.1. Study Subjects
2.2. Study Materials
2.3. Statistical Analysis
3. Results
3.1. Demographic Characteristics of the Participants and Their Attitude toward Pathologic Examination
3.2. Clinical Indications Used by the Participants for Pathological Placental Examination When the CAP Guidelines Were Not Used
4. Discussion
5. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Acknowledgments
Conflicts of Interest
References
- Turowski, G.; Parks, W.T.; Arbuckle, S.; Jacobsen, A.F.; Heazell, A. The structure and utility of the placental pathology report. APMIS 2018, 126, 638–646. [Google Scholar] [CrossRef] [PubMed]
- Walsh, C.A.; Mcauliffe, F.M.; Turowski, G.; Roald, B.; Mooney, E.E. A survey of obstetricians’ views on placental pathology reporting. Int. J. Gynecol. Obstet. 2013, 3, 275–277. [Google Scholar] [CrossRef] [PubMed]
- Magann, E.F.; Sills, A.; Steigman, C.; Ounpraseuth, S.T.; Odibo, I.; Sandlin, A.T. Pathologic examination of the placenta: Recommended versus observed practice in a university hospital. Int. J. Womens Health 2013, 5, 309–312. [Google Scholar] [CrossRef] [PubMed]
- Benirschke, K. The placenta in the litigation process. Am. J. Obstet. Gynecol. 1990, 162, 1145–1148. [Google Scholar] [CrossRef] [PubMed]
- Curtin, W.M.; Krauss, S.; Metlay, L.A.; Katzman, P.J. Pathologic examination of the placenta and observed practice. Obstet. Gynecol. 2007, 109, 35–41. [Google Scholar] [CrossRef]
- Odibo, I.; Gehlot, A.; Ounpraseuth, S.T.; Magann, E.F. Pathologic examination of the placenta and its clinical utility: A survey of obstetrics and gynecology providers. J. Matern. Fetal. Neonatal. Med. 2016, 29, 197–201. [Google Scholar] [CrossRef]
- Langston, C.; Kaplan, C.; Macpherson, T.; Manci, E. Practice guideline for examination of the placenta: Developed by the Placental Pathology Practice Guideline Development Task Force of the College of American Pathologists. Arch. Pathol. Lab. Med. 1997, 121, 449–476. [Google Scholar] [PubMed]
- Spencer, M.K.; Khong, T.Y. Conformity to guidelines for pathologic examination of the placenta. Arch. Pathol. Lab. Med. 2003, 127, 205–207. [Google Scholar] [CrossRef]
- Aljhdali, H.M.; Abdullah, L.S.; Alhazmi, D.A.; Almosallam, A.M.; Bondagji, N.S. Practice of Placenta Submission for Histopathological Examination, Experience of a Teaching/Tertiary Care Hospital in Saudi Arabia. Cureus 2021, 13, e17364. [Google Scholar] [CrossRef] [PubMed]
- Mubeen, A.; Makary, R. Pathologic examination of placenta: A study on 500 live births to assess conformity to College of American Pathologists (CAP) guidelines and clinicopathologic correlation. J. Matern. Fetal. Neonatal. Med. 2022, 35, 3867–3871. [Google Scholar] [CrossRef]
- Booth, V.J.; Nelson, K.B.; Dambrosia, J.M.; Grether, J.K. What factors influence whether placentas are submitted for pathologic examination? Am. J. Obstet. Gynecol. 1997, 176, 567–571. [Google Scholar] [CrossRef]
- Powsner, S.M.; Costa, J.; Homer, R.J. Clinicians are from Mars and pathologists are from Venus. Arch. Pathol. Lab. Med. 2000, 124, 1040–1046. [Google Scholar] [CrossRef] [PubMed]


| Maternal indications |
|
| Fetal indications |
|
| Placental indications |
|
| Study Demographics | Statistics, N (%) | |
|---|---|---|
| Level of training | Residents <15 years | 76 (26%) |
| Consultants/specialists <15 years | 75 (25.6%) | |
| Consultants/specialists ≥15 years | 141 (48.2%) | |
| Years of practice | <15 | 151 (51.7%) |
| ≥15 | 141 (48.2%) | |
| Institution | Government hospital | 252 (86.3%) |
| University hospital | 40 (13.7%) | |
| Survey Questions | Statistics, N (%) | |
| Do you routinely send placenta for pathologic examination? | No | 239 (81.8%) |
| Yes | 53 (18.2%) | |
| Are you aware of the CAP guidelines for placental pathology evaluation? | No | 192 (65.7%) |
| Yes | 100 (34.2%) | |
| Given an awareness of the CAP guidelines, are they clinically useful? | No | 56 (19.1%) |
| Yes | 236 (80.9%) | |
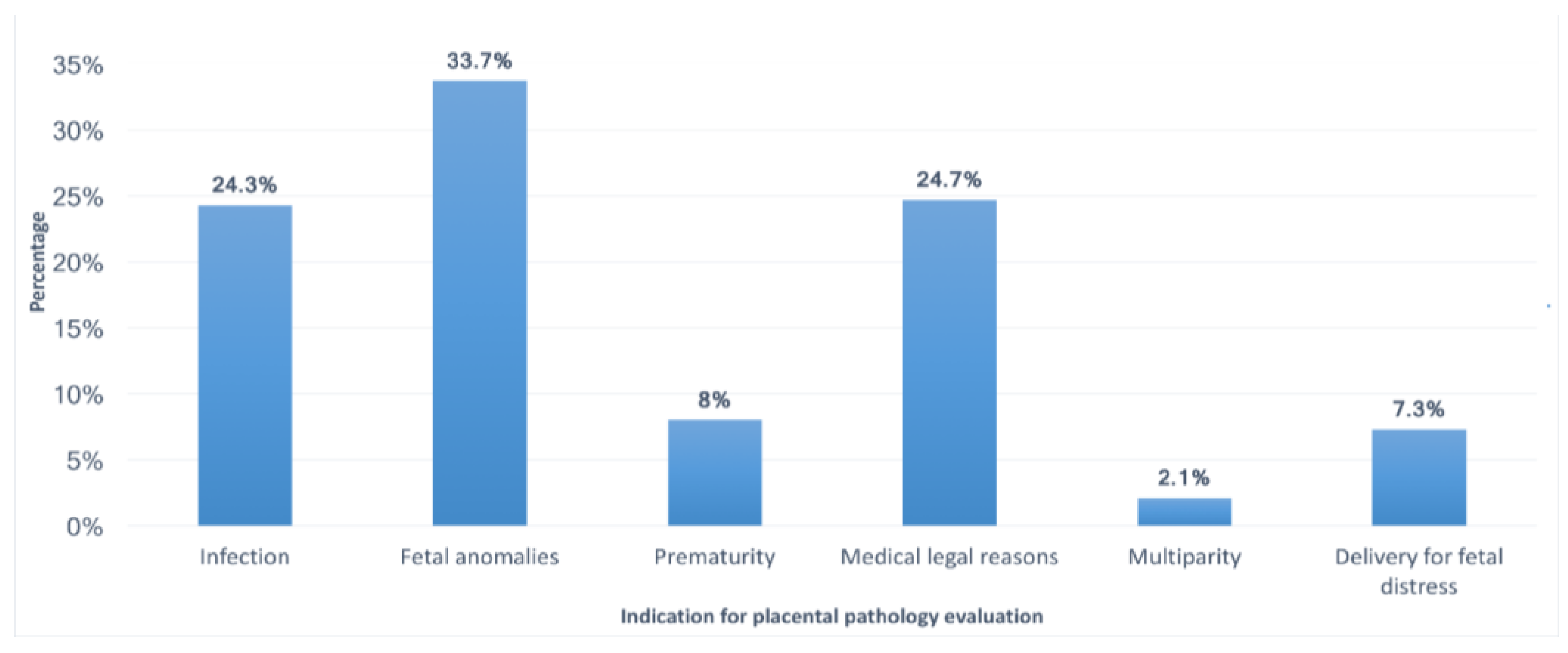
| If the CAP guidelines are not used, how do you determine the need for pathology evaluation? | Infection | 72 (24.6%) |
| Fetal anomalies | 99 (33.9%) | |
| Prematurity | 23 (7.9%) | |
| Medicolegal reasons | 71 (24.3%) | |
| Multiparty | 6 (2.1%) | |
| Delivery for fetal distress | 21 (7.2%) | |
| Do you routinely review pathology reports? | No | 86 (29.5%) |
| Yes | 206 (70.5%) | |
| If you routinely review reports, do you understand the nomenclature of the report? | No | 81 (27.7%) |
| Yes | 211 (72.3%) | |
| Are the pathology reports useful? | No | 29 (9.9%) |
| Yes | 263 (90.1%) | |
| Has the result of a placenta examination ever been useful to you in a medicolegal situation? | No | 109 (37.3%) |
| Yes | 183 (62.7%) | |
| Should we continue to send placentas for pathological evaluation? | No | 38 (13.0%) |
| Yes | 254 (87.0%) | |
| Survey Questions | Government Hospital | University Hospital | p-Value | |
|---|---|---|---|---|
| Do you routinely send placenta for pathologic examination? | No | 205 (81.3%) | 34 (85%) | 0.387 |
| Yes | 47 (18.6%) | 6 (15%) | ||
| Are you aware of the CAP guidelines for placental pathology evaluation? | No | 163 (64.6%) | 29 (72.5%) | 0.211 |
| Yes | 89 (35.3%) | 11 (27.5%) | ||
| Given an awareness of the CAP guidelines, are they clinically useful? | No | 45 (17.8%) | 11 (27.5%) | 0.11 |
| Yes | 207 (82.1%) | 29 (72.5%) | ||
| Do you routinely review pathology reports? | No | 85 (33.7%) | 1 (2.5%) | 0.000 |
| Yes | 167 (66.2%) | 39 (97.5%) | ||
| If you routinely review reports, do you understand the nomenclature of the report? | No | 80 (31.7%) | 1 (2.5%) | 0.000 |
| Yes | 172 (68.2%) | 39 (97.5%) | ||
| Are the pathology reports useful? | No | 28 (11.1%) | 1 (2.5%) | 0.064 |
| Yes | 224 (88.8%) | 39 (97.5%) | ||
| Has the result of a placenta examination ever been useful to you in a medicolegal situation? | No | 91 (36.1%) | 18 (45%) | 0.189 |
| Yes | 161 (63.1%) | 22 (55%) | ||
| Should we continue to send placentas for pathological evaluation? | No | 34 (13.1%) | 4 (10%) | 0.389 |
| Yes | 218 (86.9%) | 36 (90%) | ||
| Survey Questions | Consultant/Specialist with ≥15 Years of Experience | Consultant/Specialist with <15 Years of Experience | Resident (<15 Years of Experience) | p-Value | |
|---|---|---|---|---|---|
| Do you routinely send placenta for pathologic examination? | No | 116 (82.2%) | 60 (81.0%) | 63 (82.8%) | 0.974 |
| Yes | 25 (17.7%) | 15 (20%) | 13 (17.1%) | ||
| Are you aware of the CAP guidelines for placental pathology evaluation? | No | 87 (61.7%) | 48 (64%) | 57 (75%) | 0.184 |
| Yes | 54 (38.3%) | 27 (36.0%) | 19 (25.0%) | ||
| Given an awareness of the CAP guidelines, are they clinically useful? | No | 25 (17.7%) | 9 (12.0%) | 22 (28.9%) | 0.037 |
| Yes | 116 (82.2%) | 66 (88%) | 54 (71.1%) | ||
| Do you routinely review pathology reports? | No | 34 (24.1%) | 17 (22.6%) | 35 (46.1%) | 0.002 |
| Yes | 107 (75.8%) | 58 (77.3%) | 41 (53.9%) | ||
| If you routinely review reports, do you understand the nomenclature of the report? | No | 30 (21.2%) | 12 (16.0%) | 39 (53.9%) | 0.000 |
| Yes | 111 (78.7%) | 62 (84.0%) | 37 (48.6%) | ||
| Are the pathology reports useful? | No | 20 (14.1%) | 3 (4.0%) | 6 (7.8%) | 0.049 |
| Yes | 121 (85.8%) | 72 (96%) | 70 (92.1%) | ||
| Has the result of a placenta examination ever been useful to you in a medicolegal situation? | No | 48 (34.0%) | 27 (36.1%) | 34 (44.7%) | 0.326 |
| Yes | 93 (65.9%) | 48 (64%) | 42 (55.1%) | ||
| Should we continue to send placentas for pathological evaluation? | No | 21 (14.8%) | 5 (6.7%) | 12 (15.7%) | 0.192 |
| Yes | 120 (85.1%) | 70 (93.3%) | 64 (85.2%) |
| Variables | Odds Ratio (95% Confidence Interval), Estimate | |||||||
|---|---|---|---|---|---|---|---|---|
| Aware of the CAP Guidelines | Send Placenta | Usefulness of CAP Guidelines | Nomenclature of Report | Review Pathology Reports | Pathology Reports Are Useful | Placenta Examination Usefulness | Continue to Send Placentas | |
| Level of experience (Ref: resident) | 0.866 (0.536–1.399), −0.144 | 0.445 (0.256–0.773), −0.810 | 2.920 (1.669–5.107), 1.071 | 10.674 (5.368–21.222), 2.368 | 6.313 (3.450–11.553), 1.843 | 8.338 (2.926–23.764), 2.121 | 1.420 (0.894–2.256), 0.351 | 4.881 (2.318–10.274), 1.585 |
| Years of experience (Less than 15 years) | 0.564 (0.350–0.907), −0.573 | 0.529 (0.298–0.941), −0.636 | 1.512 (0.841–2.719), 0.413 | 2.581 (1.341–4.967), 0.948 | 2.166 (1.209–3.881), 0.773 | 13.330 (4.276–41.551), 2.590 | 0.897 (0.563–1.430), −0.109 | 4.241 (1.935–9.297), 1.445 |
| Institution (university vs. government hospital) | 0.811 (0.471–1.398), −0.209 | 0.562 (0.300–1.055), −0.575 | 1.773 (0.933–3.369), 0.573 | 0.259 (0.122–0.549), −1.350 | 0.362 (0.185–0.708), −1.016 | 0.610 (0.200–1.860), −0.494 | 1.454 (0.854–2.478), 0.375 | 1.077 (0.474–2.447), 0.74 |
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2023 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
AlOdaini, A.; AlKhalifah, G.; Alafghani, L.; Jalalah, N.B.; Alsuwailem, N.; AlMomen, Z. Awareness of Placental Pathologic Examination Criteria and Utilization of Pathology Reports among Obstetricians. Medicina 2023, 59, 574. https://doi.org/10.3390/medicina59030574
AlOdaini A, AlKhalifah G, Alafghani L, Jalalah NB, Alsuwailem N, AlMomen Z. Awareness of Placental Pathologic Examination Criteria and Utilization of Pathology Reports among Obstetricians. Medicina. 2023; 59(3):574. https://doi.org/10.3390/medicina59030574
Chicago/Turabian StyleAlOdaini, Amal, Ghaida AlKhalifah, Lina Alafghani, Nawal Bin Jalalah, Norah Alsuwailem, and Zainab AlMomen. 2023. "Awareness of Placental Pathologic Examination Criteria and Utilization of Pathology Reports among Obstetricians" Medicina 59, no. 3: 574. https://doi.org/10.3390/medicina59030574
APA StyleAlOdaini, A., AlKhalifah, G., Alafghani, L., Jalalah, N. B., Alsuwailem, N., & AlMomen, Z. (2023). Awareness of Placental Pathologic Examination Criteria and Utilization of Pathology Reports among Obstetricians. Medicina, 59(3), 574. https://doi.org/10.3390/medicina59030574




