Depression in Heart Failure with Reduced Ejection Fraction, an Undervalued Comorbidity: An Up-To-Date Review
Abstract
:1. Introduction
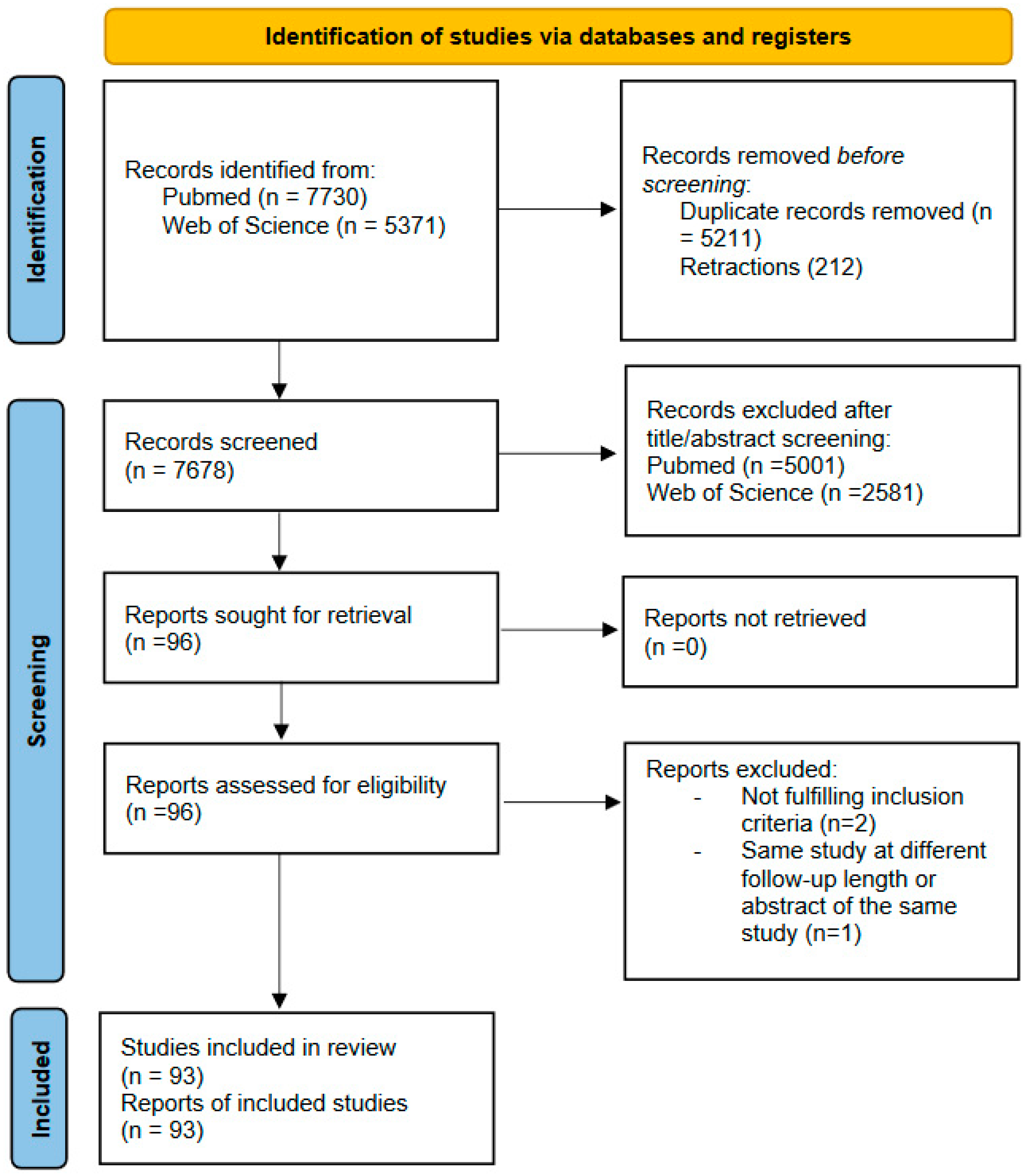
2. Materials and Methods
2.1. Study Design
2.2. Search Strategy
2.3. Study Selection
3. Results
3.1. Epidemiology
3.2. Depression in Heart Failure
3.3. Influence on Cardiovascular Outcomes of Concomitant HF and Depression
3.4. Mechanism of Comorbid Depression and HF
3.5. Depression and Heart Disease in Patients with No Previous Cardiac Diseases
3.6. Diagnosis
3.7. Treatment
3.7.1. Non-Pharmacological Therapy
3.7.2. Pharmacological Therapy
3.7.3. Integrated Care Models in the Management of Depression in Patients with Heart Disease
3.7.4. New Therapies
4. Discussion
5. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Conflicts of Interest
References
- Gilman, S.E.; Sucha, E.; Kingsbury, M.; Horton, N.J.; Murphy, J.M.; Colman, I. Depression and mortality in a longitudinal study: 1952–2011. Can. Med. Assoc. J. 2017, 189, E1304–E1310. [Google Scholar] [CrossRef] [PubMed]
- Mura, F.; Patron, E.; Messerotti Benvenuti, S.; Gentili, C.; Ponchia, A.; Palomba, D. The Influence of Emotion Regulation on the Association Between Depression and Heart Rate Variability in Cardiac Patients. Psychosom. Med. 2022, 84, 702–710. [Google Scholar] [CrossRef] [PubMed]
- Malzberg, B. Mortality among patients with involution melancholia. Am. J. Psychiatry 1937, 93, 1231–1238. [Google Scholar] [CrossRef]
- Koenig, H.G. Depression in hospitalized older patients with congestive heart failure. Gen. Hosp. Psychiatry 1998, 20, 29–43. [Google Scholar] [CrossRef]
- McDonagh, T.A.; Metra, M.; Adamo, M.; Gardner, R.S.; Baumbach, A.; Böhm, M.; Burri, H.; Butler, J.; Čelutkienė, J.; Chioncel, O.; et al. 2021 ESC Guidelines for the diagnosis and treatment of acute and chronic heart failure. Eur. Heart J. 2021, 42, 3599–3726. [Google Scholar] [CrossRef]
- Heidenreich, P.A.; Bozkurt, B.; Aguilar, D.; Allen, L.A.; Byun, J.J.; Colvin, M.M.; Deswal, A.; Drazner, M.H.; Dunlay, S.M.; Evers, L.R.; et al. 2022 AHA/ACC/HFSA Guideline for the Management of Heart Failure: Executive Summary: A Report of the American College of Cardiology/American Heart Association Joint Committee on Clinical Practice Guidelines. J. Am. Coll. Cardiol. 2022, 79, 1757–1780. [Google Scholar] [CrossRef]
- Rustad, J.K.; Stern, T.A.; Hebert, K.A.; Musselman, D.L. Diagnosis and treatment of depression in patients with congestive heart failure: A review of the literature. Prim. Care Companion CNS Disord. 2013, 15, 26254. [Google Scholar] [CrossRef]
- Walrave, R.; Beerten, S.G.; Mamouris, P.; Coteur, K.; Van Nuland, M.; Van Pottelbergh, G.; Casas, L.; Vaes, B. Trends in the epidemiology of depression and comorbidities from 2000 to 2019 in Belgium. BMC Prim. Care 2022, 23, 163. [Google Scholar] [CrossRef]
- Husaini, B.A.; Taira, D.; Norris, K.; Adhish, S.V.; Moonis, M.; Levine, R. Depression Effects on Hospital Cost of Heart Failure Patients in California: An Analysis by Ethnicity and Gender. Indian J. Community Med. 2018, 43, 49–52. [Google Scholar] [CrossRef]
- Sullivan, M.; Simon, G.; Spertus, J.; Russo, J. Depression-related costs in heart failure care. Arch. Intern. Med. 2002, 162, 1860–1866. [Google Scholar] [CrossRef]
- Salk, R.H.; Hyde, J.S.; Abramson, L.Y. Gender differences in depression in representative national samples: Meta-analyses of diagnoses and symptoms. Psychol. Bull. 2017, 143, 783–822. [Google Scholar] [CrossRef] [PubMed]
- Sutin, A.R.; Terracciano, A.; Milaneschi, Y.; An, Y.; Ferrucci, L.; Zonderman, A.B. The trajectory of depressive symptoms across the adult life span. JAMA Psychiatry 2013, 70, 803–811. [Google Scholar] [CrossRef] [PubMed]
- Harshfield, E.L.; Pennells, L.; Schwartz, J.E.; Willeit, P.; Kaptoge, S.; Bell, S.; Shaffer, J.A.; Bolton, T.; Spackman, S.; Wassertheil-Smoller, S.; et al. Association Between Depressive Symptoms and Incident Cardiovascular Diseases. JAMA 2020, 324, 2396–2405. [Google Scholar] [CrossRef]
- Gathright, E.C.; Goldstein, C.M.; Josephson, R.A.; Hughes, J.W. Depression increases the risk of mortality in patients with heart failure: A meta-analysis. J. Psychosom. Res. 2017, 94, 82–89. [Google Scholar] [CrossRef] [PubMed]
- Rutledge, T.; Reis, V.A.; Linke, S.E.; Greenberg, B.H.; Mills, P.J. Depression in heart failure. J. Am. Coll. Cardiol. 2006, 48, 1527–1537. [Google Scholar] [CrossRef]
- Sokoreli, I.; de Vries, J.J.; Pauws, S.C.; Steyerberg, E.W. Depression and anxiety as predictors of mortality among heart failure patients: Systematic review and meta-analysis. Heart Fail. Rev. 2016, 21, 49–63. [Google Scholar] [CrossRef]
- Freedland, K.E.; Rich, M.W.; Skala, J.A.; Carney, R.M.; Dávila-Román, V.G.; Jaffe, A.S. Prevalence of depression in hospitalized patients with congestive heart failure. Psychosom. Med. 2003, 65, 119–128. [Google Scholar] [CrossRef]
- Jiang, W.; Alexander, J.; Christopher, E.; Kuchibhatla, M.; Gaulden, L.H.; Cuffe, M.S.; Blazing, M.A.; Davenport, C.; Califf, R.M.; Krishnan, R.R.; et al. Relationship of depression to increased risk of mortality and rehospitalization in patients with congestive heart failure. Arch. Intern. Med. 2001, 161, 1849–1856. [Google Scholar] [CrossRef]
- Daskalopoulou, M.; George, J.; Walters, K.; Osborn, D.P.; Batty, G.D.; Stogiannis, D.; Rapsomaniki, E.; Pujades-Rodriguez, M.; Denaxas, S.; Udumyan, R.; et al. Depression as a Risk Factor for the Initial Presentation of Twelve Cardiac, Cerebrovascular, and Peripheral Arterial Diseases: Data Linkage Study of 1.9 Million Women and Men. PLoS ONE 2016, 11, e0153838. [Google Scholar] [CrossRef]
- White, J.R.; Chang, C.C.; So-Armah, K.A.; Stewart, J.C.; Gupta, S.K.; Butt, A.A.; Gibert, C.L.; Rimland, D.; Rodriguez-Barradas, M.C.; Leaf, D.A.; et al. Depression and human immunodeficiency virus infection are risk factors for incident heart failure among veterans: Veterans Aging Cohort Study. Circulation 2015, 132, 1630–1638. [Google Scholar] [CrossRef]
- Frasure-Smith, N.; Lespérance, F.; Habra, M.; Talajic, M.; Khairy, P.; Dorian, P.; Roy, D. Elevated depression symptoms predict long-term cardiovascular mortality in patients with atrial fibrillation and heart failure. Circulation 2009, 120, 134–140. [Google Scholar] [CrossRef] [PubMed]
- Friedmann, E.; Thomas, S.A.; Liu, F.; Morton, P.G.; Chapa, D.; Gottlieb, S.S.; Sudden Cardiac Death in Heart Failure Trial Investigators. Relationship of depression, anxiety, and social isolation to chronic heart failure outpatient mortality. Am. Heart J. 2006, 152, e1–e940. [Google Scholar] [CrossRef] [PubMed]
- Sancassiani, F.; Carta, M.G.; Montisci, R.; Preti, A.; Machado, S.; Moro, M.F.; Marchetti, M.F.; Meloni, L. Takotsubo Syndrome is Associated with Mood Disorders and Antidepressants Use, not with Anxiety and Impairment of Quality of Life Due to the Psychiatric Disorder. Clin. Pract. Epidemiol. Ment. Health 2018, 14, 26–32. [Google Scholar] [CrossRef]
- Bürker, B.S.; Gullestad, L.; Gude, E.; Havik, O.E.; Relbo Authen, A.; Grov, I.; Andreassen, A.K.; Fiane, A.E.; Haraldsen, I.R.; Dew, M.A. The Predictive Value of Depression in the Years After Heart Transplantation for Mortality During Long-Term Follow-Up. Psychosom. Med. 2019, 81, 513–520. [Google Scholar] [CrossRef]
- Liu, C.H.; Wang, J.H.; Weng, S.C.; Cheng, Y.H.; Yeh, M.K.; Bai, M.Y.; Chang, J.C. Is heart failure associated with risk of suicide? J. Card. Fail. 2018, 24, 795–800. [Google Scholar] [CrossRef]
- Cai, H.; Xie, X.M.; Zhang, Q.; Cui, X.; Lin, J.X.; Sim, K.; Ungvari, G.S.; Zhang, L.; Xiang, Y.T. Prevalence of Suicidality in Major Depressive Disorder: A Systematic Review and Meta-Analysis of Comparative Studies. Front. Psychiatry 2021, 12, 690130. [Google Scholar] [CrossRef] [PubMed]
- Korkmaz, H.; Korkmaz, S.; Çakar, M. Suicide risk in chronic heart failure patients and its association with depression, hopelessness and self esteem. J. Clin. Neurosci. 2019, 68, 51–54. [Google Scholar] [CrossRef]
- Moraska, A.R.; Chamberlain, A.M.; Shah, N.D.; Vickers, K.S.; Rummans, T.A.; Dunlay, S.M.; Spertus, J.A.; Weston, S.A.; McNallan, S.M.; Redfield, M.M.; et al. Depression, healthcare utilization, and death in heart failure: A community study. Circ. Heart Fail. 2013, 6, 387–394. [Google Scholar] [CrossRef]
- de Miranda Azevedo, R.; Roest, A.M.; Hoen, P.W.; de Jonge, P. Cognitive/affective and somatic/affective symptoms of depression in patients with heart disease and their association with cardiovascular prognosis: A meta-analysis. Psychol. Med. 2014, 44, 2689–2703. [Google Scholar] [CrossRef]
- Dekker, R.L.; Lennie, T.A.; Albert, N.M.; Rayens, M.K.; Chung, M.L.; Wu, J.R.; Song, E.K.; Moser, D.K. Depressive symptom trajectory predicts 1-year health-related quality of life in patients with heart failure. J. Card. Fail. 2011, 17, 755–763. [Google Scholar] [CrossRef]
- Sbolli, M.; Fiuzat, M.; Cani, D.; O’Connor, C.M. Depression and heart failure: The lonely comorbidity. Eur. J. Heart Fail. 2020, 22, 2007–2017. [Google Scholar] [CrossRef]
- Khawaja, I.S.; Westermeyer, J.J.; Gajwani, P.; Feinstein, R.E. Depression and coronary artery disease: The association, mechanisms, and therapeutic implications. Psychiatry 2009, 6, 38–51. [Google Scholar] [PubMed]
- Morel-Kopp, M.C.; McLean, L.; Chen, Q.; Tofler, G.H.; Tennant, C.; Maddison, V.; Ward, C.M. The association of depression with platelet activation: Evidence for a treatment effect. J. Thromb. Haemost. 2009, 7, 573–581. [Google Scholar] [CrossRef] [PubMed]
- Markovitz, J.H.; Shuster, J.L.; Chitwood, W.S.; May, R.S.; Tolbert, L.C. Platelet activation in depression and effects of sertraline treatment: An open-label study. Am. J. Psychiatry 2000, 157, 1006–1008. [Google Scholar] [CrossRef]
- Gehi, A.; Musselman, D.; Otte, C.; Bruce Royster, E.; Ali, S.; Whooley, M.A. Depression and platelet activation in outpatients with stable coronary heart disease: Findings from the Heart and Soul Study. Psychiatry Res. 2010, 175, 200–204. [Google Scholar] [CrossRef] [PubMed]
- Stein, P.K.; Carney, R.M.; Freedland, K.E.; Skala, J.A.; Jaffe, A.S.; Kleiger, R.E.; Rottman, J.N. Severe depression is associated with markedly reduced heart rate variability in patients with stable coronary heart disease. J. Psychosom. Res. 2000, 48, 493–500. [Google Scholar] [CrossRef]
- Frenneaux, M.P. Autonomic changes in patients with heart failure and in post-myocardial infarction patients. Heart 2004, 90, 1248–1255. [Google Scholar] [CrossRef]
- Francis, J.L.; Weinstein, A.A.; Krantz, D.S.; Haigney, M.C.; Stein, P.K.; Stone, P.H.; Gottdiener, J.S.; Kop, W.J. Association between symptoms of depression and anxiety with heart rate variability in patients with implantable cardioverter defibrillators. Psychosom. Med. 2009, 71, 821–827. [Google Scholar] [CrossRef]
- Ambade, V.; Arora, M.M.; Singh, P.; Somani, B.L.; Basannar, D. Adrenaline, Noradrenaline and Dopamine Level Estimation in Depression: Does it Help? Med. J. Armed Forces India 2009, 65, 216–220. [Google Scholar] [CrossRef]
- Hoppmann, U.; Engler, H.; Krause, S.; Rottler, E.; Hoech, J.; Szabo, F.; Radermacher, P.; Waller, C. Systemic Catecholaminergic Deficiency in Depressed Patients with and without Coronary Artery Disease. J. Clin. Med. 2021, 10, 986. [Google Scholar] [CrossRef]
- Redwine, L.S.; Wirtz, P.H.; Hong, S.; Bosch, J.A.; Ziegler, M.G.; Greenberg, B.; Mills, P.J. Depression as a potential modulator of Beta-adrenergic-associated leukocyte mobilization in heart failure patients. J. Am. Coll. Cardiol. 2010, 56, 1720–1727. [Google Scholar] [CrossRef] [PubMed]
- Luukinen, H.; Laippala, P.; Huikuri, H.V. Depressive symptoms and the risk of sudden cardiac death among the elderly. Eur. Heart J. 2003, 24, 2021–2026. [Google Scholar] [CrossRef] [PubMed]
- Wha Whang, W.; Albert, C.M.; Sears, S.F., Jr.; Lampert, R.; Conti, J.B.; Wang, P.J.; Singh, J.P.; Ruskin, J.N.; Muller, J.E.; Mittleman, M.A. Depression as a predictor for appropriate shocks among patients with implantable cardioverter-defibrillators: Results from the Triggers of Ventricular Arrhythmias (TOVA) study. J. Am. Coll. Cardiol. 2005, 45, 1090–1095. [Google Scholar] [CrossRef]
- Walter, F.A.; Gathright, E.; Redle, J.D.; Gunstad, J.; Hughes, J.W. Depressive Symptoms are Associated with Heart Rate Variability Independently of Fitness: A Cross-Sectional Study of Patients with Heart Failure. Ann. Behav. Med. 2019, 53, 955–963. [Google Scholar] [CrossRef]
- Fischer, D.; Rossa, S.; Landmesser, U.; Spiekermann, S.; Engberding, N.; Hornig, B.; Drexler, H. Endothelial dysfunction in patients with chronic heart failure is independently associated with increased incidence of hospitalization, cardiac transplantation, or death. Eur. Heart J. 2005, 26, 65–69. [Google Scholar] [CrossRef] [PubMed]
- Osto, E.; Tona, F.; Angelini, A.; Montisci, R.; Ruscazio, M.; Vinci, A.; Tarantini, G.; Ramondo, A.; Gambino, A.; Thiene, G.; et al. Determinants of coronary flow reserve in heart transplantation: A study performed with contrast-enhanced echocardiography. J. Heart Lung Transplant. 2009, 28, 453–460. [Google Scholar] [CrossRef]
- Do, D.P.; Dowd, J.B.; Ranjit, N.; House, J.S.; Kaplan, G.A. Hopelessness, depression, and early markers of endothelial dysfunction in, U.S. adults. Psychosom. Med. 2010, 72, 613–619. [Google Scholar] [CrossRef] [PubMed]
- Mommersteeg, P.M.; Schoemaker, R.G.; Eisel, U.L.; Garrelds, I.M.; Schalkwijk, C.G.; Kop, W.J. Nitric oxide dysregulation in patients with heart failure: The association of depressive symptoms with L-arginine, asymmetric dimethylarginine, symmetric dimethylarginine, and isoprostane. Psychosom. Med. 2015, 77, 292–302. [Google Scholar] [CrossRef]
- Sherwood, A.; Hinderliter, A.L.; Watkins, L.L.; Waugh, R.A.; Blumenthal, J.A. Impaired endothelial function in coronary heart disease patients with depressive symptomatology. J. Am. Coll. Cardiol. 2005, 46, 656–659. [Google Scholar] [CrossRef]
- Halaris, A. Inflammation, heart disease, and depression. Curr. Psychiatry. Rep. 2013, 15, 400. [Google Scholar] [CrossRef]
- Gimeno, D.; Kivimäki, M.; Brunner, E.J.; Elovainio, M.; De Vogli, R.; Steptoe, A.; Kumari, M.; Lowe, G.D.; Rumley, A.; Marmot, M.G.; et al. Associations of C-reactive protein and interleukin-6 with cognitive symptoms of depression: 12-year follow-up of the Whitehall II study. Psychol. Med. 2009, 39, 413–423. [Google Scholar] [CrossRef] [PubMed]
- Xiong, G.L.; Prybol, K.; Boyle, S.H.; Hall, R.; Streilein, R.D.; Steffens, D.C.; Krishnan, R.; Rogers, J.G.; O’Connor, C.M.; Jiang, W. Inflammation Markers and Major Depressive Disorder in Patients with Chronic Heart Failure: Results from the Sertraline Against Depression and Heart Disease in Chronic Heart Failure Study. Psychosom. Med. 2015, 77, 808–815. [Google Scholar] [CrossRef]
- Liang, Y.Y.; Chen, Y.; Feng, H.; Liu, X.; Ai, Q.H.; Xue, H.; Shu, X.; Weng, F.; He, Z.; Ma, J.; et al. Association of Social Isolation and Loneliness with Incident Heart Failure in a Population-Based Cohort Study. JACC Heart Fail. 2023, 11, 334–344. [Google Scholar] [CrossRef]
- Montisci, R.; Cecchetto, G.; Ruscazio, M.; Snenghi, R.; Portale, A.; Viel, G.; Nalesso, A.; Paoli, A.; Iliceto, S.; Meloni, L.; et al. Early myocardial dysfunction after chronic use of anabolic androgenic steroids: Combined pulsed-wave tissue Doppler imaging and ultrasonic integrated backscatter cyclic variations analysis. J. Am. Soc. Echocardiogr. 2010, 23, 516–522. [Google Scholar] [CrossRef]
- Luharty, M.; Taylor, A.E.; Grabski, M.; Munafò, M.R. The Association of Cigarette Smoking with Depression and Anxiety: A Systematic Review. Nicotine Tob. Res. 2017, 19, 3–13. [Google Scholar] [CrossRef]
- Brouwers, C.; Christensen, S.B.; Damen, N.L.; Denollet, J.; Torp-Pedersen, C.; Gislason, G.H.; Pedersen, S.S. Antidepressant use and risk for mortality in 121,252 heart failure patients with or without a diagnosis of clinical depression. Int. J. Cardiol. 2016, 203, 867–873. [Google Scholar] [CrossRef] [PubMed]
- Wu, J.R.; Lennie, T.A.; Dekker, R.L.; Biddle, M.J.; Moser, D.K. Medication adherence, depressive symptoms, and cardiac event-free survival in patients with heart failure. J. Card. Fail. 2013, 19, 317–324. [Google Scholar] [CrossRef] [PubMed]
- Conraads, V.M.; Deaton, C.; Piotrowicz, E.; Santaularia, N.; Tierney, S.; Piepoli, M.F.; Pieske, B.; Schmid, J.P.; Dickstein, K.; Ponikowski, P.P.; et al. Adherence of heart failure patients to exercise: Barriers and possible solutions: A position statement of the Study Group on Exercise Training in Heart Failure of the Heart Failure Association of the European Society of Cardiology. Eur. J. Heart. Fail. 2012, 14, 451–458. [Google Scholar] [CrossRef] [PubMed]
- Rock, P.L.; Roiser, J.P.; Riedel, W.J.; Blackwell, A.D. Cognitive impairment in depression: A systematic review and meta-analysis. Psychol. Med. 2014, 44, 2029–2040. [Google Scholar] [CrossRef]
- Vogels, R.L.; Scheltens, P.; Schroeder-Tanka, J.M.; Weinstein, H.C. Cognitive impairment in heart failure: A systematic review of the literature. Eur. J. Heart. Fail. 2007, 9, 440–449. [Google Scholar] [CrossRef]
- Frey, A.; Sell, R.; Homola, G.A.; Malsch, C.; Kraft, P.; Gunreben, I.; Morbach, C.; Alkonyi, B.; Schmid, E.; Colonna, I.; et al. Cognitive Deficits and Related Brain Lesions in Patients with Chronic Heart Failure. JACC Heart Fail. 2018, 6, 583–592. [Google Scholar] [CrossRef] [PubMed]
- Maurer, D.M.; Raymond, T.J.; Davis, B.N. Depression: Screening and Diagnosis. Am. Fam. Physician 2018, 98, 508–515. [Google Scholar] [PubMed]
- Ceccarini, M.; Manzoni, G.M.; Castelnuovo, G. Assessing depression in cardiac patients: What measures should be considered? Depress Res. Treat. 2014, 2014, 148256. [Google Scholar] [CrossRef]
- Nicholson, A.; Kuper, H.; Hemingway, H. Depression as an aetiologic and prognostic factor in coronary heart disease: A meta-analysis of 6362 events among 146,538 participants in 54 observational studies. Eur. Heart J. 2006, 27, 2763–2774. [Google Scholar] [CrossRef]
- Penninx, B.W.; Beekman, A.T.; Honig, A. Depression and cardiac mortality: Results from a community-based longitudinal study. Arch. Gen. Psychiatry 2001, 58, 221–227. [Google Scholar] [CrossRef] [PubMed]
- Nabi, H.; Shipley, M.J.; Vahtera, J. Effects of depressive symptoms and coronary heart disease and their interactive associations on mortality in middle-aged adults: The Whitehall II cohort study. Heart 2010, 96, 1645–1650. [Google Scholar] [CrossRef] [PubMed]
- Piepenburg, S.M.; Faller, H.; Gelbrich, G.; Störk, S.; Warrings, B.; Ertl, G.; Angermann, C.E. Comparative potential of the 2-item versus the 9-item patient health questionnaire to predict death or rehospitalization in heart failure. Circ. Heart. Fail. 2015, 8, 464–472. [Google Scholar] [CrossRef]
- Elderon, L.; Smolderen, K.G.; Na, B.; Whooley, M.A. Accuracy and prognostic value of American Heart Association: Recommended depression screening in patients with coronary heart disease: Data from the Heart and Soul Study. Circ. Cardiovasc. Qual. Outcomes 2011, 4, 533–540. [Google Scholar] [CrossRef] [PubMed]
- Hammash, M.H.; Hall, L.A.; Lennie, T.A.; Heo, S.; Chung, M.L.; Lee, K.S.; Moser, D.K. Psychometrics of the PHQ-9 as a measure of depressive symptoms in patients with heart failure. Eur. J. Cardiovasc. Nurs. 2013, 12, 446–453. [Google Scholar] [CrossRef]
- American Psychiatric Association. Diagnostic and Statistical Manual of Mental Disorders: DSM-5; American Psychiatric Association: Washington, DC, USA, 2013. [Google Scholar]
- Fulop, G.; Strain, J.J.; Stettin, G. Congestive heart failure and depression in older adults: Clinical course and health services use 6 months after hospitalization. Psychosomatics 2003, 44, 367–373. [Google Scholar] [CrossRef]
- Das, A.; Roy, B.; Schwarzer, G.; Silverman, M.G.; Ziegler, O.; Bandyopadhyay, D.; Philpotts, L.L.; Sinha, S.; Blumenthal, J.A.; Das, S. Comparison of treatment options for depression in heart failure: A network meta-analysis. J. Psychiatr. Res. 2019, 108, 7–23. [Google Scholar] [CrossRef]
- Tu, R.H.; Zeng, Z.Y.; Zhong, G.Q.; Wu, W.F.; Lu, Y.J.; Bo, Z.D.; He, Y.; Huang, W.Q.; Yao, L.M. Effects of exercise training on depression in patients with heart failure: A systematic review and meta-analysis of randomized controlled trials. Eur. J. Heart Fail. 2014, 16, 749–757. [Google Scholar] [CrossRef]
- Blumenthal, J.A.; Babyak, M.A.; O’Connor, C.; Keteyian, S.; Landzberg, J.; Howlett, J.; Kraus, W.; Gottlieb, S.; Blackburn, G.; Swank, A.; et al. Effects of exercise training on depressive symptoms in patients with chronic heart failure: The HF-ACTION randomized trial. JAMA 2012, 308, 465–474. [Google Scholar] [CrossRef] [PubMed]
- Redwine, L.S.; Wilson, K.; Pung, M.A.; Chinh, K.; Rutledge, T.; Mills, P.J.; Smith, B. A Randomized Study Examining the Effects of Mild-to-Moderate Group Exercises on Cardiovascular, Physical, and Psychological Well-being in Patients with Heart Failure. J. Cardiopulm. Rehabil. Prev. 2019, 39, 403–408. [Google Scholar] [CrossRef] [PubMed]
- Jeyanantham, K.; Kotecha, D.; Thanki, D.; Dekker, R.; Lane, D.A. Effects of cognitive behavioural therapy for depression in heart failure patients: A systematic review and meta-analysis. Heart Fail Rev. 2017, 22, 731–741. [Google Scholar] [CrossRef]
- Freedland, K.E.; Carney, R.M.; Rich, M.W.; Steinmeyer, B.C.; Rubin, E.H. Cognitive Behavior Therapy for Depression and Self-Care in Heart Failure Patients: A Randomized Clinical Trial. JAMA Intern. Med. 2015, 175, 1773–1782. [Google Scholar] [CrossRef]
- Rogers, J.G.; Patel, C.B.; Mentz, R.J.; Granger, B.B.; Steinhauser, K.E.; Fiuzat, M.; Adams, P.A.; Speck, A.; Johnson, K.S.; Krishnamoorthy, A.; et al. Palliative Care in Heart Failure: The PAL-HF Randomized, Controlled Clinical Trial. J. Am. Coll. Cardiol. 2017, 70, 331–341. [Google Scholar] [CrossRef] [PubMed]
- O’Connor, C.M.; Jiang, W.; Kuchibhatla, M.; Mehta, R.H.; Clary, G.L.; Cuffe, M.S.; Christopher, E.J.; Alexander, J.D.; Califf, R.M.; Krishnan, R.R. Antidepressant use, depression, and survival in patients with heart failure. Arch. Intern. Med. 2008, 168, 2232–2237. [Google Scholar] [CrossRef]
- O’Connor, C.M.; Jiang, W.; Kuchibhatla, M.; Silva, S.G.; Cuffe, M.S.; Callwood, D.D.; Zakhary, B.; Stough, W.G.; Arias, R.M.; Rivelli, S.K.; et al. Safety and efficacy of sertraline for depression in patients with heart failure: Results of the SADHART-CHF (Sertraline Against Depression and Heart Disease in Chronic Heart Failure) trial. J. Am. Coll. Cardiol. 2010, 56, 692–699. [Google Scholar] [CrossRef]
- Angermann, C.E.; Gelbrich, G.; Störk, S.; Gunold, H.; Edelmann, F.; Wachter, R.; Schunkert, H.; Graf, T.; Kindermann, I.; Haass, M.; et al. Effect of Escitalopram on All-Cause Mortality and Hospitalization in Patients with Heart Failure and Depression: The MOOD-HF Randomized Clinical Trial. JAMA 2016, 315, 2683–2693. [Google Scholar] [CrossRef]
- He, W.; Zhou, Y.; Ma, J.; Wei, B.; Fu, Y. Effect of antidepressants on death in patients with heart failure: A systematic review and meta-analysis. Heart Fail. Rev. 2020, 25, 919–926. [Google Scholar] [CrossRef]
- Archer, J.; Bower, P.; Gilbody, S.; Lovell, K.; Richards, D.; Gask, L.; Dickens, C.; Coventry, P. Collaborative care for depression and anxiety problems. Cochrane Database Syst. Rev. 2012, 10, CD006525. [Google Scholar] [CrossRef]
- Davidson, K.W.; Bigger, J.T.; Burg, M.M.; Carney, R.M.; Chaplin, W.F.; Czajkowski, S.; Dornelas, E.; Duer-Hefele, J.; Frasure-Smith, N.; Freedland, K.E.; et al. Centralized, stepped, patient preference-based treatment for patients with post-acute coronary syndrome depression: CODIACS vanguard randomized controlled trial. JAMA Intern. Med. 2013, 173, 997–1004. [Google Scholar] [CrossRef]
- Bekelman, D.B.; Plomondon, M.E.; Carey, E.P.; Sullivan, M.D.; Nelson, K.M.; Hattler, B.; McBryde, C.F.; Lehmann, K.G.; Gianola, K.; Heidenreich, P.A.; et al. Primary Results of the Patient-Centered Disease Management (PCDM) for Heart Failure Study: A Randomized Clinical Trial. JAMA Intern. Med. 2015, 175, 725–732. [Google Scholar] [CrossRef]
- Heijnen, W.T.; Birkenhager, T.K.; Wierdsma, A.I.; van den Broek, W.W. Antidepressant pharmacotherapy failure and response to subsequent electroconvulsive therapy: A meta-analysis. J. Clin. Psychopharmacol. 2010, 30, 616–619. [Google Scholar] [CrossRef]
- Berlim, M.T.; van den Eynde, F.; Tovar-Perdomo, S.; Daskalakis, Z.J. Response, remission and drop-out rates following high-frequency repetitive transcranial magnetic stimulation (rTMS) for treating major depression: A systematic review and meta-analysis of randomized, double-blind and sham-controlled trials. Psychol. Med. 2014, 44, 225–239. [Google Scholar] [CrossRef]
- Kim, J.; Farchione, T.; Potter, A.; Chen, Q.; Temple, R. Esketamine for Treatment-Resistant Depression—First FDA-Approved Antidepressant in a New Class. N. Engl. J. Med. 2019, 381, 1–4. [Google Scholar] [CrossRef]
- Jiang, W.; Oken, H.; Fiuzat, M.; Shaw, L.K.; Martsberger, C.; Kuchibhatla, M.; Kaddurah-Daouk, R.; Steffens, D.C.; Baillie, R.; Cuffe, M.; et al. Plasma omega-3 polyunsaturated fatty acids and survival in patients with chronic heart failure and major depressive disorder. J. Cardiovasc. Transl. Res. 2012, 5, 92–99. [Google Scholar] [CrossRef]
- Jiang, W.; Whellan, D.J.; Adams, K.F.; Babyak, M.A.; Boyle, S.H.; Wilson, J.L.; Patel, C.B.; Rogers, J.G.; Harris, W.S.; O’Connor, C.M. Long-Chain Omega-3 Fatty Acid Supplements in Depressed Heart Failure Patients: Results of the OCEAN Trial. JACC Heart Fail. 2018, 6, 833–843. [Google Scholar] [CrossRef]
- Hsich, E.M.; Grau-Sepulveda, M.V.; Hernandez, A.F.; Peterson, E.D.; Schwamm, L.H.; Bhatt, D.L.; Fonarow, G.C. Sex differences in in-hospital mortality in acute decompensated heart failure with reduced and preserved ejection fraction. Am. Heart J. 2012, 163, 430–437.e4373. [Google Scholar] [CrossRef]
- Setoguchi, M.; Hashimoto, Y.; Sasaoka, T.; Ashikaga, T.; Isobe, M. Risk factors for rehospitalization in heart failure with preserved ejection fraction compared with reduced ejection fraction. Heart Vessels. 2015, 30, 595–603. [Google Scholar] [CrossRef]
- Nolte, K.; Herrmann-Lingen, C.; Wachter, R.; Gelbrich, G.; Düngen, H.D.; Duvinage, A.; Hoischen, N.; von Oehsen, K.; Schwarz, S.; Hasenfuss, G.; et al. Effects of exercise training on different quality of life dimensions in heart failure with preserved ejection fraction: The Ex-DHF-P trial. Eur. J. Prev. Cardiol. 2015, 22, 582–593. [Google Scholar] [CrossRef]
| Author | Year | Design | Sample Size | Prevalence |
|---|---|---|---|---|
| Jiang et al. [16] | 2001 | Longitudinal study | 682 | 20% |
| Freedland et al. [15] | 2003 | Longitudinal study | 375 | 35.3% |
| Rutledge et al. [13] | 2006 | Meta-analysis | 6202 | 21.5% |
| Sokoreli et al. [14] | 2016 | Meta-analysis | 80,627 | 29% |
| Name | Elements | Time (Min) | Result | Pros | Cons |
|---|---|---|---|---|---|
| Patient Health Questionnaire-2 (PHQ-2) | 2 | <1 | 0–3 |
|
|
| Patient Health Questionnaire-9 (PHQ-9) | 9 | 5 | 0–3 |
|
|
| Hospital Anxiety and Depression Scale (HADS) | 14 (7 for depression and 7 for anxiety) | 5 | 0–3 |
|
|
| Beck Depression Inventory-II (BDI-II) | 21 | 15 | 0–4 |
|
|
| Hamilton Rating Scale for Depression (HAM-D) | 17 | 15 | 0–1 |
|
|
| Geriatric Depression Scale (GDS) | 15 or 30 | 5 | 0–3 |
|
|
| Cardiac Depression Scale (CDS) | 26 | 5 | 26–182 |
|
|
| Trial | Inclusion Criteria | Number of Patients | Drug | Mean Follow-Up | Primary Endpoints | Results |
|---|---|---|---|---|---|---|
| SADHART-CHF |
| 469 | Sertraline vs. placebo | 12 weeks |
| No significant differences between groups (p = 0.78) |
| MOOD-HF |
| 372 | Escitalopram 10–20 mg/day vs. placebo | 24 months |
| No significant between-group difference (p = 0.26) |
| OCEAN |
| 108 | High EPA vs. placebo | 12 weeks |
| No significant between-group difference |
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2023 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Basile, C.; Parlati, A.L.M.; Paolillo, S.; Marzano, F.; Nardi, E.; Chirico, A.; Buonocore, D.; Colella, A.; Fontanarosa, S.; Cotticelli, C.; et al. Depression in Heart Failure with Reduced Ejection Fraction, an Undervalued Comorbidity: An Up-To-Date Review. Medicina 2023, 59, 948. https://doi.org/10.3390/medicina59050948
Basile C, Parlati ALM, Paolillo S, Marzano F, Nardi E, Chirico A, Buonocore D, Colella A, Fontanarosa S, Cotticelli C, et al. Depression in Heart Failure with Reduced Ejection Fraction, an Undervalued Comorbidity: An Up-To-Date Review. Medicina. 2023; 59(5):948. https://doi.org/10.3390/medicina59050948
Chicago/Turabian StyleBasile, Christian, Antonio Luca Maria Parlati, Stefania Paolillo, Federica Marzano, Ermanno Nardi, Alfonsina Chirico, Davide Buonocore, Angela Colella, Sara Fontanarosa, Ciro Cotticelli, and et al. 2023. "Depression in Heart Failure with Reduced Ejection Fraction, an Undervalued Comorbidity: An Up-To-Date Review" Medicina 59, no. 5: 948. https://doi.org/10.3390/medicina59050948
APA StyleBasile, C., Parlati, A. L. M., Paolillo, S., Marzano, F., Nardi, E., Chirico, A., Buonocore, D., Colella, A., Fontanarosa, S., Cotticelli, C., Marchesi, A., Rodolico, D., Dellegrottaglie, S., Gargiulo, P., Prastaro, M., Perrone-Filardi, P., & Montisci, R. (2023). Depression in Heart Failure with Reduced Ejection Fraction, an Undervalued Comorbidity: An Up-To-Date Review. Medicina, 59(5), 948. https://doi.org/10.3390/medicina59050948






