COVID-19 Infection Was Associated with the Functional Outcomes of Hip Fracture among Older Adults during the COVID-19 Pandemic Apex
Abstract
:1. Introduction
2. Materials and Methods
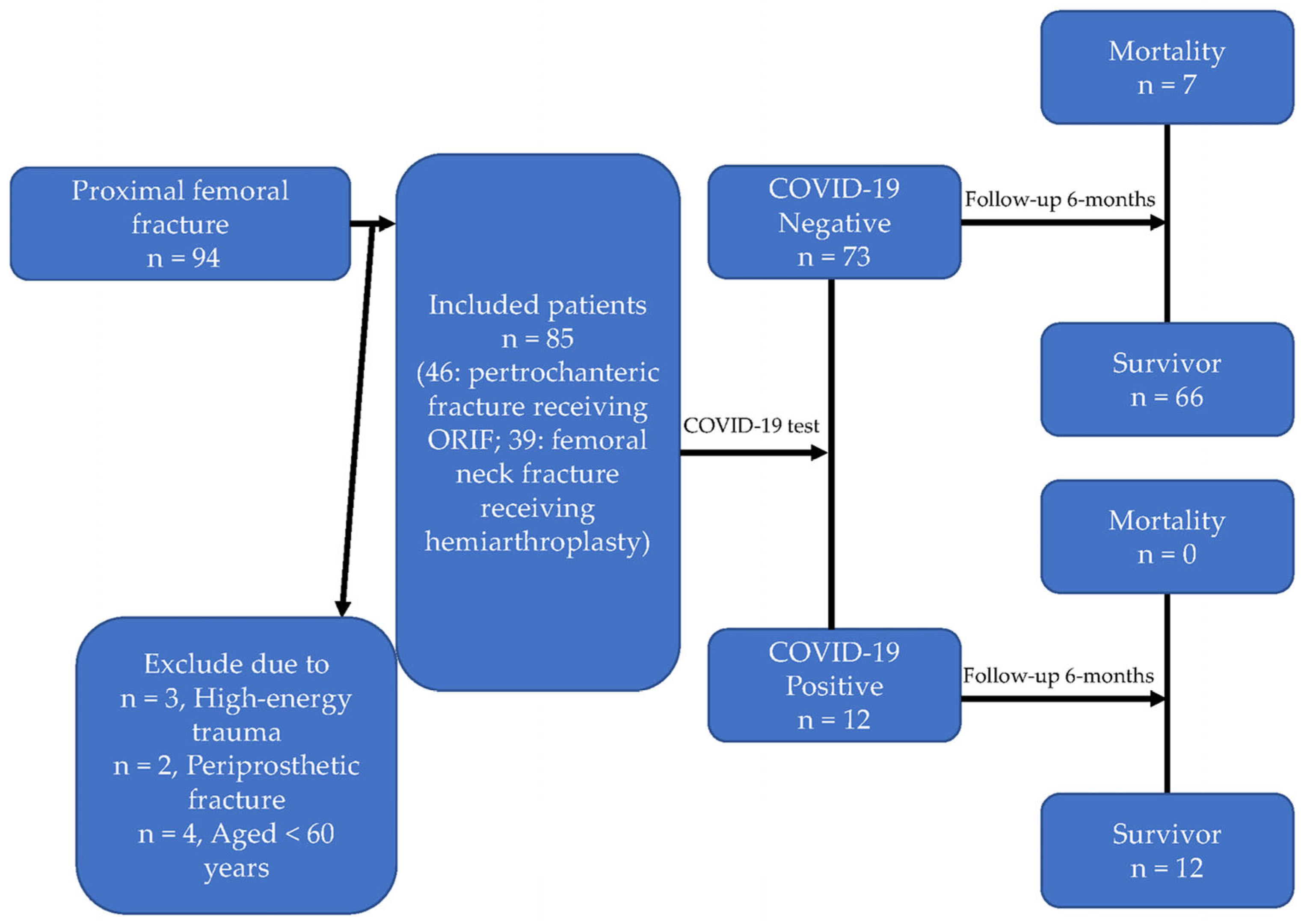
2.1. Study Design and Population
2.2. Data Collection
2.3. Statistical Analysis
3. Results
4. Discussion
5. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Conflicts of Interest
References
- Cooper, C.; Campion, G.; Melton, L.J., 3rd. Hip fractures in the elderly: A world-wide projection. Osteoporos. Int. 1992, 2, 285–289. [Google Scholar] [CrossRef] [PubMed]
- Gullberg, B.; Johnell, O.; Kanis, J.A. World-wide projections for hip fracture. Osteoporos. Int. 1997, 7, 407–413. [Google Scholar] [CrossRef] [PubMed]
- Leibson, C.L.; Tosteson, A.N.; Gabriel, S.E.; Ransom, J.E.; Melton, L.J. Mortality, disability, and nursing home use for persons with and without hip fracture: A population-based study. J. Am. Geriatr. Soc. 2002, 50, 1644–1650. [Google Scholar] [CrossRef] [PubMed]
- Magaziner, J.; Lydick, E.; Hawkes, W.; Fox, K.M.; Zimmerman, S.I.; Epstein, R.S.; Hebel, J.R. Excess mortality attributable to hip fracture in white women aged 70 years and older. Am. J. Public Health 1997, 87, 1630–1636. [Google Scholar] [CrossRef] [PubMed]
- Riggs, B.L.; Melton, L.J., 3rd. The worldwide problem of osteoporosis: Insights afforded by epidemiology. Bone 1995, 17 (Suppl. S5), 505S–511S. [Google Scholar] [CrossRef]
- Magaziner, J.; Simonsick, E.M.; Kashner, T.M.; Hebel, J.R.; Kenzora, J.E. Predictors of functional recovery one year following hospital discharge for hip fracture: A prospective study. J. Gerontol. 1990, 45, M101–M107. [Google Scholar] [CrossRef]
- Cheng, S.C.; Chang, Y.C.; Fan Chiang, Y.L.; Chien, Y.C.; Cheng, M.; Yang, C.H.; Huang, C.H.; Hsu, Y.N. First case of Coronavirus Disease 2019 (COVID-19) pneumonia in Taiwan. J. Formos. Med. Assoc. 2020, 119, 747–751. [Google Scholar] [CrossRef]
- Wang, K.C.; Xiao, R.; Cheung, Z.B.; Barbera, J.P.; Forsh, D.A. Early mortality after hip fracture surgery in COVID-19 patients: A systematic review and meta-analysis. J. Orthop. 2020, 22, 584–591. [Google Scholar] [CrossRef]
- Moldovan, F.; Gligor, A.; Moldovan, L.; Bataga, T. An Investigation for Future Practice of Elective Hip and Knee Arthroplasties during COVID-19 in Romania. Medicina 2023, 59, 314. [Google Scholar] [CrossRef]
- Zhong, H.; Poeran, J.; Liu, J.; Wilson, L.A.; Memtsoudis, S.G. Hip fracture characteristics and outcomes during COVID-19: A large retrospective national database review. Br. J. Anaesth. 2021, 127, 15–22. [Google Scholar] [CrossRef]
- Kim, K.K.; Lee, S.W.; Choi, J.K.; Won, Y.Y. Epidemiology and postoperative complications of hip fracture during COVID-19 pandemic. Osteoporos. Sarcopenia 2022, 8, 17–23. [Google Scholar] [CrossRef] [PubMed]
- Tayyebi, H.; Hasanikhah, M.; Heidarikhoo, M.; Fakoor, S.; Aminian, A. Length of hospital stay and mortality of hip fracture surgery in patients with Coronavirus disease 2019 (COVID-19) infection: A systematic review and meta-analysis. Curr. Orthop. Pract. 2022, 33, 172–177. [Google Scholar] [CrossRef] [PubMed]
- Isla, A.; Landy, D.; Teasdall, R.; Mittwede, P.; Albano, A.; Tornetta, P., 3rd; Bhandari, M.; Aneja, A. Postoperative mortality in the COVID-positive hip fracture patient, a systematic review and meta-analysis. Eur. J. Orthop. Surg. Traumatol. 2023, 33, 927–935. [Google Scholar] [CrossRef]
- Mastan, S.; Hodhody, G.; Sajid, M.; Malik, R.; Charalambous, C.P. COVID-19 Is Associated With a 4-Fold Increase in 30-day Mortality Risk in Hip Fracture Patients in the United Kingdom: A Systematic Review and Meta-Analysis. Geriatr. Orthop. Surg. Rehabil. 2022, 13, 21514593221099375. [Google Scholar] [CrossRef] [PubMed]
- Raheman, F.J.; Rojoa, D.M.; Nayan Parekh, J.; Berber, R.; Ashford, R. Meta-analysis and metaregression of risk factors associated with mortality in hip fracture patients during the COVID-19 pandemic. Sci. Rep. 2021, 11, 10157. [Google Scholar] [CrossRef]
- Parker, M.; Johansen, A. Hip fracture. BMJ 2006, 333, 27–30. [Google Scholar] [CrossRef]
- Mak, J.C.; Cameron, I.D.; March, L.M.; National Health and Medical Research Council. Evidence-based guidelines for the management of hip fractures in older persons: An update. Med. J. Aust. 2010, 192, 37–41. [Google Scholar] [CrossRef]
- Ftouh, S.; Morga, A.; Swift, C.; Guideline Development Group. Management of hip fracture in adults: Summary of NICE guidance. BMJ 2011, 342, d3304. [Google Scholar] [CrossRef]
- Swierstra, B.A.; Vervest, A.M.; Walenkamp, G.H.; Schreurs, B.W.; Spierings, P.T.; Heyligers, I.C.; van Susante, J.L.; Ettema, H.B.; Jansen, M.J.; Hennis, P.J.; et al. Dutch guideline on total hip prosthesis. Acta. Orthop. 2011, 82, 567–576. [Google Scholar] [CrossRef]
- Kristensen, M.T.; Bandholm, T.; Bencke, J.; Ekdahl, C.; Kehlet, H. Knee-extension strength, postural control and function are related to fracture type and thigh edema in patients with hip fracture. Clin. Biomech. 2009, 24, 218–224. [Google Scholar] [CrossRef]
- Lamb, S.E.; Morse, R.E.; Evans, J.G. Mobility after proximal femoral fracture: The relevance of leg extensor power, postural sway and other factors. Age Ageing. 1995, 24, 308–314. [Google Scholar] [CrossRef] [PubMed]
- Sherrington, C.; Lord, S.R.; Herbert, R.D. A randomised trial of weight-bearing versus non-weight-bearing exercise for improving physical ability in inpatients after hip fracture. Aust. J. Physiother. 2003, 49, 15–22. [Google Scholar] [CrossRef] [PubMed]
- Kronborg, L.; Bandholm, T.; Palm, H.; Kehlet, H.; Kristensen, M.T. Feasibility of progressive strength training implemented in the acute ward after hip fracture surgery. PLoS ONE 2014, 9, e93332. [Google Scholar] [CrossRef] [PubMed]
- Rizkalla, J.M.; Gladnick, B.P.; Bhimani, A.A.; Wood, D.S.; Kitziger, K.J.; Peters, P.C., Jr. Triaging Total Hip Arthroplasty during the COVID-19 Pandemic. Curr. Rev. Musculoskelet. Med. 2020, 13, 416–424. [Google Scholar] [CrossRef]
- Teo, S.H.; Abd Rahim, M.R.; Nizlan, N.M. The impact of COVID-19 pandemic on orthopaedic specialty in Malaysia: A cross-sectional survey. J. Orthop. Surg. 2020, 28, 2309499020938877. [Google Scholar] [CrossRef] [PubMed]
- Moldovan, F.; Gligor, A.; Moldovan, L.; Bataga, T. The Impact of the COVID-19 Pandemic on the Orthopedic Residents: A Pan-Romanian Survey. Int. J. Environ. Res. Public Health. 2022, 19, 9176. [Google Scholar] [CrossRef] [PubMed]
- Shih, C.L.; Huang, P.J.; Huang, H.T.; Chen, C.H.; Lee, T.C.; Hsu, C.H. Impact of the COVID-19 pandemic and its related psychological effect on orthopedic surgeries conducted in different types of hospitals in Taiwan. J. Orthop. Surg. 2021, 29, 2309499021996072. [Google Scholar] [CrossRef]
- Siegmeth, A.W.; Gurusamy, K.; Parker, M.J. Delay to surgery prolongs hospital stay in patients with fractures of the proximal femur. J. Bone Jt. Surg. Br. 2005, 87, 1123–1126. [Google Scholar] [CrossRef]
- Qin, H.C.; He, Z.; Luo, Z.W.; Zhu, Y.L. Management of hip fracture in COVID-19 infected patients. World J. Orthop. 2022, 13, 544–554. [Google Scholar] [CrossRef]
- Shin, S.; Kim, S.H.; Park, K.K.; Kim, S.J.; Bae, J.C.; Choi, Y.S. Effects of Anesthesia Techniques on Outcomes after Hip Fracture Surgery in Elderly Patients: A Prospective, Randomized, Controlled Trial. J. Clin. Med. 2020, 9, 1605. [Google Scholar] [CrossRef]
- Liu, Y.; Yang, Y.; Liu, H.; Wu, W.; Wu, X.; Wang, T. A systematic review and meta-analysis of fall incidence and risk factors in elderly patients after total joint arthroplasty. Medicine 2020, 99, e23664. [Google Scholar] [CrossRef] [PubMed]
- Hwang, T.J.; Rabheru, K.; Peisah, C.; Reichman, W.; Ikeda, M. Loneliness and social isolation during the COVID-19 pandemic. Int. Psychogeriatr. 2020, 32, 1217–1220. [Google Scholar] [CrossRef] [PubMed]
- Obamiro, E.; Trivedi, R.; Ahmed, N. Changes in trends of orthopedic services due to the COVID-19 pandemic: A review. World J. Orthop. 2022, 13, 955–968. [Google Scholar] [CrossRef] [PubMed]
- Berggren, M.; Karlsson, Å.; Lindelöf, N.; Englund, U.; Olofsson, B.; Nordström, P.; Gustafson, Y.; Stenvall, M. Effects of geriatric interdisciplinary home rehabilitation on complications and readmissions after hip fracture: A randomized controlled trial. Clin. Rehabil. 2019, 33, 64–73. [Google Scholar] [CrossRef]
- Markotegi, M.; Irazusta, J.; Sanz, B.; Rodriguez-Larrad, A. Effect of the COVID-19 pandemic on the physical and psychoaffective health of older adults in a physical exercise program. Exp. Gerontol. 2021, 155, 111580. [Google Scholar] [CrossRef]
- Sykes, D.L.; Holdsworth, L.; Jawad, N.; Gunasekera, P.; Morice, A.H.; Crooks, M.G. Post-COVID-19 Symptom Burden: What Is Long-COVID and How Should We Manage It? Lung 2021, 199, 113–119. [Google Scholar] [CrossRef]
- Dryden, M.; Mudara, C.; Vika, C.; Blumberg, L.; Mayet, N.; Cohen, C.; Tempia, S.; Parker, A.; Nel, J.; Perumal, R.; et al. Post-COVID-19 condition 3 months after hospitalisation with SARS-CoV-2 in South Africa: A prospective cohort study. Lancet Glob. Health 2022, 10, e1247–e1256. [Google Scholar] [CrossRef]
- Risbridger, S.; Walker, R.; Gray, W.K.; Kamaruzzaman, S.B.; Ai-Vyrn, C.; Hairi, N.N.; Khoo, P.L.; Pin, T.M. Social Participation’s Association with Falls and Frailty in Malaysia: A Cross-Sectional Study. J. Frailty Aging 2022, 11, 199–205. [Google Scholar] [CrossRef]
- Clemente-Suárez, V.J.; Martínez-González, M.B.; Benitez-Agudelo, J.C.; Navarro-Jiménez, E.; Beltran-Velasco, A.I.; Ruisoto, P.; Diaz Arroyo, E.; Laborde-Cárdenas, C.C.; Tornero-Aguilera, J.F. The Impact of the COVID-19 Pandemic on Mental Disorders. A Critical Review. Int. J. Environ. Res. Public Health 2021, 18, 10041. [Google Scholar] [CrossRef]
| Variable | COVID-19 Infection | Total | p | |
|---|---|---|---|---|
| Negative | Positive | |||
| N | 73 | 12 | 85 | |
| Age | 79.18 ± 9.43 | 80.92 ± 10.44 | 79.42 ± 9.53 | 0.561 |
| Body mass index (kg/m2) | 22.42 ± 3.76 | 23.54 ± 3.48 | 22.58 ± 3.72 | 0.339 |
| Gender | - | - | - | 0.051 |
| Male | 28 (38.4%) | 1 (8.3%) | 29 (34.1%) | |
| Female | 45 (61.6%) | 11 (91.7%) | 56 (65.9%) | |
| ASA physical status classification | - | - | - | 0.755 |
| 1 | 7 (9.6%) | 0 (0.0%) | 7 (8.2%) | |
| 2 | 25 (34.2%) | 4 (33.3%) | 29 (34.1%) | |
| 3 | 31 (42.5%) | 7 (58.3%) | 38 (44.7%) | |
| 4 | 10 (13.7%) | 1 (8.3%) | 11 (12.9%) | |
| Fracture type | - | - | - | 0.119 |
| Pertrochanteric | 31 (42.5%) | 8 (66.7%) | 39 (45.9%) | |
| Femoral neck fracture | 42 (57.5%) | 4 (33.3%) | 46 (54.1%) | |
| Preoperative blood test | ||||
| Hemoglobin (g/dL) | 11.34 ± 2.12 | 10.86 ± 2.50 | 11.27 ± 2.17 | 0.478 |
| Platelet (×103/uL) | 205.21 ± 64.4 | 218.83 ± 88.46 | 207.13 ± 67.85 | 0.522 |
| PT (s) | 11.10 ± 2.22 | 10.96 ± 0.63 | 11.08 ± 2.07 | 0.822 |
| aPTT (s) | 26.65 ± 4.26 | 28.97 ± 3.99 | 26.98 ± 4.27 | 0.082 |
| INR | 1.07 ± 0.22 | 1.07 ± 0.06 | 1.07 ± 0.21 | 0.949 |
| ALT (U/L) | 22.01 ± 18.43 | 28.83 ± 36.49 | 22.98 ± 21.71 | 0.316 |
| BUN (mg/dL) | 27.86 ± 21.61 | 16.67 ± 6.97 | 26.28 ± 20.55 | 0.080 |
| Creatinine (mg/dL) | 1.32 ± 1.39 | 0.75 ± 0.19 | 1.24 ± 1.30 | 0.164 |
| Na (mmol/L) | 137.16 ± 4.37 | 135.92 ± 6.73 | 136.71 ± 4.86 | 0.055 |
| K (mmol/L) | 5.76 ± 15.70 | 3.92 ± 0.63 | 5.50 ± 14.55 | 0.687 |
| Charlson comorbidity index | 5.26 ± 2.04 | 4.92 ± 1.93 | 5.21 ± 2.02 | 0.588 |
| Comorbidity number | 1.81 ± 1.25 | 2.25 ± 0.97 | 1.87 ± 1.22 | 0.248 |
| Preoperative Barthel index | 93.01 ± 14.71 | 93.75 ± 11.31 | 93.12 ± 14.23 | 0.869 |
| Variable | COVID-19 Infection | Total | p | |
|---|---|---|---|---|
| Negative | Positive | |||
| Surgical method | - | - | - | 0.119 |
| Hemiarthroplasty | 42 (57.5%) | 4 (33.3%) | 46 (54.1%) | |
| ORIF | 31 (42.5%) | 8 (66.7%) | 39 (45.9%) | |
| Anesthesia method | - | - | - | 1.000 |
| General | 45 (61.6%) | 8 (66.7%) | 53 (62.4%) | |
| Neuroaxial | 28 (38.4%) | 4 (33.3%) | 32 (37.6%) | |
| Perioperative nerve block | 57 (78.1%) | 11 (91.7%) | 68 (80.0%) | 0.445 |
| Preoperative NPO time (h) | 12.18 ± 3.34 | 13.00 ± 3.81 | 12.29 ± 3.40 | 0.441 |
| Time to operation (day) | 1.38 ± 0.49 | 1.58 ± 0.51 | 1.41 ± 0.50 | 0.197 |
| Operation time (min) | 67.34 ± 20.92 | 73.83 ± 22.76 | 68.26 ± 21.17 | 0.328 |
| Anesthesia time (min) | 137.73 ± 32.30 | 158.25 ± 40.24 | 140.62 ± 34.03 | 0.046 |
| Blood loss (mL) | 190.41 ± 135.61 | 245.83 ± 178.96 | 198.24 ± 142.60 | 0.214 |
| Postoperative hemoglobin level (g/dL) | 10.07 ± 1.81 | 9.85 ± 2.03 | 10.04 ± 1.83 | 0.696 |
| Variable | COVID-19 Infection | Total | p | |
|---|---|---|---|---|
| Negative | Positive | |||
| Length of stay (day) | 11.00 ± 9.85 | 11.08 ± 5.16 | 11.01 ± 9.31 | 0.977 |
| Postoperative complication numbers | 1.00 ± 0.91 | 0.92 ± 1.24 | 0.99 ± 0.96 | 0.782 |
| Postoperative ECOG performance status | 1.79 ± 0.83 | 2.00 ± 0.74 | 1.82 ± 0.82 | 0.412 |
| Postoperative Barthel index | 88.03 ± 16.82 | 74.58 ± 17.64 | 85.96 ± 17.53 | 0.014 * |
| Postoperative modified Harrison hip score | 73.42 ± 14.01 | 66.00 ± 11.79 | 72.28 ± 13.89 | 0.089 |
| Mortality | 7 (9.6%) | 0 (0.0%) | 7 (8.2%) | 0.586 |
| Variable | Incidence of Complications | ECOG Status | Bathal Index | HHS | ||||
|---|---|---|---|---|---|---|---|---|
| β (95% CI) | p | β (95% CI) | p | β (95% CI) | p | β (95% CI) | p | |
| Age | 0.004 (−0.021, 0.029) | 0.762 | 0.004 (−0.016, 0.023) | 0.699 | 0.02 (−0.36, 0.40) | 0.906 | −0.09 (−0.46, 0.28) | 0.637 |
| Gender (Male vs. Female) | −0.09 (−0.53, 0.35) | 0.689 | 0.06 (−0.30, 0.42) | 0.732 | −0.16 (−7.19, 6.86) | 0.963 | −3.71 (−10.62, 3.20) | 0.287 |
| COVID-19 infection (Positive vs. Negative) | −0.19 (−0.78, 0.40) | 0.523 | 0.37 (−0.07, 0.82) | 0.098 | −15.59 (−24.29, −6.89) | 0.001 * | −8.20 (−16.75, −0.35) | 0.048 * |
| ASA physical status classification | 0.13 (−0.18, 0.43) | 0.408 | −0.07 (−0.31, 0.17) | 0.567 | 4.62 (−0.10, 9.34) | 0.055 | 1.77 (−2.87, 6.41) | 0.449 |
| Fracture type (Pertrochanteric vs. Femoral neck) | 0.08 (−0.35, 0.51) | 0.725 | 0.04 (−0.30, 0.37) | 0.829 | −3.22 (−9.73, 3.28) | 0.326 | −1.98 (−8.38, 4.41) | 0.538 |
| Anesthesia (General vs. Neuraxial) | 0.50 (0.06, 0.94) | 0.026 * | 0.14 (−0.20, 0.48) | 0.416 | −1.74 (−8.47, 5.00) | 0.608 | −3.95 (−10.57, 2.67) | 0.238 |
| Peripheral Nerve block (Yes vs. No) | 0.11 (−0.40, 0.63) | 0.660 | 0.03 (−0.38, 0.44) | 0.882 | −2.25 (−10.23, 5.72) | 0.575 | −3.06 (−10.89, 4.78) | 0.439 |
| Charlson Comorbidity Index | 0.08 (−0.05, 0.20) | 0.238 | 0.08 (−0.02, 0.18) | 0.099 | −3.30 (−5.18, −1.42) | 0.001 * | −1.78 (−3.62, −0.07) | 0.049 * |
| Preoperative Barthel Index | 0.01 (−0.01, 0.02) | 0.194 | −0.03 (−0.04, −0.02) | <0.001* | 0.65 (0.43, 0.87) | <0.001 * | 0.36 (0.15, 0.58) | 0.001 * |
| Time to operation | −0.02 (−0.46, 0.42) | 0.943 | −0.31 (−0.65, 0.03) | 0.073 | 1.18 (−5.51, 7.87) | 0.726 | 2.29 (−4.29, 8.86) | 0.489 |
| Operation time | −0.004 (−0.014, 0.006) | 0.473 | −0.004 (−0.012, 0.003) | 0.266 | −0.04 (−0.19, 0.12) | 0.651 | −0.03 (−0.18, 0.12) | 0.674 |
| Blood loss | 0.001 (−0.001, 0.002) | 0.411 | −0.001 (−0.002, 0.001) | 0.439 | 0.01 (−0.01, 0.04) | 0.325 | −0.004 (−0.029, 0.021) | 0.726 |
| Length of Stay | 0.04 (0.01, 0.06) | 0.004 * | 0.01 (−0.01, 0.03) | 0.195 | 0.01 (−0.37, 0.39) | 0.958 | 0.00 (−0.37, 0.37) | 0.998 |
| Variable | Crude | Adjusted | ||
|---|---|---|---|---|
| OR (95% CI) | p | OR (95% CI) | p | |
| Age | 1.03 (0.94, 1.12) | 0.533 | 1.25 (1.001, 1.55) | 0.049 * |
| Gender (Male vs. Female) | 14.35 (1.63, 125.94) | 0.016 * | 342.45 (3.56, 32,910.44) | 0.012 * |
| COVID-19 infection (Positive vs. Negative) | 0.00 (NA) | 0.999 | ||
| ASA physical status classification | 2.60 (0.87, 7.74) | 0.086 | 28.96 (1.42, 590.37) | 0.029 * |
| Fracture type (Pertrochanteric vs. Femoral neck) | 0.88 (0.18, 4.17) | 0.867 | 3.48 (0.13, 95.13) | 0.460 |
| Anesthesia (General vs. Neuraxial) | 2.46 × 108 (NA) | 0.998 | ||
| Peripheral nerve block (Yes vs. No) | 0.60 (0.11, 3.37) | 0.558 | 8.88 (0.16, 505.33) | 0.289 |
| Charlson comorbidity index | 0.98 (0.66, 1.45) | 0.924 | 0.22 (0.06, 0.85) | 0.028 * |
| Preoperative Barthel index | 0.99 (0.94, 1.04) | 0.742 | 1.03 (0.91, 1.16) | 0.663 |
| Time to operation | 2.02 (0.42, 9.66) | 0.378 | 0.23 (0.01, 6.44) | 0.390 |
| Operation time | 0.98 (0.94, 1.02) | 0.355 | 0.97 (0.90, 1.05) | 0.486 |
| Blood loss | 1.001 (0.996, 1.006) | 0.672 | 1.01 (0.998, 1.02) | 0.101 |
| Length of stay | 1.04 (0.98, 1.10) | 0.170 | 1.06 (0.93, 1.20) | 0.390 |
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2023 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Tay, H.-Y.; Wu, W.-T.; Peng, C.-H.; Liu, K.-L.; Yu, T.-C.; Chen, I.-H.; Yao, T.-K.; Chang, C.-M.; Chua, J.-Y.; Wang, J.-H.; et al. COVID-19 Infection Was Associated with the Functional Outcomes of Hip Fracture among Older Adults during the COVID-19 Pandemic Apex. Medicina 2023, 59, 1640. https://doi.org/10.3390/medicina59091640
Tay H-Y, Wu W-T, Peng C-H, Liu K-L, Yu T-C, Chen I-H, Yao T-K, Chang C-M, Chua J-Y, Wang J-H, et al. COVID-19 Infection Was Associated with the Functional Outcomes of Hip Fracture among Older Adults during the COVID-19 Pandemic Apex. Medicina. 2023; 59(9):1640. https://doi.org/10.3390/medicina59091640
Chicago/Turabian StyleTay, Hua-Yong, Wen-Tien Wu, Cheng-Huan Peng, Kuan-Lin Liu, Tzai-Chiu Yu, Ing-Ho Chen, Ting-Kuo Yao, Chia-Ming Chang, Jian-Yuan Chua, Jen-Hung Wang, and et al. 2023. "COVID-19 Infection Was Associated with the Functional Outcomes of Hip Fracture among Older Adults during the COVID-19 Pandemic Apex" Medicina 59, no. 9: 1640. https://doi.org/10.3390/medicina59091640
APA StyleTay, H.-Y., Wu, W.-T., Peng, C.-H., Liu, K.-L., Yu, T.-C., Chen, I.-H., Yao, T.-K., Chang, C.-M., Chua, J.-Y., Wang, J.-H., & Yeh, K.-T. (2023). COVID-19 Infection Was Associated with the Functional Outcomes of Hip Fracture among Older Adults during the COVID-19 Pandemic Apex. Medicina, 59(9), 1640. https://doi.org/10.3390/medicina59091640











