Evaluation of Blood Pressure Status and Mortality in Turkey: Findings from Chronic Diseases and Risk Factors Cohort Study
Abstract
:1. Introduction
2. Materials and Methods
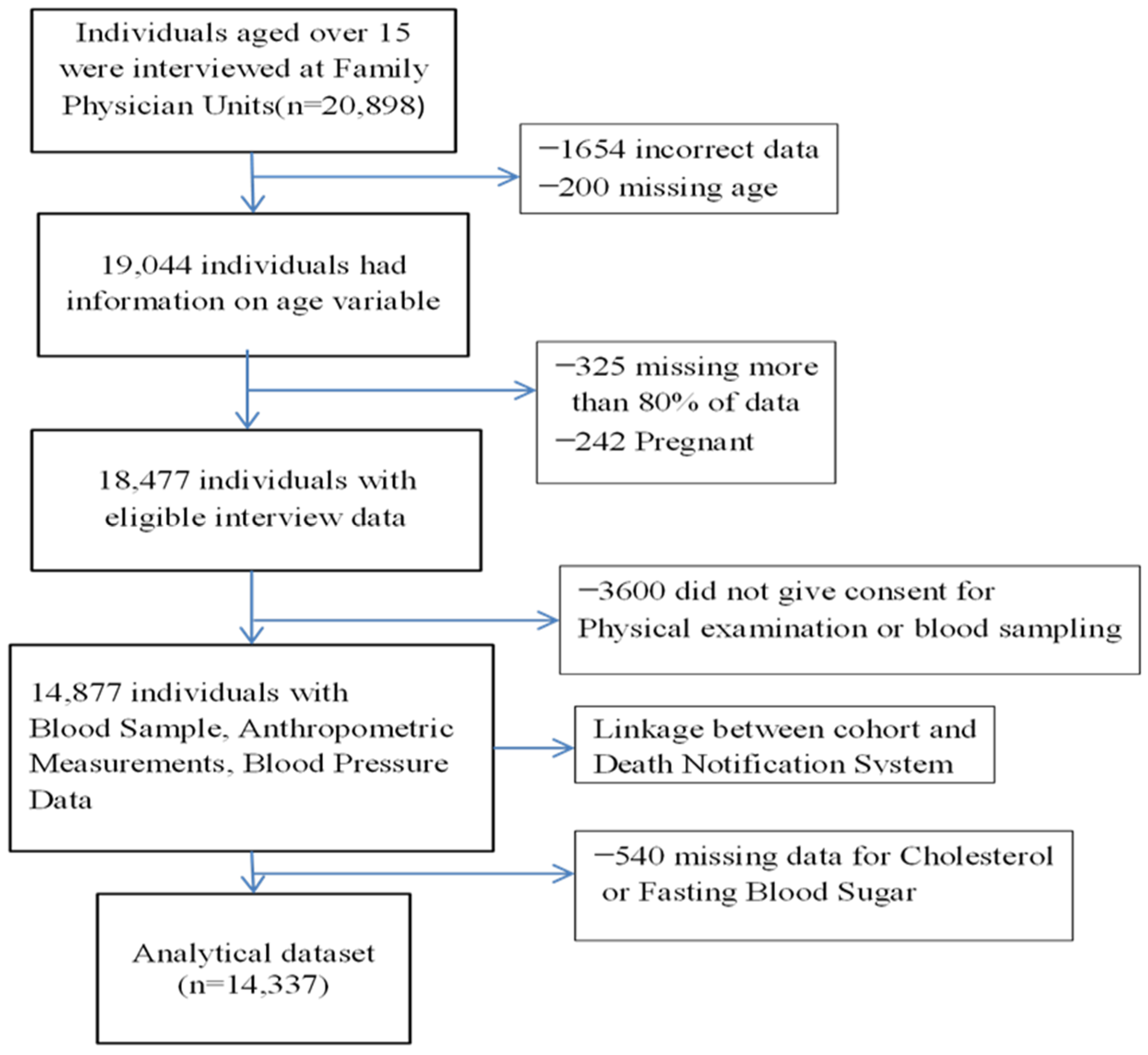
2.1. Study Population and Data Collection
2.2. Outcomes
2.3. Covariates
2.4. Statistical Methods
3. Results
3.1. Baseline Characteristics
3.2. Survival
4. Discussion
5. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Acknowledgments
Conflicts of Interest
References
- WHO. Cardiovascular Diseases (CVDs) Fact sheet. Available online: https://www.who.int/en/news-room/fact-sheets/detail/cardiovascular-diseases-(cvds) (accessed on 18 March 2023).
- Olsen, M.H.; Angell, S.Y.; Asma, S.; Boutouyrie, P.; Burger, D.; Chirinos, J.A.; Damasceno, A.; Delles, C.; Gimenez-Roqueplo, A.P.; Hering, D.; et al. A call to action and a lifecourse strategy to address the global burden of raised blood pressure on current and future generations: The Lancet Commission on hypertension. Lancet 2016, 388, 2665–2712. [Google Scholar] [CrossRef]
- Bundy, J.D.; Li, C.; Stuchlik, P.; Bu, X.; Kelly, T.N.; Mills, K.T.; He, H.; Chen, J.; Whelton, P.K.; He, J. Systolic Blood Pressure Reduction and Risk of Cardiovascular Disease and Mortality: A Systematic Review and Network Meta-analysis. JAMA Cardiol. 2017, 2, 775–781. [Google Scholar] [CrossRef] [Green Version]
- Yusuf, S.; Joseph, P.; Rangarajan, S.; Islam, S.; Mente, A.; Hystad, P.; Brauer, M.; Kutty, V.R.; Gupta, R.; Wielgosz, A.; et al. Modifiable risk factors, cardiovascular disease, and mortality in 155,722 individuals from 21 high-income, middle-income, and low-income countries (PURE): A prospective cohort study. Lancet 2020, 395, 795–808. [Google Scholar] [CrossRef] [Green Version]
- UN. Transforming Our World: The 2030 Agenda for Sustainable Development; UN: New York, NY, USA, 2015. [Google Scholar]
- Canoy, D.; Nazarzadeh, M.; Copland, E.; Bidel, Z.; Rao, S.; Li, Y.; Rahimi, K. How Much Lowering of Blood Pressure Is Required to Prevent Cardiovascular Disease in Patients With and Without Previous Cardiovascular Disease? Curr. Cardiol. Rep. 2022, 24, 851–860. [Google Scholar] [CrossRef]
- Ettehad, D.; Emdin, C.A.; Kiran, A.; Anderson, S.G.; Callender, T.; Emberson, J.; Chalmers, J.; Rodgers, A.; Rahimi, K. Blood pressure lowering for prevention of cardiovascular disease and death: A systematic review and meta-analysis. Lancet 2016, 387, 957–967. [Google Scholar] [CrossRef] [Green Version]
- NCD Risk Factor Collaboration. Worldwide trends in hypertension prevalence and progress in treatment and control from 1990 to 2019: A pooled analysis of 1201 population-representative studies with 104 million participants. Lancet 2021, 398, 957–980. [Google Scholar] [CrossRef]
- MoH. Health Statistics Yearbook of Turkey; Ministry of Health of Turkey: Ankara, Turkey, 2020. [Google Scholar]
- Unal, B.; Sözmen, K.; Arık, H.; Gerçeklioğlu, G.; Altun, D.U.; Şimşek, H.; Doganay, S.; Demiral, Y.; Aslan, Ö.; Bennett, K.; et al. Explaining the decline in coronary heart disease mortality in Turkey between 1995 and 2008. BMC Public Health 2013, 13, 1135. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Dinç, G.; Sözmen, K.; Gerçeklioğlu, G.; Arık, H.; Critchley, J.; Unal, B. Decreasing trends in cardiovascular mortality in Turkey between 1988 and 2008. BMC Public Health 2013, 13, 896. [Google Scholar] [CrossRef] [Green Version]
- Kılıçkap, M.; Barçın, C.; Göksülük, H.; Karaaslan, D.; Özer, N.; Kayıkçıoğlu, M.; Ural, D.; Yılmaz, M.B.; Abacı, A.; Arıcı, M.; et al. Data on prevalence of hypertension and blood pressure in Turkey: Systematic review, meta-analysis and meta-regression of epidemiological studies on cardiovascular risk factors. Turk Kardiyol. Dern. Ars. Turk Kardiyol. Derneginin Yayin. Organidir 2018, 46, 525–545. [Google Scholar]
- Dastan, I.; Erem, A.; Cetinkaya, V. Awareness, treatment, control of hypertension, and associated factors: Results from a Turkish national study. Clin. Exp. Hypertens. 2018, 40, 90–98. [Google Scholar] [CrossRef]
- Ünal, B.; Ergör, G.; Horasan, G.; Kalaça, S.; Sözmen, K. Chronic Diseases and Risk Factors Survey in Turkey; Ministry of Health of Turkey: Ankara, Turkey, 2013. [Google Scholar]
- Ünal, B.; Ergör, G.; Horasan, G.; Kalaça, S.; Sözmen, K. Noncommunicable Diseases and Risk Factors Cohort Study in Turkey; 1206; Ministry of Health: Ankara, Turkey, 2020. [Google Scholar]
- Sahan, C.; Sozmen, K.; Unal, B.; O’Flaherty, M.; Critchley, J. Potential benefits of healthy food and lifestyle policies for reducing coronary heart disease mortality in Turkish adults by 2025: A modelling study. BMJ Open 2016, 6, e011217. [Google Scholar] [CrossRef] [Green Version]
- Özdemir, R.; Rao, C.; Öcek, Z.; Dinç Horasan, G. Reliable mortality statistics for Turkey: Are we there yet? BMC Public Health 2015, 15, 545. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- OECD. Rural Well-Being: Geography of Opportunities, Country Note for Turkey. Available online: https://www.oecd.org/regional/Rural-WellBeing-Turkey.pdf (accessed on 15 March 2023).
- Wang, D.D.; Li, Y.; Bhupathiraju, S.N.; Rosner, B.A.; Sun, Q.; Giovannucci, E.L.; Rimm, E.B.; Manson, J.E.; Willett, W.C.; Stampfer, M.J.; et al. Fruit and Vegetable Intake and Mortality: Results From 2 Prospective Cohort Studies of US Men and Women and a Meta-Analysis of 26 Cohort Studies. Circulation 2021, 143, 1642–1654. [Google Scholar] [CrossRef]
- WHO. WHO Guidelines on Physical Activity and Sedentary Behaviour; World Health Organization: Geneva, Switzerland, 2020; pp. 1–582. [Google Scholar]
- Janssen, I.; Katzmarzyk, P.T.; Ross, R. Body mass index, waist circumference, and health risk: Evidence in support of current National Institutes of Health guidelines. Arch. Intern. Med. 2002, 162, 2074–2079. [Google Scholar] [CrossRef] [Green Version]
- Johnston, M.C.; Crilly, M.; Black, C.; Prescott, G.J.; Mercer, S.W. Defining and measuring multimorbidity: A systematic review of systematic reviews. Eur. J. Public Health 2019, 29, 182–189. [Google Scholar] [CrossRef]
- Magliano, D.J.; Boyko, E.J. IDF Diabetes Atlas, 10th ed.; International diabetes Federation: Brussels, Belgium, 2021. [Google Scholar]
- Chobanian, A.V.; Bakris, G.L.; Black, H.R.; Cushman, W.C.; Green, L.A.; Izzo, J.L., Jr.; Jones, D.W.; Materson, B.J.; Oparil, S.; Wright, J.T., Jr.; et al. Seventh report of the Joint National Committee on Prevention, Detection, Evaluation, and Treatment of High Blood Pressure. Hypertension 2003, 42, 1206–1252. [Google Scholar] [CrossRef] [Green Version]
- Williams, B.; Mancia, G.; Spiering, W.; Agabiti Rosei, E.; Azizi, M.; Burnier, M.; Clement, D.L.; Coca, A.; de Simone, G.; Dominiczak, A.; et al. 2018 ESC/ESH Guidelines for the management of arterial hypertension. Eur. Heart J. 2018, 39, 3021–3104. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- D’Agostino, R.B., Sr.; Vasan, R.S.; Pencina, M.J.; Wolf, P.A.; Cobain, M.; Massaro, J.M.; Kannel, W.B. General cardiovascular risk profile for use in primary care: The Framingham Heart Study. Circulation 2008, 117, 743–753. [Google Scholar] [CrossRef] [Green Version]
- Üner, S.; Balcılar, M.; Ergüder, T. Türkiye Hanehalkı Sağlık Araştırması: Bulaşıcı Olmayan Hastalıkların Risk Faktörleri Prevalansı 2017 (STEPS); Ministry of Health of Turkey: Ankara, Turkey, 2019. [Google Scholar]
- Sepanlou, S.; Najafi, F.; Poustchi, H.; Parsaeian, M.; Ahmadi, A.; Somi, M.; Moradpour, F.; Alizadeh-Navaei, R.; Gohari, A.; Zamani, B.; et al. Prevalence, awareness, treatment, and control of hypertension based on ACC/AHA versus JNC7 guidelines in the PERSIAN cohort study. Sci. Rep. 2022, 12, 4057. [Google Scholar] [CrossRef]
- Böhm, M.; Schumacher, H.; Teo, K.K.; Lonn, E.M.; Mahfoud, F.; Mann, J.F.E.; Mancia, G.; Redon, J.; Schmieder, R.E.; Marx, N.; et al. Cardiovascular outcomes and achieved blood pressure in patients with and without diabetes at high cardiovascular risk. Eur. Heart J. 2019, 40, 2032–2043. [Google Scholar] [CrossRef] [Green Version]
- Sim, J.J.; Shi, J.; Kovesdy, C.P.; Kalantar-Zadeh, K.; Jacobsen, S.J. Impact of achieved blood pressures on mortality risk and end-stage renal disease among a large, diverse hypertension population. J. Am. Coll. Cardiol. 2014, 64, 588–597. [Google Scholar] [CrossRef] [Green Version]
- Choudhry, N.K.; Kronish, I.M.; Vongpatanasin, W.; Ferdinand, K.C.; Pavlik, V.N.; Egan, B.M.; Schoenthaler, A.; Houston Miller, N.; Hyman, D.J. Medication Adherence and Blood Pressure Control: A Scientific Statement From the American Heart Association. Hypertension 2022, 79, e1–e14. [Google Scholar] [CrossRef]
- Ferdinand, K.C.; Senatore, F.F.; Clayton-Jeter, H.; Cryer, D.R.; Lewin, J.C.; Nasser, S.A.; Fiuzat, M.; Califf, R.M. Improving Medication Adherence in Cardiometabolic Disease: Practical and Regulatory Implications. J. Am. Coll. Cardiol. 2017, 69, 437–451. [Google Scholar] [CrossRef]
- Tarı Selçuk, K.; Mercan, Y.; Aydın, T. Uncontrolled Blood Pressure in Patients with Hypertension and Associated Factors: The Role of Low Health Literacy. Erciyes Med. J. 2018, 40, 222–227. [Google Scholar] [CrossRef]
- Sørensen, K.; Van den Broucke, S.; Fullam, J.; Doyle, G.; Pelikan, J.; Slonska, Z.; Brand, H. Health literacy and public health: A systematic review and integration of definitions and models. BMC Public Health 2012, 12, 80. [Google Scholar] [CrossRef] [Green Version]
- De Feo, M.; Del Pinto, R.; Pagliacci, S.; Grassi, D.; Ferri, C. Real-World Hypertension Prevalence, Awareness, Treatment, and Control in Adult Diabetic Individuals: An Italian Nationwide Epidemiological Survey. High Blood Press. Cardiovasc. Prev. Off. J. Ital. Soc. Hypertens. 2021, 28, 301–307. [Google Scholar] [CrossRef]
- Muleta, S.; Melaku, T.; Chelkeba, L.; Assefa, D. Blood pressure control and its determinants among diabetes mellitus co-morbid hypertensive patients at Jimma University medical center, South West Ethiopia. Clin. Hypertens. 2017, 23, 29. [Google Scholar] [CrossRef] [Green Version]
- Singh, M.; Mensah, G.A.; Bakris, G. Pathogenesis and clinical physiology of hypertension. Cardiol. Clin. 2010, 28, 545–559. [Google Scholar] [CrossRef]
- Del Pinto, R.; Pietropaoli, D.; Munoz-Aguilera, E.; D’Aiuto, F.; Czesnikiewicz-Guzik, M.; Monaco, A.; Guzik, T.J.; Ferri, C. Periodontitis and Hypertension: Is the Association Causal? High Blood Press. Cardiovasc. Prev. Off. J. Ital. Soc. Hypertens. 2020, 27, 281–289. [Google Scholar] [CrossRef]
- Przezak, A.; Bielka, W.; Pawlik, A. Hypertension and Type 2 Diabetes-The Novel Treatment Possibilities. Int. J. Mol. Sci. 2022, 23, 6500. [Google Scholar] [CrossRef]
- Qu, Y.; Niu, H.; Li, L.; Li, M.; Yan, S.; Li, M.; Jiang, S.; Ma, X.; Li, B.; Wu, H. Analysis of Dose-response Relationship between BMI and Hypertension in Northeastern China Using Restricted Cubic Spline Functions. Sci. Rep. 2019, 9, 18208. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Bhandari, P.; Prakash, V.; Flack, J.M. Influence of Obesity on Blood Pressure Responses to Antihypertensive Drug Therapy in an Urban Hypertension Specialty Clinic. Am. J. Hypertens. 2022, 35, 740–744. [Google Scholar] [CrossRef]
- Aronow, W.S. Association of obesity with hypertension. Ann. Transl. Med. 2017, 5, 350. [Google Scholar] [CrossRef] [Green Version]
- Barengo, N.C.; Antikainen, R.; Kastarinen, M.; Laatikainen, T.; Tuomilehto, J. The effects of control of systolic and diastolic hypertension on cardiovascular and all-cause mortality in a community-based population cohort. J. Hum. Hypertens. 2013, 27, 693–697. [Google Scholar] [CrossRef]
- Jaeger, B.C.; Bress, A.P.; Bundy, J.D.; Cheung, A.K.; Cushman, W.C.; Drawz, P.E.; Johnson, K.C.; Lewis, C.E.; Oparil, S.; Rocco, M.V.; et al. Longer-Term All-Cause and Cardiovascular Mortality With Intensive Blood Pressure Control: A Secondary Analysis of a Randomized Clinical Trial. JAMA Cardiol. 2022, 7, 1138–1146. [Google Scholar] [CrossRef] [PubMed]
- Zhou, D.; Xi, B.; Zhao, M.; Wang, L.; Veeranki, S.P. Uncontrolled hypertension increases risk of all-cause and cardiovascular disease mortality in US adults: The NHANES III Linked Mortality Study. Sci. Rep. 2018, 8, 9418. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Douros, A.; Tölle, M.; Ebert, N.; Gaedeke, J.; Huscher, D.; Kreutz, R.; Kuhlmann, M.K.; Martus, P.; Mielke, N.; Schneider, A.; et al. Control of blood pressure and risk of mortality in a cohort of older adults: The Berlin Initiative Study. Eur. Heart J. 2019, 40, 2021–2028. [Google Scholar] [CrossRef]
- Whelton, P.K.; Carey, R.M.; Aronow, W.S.; Casey, D.E., Jr.; Collins, K.J.; Dennison Himmelfarb, C.; DePalma, S.M.; Gidding, S.; Jamerson, K.A.; Jones, D.W.; et al. 2017 ACC/AHA/AAPA/ABC/ACPM/AGS/APhA/ASH/ASPC/NMA/PCNA Guideline for the Prevention, Detection, Evaluation, and Management of High Blood Pressure in Adults: Executive Summary: A Report of the American College of Cardiology/American Heart Association Task Force on Clinical Practice Guidelines. Circulation 2018, 138, e426–e483. [Google Scholar]
- MOH. Aile Hekimliği Uygulamasında Önerilen Periyodik Sağlık Muayeneleri ve Tarama Testleri; Public Health Institution, Ministry of Health of Turkey: Ankara, Turkey, 2015. [Google Scholar]
- Tokgozoglu, L.; Kayikcioglu, M.; Ekinci, B. The landscape of preventive cardiology in Turkey: Challenges and successes. Am. J. Prev. Cardiol. 2021, 6, 100184. [Google Scholar] [CrossRef]
- Demirci, D.; Ersan Demirci, D. Comparison of SCORE-Turkey and SCORE for high-risk countries: A cross-sectional analysis of patients presenting with initial episode of acute coronary syndrome. Turk Kardiyol. Dern. Ars. Turk Kardiyol. Derneginin Yayin. Organidir 2019, 47, 646–656. [Google Scholar] [CrossRef]
- Günaydın, Z.Y.; Karagöz, A.; Bektaş, O.; Kaya, A.; Kırış, T.; Erdoğan, G.; Işık, T.; Ayhan, E. Comparison of the Framingham risk and SCORE models in predicting the presence and severity of coronary artery disease considering SYNTAX score. Anatol. J. Cardiol. 2016, 16, 412–418. [Google Scholar] [PubMed]




| Variables | Normotensive | Untreated | Treated & Controlled | Treated & Uncontrolled | p |
|---|---|---|---|---|---|
| N (%) | 10,921 (75.5) | 1484 (10.3) | 1066 (7.4) | 996 (6.9) | |
| Age (years) (%) | <0.001 | ||||
| 18–39 | 54.0 | 22.1 | 4.3 | 2.8 | |
| 40–59 | 29.9 | 48.3 | 44.5 | 38.5 | |
| ≥60 | 16.1 | 29.5 | 51.2 | 58.7 | |
| Female (%) | 51.3 | 47.8 | 64.9 | 68.7 | <0.001 |
| Marital status (%) | |||||
| Married | 67.7 | 78.2 | 76.6 | 72.5 | <0.001 |
| Single/Divorced/widowed | 32.3 | 21.8 | 23.4 | 27.5 | |
| Education status (%) | |||||
| Primary school or less | 49.2 | 71.5 | 77.1 | 82.8 | <0.001 |
| High school | 40.5 | 21.4 | 15.0 | 12.8 | |
| University degree or higher | 10.3 | 7.1 | 7.9 | 4.4 | |
| Fruit and vegetable (%) | 13.6 | 14.1 | 18.1 | 16.7 | <0.001 |
| Smoking (%) | |||||
| Non-smoker | 66.3 | 66.2 | 73.1 | 76.7 | <0.001 |
| Ex-smoker | 7.3 | 11.9 | 15.3 | 13.2 | |
| Current smoker | 26.4 | 21.9 | 11.6 | 10.2 | |
| VAS score | 66.9 ± 30.6 | 63.84 ± 27.7 | 59.17 ± 25.33 | 57.80 ± 24.73 | <0.001 |
| BMI > 30 kg/m2 (%) | 17.4 | 42.2 | 47.3 | 56.4 | <0.001 |
| High waist circumference (%) | 26.7 | 55.5 | 67.0 | 75.6 | <0.001 |
| Area lived (%) | |||||
| Rural | 30.6 | 36.2 | 30.1 | 38.4 | <0.001 |
| Multimorbidity (%) | |||||
| ≥2 | 5.9 | 27.5 | 56.7 | 59.4 | <0.001 |
| Total Cholesterol (mg/dL) | 174.9 ± 38.9 | 192.4 ± 40.6 | 195.1 ± 42.5 | 199.1 ± 44.2 | <0.001 |
| LDL Cholesterol (mg/dL) | 104.6 ± 34.9 | 117.9 ± 37.1 | 118.5 ± 39.3 | 120.6 ± 37.1 | <0.001 |
| Coronary Heart Disease (%) | 1.2 | 2.9 | 12.1 | 17.0 | <0.001 |
| Stroke (%) | 1.3 | 2.4 | 6.3 | 8.1 | <0.001 |
| Diabetes (%) | 5.2 | 15.9 | 32.5 | 35.6 | <0.001 |
| Systolic Blood Pressure (mmHg) | 112.0 ± 11.8 | 139.0 ± 18.4 | 119.7 ± 11.0 | 148.9 ± 17.6 | <0.001 |
| Diastolic Blood Pressure (mmHg) | 70.8 ± 8.8 | 88.0 ± 11.3 | 74.4 ± 7.9 | 87.6 ± 11.8 | <0.001 |
| Framingham Risk Score > 20 (%) | 9.1 | 22.0 | 42.7 | 44.4 | <0.001 |
| Status | N | Number of Deaths | Number of Deaths Per 100,000 Person-Years (95% CI) | Incidence Rate Ratio (95% CI) | Age- and Sex-Adjusted HR (95% CI) | Multivariable Adjusted HR (95% CI) a |
|---|---|---|---|---|---|---|
| All-Cause Mortality | ||||||
| Normal | 10,921 | 266 | 330.91 (293.95–373.90) | 1 | 1 | 1 |
| Untreateda | 1484 | 120 | 1130.62 (948.31–1357.02) | 1.15 (0.93–1.41) | 1.12 (0.90–1.40) | 1.14 (0.92–1.44) |
| Treated & Controlled | 1066 | 136 | 1818.09 (1543.14–2155.81) | 1.22 (0.99–1.50) | 1.24 (1.00–1.54) | 1.16 (0.93–1.45) |
| Treated & Uncontrolled | 966 | 163 | 2370.35 (2041.49–2766.27) | 1.48 (1.22–1.79) | 1.44 (1.17–1.78) | 1.32 (1.06–1.65) |
| Cardiovascular Mortality | ||||||
| Normal | 10,921 | 62 | 77.13 (60.50–99.92) | 1 | 1 | 1 |
| Untreated | 1484 | 35 | 329.59 (239.15–467.35) | 1.25 (0.82–1.91) | 1.23 (0.80–1.87) | 1.27 (0.83–1.95) |
| Treated & Controlled | 1066 | 53 | 708.52 (546.03–936.19) | 1.79 (1.23–2.63) | 1.73 (1.18–2.53) | 1.57 (1.06–2.32) |
| Treated & Uncontrolled | 966 | 75 | 1090.652 (875.62–1375.43) | 2.42 (1.69–3.48) | 2.30 (1.61–3.30) | 2.11 (1.46–3.06) |
| Heart Disease Mortality | ||||||
| Normal | 10,921 | 47 | 58.46 (44.27–78.89) | 1 | 1 | 1 |
| Untreated | 1484 | 25 | 235.42 (161.16–358.10) | 1.21 (0.74–1.98) | 1.18 (0.72–1.94) | 1.21 (0.74–1.99) |
| Treated & Controlled | 1066 | 35 | 467.89 (339.76–662.72) | 1.61 (1.03–2.55) | 1.55 (0.99–2.45) | 1.39 (0.88–2.23) |
| Treated & Uncontrolled | 966 | 58 | 843.43 (657.26–1100.21) | 2.56 (1.69–3.87) | 2.43 (1.61–3.68) | 2.24 (1.46–3.43) |
| Coronary Heart Disease Mortality | ||||||
| Normal | 10,921 | 31 | 38.57 (27.41–56.06) | 1 | 1 | 1 |
| Untreated | 1484 | 20 | 188.34 (123.34–302.65) | 1.21 (0.74–1.98) | 1.57 (0.88–2.79) | 1.57 (0.87–2.83) |
| Treated & Controlled | 1066 | 19 | 253.99 (164.62–413.46) | 1.61 (1.02–2.54) | 1.43 (0.79–2.59) | 1.27 (0.68–2.35) |
| Treated & Uncontrolled | 966 | 40 | 581.68 (430.95–804.48) | 2.56 (1.70–3.87) | 2.92 (1.76–4.86) | 2.66 (1.56–4.53) |
| Mortality Status * | ||||
|---|---|---|---|---|
| All-Cause Mortality | Cardiovascular Mortality | Heart Disease Mortality | Coronary Heart Disease Mortality | |
| Systolic Blood Pressure | ||||
| 120< | 1.02 (0.83–1.24) | 0.94 (0.65–1.35) | 0.90 (0.60–1.35) | 0.97 (0.59–1.57) |
| ≥120 | 1.07 (1.02–1.12) | 1.06 (0.98–1.14) | 1.12 (1.10–1.14) | 1.18 (1.06–1.31) |
| Diastolic Blood Pressure | ||||
| <80 | 1.04 (0.84–1.28) | 1.10 (0.73–1.68) | 1.05 (0.66–1.71) | 0.91 (0.51–1.59) |
| ≥80 | 1.15 (1.03–1.29) | 1.15 (0.96–1.39) | 1.31 (1.07–1.61) | 1.46 (1.17–1.84) |
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2023 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Sozmen, K.; Ergor, G.; Sakarya, S.; Dinc Horasan, G.; Sahan, C.; Ekinci, B.; Arikan, A.; Sis, S.; Unal, B. Evaluation of Blood Pressure Status and Mortality in Turkey: Findings from Chronic Diseases and Risk Factors Cohort Study. Medicina 2023, 59, 1366. https://doi.org/10.3390/medicina59081366
Sozmen K, Ergor G, Sakarya S, Dinc Horasan G, Sahan C, Ekinci B, Arikan A, Sis S, Unal B. Evaluation of Blood Pressure Status and Mortality in Turkey: Findings from Chronic Diseases and Risk Factors Cohort Study. Medicina. 2023; 59(8):1366. https://doi.org/10.3390/medicina59081366
Chicago/Turabian StyleSozmen, Kaan, Gul Ergor, Sibel Sakarya, Gonul Dinc Horasan, Ceyda Sahan, Banu Ekinci, Ahmet Arikan, Secil Sis, and Belgin Unal. 2023. "Evaluation of Blood Pressure Status and Mortality in Turkey: Findings from Chronic Diseases and Risk Factors Cohort Study" Medicina 59, no. 8: 1366. https://doi.org/10.3390/medicina59081366





