The Attitude of Egyptian Patients with Autoimmune and Rheumatic Diseases towards Telemedicine
Abstract
:1. Introduction
2. Materials and Methods
2.1. Study Design and Settings
2.2. Ethical Consideration
2.3. Sample Size and Sampling Procedure
2.4. Survey
2.5. Survey Administration
2.6. Variables Recorded
2.7. Statistical Analysis
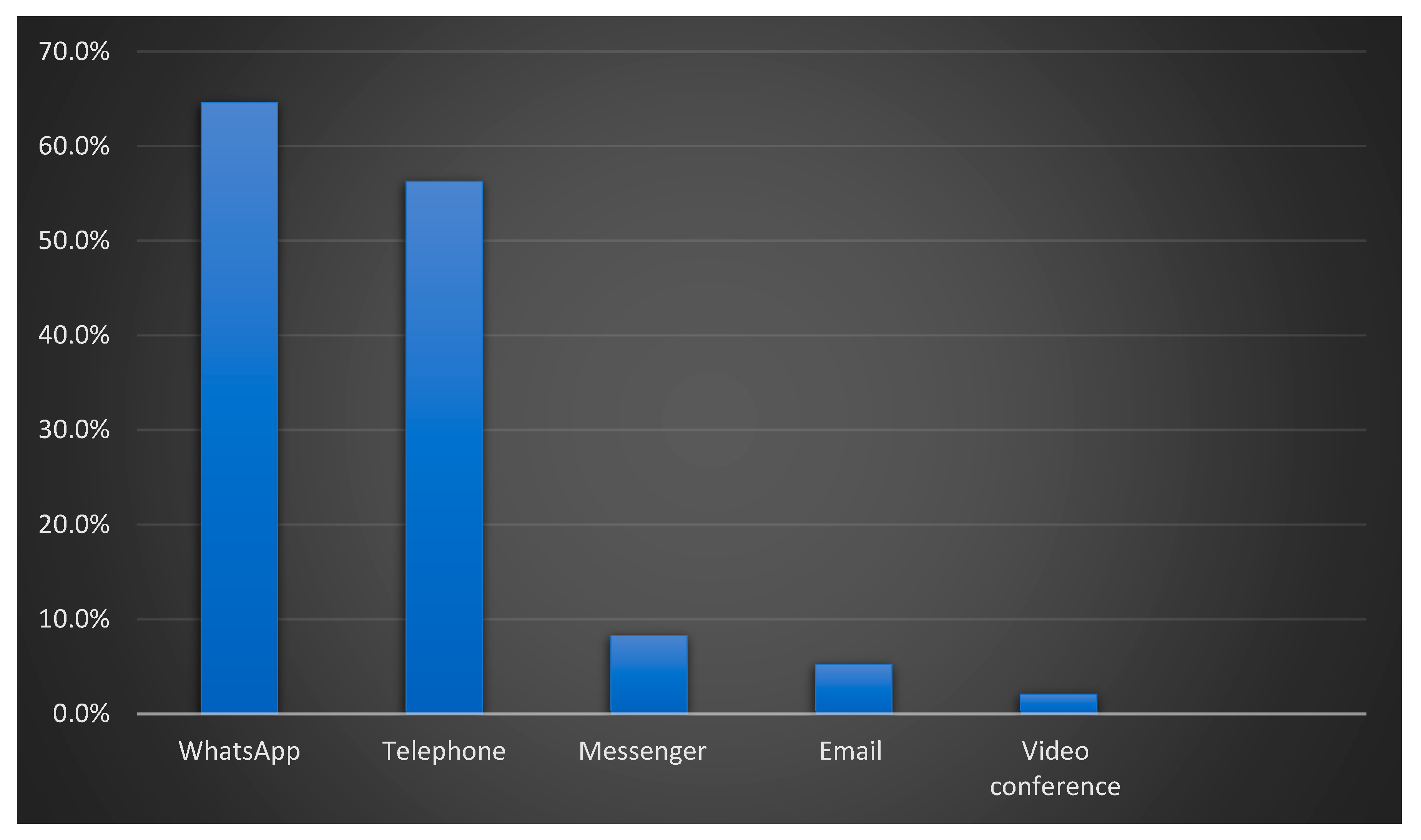
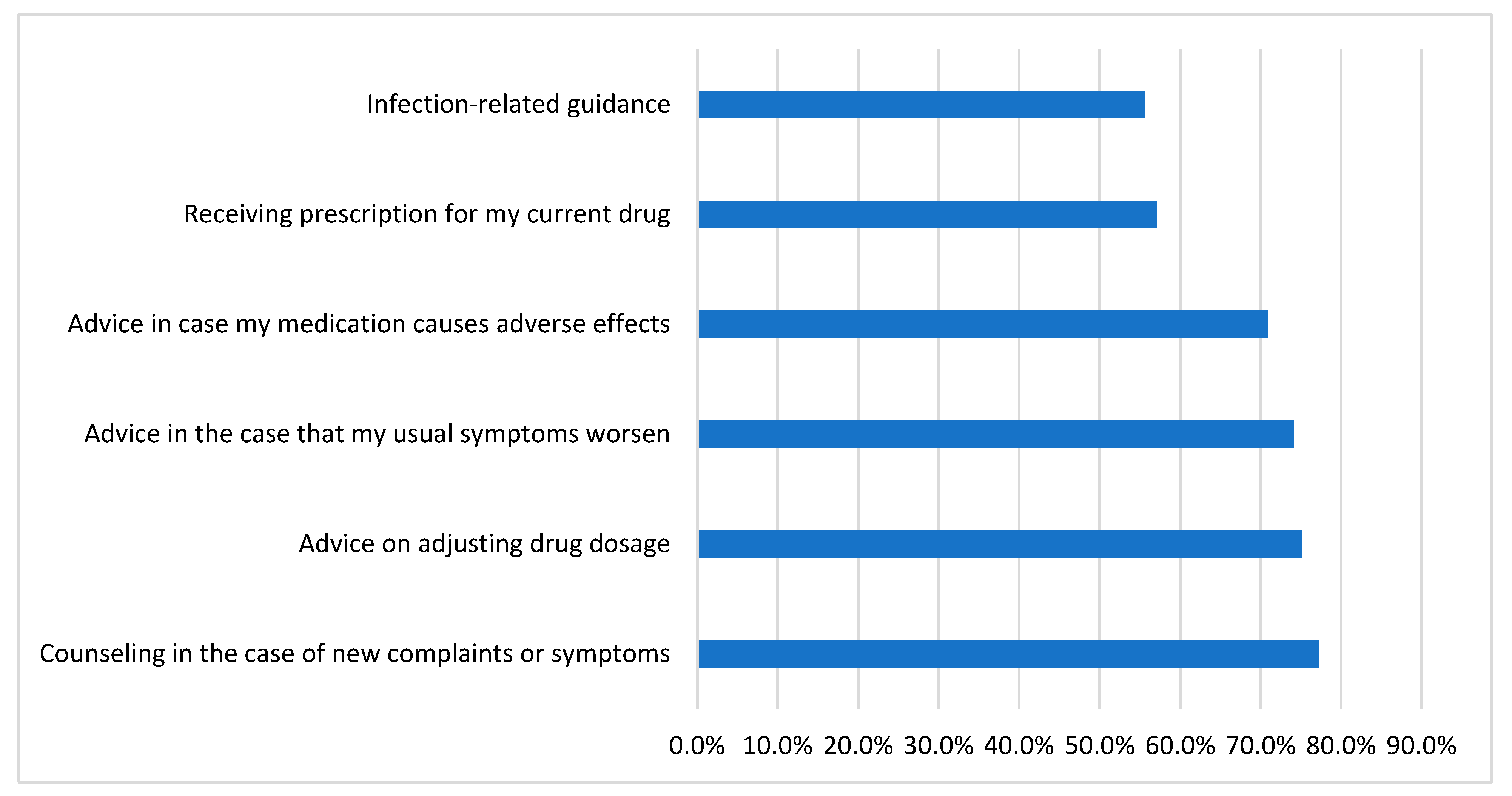
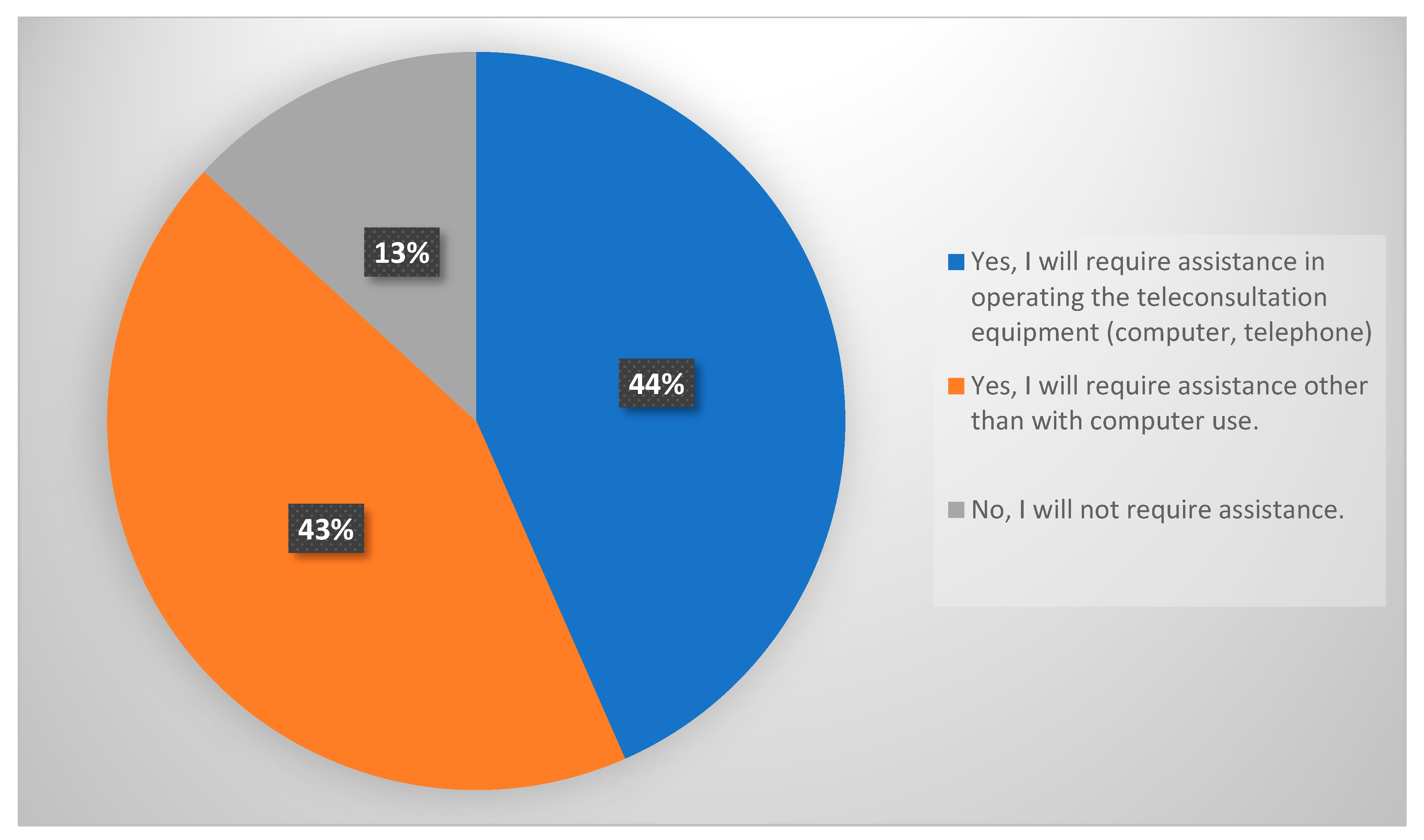
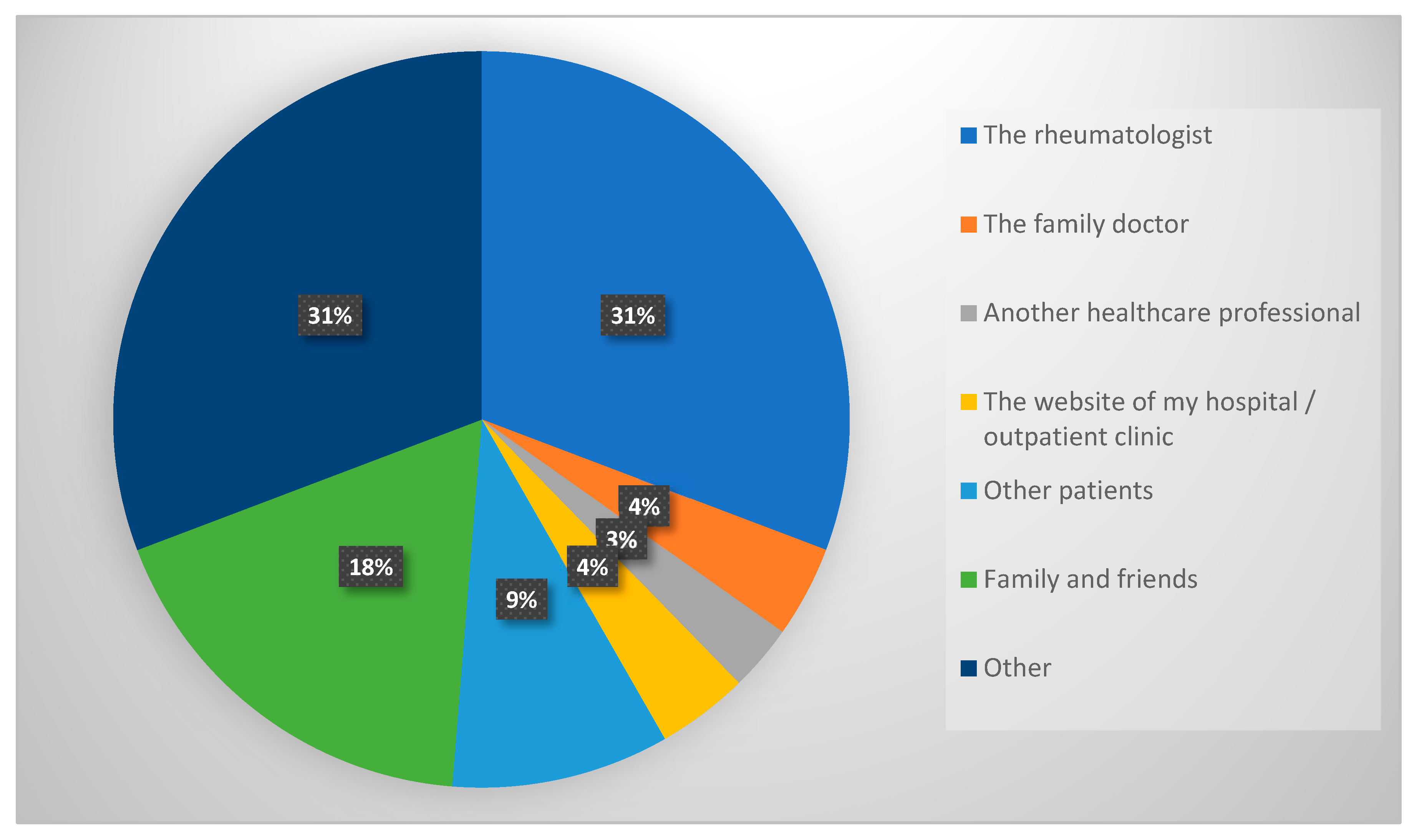
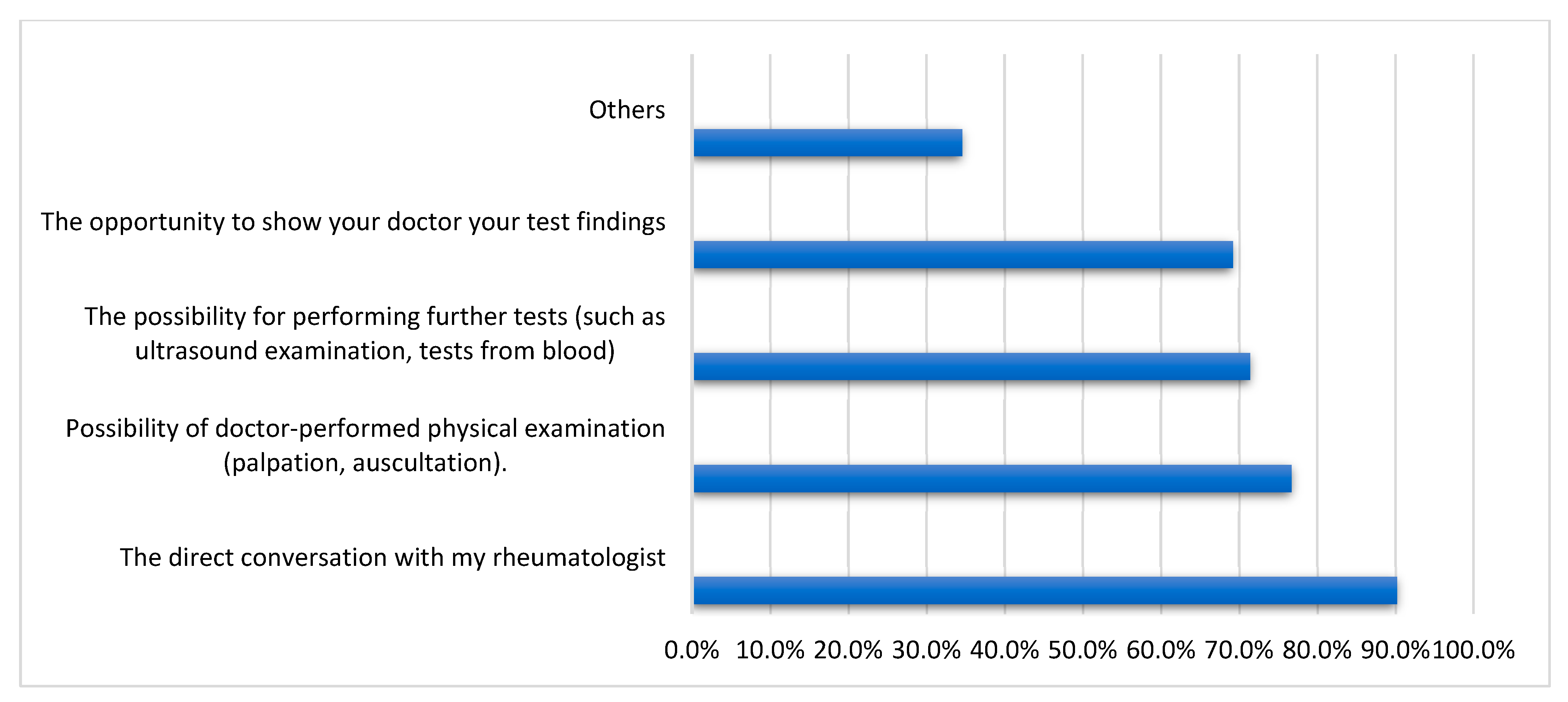
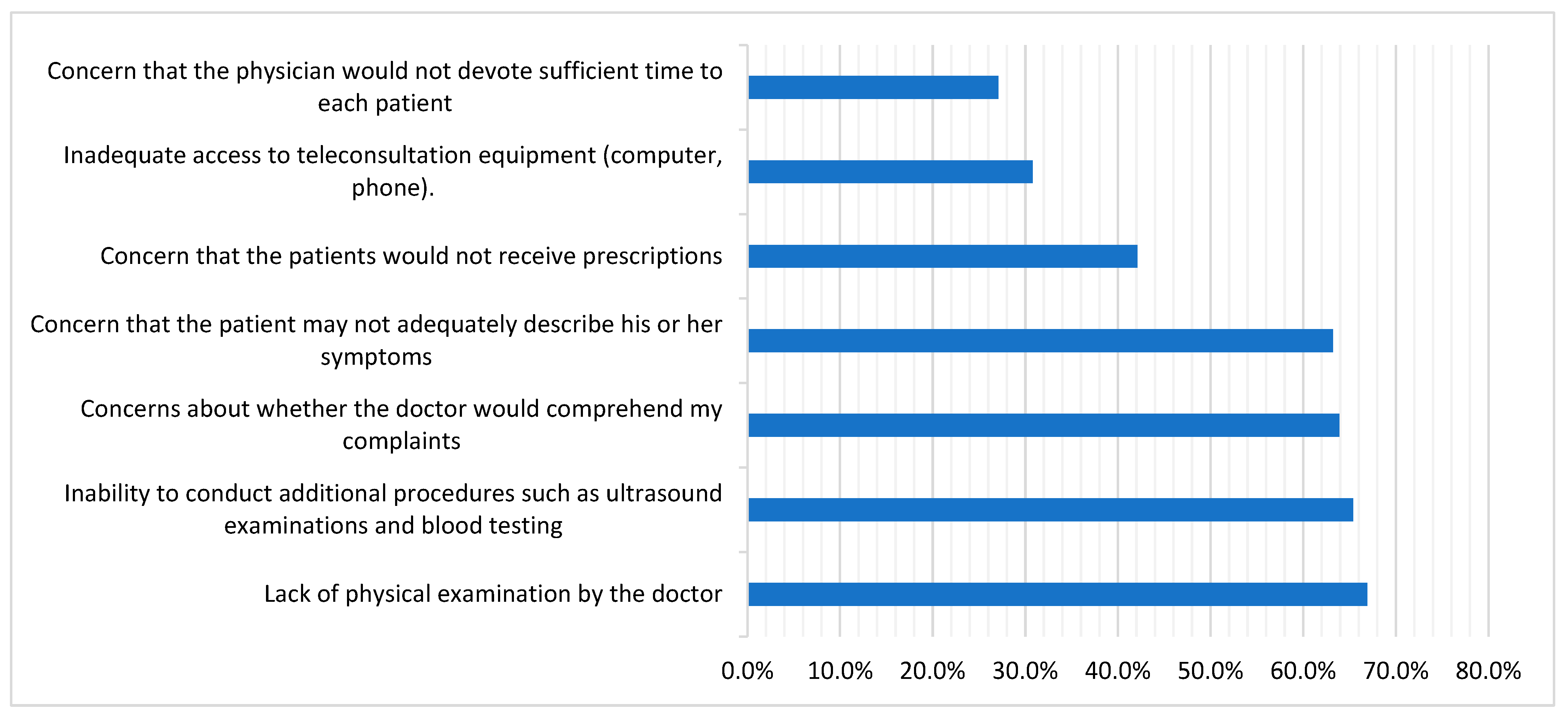
3. Results
4. Discussion
5. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Conflicts of Interest
Abbreviations
| ARDs | autoimmune and rheumatic diseases |
| COVID-19 | coronavirus disease 2019 |
| EULAR | European Alliance of Associations for Rheumatology |
| OA | osteoarthritis |
| OPC | outpatient clinic |
| RA | rheumatoid arthritis |
| SLE | systemic lupus erythematosus |
| TM | telemedicine |
| WHO | World Health Organization |
References
- Cucinotta, D.; Vanelli, M. WHO Declares COVID-19 a Pandemic. Acta Biomed. 2020, 91, 157–160. [Google Scholar] [CrossRef]
- Nicola, M.; Alsafi, Z.; Sohrabi, C.; Kerwan, A.; Al-Jabir, A.; Iosifidis, C.; Agha, M.; Agha, R. The socio-economic implications of the coronavirus pandemic (COVID-19): A review. Int. J. Surg. 2020, 78, 185–193. [Google Scholar] [CrossRef]
- Hartnett, K.P.; Kite-Powell, A.; DeVies, J.; Coletta, M.A.; Boehmer, T.K.; Adjemian, J.; Gundlapalli, A.V.; National Syndromic Surveillance Program Community of Practice. Impact of the COVID-19 Pandemic on Emergency Department Visits—United States, January 1, 2019–May 30, 2020. MMWR Morb. Mortal. Wkly. Rep. 2020, 69, 699–704. [Google Scholar] [CrossRef]
- Emanuel, E.J.; Persad, G.; Upshur, R.; Thome, B.; Parker, M.; Glickman, A.; Zhang, C.; Boyle, C.; Smith, M.; Phillips, J.P. Fair Allocation of Scarce Medical Resources in the Time of COVID-19. N. Engl. J. Med. 2020, 382, 2049–2055. [Google Scholar] [CrossRef]
- Tharwat, S.; Mohamed, S.Z.; Nassar, M.K. Challenges of Egyptian patients with systemic lupus erythematosus during the COVID-19 pandemic. Reumatologia 2021, 59, 237–243. [Google Scholar] [CrossRef]
- Garfan, S.; Alamoodi, A.H.; Zaidan, B.B.; Al-Zobbi, M.; Hamid, R.A.; Alwan, J.K.; Ahmaro, I.Y.Y.; Khalid, E.T.; Jumaah, F.M.; Albahri, O.S.; et al. Telehealth utilization during the Covid-19 pandemic: A systematic review. Comput. Biol. Med. 2021, 138, 104878. [Google Scholar] [CrossRef]
- Danila, M.I.; Gavigan, K.; Rivera, E.; Nowell, W.B.; George, M.D.; Curtis, J.R.; Christopher-Stein, L.; Banerjee, S.; Merkel, P.A.; Young, K.; et al. Patient Perceptions and Preferences Regarding Telemedicine for Autoimmune Rheumatic Diseases Care During the COVID-19 Pandemic. Arthritis Care Res. 2022, 74, 1049–1057. [Google Scholar] [CrossRef]
- Ahmed, S.; Grainger, R.; Santosa, A.; Adnan, A.; Alnaqbi, K.A.; Chen, Y.-H.; Kavadichanda, C.; Kaw, N.S.K.; Kelly, A.; Khan, S.E.A.; et al. APLAR recommendations on the practice of telemedicine in rheumatology. Int. J. Rheum. Dis. 2022, 25, 247–258. [Google Scholar] [CrossRef]
- Friedman, A.B.; Gervasi, S.; Song, H.; Bond, A.M.; Chen, A.T.; Bergman, A.; David, G.; Bailey, J.M.; Brooks, R.; Smith-McLallen, A. Telemedicine catches on: Changes in the utilization of telemedicine services during the COVID-19 pandemic. Am. J. Manag. Care 2022, 28, e1–e6. [Google Scholar] [CrossRef] [PubMed]
- Mehraeen, E.; SeyedAlinaghi, S.; Heydari, M.; Karimi, A.; Mahdavi, A.; Mashoufi, M.; Sarmad, A.; Mirghaderi, P.; Shamsabadi, A.; Qaderi, K.; et al. Telemedicine technologies and applications in the era of COVID-19 pandemic: A systematic review. Health Inform. J. 2023, 29, 14604582231167432. [Google Scholar] [CrossRef]
- Michel, J.; Schmid, S.; Aebersold, E.R.; Mettler, A.; Sauter, T.C. Did the pandemic influence telehealth use among Swiss emergency department patients? A sequential explanatory study. BMJ Open 2023, 13, e070046. [Google Scholar] [CrossRef] [PubMed]
- Cavagna, L.; Zanframundo, G.; Codullo, V.; Pisu, M.G.; Caporali, R.; Montecucco, C. Telemedicine in rheumatology: A reliable approach beyond the pandemic. Rheumatology 2021, 60, 366–370. [Google Scholar] [CrossRef]
- Schulze-Koops, H.; Specker, C.; Krueger, K. Telemedicine holds many promises but needs to be developed to be accepted by patients as an alternative to a visit to the doctor. Response to:‘Patient acceptance of using telemedicine for follow-up of lupus nephritis in the COVID-19 outbreak’by So et al. Ann. Rheum. Dis. 2020, 80, e97. [Google Scholar]
- Maheswaranathan, M.; Miller, B.; Ung, N.; Sinha, R.; Harrison, C.; Egeli, B.H.; Degirmenci, H.B.; Sirotich, E.; Liew, J.W.; Grainger, R.; et al. Patient perspectives on telemedicine use in rheumatology during the COVID-19 pandemic: Survey results from the COVID-19 Global Rheumatology Alliance. Clin. Rheumatol. 2023, 1–10. [Google Scholar] [CrossRef]
- Gierek, M.; Kitala, D.; Łabuś, W.; Glik, J.; Szyluk, K.; Pietrauszka, K.; Bergler-Czop, B.; Niemiec, P. The Impact of Telemedicine on Patients with Hidradenitis Suppurativa in the COVID-19 Era. Healthcare 2023, 11, 1453. [Google Scholar] [CrossRef] [PubMed]
- Muehlensiepen, F.; Knitza, J.; Marquardt, W.; May, S.; Krusche, M.; Hueber, A.; Schwarz, J.; Vuillerme, N.; Heinze, M.; Welcker, M. Opportunities and Barriers of Telemedicine in Rheumatology: A Participatory, Mixed-Methods Study. Int. J. Environ. Res. Public Health 2021, 18, 13127. [Google Scholar] [CrossRef]
- de Thurah, A.; Marques, A.; de Souza, S.; Crowson, C.S.; Myasoedova, E. Future challenges in rheumatology—Is telemedicine the solution? Ther. Adv. Musculoskelet. Dis. 2022, 14, 1759720X221081638. [Google Scholar] [CrossRef]
- Kataria, S.; Ravindran, V. Digital health: A new dimension in rheumatology patient care. Rheumatol. Int. 2018, 38, 1949–1957. [Google Scholar] [CrossRef]
- Alboraie, M.; Allam, M.A.; Youssef, N.; Abdalgaber, M.; El-Raey, F.; Abdeen, N.; Mahdy, R.E.; Elshaarawy, O.; Elgebaly, A.; Haydara, T.; et al. Knowledge, Applicability, and Barriers of Telemedicine in Egypt: A National Survey. Int. J. Telemed. Appl. 2021, 2021, e5565652. [Google Scholar] [CrossRef]
- General Assembly of the World Medical Association World Medical Association Declaration of Helsinki: Ethical principles for medical research involving human subjects. J. Am. Coll. Dent. 2014, 81, 14–18.
- Piga, M.; Cangemi, I.; Mathieu, A.; Cauli, A. Telemedicine for patients with rheumatic diseases: Systematic review and proposal for research agenda. Semin. Arthritis Rheum. 2017, 47, 121–128. [Google Scholar] [CrossRef]
- Ward, I.M.; Schmidt, T.W.; Lappan, C.; Battafarano, D.F. How Critical is Tele-Medicine to the Rheumatology Workforce? Arthritis Care Res. 2016, 68, 1387–1389. [Google Scholar] [CrossRef]
- Devadula, S.; Langbecker, D.; Vecchio, P.; Tesiram, J.; Meiklejohn, J.; Benham, H. Tele-Rheumatology to Regional Hospital Outpatient Clinics: Patient Perspectives on a New Model of Care. Telemed. J. e-Health 2020, 26, 912–919. [Google Scholar] [CrossRef]
- Sloan, M.; Lever, E.; Harwood, R.; Gordon, C.; Wincup, C.; Blane, M.; Brimicombe, J.; Lanyon, P.; Howard, P.; Sutton, S.; et al. Telemedicine in rheumatology: A mixed methods study exploring acceptability, preferences and experiences among patients and clinicians. Rheumatology 2022, 61, 2262–2274. [Google Scholar] [CrossRef]
- Tornero-Molina, J.; Sánchez-Alonso, F.; Fernández-Prada, M.; Bris-Ochaita, M.-L.; Sifuentes-Giraldo, A.; Vidal-Fuentes, J. Tele-Rheumatology during the COVID-19 pandemic. Reumatol. Clin. (Engl. Ed.) 2022, 18, 157–163. [Google Scholar] [CrossRef] [PubMed]
- Montag, C.; Błaszkiewicz, K.; Sariyska, R.; Lachmann, B.; Andone, I.; Trendafilov, B.; Eibes, M.; Markowetz, A. Smartphone usage in the 21st century: Who is active on WhatsApp? BMC Res. Notes 2015, 8, 331. [Google Scholar] [CrossRef] [PubMed]
- Servadei, F.; Zaed, I. Editorial. The role of telemedicine in countries with limited facilities: Which peculiarities? Neurosurg. Focus 2022, 52, E6. [Google Scholar] [CrossRef] [PubMed]
- Hollander, J.E.; Carr, B.G. Virtually Perfect? Telemedicine for Covid-19. N. Engl. J. Med. 2020, 382, 1679–1681. [Google Scholar] [CrossRef]
- Bozzalla Cassione, E.; Zanframundo, G.; Biglia, A.; Codullo, V.; Montecucco, C.; Cavagna, L. COVID-19 infection in a northern-Italian cohort of systemic lupus erythematosus assessed by telemedicine. Ann. Rheum. Dis. 2020, 79, 1382–1383. [Google Scholar] [CrossRef]
- Zhang, Y.; Wang, J.; Zhao, L.; Xiao, J.; Shi, Z. Online management of rheumatoid arthritis during COVID-19 pandemic. Ann. Rheum. Dis. 2021, 80, e4. [Google Scholar] [CrossRef]
- McDougall, J.A.; Ferucci, E.D.; Glover, J.; Fraenkel, L. Telerheumatology: A Systematic Review. Arthritis Care Res. 2017, 69, 1546–1557. [Google Scholar] [CrossRef]
- MacLean, C.H.; Louie, R.; Leake, B.; McCaffrey, D.F.; Paulus, H.E.; Brook, R.H.; Shekelle, P.G. Quality of care for patients with rheumatoid arthritis. JAMA 2000, 284, 984–992. [Google Scholar] [CrossRef] [PubMed]
- Lacaille, D.; Anis, A.H.; Guh, D.P.; Esdaile, J.M. Gaps in care for rheumatoid arthritis: A population study. Arthritis Rheum. 2005, 53, 241–248. [Google Scholar] [CrossRef]
- Lockwood, M.M.; Wallwork, R.S.; Lima, K.; Dua, A.B.; Seo, P.; Bolster, M.B. Telemedicine in Adult Rheumatology: In Practice and in Training. Arthritis Care Res. 2022, 74, 1227–1233. [Google Scholar] [CrossRef]
- Opinc, A.; Łukasik, Z.; Makowska, J. The attitude of Polish rheumatology patients towards telemedicine in the age of the COVID-19 pandemic. Reumatol./Rheumatol. Suppl. 2021, 2021, 134–141. [Google Scholar] [CrossRef]
- Kulcsar, Z.; Albert, D.; Ercolano, E.; Mecchella, J.N. Telerheumatology: A technology appropriate for virtually all. Semin. Arthritis Rheum. 2016, 46, 380–385. [Google Scholar] [CrossRef] [PubMed]
- Scott Kruse, C.; Karem, P.; Shifflett, K.; Vegi, L.; Ravi, K.; Brooks, M. Evaluating barriers to adopting telemedicine worldwide: A systematic review. J. Telemed. Telecare 2018, 24, 4–12. [Google Scholar] [CrossRef] [PubMed]
- Dorsey, E.R.; Topol, E.J. State of Telehealth. N. Engl. J. Med. 2016, 375, 154–161. [Google Scholar] [CrossRef] [PubMed]
- Russo, J.E.; McCool, R.R.; Davies, L. VA Telemedicine: An Analysis of Cost and Time Savings. Telemed. J. e-Health 2016, 22, 209–215. [Google Scholar] [CrossRef]
- Santos-Moreno, P.; Chavez-Chavez, J.; Hernández-Zambrano, S.M.; Rivera-Triana, D.P.; Castiblanco-Montañez, R.A.; Aza, A.; Buitrago-Garcia, D.; Villarreal, L.; Rojas-Villarraga, A. Experience of telemedicine use in a big cohort of patients with rheumatoid arthritis during COVID-19 pandemic. Ann. Rheum. Dis. 2021, 80, e65. [Google Scholar] [CrossRef]
- Mehrotra, A.; Ray, K.; Brockmeyer, D.M.; Barnett, M.L.; Bender, J.A. Rapidly Converting to “Virtual Practices”: Outpatient Care in the Era of COVID-19. Catalyst 2020, 1. [Google Scholar]
- Bos, W.H.; van Tubergen, A.; Vonkeman, H.E. Telemedicine for patients with rheumatic and musculoskeletal diseases during the COVID-19 pandemic; a positive experience in the Netherlands. Rheumatol. Int. 2021, 41, 565–573. [Google Scholar] [CrossRef] [PubMed]
| Variable Mean ± SD, n (%) | Total (n = 189) | Non-Acceptant Group (n = 133) | Acceptant Group (n = 56) | p |
|---|---|---|---|---|
| Gender | 0.320 | |||
| Female | 167 (88.4) | 115 (86.5) | 52 (92.9) | |
| Male | 22 (11.6) | 18 (13.5) | 4 (7.1) | |
| Age (years) | 37.41 ± 11.71 | 36.77 ± 10.82 | 38.95 ± 13.75 | 0.289 |
| Marital status | 0.755 | |||
| Single | 41 (21.7) | 31 (23.3) | 10 (17.9) | |
| Widow | 7 (3.7) | 5 (3.8) | 2 (3.6) | |
| Divorced | 7 (3.7) | 4 (3.0) | 3 (5.4) | |
| Married | 134 (70.9) | 93 (69.9) | 41 (73.2) | |
| Residence | 0.910 | |||
| Rural | 63 (33.3) | 44 (33.1) | 19 (33.9) | |
| Urban | 126 (66.7) | 89 (66.9) | 37 (66.1) | |
| Socioeconomic status | 0.316 | |||
| Low | 30 (15.9) | 20 (15.0) | 10 (17.9) | |
| Intermediate | 154 (81.5) | 108 (81.2) | 46 (82.1) | |
| High | 5 (2.6) | 5 (3.8) | 0 | |
| Education level | 0.001 * | |||
| No formal education | 13 (6.9) | 4 (3.0) | 9 (16.1) | |
| Primary/secondary school | 7 (3.7) | 2 (1.5) | 5 (8.9) | |
| High School | 48 (25.4) | 38 (28.6) | 10 (17.9) | |
| Graduate | 96 (50.8) | 70 (52.6) | 26 (46.4) | |
| Postgraduate | 25 (13.2) | 19 (14.3) | 6 (10.7) | |
| Employment | 0.501 | |||
| Employed | 66 (34.9) | 50 (37.6) | 16 (28.6) | |
| Retired | 5 (2.6) | 4 (3.0) | 1 (1.8) | |
| Out of work | 98 (51.9) | 67 (50.4) | 31 (55.4) | |
| Still a student | 20 (10.6) | 12 (9.0) | 8 (14.3) | |
| Smoking habit | 0.502 | |||
| Smoker | 7 (3.7) | 6 (4.5) | 1 (1.8) | |
| Former smoker | 7 (3.7) | 4 (3.0) | 3 (5.4) | |
| Never | 175 (92.6) | 123 (92.5) | 52 (92.9) |
| Variable Median (Min–Max) n (%) | Total (n = 189) | Non-Acceptant Group (n = 133) | Acceptant Group (n = 56) | p |
|---|---|---|---|---|
| Diagnosis | 0.304 | |||
| Osteoarthritis | 30 (15.9) | 17 (12.8) | 13 (23.2) | |
| Psoriatic arthritis | 1 (0.5) | 1 (0.8) | 0 | |
| Systemic lupus erythematosus | 39 (20.6) | 33 (24.8) | 6 (10.7) | |
| Rheumatoid arthritis | 45 (23.8) | 29 (21.8) | 16 (28.6) | |
| Sjogren syndrome | 2 (1.1) | 2 (1.5) | 0 | |
| Ankylosing spondylitis | 8 (4.2) | 7 (5.3) | 1 (1.8) | |
| Idiopathic inflammatory myositis | 13 (6.9) | 9 (6.8) | 4 (7.1) | |
| Gout | 5 (2.6) | 3 (2.3) | 2 (3.6) | |
| Systemic sclerosis | 6 (3.2) | 4 (3.0) | 2 (3.6) | |
| Juvenile idiopathic arthritis | 1 (0.5) | 0 | 1 (1.8) | |
| Vasculitis | 2 (1.1) | 1 (0.8) | 1 (1.8) | |
| Others | 37 (19.6) | 27 (20.3) | 10 (17.9) | |
| Disease duration (months) | 48 (1–360) | 48 (1–360) | 38 (2–324) | 0.651 |
| Self-reported disease severity (past week) | 0.306 | |||
| Under control | 12 (6.3) | 6 (4.5) | 6 (10.7) | |
| Mild | 44 (23.3) | 31 (23.3) | 13 (23.2) | |
| Moderate | 88 (46.6) | 61 (45.9) | 27 (48.2) | |
| Severe | 45 (23.8) | 35 (26.3) | 10 (17.9) | |
| Comorbidities | ||||
| Hypertension | 60 (31.7) | 44 (33.1) | 16 (28.6) | 0.543 |
| Lung disease | 30 (15.9) | 22 (16.5) | 8 (14.3) | 0.698 |
| Diabetes mellitus | 18 (9.5) | 14 (10.5) | 4 (7.1) | 0.469 |
| Kidney disease | 21 (11.1) | 20 (15.0) | 1 (1.8) | 0.008 * |
| Heart disease | 19 (10.1) | 18 (13.5) | 1 (1.8) | 0.014 * |
| Malignancy | 3 (1.6) | 3 (2.3) | 0 | - |
| Medications | ||||
| Corticosteroids | 98 (51.9) | 72 (54.1) | 26 (46.4) | 0.333 |
| csDMARDs | ||||
| Methotrexate | 45 (23.8) | 30 (22.6) | 15 (26.8) | 0.533 |
| Hydroxychloroquine | 93 (49.2) | 72 (54.1) | 21 (37.5) | 0.037 * |
| Mycophenolate mofetil | 30 (15.9) | 22 (16.5) | 8 (14.3) | 0.698 |
| Leflunomide | 37 (19.6) | 26 (19.5) | 11 (19.6) | 0.988 |
| Biologic or targeted DMARDs | ||||
| TNF-alpha inhibitors | 17 (9.0) | 14 (10.5) | 3 (5.4) | 0.404 |
| Interleukin-6 inhibitors | 5 (2.6) | 3 (2.3) | 2 (3.6) | 0.634 |
| Rituximab | 9 (4.8) | 7 (5.3) | 2 (3.6) | 1 |
| Interleukin-17 inhibitors | 8 (4.2) | 6 (4.5) | 2 (3.6) | 1 |
| Interleukin-1 inhibitors | 2 (1.1) | 1 (0.8) | 1 (1.8) | 0.506 |
| JAK inhibitors | 3 (1.6) | 2 (1.5) | 1 (1.8) | 1 |
| Others | 122 (64.6) | 87 (65.4) | 35 (62.5) | 0.702 |
| Variable Mean ± SD, Median (Min–Max) n (%) | Total (n = 189) | Non-Acceptant Group (n = 133) | Acceptant Group (n = 56) | p |
|---|---|---|---|---|
| Distance from the outpatient clinic | 0.461 | |||
| Living in the same province | 16 (8.5) | 13 (9.8) | 3 (5.4) | |
| In another province within the same region | 20 (10.6) | 16 (12.0) | 4 (7.1) | |
| Living in another region | 148 (78.3) | 100 (75.2) | 48 (85.7) | |
| Being accompanied to the hospital | 5 (2.6) | 4 (3.0) | 1 (1.8) | |
| Frequency of visits to rheumatologist in the last year | 0.227 | |||
| Every < 4 months | 105 (55.6) | 72 (54.1) | 33 (58.9) | |
| Every 4–6 months | 34 (18.0) | 28 (21.1) | 6 (10.7) | |
| Every > 6 months | 50 (26.5) | 33 (24.8) | 17 (30.4) | |
| Exemption from insurance copayments | 0.940 | |||
| Complete | 38 (20.1) | 27 (20.3) | 11 (19.6) | |
| Partial | 31 (16.4) | 21 (15.8) | 10 (17.9) | |
| No exemption | 120 (63.5) | 85 (63.9) | 35 (62.5) | |
| Prior infection with COVID-19 | 96 (50.8) | 72 (54.1) | 24 (42.9) | 0.157 |
| Virtual rheumatology appointment during the COVID-19 pandemic | 96 (50.8) | 71 (53.4) | 25 (44.6) | 0.272 |
| Variable | Acceptant Group n (%) |
|---|---|
| Walking difficulties | 43 (76.8) |
| Transport options to the rheumatology outpatient clinic are limited | 41 (73.2) |
| Fear of becoming infected | 41 (73.2) |
| Too long of a wait for an appointment | 43 (76.8) |
| The potential for reducing wait times for outpatient clinic appointments | 47 (83.9) |
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2023 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Tharwat, S.; Gamal, D. The Attitude of Egyptian Patients with Autoimmune and Rheumatic Diseases towards Telemedicine. Medicina 2023, 59, 1595. https://doi.org/10.3390/medicina59091595
Tharwat S, Gamal D. The Attitude of Egyptian Patients with Autoimmune and Rheumatic Diseases towards Telemedicine. Medicina. 2023; 59(9):1595. https://doi.org/10.3390/medicina59091595
Chicago/Turabian StyleTharwat, Samar, and Doaa Gamal. 2023. "The Attitude of Egyptian Patients with Autoimmune and Rheumatic Diseases towards Telemedicine" Medicina 59, no. 9: 1595. https://doi.org/10.3390/medicina59091595





