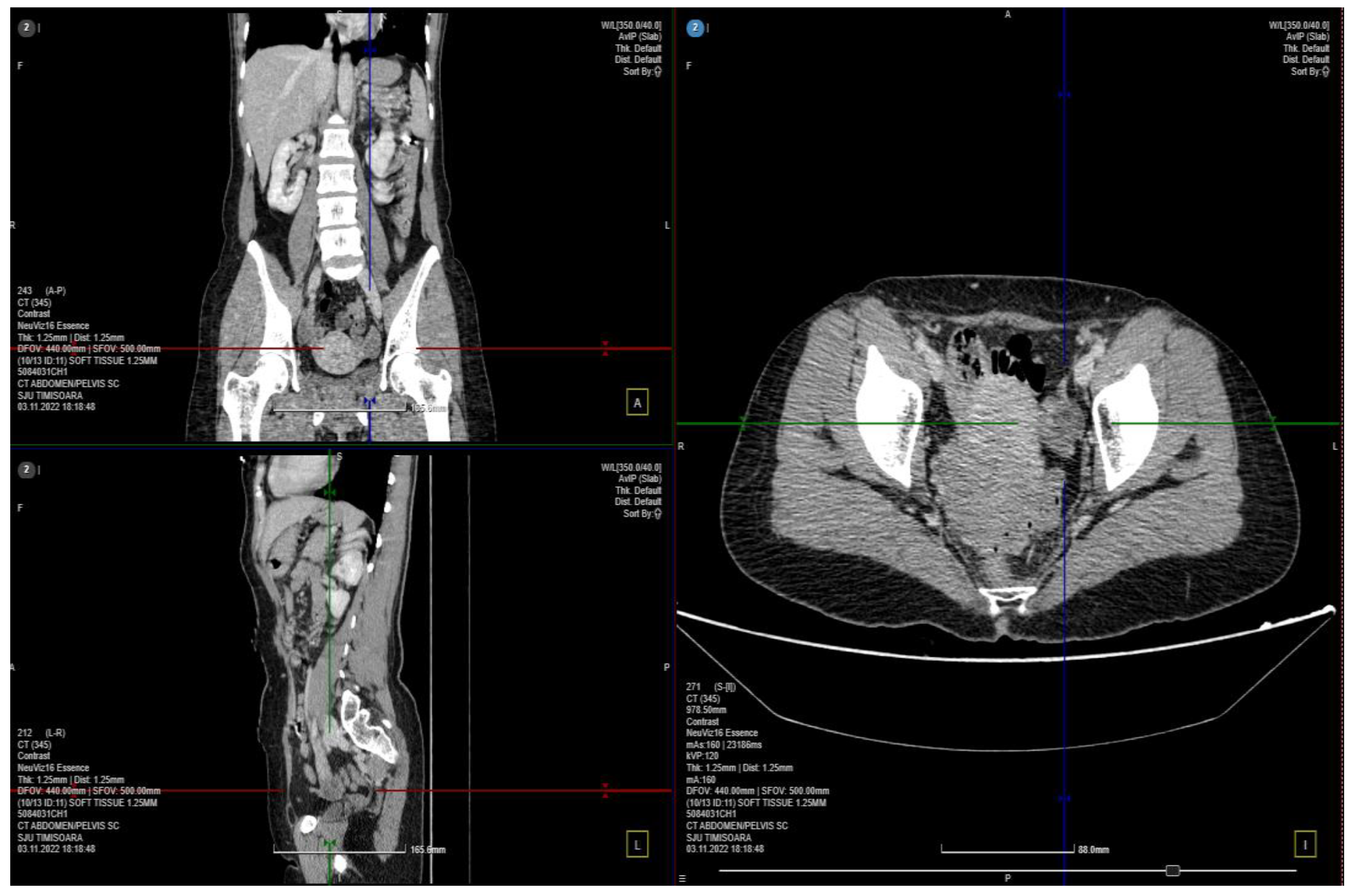
Female Gonadal Venous Insufficiency in a Clinical Presentation Which Suggested an Acute Abdomen—A Case Report and Literature Review
Abstract
:1. Introduction
2. Materials and Methods
3. Discussion
4. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Acknowledgments
Conflicts of Interest
References
- Gasparini, D.; Geatti, O.; Orsolon, P.G.; Shapiro, B. Female “varicocele”: Two cases diagnosed by labeled red blood cell angioscintigraphy and treated by percutaneous phlebography and embolization. Clin. Nucl. Med. 1998, 23, 420–422. [Google Scholar]
- Hobbs, J.T. Varicose veins arising from the pelvis due to ovarian vein incompetence. Int. J. Clin. Pract. 2005, 59, 1195–1203. [Google Scholar]
- Van der Plas, L.G.; van Vliet, A.; Bousema, M.T.; Sanders, C.J.; Mali, W.P. Women with pelvic complaints and atypical varicose veins, varicose veins of the vulva and insufficiency of the pelvic veins; treatment with embolisation. Ned. Tijdschr. Geneeskd. 2005, 149, 557–560. [Google Scholar]
- Meissner, M.H.; Khilnani, N.M.; Labropoulos, N.; Gasparis, A.P.; Gibson, K.; Greiner, M.; Learman, L.A.; Atashroo, D.; Lurie, F.; Passman, M.A.; et al. The Symptoms-Varices-Pathophysiology classification of pelvic venous disorders: A report of the American Vein & Lymphatic Society International Working Group on Pelvic Venous Disorders. Phlebology 2021, 36, 342–360. [Google Scholar]
- Nagib, S.; Fakhry, A. Pelvic congestion syndrome. In Yearbook of Vascular and Endovascular Surgery—3; Jaypee Brothers Medical Publishers (P) Ltd.: New Delhi, India, 2021; pp. 54–65. [Google Scholar]
- Joh, M.; Grewal, S.; Gupta, R. Ovarian Vein Embolization: How and When Should It Be Done? Tech. Vasc. Interv. Radiol. 2021, 24, 100732. [Google Scholar]
- Jambon, E.; Le Bras, Y.; Coussy, A.; Petitpierre, F.; Hans, H.; Lasserre, A.; Cazalas, G.; Grenier, N.; Marcelin, C. Embolization in pelvic venous disorders using ethylene vinyl alcohol copolymer (Onyx®) and Aetoxysclerol: A prospective evaluation of safety and long-term efficacy. Eur. Radiol. 2022, 32, 4679–4686. [Google Scholar]
- Marcelin, C.; Le Bras, Y.; Molina Andreo, I.; Jambon, E.; Grenier, N. Diagnosis and Management of Pelvic Venous Disorders in Females. Diagnostics 2022, 12, 2337. [Google Scholar] [CrossRef]
- Kim, H.S.; Malhotra, A.D.; Rowe, P.C.; Lee, J.M.; Venbrux, A.C. Embolotherapy for pelvic congestion syndrome: Long-term results. J. Vasc. Interv. Radiol. 2006, 17 Pt 1, 289–297. [Google Scholar]
- Meissner, M.H.; Gibson, K. Clinical outcome after treatment of pelvic congestion syndrome: Sense and nonsense. Phlebology 2015, 30 (Suppl. S1), 73–80. [Google Scholar]
- Asciutto, G.; Asciutto, K.C.; Mumme, A.; Geier, B. Pelvic venous incompetence: Reflux patterns and treatment results. Eur. J. Vasc. Endovasc. Surg. 2009, 38, 381–386. [Google Scholar]
- Lakhanpal, G.; Kennedy, R.; Lakhanpal, S.; Sulakvelidze, L.; Pappas, P.J. Pelvic venous insufficiency secondary to iliac vein stenosis and ovarian vein reflux treated with iliac vein stenting alone. J. Vasc. Surg. Venous Lymphat. Disord. 2021, 9, 1193–1198. [Google Scholar]
- Koo, S.; Fan, C.M. Pelvic congestion syndrome and pelvic varicosities. Tech. Vasc. Interv. Radiol. 2014, 17, 90–95. [Google Scholar]
- Daniels, J.; Gray, R.; Hills, R.K.; Latthe, P.; Buckley, L.; Gupta, J.; Selman, T.; Adey, E.; Xiong, T.; Champaneria, R.; et al. Laparoscopic uterosacral nerve ablation for alleviating chronic pelvic pain: A randomized controlled trial. JAMA 2009, 302, 955–961. [Google Scholar]
- Eken, A.; Akbas, T.; Arpaci, T. Spontaneous rupture of the ureter. Singap. Med. J. 2015, 56, e29–e31. [Google Scholar]
- Oray, D.; Limon, O.; Ertan, C.; Ugurhan, A. Spontaneous Bladder Rupture and Pelvic Fracture Due To Bladder Cancer. Turk. J. Emerg. Med. 2016, 14, 139–141. [Google Scholar]
- Riding, D.M.; Hansrani, V.; McCollum, C. Pelvic vein incompetence: Clinical perspectives. Vasc. Health Risk Manag. 2017, 13, 439–447. [Google Scholar]
- Hansrani, V.; Dhorat, Z.; McCollum, C.N. Diagnosing of pelvic vein incompetence using minimally invasive ultrasound techniques. Vascular 2017, 25, 253–259. [Google Scholar]
- Sozutok, S.; Piskin, F.C.; Balli, H.T.; Onan, H.B.; Kaya, O.; Aksungur, E.H. Efficacy of the endovascular ovarian vein embolization technique in pelvic venous congestion syndrome. Pol. J. Radiol. 2002, 87, e510–e515. [Google Scholar]
- Mahmoud, O.; Vikatmaa, P.; Aho, P.; Halmesmäki, K.; Albäck, A.; Rahkola-Soisalo, P.; Lappalainen, K.; Venermo, M. Efficacy of endovascular treatment for pelvic congestion syndrome. J. Vasc. Surg. Venous Lymphat. Disord. 2016, 4, 355–370. [Google Scholar]
- Gloviczki, P.; Comerota, A.J.; Dalsing, M.C.; Eklof, B.G.; Gillespie, D.L.; Gloviczki, M.L.; Lohr, J.M.; McLafferty, R.B.; Meissner, M.H.; Murad, M.H.; et al. Society for Vascular Surgery; American Venous Forum. The care of patients with varicose veins and associated chronic venous diseases: Clinical practice guidelines of the Society for Vascular Surgery and the American Venous Forum. J. Vasc. Surg. 2011, 53 (Suppl. S5), 2S–48S. [Google Scholar]
- Lopez, A.J. Female Pelvic Vein Embolization: Indications, Techniques, and Outcomes. Cardiovasc. Interv. Radiol. 2015, 38, 806–820. [Google Scholar]
- Edwards, R.D.; Robertson, I.R.; MacLean, A.B.; Hemingway, A.P. Case report: Pelvic pain syndrome—Successful treatment of a case by ovarian vein embolization. Clin. Radiol. 1993, 47, 429–431. [Google Scholar]
- Venbrux, A.C.; Chang, A.H.; Kim, H.S.; Montague, B.J.; Hebert, J.B.; Arepally, A.; Rowe, P.C.; Barron, D.F.; Lambert, D.; Robinson, J.C. Pelvic congestion syndrome (pelvic venous incompetence): Impact of ovarian and internal iliac vein embolotherapy on menstrual cycle and chronic pelvic pain. J. Vasc. Interv. Radiol. 2002, 13 Pt 1, 171–178. [Google Scholar]
- LaVasseur, C.; Neukam, S.; Kartika, T.; Samuelson Bannow, B.; Shatzel, J.; DeLoughery, T.G. Hormonal therapies and venous thrombosis: Considerations for prevention and management. Res. Pract. Thromb. Haemost. 2022, 6, e12763. [Google Scholar]
- Rosendaal, F.R.; Van Hylckama Vlieg, A.; Tanis, B.C.; Helmerhorst, F.M. Estrogens, progestogens and thrombosis. J. Thromb. Haemost. 2003, 1, 1371–1380. [Google Scholar]
- Labropoulos, N.; Shifrin, D.A.; Kandarpa, K. Effectiveness of micronized purified flavonoid fraction (Daflon) for the treatment of pelvic pain related to chronic pelvic venous incompetence: A double-blind, placebo-controlled study. Vasc. Endovasc. Surg. 2005, 39, 441–447. [Google Scholar]
- Bellelis, P.; Barboza, F.R.; Castro, R.A.; Dias, M.M.; Ribeiro, I.L.; Zugaib, M. Oral diosmin and hesperidin in the management of chronic venous insufficiency and hemorrhoidal disease: Results of a randomized, double-blind, placebo-controlled trial. Phlebology 2019, 34, 101–109. [Google Scholar]
- Steinbruch, M.; Nunes, C.; Gama, R.; Kaufman, R.; Gama, G.; Suchmacher, N.M.; Nigri, R.; Cytrynbaum, N.; Brauer, O.L.; Bertaina, I.; et al. Is NonmicronizedDiosmin 600 mg as Effective as Micronized Diosmin 900 mg plus Hesperidin 100 mg on Chronic Venous Disease Symptoms? Results of a Noninferiority Study. Int. J. Vasc. Med. 2020, 2020, 4237204. [Google Scholar]
- Cazaubon, M.; Benigni, J.P.; Steinbruch, M.; Jabbour, V.; Gouhier-Kodas, C. Is There a Difference in the Clinical Efficacy of Diosmin and Micronized Purified Flavonoid Fraction for the Treatment of Chronic Venous Disorders? Review of Available Evidence. Vasc. Health Risk Manag. 2021, 17, 591–600. [Google Scholar]
- Romanenko, T.G.; Sulimenko, O.M. Prevention of preeclampsia in women with multiple pregnancy after assisted reproduction. Wiad. Lek. 2020, 73, 494–497. [Google Scholar]
- Macher, J.; Brahmbhatt, A.; Shetty, A.; Chughtai, K.; Baran, T.; Baah, N.O.; Dogra, V. Predicting pelvic congestion syndrome: Concomitant pelvic pain diagnoses do not affect venography or embolization outcomes. J. Clin. Imaging Sci. 2021, 11, 61. [Google Scholar]
- Bałabuszek, K.; Toborek, M.; Pietura, R. Comprehensive overview of the venous disorder known as pelvic congestion syndrome. Ann. Med. 2022, 54, 22–36. [Google Scholar]
- Ueno, S.; Obara, H.; Ito, H. Pelvic congestion syndrome: Its diagnosis and treatment. Prog. Med. 2012, 32, 1681–1687. [Google Scholar]
- Bittles, M.A.; Hoffer, E.K. Gonadal vein embolization: Treatment of varicocele and pelvic congestion syndrome. Semin. Interv. Radiol. 2008, 25, 261–270. [Google Scholar]
- Liddle, A.D.; Davies, A.H. Pelvic congestion syndrome: Chronic pelvic pain caused by ovarian and internal iliac varices. Phlebology 2007, 22, 100–104. [Google Scholar]
- Brown, C.L.; Rizer, M.; Alexander, R.; Sharpe, E.E., III; Rochon, P.J. Pelvic Congestion Syndrome: Systematic Review of Treatment Success. Semin. Interv. Radiol. 2018, 35, 35–40. [Google Scholar]




Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2023 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Matei, S.-C.; Dumitru, C.Ș.; Oprițoiu, A.-I.; Marian, L.; Murariu, M.-S.; Olariu, S. Female Gonadal Venous Insufficiency in a Clinical Presentation Which Suggested an Acute Abdomen—A Case Report and Literature Review. Medicina 2023, 59, 884. https://doi.org/10.3390/medicina59050884
Matei S-C, Dumitru CȘ, Oprițoiu A-I, Marian L, Murariu M-S, Olariu S. Female Gonadal Venous Insufficiency in a Clinical Presentation Which Suggested an Acute Abdomen—A Case Report and Literature Review. Medicina. 2023; 59(5):884. https://doi.org/10.3390/medicina59050884
Chicago/Turabian StyleMatei, Sergiu-Ciprian, Cristina Ștefania Dumitru, Andrei-Ion Oprițoiu, Lucian Marian, Marius-Sorin Murariu, and Sorin Olariu. 2023. "Female Gonadal Venous Insufficiency in a Clinical Presentation Which Suggested an Acute Abdomen—A Case Report and Literature Review" Medicina 59, no. 5: 884. https://doi.org/10.3390/medicina59050884
APA StyleMatei, S.-C., Dumitru, C. Ș., Oprițoiu, A.-I., Marian, L., Murariu, M.-S., & Olariu, S. (2023). Female Gonadal Venous Insufficiency in a Clinical Presentation Which Suggested an Acute Abdomen—A Case Report and Literature Review. Medicina, 59(5), 884. https://doi.org/10.3390/medicina59050884





