Impact of Long-Term Cyclamate and Saccharin Consumption on Biochemical Parameters in Healthy Individuals and Type 2 Diabetes Mellitus Patients
Abstract
:1. Introduction
2. Materials and Methods
2.1. Study Design and Sampling
2.2. Study Groups
2.3. Collection of Samples
2.4. Methods
2.5. Statistical Analysis
3. Results
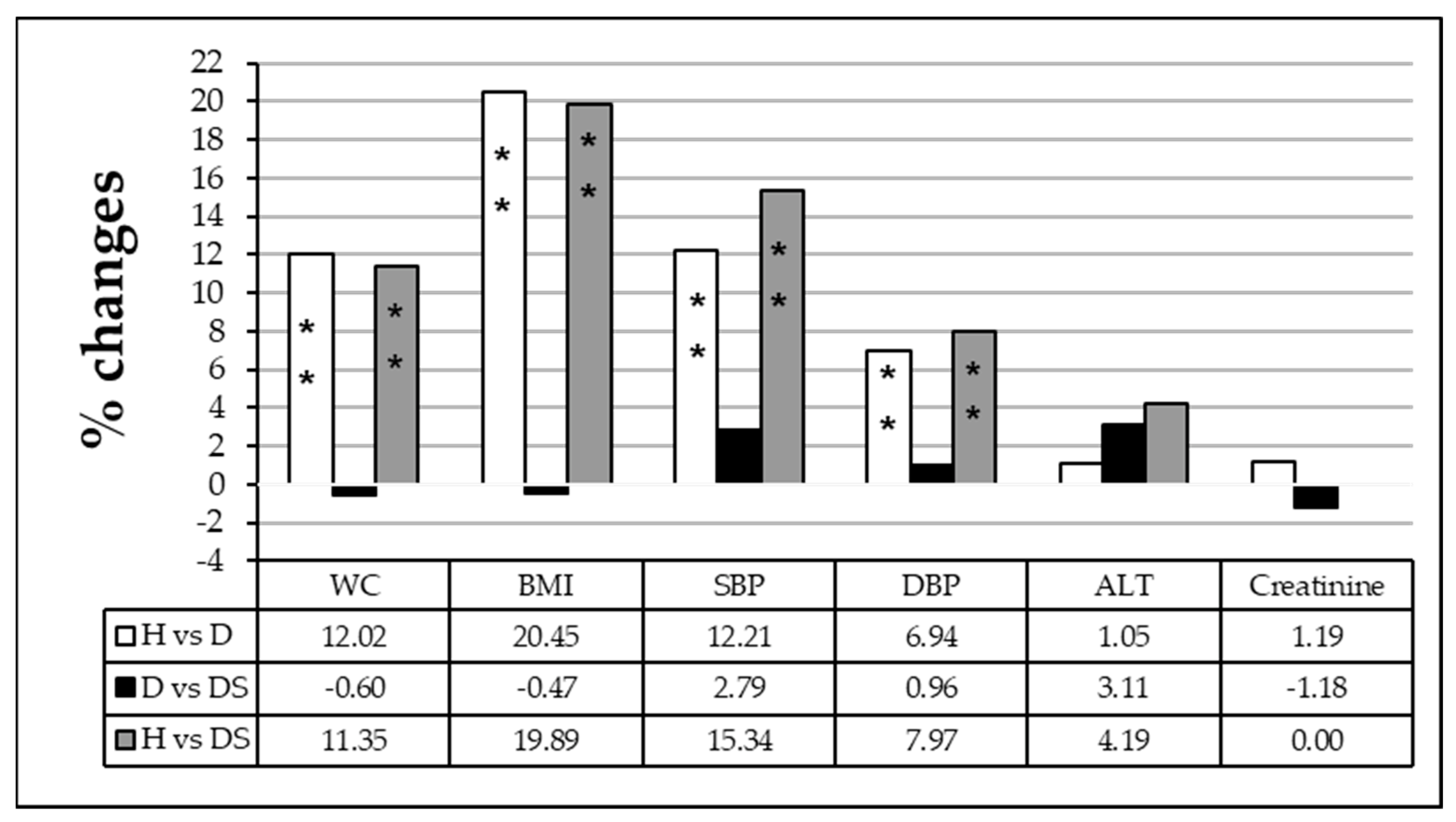
3.1. Effect of Long-Term Consumption of Artificial Sweeteners on Anthropometric and Biochemical Parameters in Diabetic Patients
3.1.1. Effect of Long-Term Artificial Sweetener Consumption on Lipid Profile
3.1.2. Effect of Long-Term Artificial Sweetener Consumption on Oxidative Stress Biomarkers
3.1.3. Effect of the Amount of Sweetener Consumed Daily by Diabetic Patients on Anthropometric and Biochemical Parameters
3.1.4. Effect of the Duration of Daily Sweetener Consumption
4. Discussion
4.1. Effect of Artificial Sweeteners Consumption on Anthropometric Measurements
4.2. Effect of Artificial Sweeteners Consumption on Serum Glucose and Glycated Hemoglobin
4.3. Effect of Artificial Sweeteners Consumption on the Liver and Renal Functions
4.4. Effect of Artificial Sweeteners Consumption on Lipid Profile
4.5. Effect of Artificial Sweetener Consumption on Biomarkers of Serum Oxidative Stress
5. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Acknowledgments
Conflicts of Interest
References
- Wadhwa, P.D.; Buss, C.; Entringer, S.; Swanson, J.M. Developmental Origins of Health and Disease: Brief History of the Approach and Current Focus on Epigenetic Mechanisms. Semin. Reprod. Med. 2009, 27, 358–368. [Google Scholar] [CrossRef] [PubMed]
- Arshad, S.; Rehman, T.; Saif, S.; Rajoka, M.S.R.; Ranjha, M.M.A.N.; Hassoun, A.; Aadil, R.M. Replacement of refined sugar by natural sweeteners: Focus on potential health benefits. Heliyon 2022, 8, e10711. [Google Scholar] [CrossRef] [PubMed]
- Saad, A.; Khan, F.A.; Hayee, A.; Nazir, M.S. A Review on Potential Toxicity of Artificial Sweetners vs Safety of Stevia: A Natural Bio-Sweetner. J. Biol. Agric. Healthc. 2014, 4, 137–148. [Google Scholar]
- Saraiva, A.; Carrascosa, C.; Raheem, D.; Ramos, F.; Raposo, A. Natural Sweeteners: The Relevance of Food Naturalness for Consumers, Food Security Aspects, Sustainability and Health Impacts. Int. J. Environ. Res. Public Health 2020, 17, 6285. [Google Scholar] [CrossRef]
- Surana, S.J.; Gokhale, S.B.; Rajmane, R.A.; RB Jadhav, R.B. Non-saccharide natural intense sweeteners an overview of current status. Nat. Prod. Radiance 2006, 5, 270–278. [Google Scholar]
- Mukhopadhyay, M.; Mukherjee, A.; Chakrabarti, J. In vivo cytogenetic studies on blends of aspartame and acesulfame-K. Food Chem. Toxicol. 2000, 38, 75–77. [Google Scholar] [CrossRef]
- Popkin, B.M.; Hawkes, C. Sweetening of the global diet, particularly beverages: Patterns, trends, and policy responses. Lancet Diabetes Endocrinol. 2016, 4, 174–186. [Google Scholar] [CrossRef]
- Bandyopadhyay, A.; Ghoshal, S.; Mukherjee, A. Genotoxicity Testing of Low-Calorie Sweeteners. Drug Chem. Toxicol. 2008, 31, 447–457. [Google Scholar] [CrossRef]
- Chattopadhyay, S.; Raychaudhuri, U.; Chakraborty, R. Artificial sweeteners—A review. J. Food Sci. Technol. 2014, 51, 611–621. [Google Scholar] [CrossRef]
- Hinson, A.L.; Nicol, W.M. Monitoring sweetener consumption in Great Britain. Food Addit. Contam. 1992, 9, 669–680. [Google Scholar] [CrossRef]
- Zeynep, F.; Sifa, T. Determination of the effects of some artificial sweeteners on human peripheral lymphocytes using the comet assay. J. Toxicol. Environ. Health Sci. 2014, 6, 147–153. [Google Scholar] [CrossRef]
- Swithers, S.E.; Martin, A.A.; Clark, K.M.; Laboy, A.F.; Davidson, T. Body weight gain in rats consuming sweetened liquids. Effects of caffeine and diet composition. PMC 2011, 55, 528–533. [Google Scholar] [CrossRef]
- Yoshikawa, T.; Naito, Y. What is oxidative stress? Jpn. Med. Assoc. J. 2002, 45, 271–276. [Google Scholar]
- Amin, K.A.; Al-Muzafar, H.M.; Elsttar, A.H.A. Effect of sweetener and flavoring agent on oxidative indices, liver and kidney function levels in rats. Ind. J. Exp. Biol. 2016, 54, 56–63. [Google Scholar]
- Abdallah, I.Z. Physiological Changes Induced by Long Term Administration of Saccharin Compared with Aspartame to Male Albino Rats. Egypt. J. Hosp. Med. 2002, 8, 70–81. [Google Scholar] [CrossRef]
- Trinder, P. Determination of Glucose in Blood Using Glucose Oxidase with an Alternative Oxygen Acceptor. Ann. Clin. Biochem. 1969, 6, 24–27. [Google Scholar] [CrossRef]
- Allain, C.C.; Poon, L.S.; Chan, C.S.; Richmond, W.; Fu, P.C. Enzymatic Determination of Total Serum Cholesterol. Clin. Chem. 1974, 20, 470–475. [Google Scholar] [CrossRef]
- Fossati, P.; Prencipe, L. Serum triglycerides determined colorimetrically with an enzyme that produces hydrogen peroxide. Clin. Chem. 1982, 28, 2077–2080. [Google Scholar] [CrossRef]
- Burtis, C.A.; Ashwood, E.R.; Saunders, W.B. Tietz Textbook of Clinical Chemistry, 3rd ed.; WB Saunders: Philadelphia, PA, USA, 1999; p. 283. [Google Scholar]
- Vujovic, A.; Kotur-Stevuljevic, J.; Spasic, S.; Bujisic, N.; Martinovic, J.; Vujovic, M.; Spasojevic-Kalimanovska, V.; Zeljkovic, A.; Pajic, D. Evaluation of different formulas for LDL-C calculation. Lipids Health Dis. 2010, 9, 27. [Google Scholar] [CrossRef]
- Delanghe, J.R.; Speeckaert, M.M. Creatinine determination according to Jaffe—What does it stand for? NDT Plus 2011, 4, 83–86. [Google Scholar] [CrossRef]
- Menden, E.E.; Boiano, J.M.; Murthy, L.; Petering, H.G. Modification of a P-Phenylenediamine Oxidase Method to Permit Non-Automated Ceruloplasmin Determinations in batches of Rat Serum or Plasma Microsamples. Anal. Lett. 1977, 10, 197–204. [Google Scholar] [CrossRef]
- Louis, W.Y.; Latriano, L.; Duncan, S.; Hartwick, R.A.; Witz, G. High-performance liquid chromatography analysis of the thiobarbituric acid adducts of malonaldehyde and trans, trans-muconaldehyde. Anal. Biochem. 1986, 156, 326–333. [Google Scholar]
- Sinnhuber, R.O.; Yu, T.C.; Yu, T.C. Characterization of the red pigment formed in the 2-thiobarbituric acid determination of oxidative rancidity. Food Res. 1958, 23, 626–634. [Google Scholar] [CrossRef]
- Louis, W.Y.; Latriano, L.; Duncan, S.; Hartwick, R.A.; Witz, G. Intracellular but not extracellular conversion of nitroxyl anion into nitric oxide leads to stimulation of human neutrophil migration. Biochem. J. 1998, 330, 719–722. [Google Scholar]
- Stanley, R.M.D.; Sam Frankel, P.D. A colorimetric method for the determination of serum glutamic oxalacetic and glutamic pyruvic transaminases. Am. J. Clin. Pathol. 1957, 28, 56–63. [Google Scholar]
- Hadwan, M.H.; Abed, H.N. Data in Brief Data supporting the spectrophotometric method for the estimation of catalase activity. Data Brief 2016, 6, 194–199. [Google Scholar] [CrossRef]
- Pang, M.D.; Goossens, G.H.; Blaak, E.E. The Impact of Artificial Sweeteners on Body Weight Control and Glucose Homeostasis. Front. Nutr. 2021, 7, 598340. [Google Scholar] [CrossRef]
- Davidson, T.L.; Swithers, S.E. A Pavlovian approach to the problem of obesity. Int. J. Obes. 2004, 28, 933–935. [Google Scholar] [CrossRef]
- Bray, G.A.; Nielsen, S.J.; Popkin, B.M. Consumption of high-fructose corn syrup in beverages may play a role in the epidemic of obesity. Am. J. Clin. Nutr. 2004, 79, 537–543. [Google Scholar] [CrossRef]
- Swithers, S.E.; Davidson, T.L. A role for sweet taste: Calorie predictive relations in energy regulation by rats. Behav. Neurosci. 2008, 122, 161–173. [Google Scholar] [CrossRef]
- Hampton, T. Sugar Substitutes Linked to Weight Gain. JAMA 2008, 299, 2137–2138. [Google Scholar] [CrossRef]
- Tandel, K.R. Sugar substitutes: Health controversy over perceived benefits. J. Pharmacol. Pharmacother. 2011, 2, 236–243. [Google Scholar] [CrossRef]
- Nguyen, S.; Choi, H.K.; Lustig, R.H. Sugar Sweetened Beverages, Serum Uric Acid, and Blood Pressure in Adolescents. J. Pediatr. 2009, 154, 807–813. [Google Scholar] [CrossRef]
- Karalius, V.P.; Shoham, D.A. Dietary Sugar and Artificial Sweetener Intake and Chronic Kidney Disease: A Review. Adv. Chronic Kidney Dis. 2013, 20, 157–164. [Google Scholar] [CrossRef]
- Dhingra, R.; Sullivan, L.; Jacques, P.F.; Wang, T.J.; Fox, C.S.; Meigs, J.B.; D’Agostino, R.B.; Gaziano, J.M.; Vasan, R.S. Soft Drink Consumption and Risk of Developing Cardiometabolic Risk Factors and the Metabolic Syndrome in Middle-Aged Adults in the Community. Circulation 2007, 116, 480–488. [Google Scholar] [CrossRef]
- Gougeon, R.; Spidel, M.; Lee, K.; Field, C.J. Canadian Diabetes Association National Nutrition Commitee Technicl Review: Non-nutritive Intense Sweeteners in Diabetis Management. Can. J. Diabetes 2004, 28, 385–399. [Google Scholar]
- Suez, J.; Korem, T.; Zeevi, D.; Zilberman-Schapira, G.; Thaiss, C.A.; Maza, O.; Israeli, D.; Zmora, N.; Gilad, S.; Weinberger, A.; et al. Artificial sweeteners induce glucose intolerance by altering the gut microbiota. Nature 2014, 514, 181–186. [Google Scholar] [CrossRef]
- Garden, L.; Paterson, K. Artificial sweeteners and glucose intolerance: A dietitians’ perspective. Pract. Diabetes 2015, 32, 73–75. [Google Scholar] [CrossRef]
- Brown, R.J.; De Banate, M.A.; Rother, K.I. Artificial Sweeteners: A systematic review of metabolic effects in youth Rebecca. Int. J. Pediatr. Obes. 2010, 5, 305–312. [Google Scholar] [CrossRef]
- Abdelaziz, I.; Ashour, A.E.R.A. Effect of saccharin on albino rats’ blood indices and the therapeutic action of vitamins C and E. Hum. Exp. Toxicol. 2011, 30, 129–137. [Google Scholar] [CrossRef]
- Azeez, O.H.; Alkass, S.Y.; Persike, D.S. Long-Term Saccharin Consumption and Increased Risk of Obesity, Diabetes, Hepatic Dysfunction, and Renal Impairment in Rats. Medicina 2019, 55, 681. [Google Scholar] [CrossRef] [PubMed]
- Alkafafy, M.E.-S.; Ibrahim, Z.S.; Ahmed, M.; El-Shazly, S.A. Impact of aspartame and saccharin on the rat liver: Biochemical, molecular, and histological approach. Int. J. Immunopathol. Pharmacol. 2015, 28, 247–255. [Google Scholar] [CrossRef] [PubMed]
- Turley, S.D.; Dietschy, J.M. Sterol absorption by the small intestine. Curr. Opin. Infect. Dis. 2003, 14, 233–240. [Google Scholar] [CrossRef] [PubMed]
- Sharma, S.; Goyal, R.P.; Chakravarty, G.; Sharma, A. Tomato red toxicity: Hematological and serological changes in the blood of albino mice, Mus Musculus. Indian J. Environ. Sci. 2006, 10, 145–148. [Google Scholar]
- Amin, K.A.; Almuzafar, H.M. Alterations in lipid profile, oxidative stress and hepatic function in rat fed with saccharin and methyl-salicylates. Int. J. Clin. Exp. Med. 2015, 8, 6133–6144. [Google Scholar]
- Osfor, M.M.; Elias, T.R. Nutritional and biochemical studies on some artificial sweerteners administrated to male albino rats. Bull. Nat. Res. Cent. 2003, 28, 377–401. [Google Scholar]
- Jang, W.; Jeoung, N.H.; Cho, K.H. Modified apolipoprotein (apo) A-I by artificial sweetener causes severe premature cellular senescence and atherosclerosis with impairment of functional and structural properties of apoA-I in lipid-free and lipid-bound state. Mol. Cells 2011, 31, 461–470. [Google Scholar] [CrossRef]
- Schiano, C.; Grimaldi, V.; Scognamiglio, M.; Costa, D.; Soricelli, A.; Nicoletti, G.F.; Napoli, C. Soft drinks and sweeteners intake: Possible contribution to the development of metabolic syndrome and cardiovascular diseases. Beneficial or detrimental action of alternative sweeteners? Food Res. Int. 2021, 142, 110220. [Google Scholar] [CrossRef]
- Cho, K.H. Biomedicinal implications of high-density lipoprotein: Its composition, structure, functions, and clinical applications. BMB Rep. 2009, 42, 393–400. [Google Scholar] [CrossRef]
- Feng, H.; Li, X.-A. Dysfunctional high-density lipoprotein. Curr. Opin. Endocrinol. Diabetes 2009, 16, 156–162. [Google Scholar] [CrossRef]
- Park, K.-H.; Jang, W.; Kim, K.-Y.; Kim, J.-R.; Cho, K.-H. Fructated apolipoprotein A-I showed severe structural modification and loss of beneficial functions in lipid-free and lipid-bound state with acceleration of atherosclerosis and senescence. Biochem. Biophys. Res. Commun. 2010, 392, 295–300. [Google Scholar] [CrossRef]
- Vaziri, N.D. Oxidative stress in uremia: Nature, mechanisms, and potential consequences. Semin. Nephrol. 2004, 24, 469–473. [Google Scholar] [CrossRef]
- Al-Saleh, A.M.; Corkey, B.; Deeney, J.; Tornheim, K.; Bauer, E. Effect of artificial sweeteners on insulin secretion, ROS, and oxygen consumption in pancreatic beta cells. FASEB J. 2011, 25, 530–531. [Google Scholar]
- Frenkel, K. Carcinogen-mediated oxidant formation and oxidative DNA damage. Pharm. Ther. 1992, 53, 127–166. [Google Scholar] [CrossRef]
- Jourd’heuil, D.; Jourd’heuil, F.L.; Kutchukian, P.S.; Musah, R.A.; Wink, D.A.; Grisham, M.B. Reaction of superoxide and nitric oxide with peroxynitrite. Implications for peroxynitrite-mediated oxidation reactions in vivo. J. Biol. Chem. 2001, 276, 28799–28805. [Google Scholar] [CrossRef]
- Ischiropoulos, H.; Zhu, L.; Chen, J.; Tsai, M.; Martin, J.C.; Smith, C.D.; Beckman, J.S. Peroxynitrite-mediated tyrosine nitration catalyzed by superoxide dismutase. Arch. Biochem. Biophys. 1992, 298, 431–437. [Google Scholar] [CrossRef]
- Beckmann, J.S.; Zu Ye, Y.; Anderson, P.G.; Chen, J.; Accavitti, M.A.; Tarpey, M.M.; White, C.R. Extensive Nitration of Protein Tyrosines in Human Atherosclerosis Detected by Immunohistochemistry. Biol. Chem. Hoppe-Seyler 1994, 375, 81–88. [Google Scholar] [CrossRef]
- Harris, Z.L. Aceruloplasminemia. J. Neurol. Sci. 2003, 207, 108–109. [Google Scholar] [CrossRef]
- Shukla, N.; Maher, J.; Masters, J.; Angelini, G.D.; Jeremy, J.Y. Does oxidative stress change ceruloplasmin from a protective to a vasculopathic factor? Atherosclerosis 2006, 187, 238–250. [Google Scholar] [CrossRef]
- Satyanarayana, G.; Keisham, N.; Batra, H.S.; Velamakanni, S.M.; Khan, M.; Gupta, S.; Mahindra, V. Evaluation of Serum Ceruloplasmin Levels as a Biomarker for Oxidative Stress in Patients With Diabetic Retinopathy. Cureus J. Med. Sci. 2021, 13, e13070. [Google Scholar] [CrossRef]






| Variables | T2DM without Sweeteners (D) (n = 93) (Mean ± SD) | T2DM with Sweeteners (DS) (n = 88) (Mean ± SD) | p * Value |
|---|---|---|---|
| WC (cm) | 106.04 ± 7.91 | 105.40 ± 9.83 | NS |
| BMI (Kg/m2) | 31.80 ± 4.49 | 31.65 ± 4.78 | NS |
| Systolic BP (mm Hg) | 136.13 ± 15.18 | 139.93 ± 16.67 | NS |
| Diastolic BP (mm Hg) | 85.32 ± 6.79 | 86.14 ± 7.46 | NS |
| FSG (mg/dL) | 189.91 ± 60.55 | 223.16 ± 80.56 | 0.002 |
| HbA1c (%) | 7.91 ± 1.6 | 8.34 ± 1.71 | NS |
| ALT (IU/L) | 12.53 ± 4.78 | 12.92 ± 4.62 | NS |
| Creatinine (mg/dL) | 0.85 ± 0.19 | 0.84 ± 0.21 | NS |
| Total Cholesterol (mg/dL) | 194.91 ± 53.07 | 185.92 ± 44.51 | NS |
| Triglyceride (mg/dL) | 159.54 ± 63.10 | 172.09 ± 94.60 | NS |
| HDL (mg/dL) | 42.23 ± 11.18 | 41.14 ± 11.59 | NS |
| LDL (mg/dL) | 120.78 ± 45.51 | 109.19 ± 37.55 | NS |
| TC/HDL | 4.80 ± 1.43 | 4.85 ± 1.76 | NS |
| Ceruloplasmin (mg/mL) | 24.23 ± 9.92 | 27.42 ± 9.14 | 0.025 |
| Catalase (kU/L) | 10.26 ± 4.66 | 8.99 ± 2.58 | 0.026 |
| MDA (nmol/mL) | 2.13 ± 0.65 | 2.32 ± 0.54 | 0.033 |
| Peroxynitrite (mmol/L) | 1.81 ± 0.59 | 1.66 ± 0.6 | NS |
| Variables | Healthy without Sweeteners (H) (n = 68) (Mean ± SD) | Healthy with Sweeteners (HS) (n = 14) (Mean ± SD) | p * Value |
|---|---|---|---|
| WC (cm) | 94.66 ± 7.7 | 100 ± 8.74 | NS |
| BMI (Kg/m2) | 26.4 ± 2.53 | 29.18 ± 2.75 | 0.001 |
| Systolic B (mm Hg) | 121.32 ± 8.67 | 123.57 ± 10.82 | NS |
| Diastolic BP (mm Hg) | 79.78 ± 6.32 | 80.71 ± 5.84 | NS |
| FSG (mg/dL) | 89.24 ± 11.95 | 90.71 ± 7.88 | NS |
| HbA1c (%) | 4.80 ± 0.44 | 5.38 ± 0.64 | <0.001 |
| ALT (IU/L) | 12.4 ± 4.3 | 13.94 ± 4.39 | NS |
| Creatinine (mg/dL) | 0.84 ± 0.17 | 0.89 ± 0.14 | NS |
| Total Cholesterol (mg/dL) | 171.90 ± 38.68 | 185.43 ± 21.58 | NS |
| Triglyceride (mg/dL) | 114.09 ± 41.97 | 134.43 ± 60.34 | NS |
| HDL (mg/dL) | 45.71 ± 11.62 | 43.14 ± 8.05 | NS |
| LDL (mg/dL) | 103.37 ± 33.09 | 115.40 ± 17.45 | NS |
| TC/HDL | 3.96 ± 1.23 | 4.40 ± 0.76 | NS |
| Ceruloplasmin (mg/mL) | 22.93 ± 8.01 | 15.86 ± 2.98 | 0.002 |
| Catalase (kU/L) | 13.76 ±5.63 | 8.31 ± 1.72 | 0.001 |
| MDA (nmol/mL) | 1.64 ± 0.63 | 2.56 ± 0.32 | <0.001 |
| Peroxynitrite (mmol/L) | 1.29 ± 0.55 | 1.17 ± 0.431 | NS |
| Variables | H vs. HS | p * Value |
|---|---|---|
| WC (Cm) | 5.64 | 0.049 |
| BMI (Kg/m2) | 10.53 | 0.003 |
| SBP (mm Hg) | 1.85 | NS |
| DBP (mm Hg) | 1.17 | NS |
| FSG (mg/dL) | 1.65 | NS |
| HbA1c (%) | 12.08 | 0.005 |
| ALT (U/L) | 12.42 | NS |
| Creatinine (mg/dL) | 5.95 | NS |
| TC (mg/dL) | 7.87 | NS |
| TG (mg/dL) | 17.83 | NS |
| HDL (mg/dL) | −5.62 | NS |
| LDL (mg/dL) | 11.64 | NS |
| TC/HDL | 11.11 | NS |
| Ceruloplasmin (mg/mL) | −30.83 | <0.001 |
| Catalase (kU/L) | −39.61 | <0.001 |
| MDA (nmol/mL) | 56.10 | <0.001 |
| Peroxynitrite (mmol/L) | −9.30 | NS |
| Variables | Amount of Sweetener Consumption for ≥1 Year in T2DM Patients | p * Value | ||
|---|---|---|---|---|
| <5 Tablets/Day | 5–10 Tablets/Day | >10 Tablets/Day | ||
| (N = 35) | (N = 44) | (N = 9) | ||
| WC ** (cm) | 105.3 ± 9.67 | 105.84 ± 10.1 | 104.67 ± 10.08 | NS |
| BMI ** (Kg/m2) | 31.9 ± 4.72 | 31.59 ± 5.06 | 30.97 ± 3.92 | NS |
| Systolic BP ** (mm Hg) | 137.71 ± 16.73 | 142.39 ± 16.76 | 136.56 ± 16.02 | NS |
| Diastolic BP **(mm Hg) | 85 ± 9.16 | 87.16 ± 6.32 | 85.56 ± 5.27 | NS |
| FSG ** (mg/dL) | 196.97 ± 69.89 | 242.5 ± 86.27 | 230.44 ± 68.53 | 0.041 |
| HbA1c ** (%) | 7.98 ± 1.69 | 8.53 ± 1.66 | 8.85 ± 1.93 | NS |
| ALT ** (IU/L) | 13.6 ± 4.94 | 12.63 ± 4.21 | 11.66 ± 5.36 | NS |
| Creatinine ** (mg/dL) | 0.76 ± 0.19 | 0.9 ± 0.19 | 0.87 ± 0.25 | 0.008 |
| Total Cholesterol ** (mg/dL) | 186.4 ± 4.07 | 189 ± 50.17 | 169 ± 28.61 | NS |
| Triglyceride ** (mg/dL) | 155.77 ± 60.19 | 193.5 ± 116.88 | 130.89 ± 53.88 | NS |
| HDL ** (mg/dL) | 41.86 ± 12.11 | 40.61 ± 11.92 | 40.89 ± 8.36 | NS |
| LDL ** (mg/dL) | 108.66 ± 38.65 | 111.65 ± 38.52 | 99.22 ± 29.33 | NS |
| TC/HDL ** | 4.89 ± 1.96 | 4.92 ± 1.69 | 4.31 ± 1.25 | NS |
| MDA ** (nmol/mL) | 2.46 ± 0.57 | 2.21 ± 0.51 | 2.29 ± 0.51 | NS |
| Ceruloplasmin ** (mg/mL) | 30 ± 5.54 | 26.37 ± 9.28 | 22.52 ± 8.62 | 0.049 |
| Peroxynitrite ** (mmol/L) | 1.74 ± 0.65 | 1.69 ± 0.56 | 1.2 ± 0.41 | 0.052 |
| Catalase ** (kU/L) | 9.66 ± 2.37 | 8.85 ± 2.72 | 6.97 ± 1.30 | 0.015 |
| Variables | Duration of Sweetener Consumption ≥1 Tablet/Day in Diabetic Patients | p * Value | ||
|---|---|---|---|---|
| <5 Years | 5–10 Years | >10 Years | ||
| (N = 49) | (N = 29) | (N = 10) | ||
| WC (cm) | 106.35 ± 10.89 | 103.34 ± 7.9 | 106.7 ± 9.35 | NS |
| BMI (Kg/m2) | 32.42 ± 4.93 | 30.71 ± 4.39 | 30.61 ± 4.9 | NS |
| Systolic BP (mm Hg) | 138.55 ± 16.49 | 140.72 ± 16.27 | 141.5 ± 19.73 | NS |
| Diastolic BP (mm Hg) | 86.94 ± 7.89 | 85.34 ± 6.4 | 84.50 ± 8.32 | NS |
| FSG (mg/dL) | 211.82 ± 81.87 | 228.38 ± 77.54 | 263.6 ± 75.37 | NS |
| HbA1c (%) | 8.07 ± 1.74 | 8.65 ± 1.77 | 8.8 ± 1.19 | NS |
| ALT (IU/L) | 13.55 ± 4.43 | 12.22 ± 5.24 | 11.86 ± 3.32 | NS |
| Creatinine (mg/dL) | 0.84 ± 0.21 | 0.84 ± 0.22 | 0.84 ± 0.16 | NS |
| Total Cholesterol (mg/dL) | 188.2 ± 42.47 | 174.62 ± 47.54 | 207.5 ± 39.29 | NS |
| Triglyceride (mg/dL) | 164.9 ± 77.91 | 158.86 ± 91.42 | 245.7 ± 145.84 | 0.03 |
| HDL (mg/dL) | 40.33 ± 9.39 | 44 ± 14.96 | 36.8 ± 8.95 | NS |
| LDL (mg/dL) | 111.82 ± 35.76 | 97.67 ± 37.83 | 129.72 ± 37.72 | 0.049 |
| TC/HDL | 4.88 ± 1.43 | 4.38 ± 1.95 | 6.05 ± 2.22 | 0.033 |
| MDA (nmole/mL) | 2.37 ± 0.60 | 2.26 ± 0.40 | 2.21 ± 0.59 | NS |
| Ceruloplasmin (mg/mL) | 27.74 ± 9.11 | 28.10 ± 10.10 | 23.87 ± 5.6 | NS |
| Peroxynitrite (mmole/L) | 1.67 ± 0.61 | 1.58 ± 0.59 | 1.86 ± 0.60 | NS |
| Catalase (kU/L) | 9.37 ± 2.51 | 8.52 ± 2.79 | 8.44 ± 2.12 | NS |
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2023 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Hasan, H.M.; Alkass, S.Y.; de Oliveira, D.S.P. Impact of Long-Term Cyclamate and Saccharin Consumption on Biochemical Parameters in Healthy Individuals and Type 2 Diabetes Mellitus Patients. Medicina 2023, 59, 698. https://doi.org/10.3390/medicina59040698
Hasan HM, Alkass SY, de Oliveira DSP. Impact of Long-Term Cyclamate and Saccharin Consumption on Biochemical Parameters in Healthy Individuals and Type 2 Diabetes Mellitus Patients. Medicina. 2023; 59(4):698. https://doi.org/10.3390/medicina59040698
Chicago/Turabian StyleHasan, Husni Mohammed, Suad Yousif Alkass, and Daniele Suzete Persike de Oliveira. 2023. "Impact of Long-Term Cyclamate and Saccharin Consumption on Biochemical Parameters in Healthy Individuals and Type 2 Diabetes Mellitus Patients" Medicina 59, no. 4: 698. https://doi.org/10.3390/medicina59040698
APA StyleHasan, H. M., Alkass, S. Y., & de Oliveira, D. S. P. (2023). Impact of Long-Term Cyclamate and Saccharin Consumption on Biochemical Parameters in Healthy Individuals and Type 2 Diabetes Mellitus Patients. Medicina, 59(4), 698. https://doi.org/10.3390/medicina59040698






