Denture Adhesive Utilization and Associated Factors among Dental Practitioners in the Eastern Province, Saudi Arabia
Abstract
:1. Introduction
2. Materials and Methods
2.1. Study Design, Participants, and Settings
2.2. Ethical Consideration
2.3. Measurement of Study Variables
2.4. Statistical Analysis
3. Results
4. Discussion
5. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Acknowledgments
Conflicts of Interest
References
- Nesbit, S.P.; Barrero, C. Diagnosis and Treatment Planning in Dentistry, 3rd ed.; Elsevier: St Louis, MO, USA, 2017. [Google Scholar]
- Bartlett, D.; Carter, N.; Felton, D.; Goffin, G.; Kawai, Y.; Muller, F.; Polyzois, G.; Walls, A. Global Task Force for Development of Guidelines on Use of Denture Adhesives. 2019, pp. 1–56. Available online: https://www.haleonhealthpartner.com/content/dam/cf-consumer-healthcare/health-professionals/en_US/pdf/SM1064+Global+Denture+Adhesives+Guidelines+1+SCREEN_READY.pdf (accessed on 30 September 2021).
- Kanazawa, M.; Tanoue, M.; Miyayasu, A.; Takeshita, S.; Sato, D.; Asami, M.; Lam, T.V.; Thu, K.M.; Oda, K.; Komagamine, Y.; et al. The patient general satisfaction of mandibular single-implant overdentures and conventional complete dentures: Study protocol for a randomized crossover trial. Medicine 2018, 97, e10721. [Google Scholar] [CrossRef]
- Felton, D.; Cooper, L.; Duqum, I.; Minsley, G.; Guckes, A.; Haug, S.; Meredith, P.; Solie, C.; Avery, D.; Chandler, N.D. Evidence- based guidelines for the care and maintenance of complete dentures: A publication of the American College of Prosthodontists. J. Prosthodont. 2011, 20, S1–S12. [Google Scholar] [CrossRef] [PubMed]
- Mantri, S.; Vinay, S.; Deogade, S.; Mishra, P.; Galav, A.; Sharma, K. Knowledge, attitude and practices of denture adhesives use among private dental practitioners’ of jabalpur city, madhya pradesh: A cross sectional survey. J. Indian Prosthodont. Soc. 2014, 14, 243–250. [Google Scholar] [CrossRef]
- Ohwada, G.; Minakuchi, S.; Sato, Y.; Kondo, H.; Nomura, T.; Tsuboi, A.; Hong, G.; Itoh, Y.; Kawai, Y.; Kimoto, S.; et al. Subjective Evaluation of Denture Adhesives: A Multicenter Randomized Controlled Trial. JDR Clin. Trans. Res. 2020, 5, 50–61. [Google Scholar] [CrossRef]
- Torres-Sánchez, C.; Montoya-Salazar, V.; Torres-Lagares, D.; Gutierrez-Pérez, J.-L.; Jimenez-Castellanos, E. Satisfaction in complete denture wearers with and without adhesives: A randomized, crossover, double-blind clinical trial. J. Clin. Exp. Dent. 2018, 10, e585–e590. [Google Scholar] [CrossRef] [PubMed]
- Coates, A.J. Usage of denture adhesives. J. Dent. 2000, 28, 137–140. [Google Scholar] [CrossRef]
- Shrestha, B.; Parajuli, P.K.; Basnet, B.B.; Adhikari, G.; Pun, D.B.; Rokaya, D.; Bhandari, A. Knowledge and Attitude of Nepalese Dental Interns towards Adhesives for Removal Dentures. J. BP Koirala Inst. Health Sci. 2019, 2, 40–45. [Google Scholar] [CrossRef]
- Murthy, V.; Reddy, V.K.; Vidyalakshmi, S. Awareness of zinc toxicity in denture adhesives among dental practitioners in Puducherry-A cross-sectional study. Int. J. Adv. Res. 2017, 4, 147–151. [Google Scholar] [CrossRef]
- Thakur, S.N.; Khanal, B.; Chaulagain, R.; Shrestha, P.; Maharjan, A.; Singh, H. Knowledge, Attitude and Practices of Dental Adhesives use among Dental Practitioners of Chitwan. J. Nepal. Prosthodont. Soc. 2020, 3, 1–8. [Google Scholar] [CrossRef]
- Muneer, M.U.; Ahmed, A.R.; Kamran, M.F. Awareness of dentists and complete denture wearers towards denture adhesives. Pak. Oral Dent. J. 2013, 33, 192–194. [Google Scholar]
- Fallahi, A.; Khadivi, N.; Roohpour, N.; Middleton, A.M.; Kazemzadeh-Narbat, M.; Annabi, N.; Khademhosseini, A.; Tamayol, A. Characterization, mechanistic analysis and improving the properties of denture adhesives. Dent. Mater. 2018, 34, 120–131. [Google Scholar] [CrossRef] [PubMed]
- Kumar, P.R.; Shajahan, P.A.; Mathew, J.; Koruthu, A.; Aravind, P.; Ahammed, M.F. Denture adhesives in prosthodontics: An overview. J. Int. Oral Health JIOH 2015, 7 (Suppl. 1), 93–95. [Google Scholar] [PubMed]
- Bo, T.M.; Hama, Y.; Akiba, N.; Minakuchi, S. Utilization of denture adhesives and the factors associated with its use: A cross-sectional survey. BMC Oral Health 2020, 20, 194. [Google Scholar] [CrossRef] [PubMed]
- Shamsolketabi, S.; Nili, M. The effect of denture adhesive on the efficiency of complete denture in patients with different alveolar ridges. Dent. Res. J. 2018, 15, 271–275. [Google Scholar]
- Ministry of Health. Available online: https://www.moh.gov.sa/en/Ministry/Statistics/book/Pages/default.aspx (accessed on 13 August 2022).
- Polyzois, G.; Lagouvardos, P.; Omar, R.; Brunton, P. Attitudes of dentists toward denture adhesives: A questionnaire survey in Greece. J. Prosthet. Dent. 2017, 118, 643–649. [Google Scholar] [CrossRef]
- Surabathula, V.; Desai, Y.; Pandey, S.; Modh, H.; Bhat, D. Knowledge and Awareness Among Dentists and Dental Students Regarding Dental Adhesives in Navi Mumbai. J. Clin. Case Rep. Med. Res. 2020, 1, 6. [Google Scholar]
- Koksal, T.; Dikbas, I.; Ozkurt, Z.; Bal, B.; Kazaoglu, E. Professional attitudes toward the use of denture adhesives: A survey among Nepalese prosthodontists. VARIA 2007, 6, 33–39. [Google Scholar]
- Al Taweel, S.M.; Al Shehri, H.A. Knowledge and attitudes of dental interns toward denture adhesives in King Saud University, Riyadh, Saudi Arabia. Eur. J. Dent. 2016, 10, 536–540. [Google Scholar] [CrossRef]
- Anwar, A.; Syreen, S.; Kumar, B.; Narayan, J.P.; Kumari, N. Knowledge and Attitude of Dental Surgeons about Use of Denture Adhesive. Quest. Based Study 2020, 4, 32–34. [Google Scholar] [CrossRef]
- Ozcan, M.; Kulak, Y.; Arikan, A.; Silahtar, E. The attitude of complete denture wearers towards denture adhesives in Istanbul. J. Oral Rehabil. 2004, 31, 131–134. [Google Scholar] [CrossRef] [PubMed]
- Costa, R.T.; Vila-Nova, T.E.; de França, A.J.; da Silva Casado, B.G.; de Souza Leão, R.; de Moraes, S.L. Masticatory performance of denture wearers with the use of denture adhesives: A systematic review. J. Prosthet. Dent. 2020, 127, 233–238. [Google Scholar] [CrossRef] [PubMed]
- Harada, K.; Horinouchi, R.; Murakami, M.; Yamashita, Y.; Yanagisawa, T.; Shimotahira, N.; Kamashita, Y.; Hamada, T.; Nishi, Y.; Nishimura, M. An in vitro study on the selection of surfactants for removal of cream denture adhesives from dentures and their application to denture cleaners. J. Prosthodont. Res. 2023, 67, 262–270. [Google Scholar] [CrossRef] [PubMed]
- Ozkan, Y.K.; Ucankale, M.; Ozcan, M.; Uner, N. Effect of denture adhesive on the micro-organisms in vivo. Gerodontology 2012, 29, 9–16. [Google Scholar] [CrossRef]
- Mendes, J.; Mendes, J.M.; Barreiros, P.; Aroso, C.; Silva, A.S. Retention Capacity of Original Denture Adhesives and White Brands for Conventional Complete Dentures: An In Vitro Study. Polymers 2022, 14, 1749. [Google Scholar] [CrossRef] [PubMed]
- Lemos, C.A.; Carreiro, A.D.; Rosa, C.D.; Gomes, J.M.; de Oliveira Limirio, J.P.; Mendonça, G.; Pellizzer, E.P. Does the use of an adhesive improve conventional complete dentures? A systematic review of randomized controlled trials. J. Prosthet. Dent. 2021, 128, 150–157. [Google Scholar] [CrossRef]

| Variables | Frequency (n) | Percent (%) |
|---|---|---|
| Age | ||
| ≤35 years | 172 | 61.6 |
| >35 years | 107 | 38.4 |
| Gender | ||
| Male | 158 | 56.6 |
| Female | 121 | 43.4 |
| Professional qualification | ||
| General dentist | 160 | 57.3 |
| Advanced general dentist/specialist/consultant | 119 | 42.7 |
| Place of work | ||
| Government sector | 112 | 40.1 |
| Private sector | 167 | 59.9 |
| Years in dental practice/teaching: | ||
| ≤10 years | 167 | 59.9 |
| >10 years | 112 | 40.1 |
| Variables | Frequency (n) | Percent (%) |
|---|---|---|
| Used denture adhesives in your dental practice | ||
| Yes | 110 | 39.4 |
| No | 169 | 60.6 |
| Recommended using denture adhesive with normal cases | ||
| Yes, as a routine practice for all patients | 8 | 2.9 |
| Yes, when needed | 180 | 64.5 |
| No, not at all | 91 | 32.6 |
| Recalled your patients using denture adhesives periodically | ||
| Yes | 101 | 36.2 |
| No | 178 | 63.8 |
| Taught about denture adhesives in your undergraduate program | ||
| Yes | 154 | 55.2 |
| No | 125 | 44.8 |
| Attended a continuing education program about denture adhesives. | ||
| Yes | 35 | 12.5 |
| No | 244 | 87.5 |
| Updated knowledge about denture adhesive by reading books/journals etc. | ||
| Yes | 60 | 21.5 |
| No | 219 | 78.5 |
| Items | Yes, Very Much n (%) | Yes, but Only Limited Knowledge n (%) | No n (%) |
| Familiar with denture adhesives | 53 (19.0) | 202 (72.4) | 24 (8.6) |
| Knew the chemical composition of denture adhesives | 31 (11.1) | 83 (29.7) | 165 (59.1) |
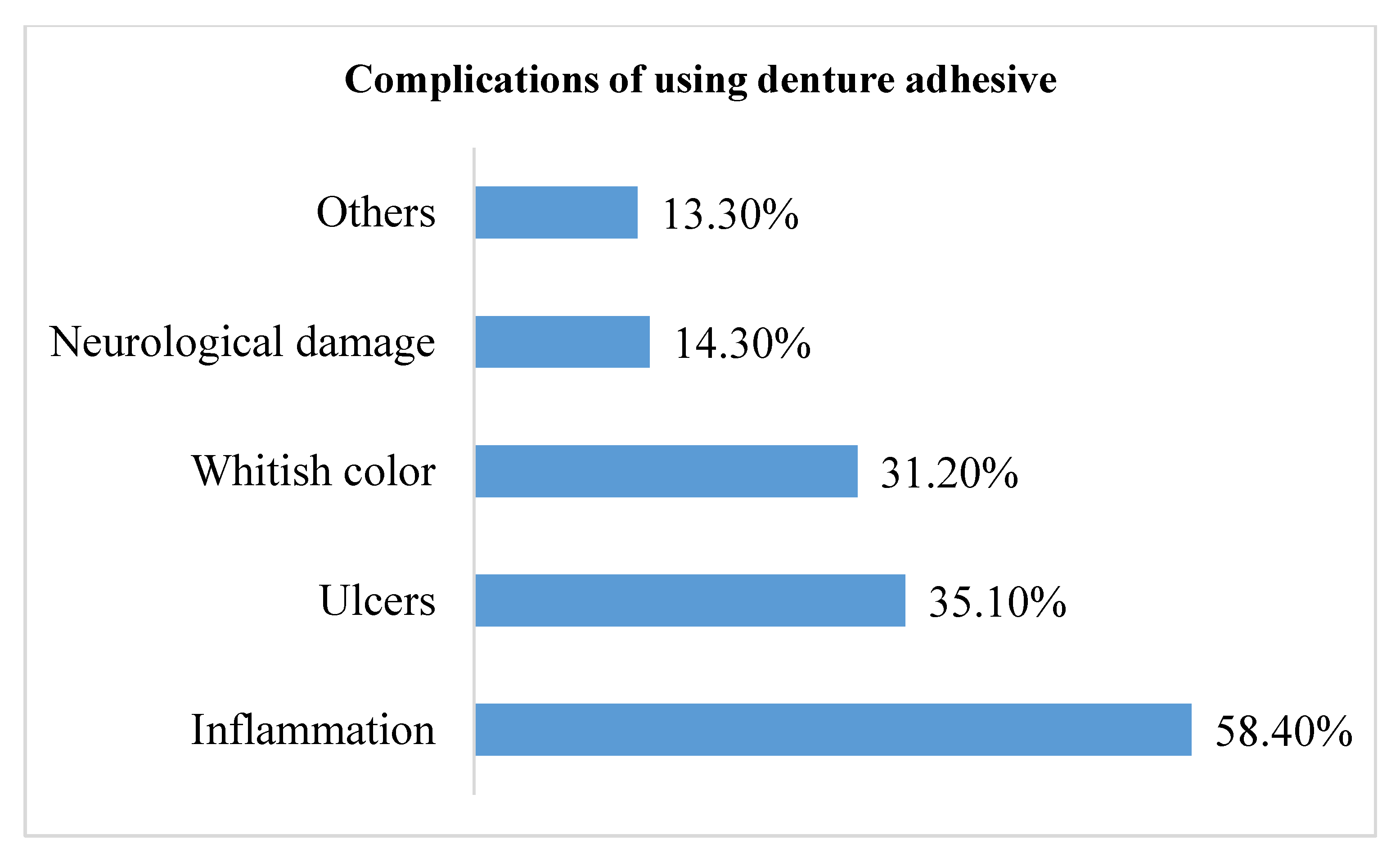
| Aware of any disadvantages of denture adhesives | 47 (16.8) | 109 (39.1) | 123 (44.1) |
| Aware of denture adhesives guidelines by Oral Health Foundation | 25 (9.0) | 71 (25.4) | 183 (65.6) |
| Knew any alternatives to denture adhesives | 37 (13.3) | 60 (21.5) | 182 (65.2) |
| Items | Yes n(%) | No n(%) | Not sure n(%) |
| Denture adhesives is considered a temporary solution | 176 (63.1) | 29 (10.4) | 74 (26.5) |
| Denture adhesives can produce allergic reaction | 175 (62.7) | 21 (7.5) | 83 (29.7) |
| Use of denture adhesives improves the denture foundation area | 75 (26.9) | 92 (33.0) | 112 (40.1) |
| Use of denture adhesive is more effective than a clinical intervention such as relining | 24 (8.6) | 146 (52.3) | 109 (39.1) |
| Denture adhesive is soluble in saliva | 68 (24.4) | 90 (32.3) | 121 (43.4) |
| Improper use of denture adhesives can cause denture stomatitis | 155 (55.6) | 28 (10.0) | 96 (34.4) |
| Prolonged use of denture adhesives with ill-fitting dentures can cause residual ridge resorption | 137 (49.1) | 44 (15.8) | 98 (35.1) |
| Excessive use of zinc containing denture adhesives can cause neurological disease | 44 (15.8) | 48 (17.2) | 187 (67.0) |
| Variables | Unadjusted OR | p-Value |
|---|---|---|
| Age ≤35 years >35 years | 0.50 (0.31, 0.83) | 0.006 |
| Gender Male Female | 1.71 (1.05, 2.81) | 0.031 |
| Professional qualification General dentist Advanced general dentist/ specialist/ consultant | 0.73 (0.45, 1.19) | 0.208 |
| Place of work Government sector Private sector | 1.01 (0.62, 1.65) | 0.970 |
| Years in dental practice ≤10 years >10 years | 0.61 (0.38, 1.00) | 0.050 |
| Taught about denture adhesives in your undergraduate program | 1.02 (0.63, 1.65) | 0.944 |
| Attended a continuing education program about denture adhesives | 3.46 (1.64, 7.29) | 0.001 |
| Updated knowledge about denture adhesives by reading books/journals, etc. | 5.18 (2.78, 9.65) | <0.001 |
| Variables | Adjusted OR | p-Value |
|---|---|---|
| Age ≤35 years >35 years (Reference category) | 0.46 (0.19, 1.09) | 0.078 |
| Gender Male Female (Reference category) | 1.30 (0.74, 2.29) | 0.364 |
| Professional qualification General dentist Advanced general dentist/specialist/consultant (Reference category) | 1.21 (0.65, 2.28) | 0.548 |
| Place of work Government sector Private sector (Reference category) | 0.97 (0.55, 1.71) | 0.920 |
| Years in dental practice ≤10 years >10 years (Reference category) | 1.22 (0.51, 2.93) | 0.658 |
| Taught about denture adhesives in your undergraduate program Yes No (Reference category) | 1.11 (0.65, 1.91) | 0.705 |
| Attended a continuing education program about denture adhesives Yes No (Reference category) | 2.41 (1.06, 5.46) | 0.036 |
| Updated knowledge about denture adhesives by reading books/journals etc. Yes No (Reference category) | 4.43 (2.31, 8.48) | <0.001 |
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2023 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Gad, M.M.; Almusallam, M.O.; Almarar, F.H.; Al khaldi, H.O.; Aldossary, A.K.; Almutairi, W.M.; Alghamdi, N.A.; Alssaialiy, Y.S.; Alghamdi, N.I.; Nazir, M.A. Denture Adhesive Utilization and Associated Factors among Dental Practitioners in the Eastern Province, Saudi Arabia. Medicina 2023, 59, 974. https://doi.org/10.3390/medicina59050974
Gad MM, Almusallam MO, Almarar FH, Al khaldi HO, Aldossary AK, Almutairi WM, Alghamdi NA, Alssaialiy YS, Alghamdi NI, Nazir MA. Denture Adhesive Utilization and Associated Factors among Dental Practitioners in the Eastern Province, Saudi Arabia. Medicina. 2023; 59(5):974. https://doi.org/10.3390/medicina59050974
Chicago/Turabian StyleGad, Mohammed M., Mayyasah O. Almusallam, Fadak H. Almarar, Haya O. Al khaldi, Alhanoof K. Aldossary, Wejdan M. Almutairi, Nawaf A. Alghamdi, Yasser S. Alssaialiy, Nawaf I. Alghamdi, and Muhammad A. Nazir. 2023. "Denture Adhesive Utilization and Associated Factors among Dental Practitioners in the Eastern Province, Saudi Arabia" Medicina 59, no. 5: 974. https://doi.org/10.3390/medicina59050974
APA StyleGad, M. M., Almusallam, M. O., Almarar, F. H., Al khaldi, H. O., Aldossary, A. K., Almutairi, W. M., Alghamdi, N. A., Alssaialiy, Y. S., Alghamdi, N. I., & Nazir, M. A. (2023). Denture Adhesive Utilization and Associated Factors among Dental Practitioners in the Eastern Province, Saudi Arabia. Medicina, 59(5), 974. https://doi.org/10.3390/medicina59050974







