Analysis of Cervical Range of Motion in Subjects Affected by Temporomandibular Disorders: A Controlled Study
Abstract
:1. Introduction
2. Materials and Methods
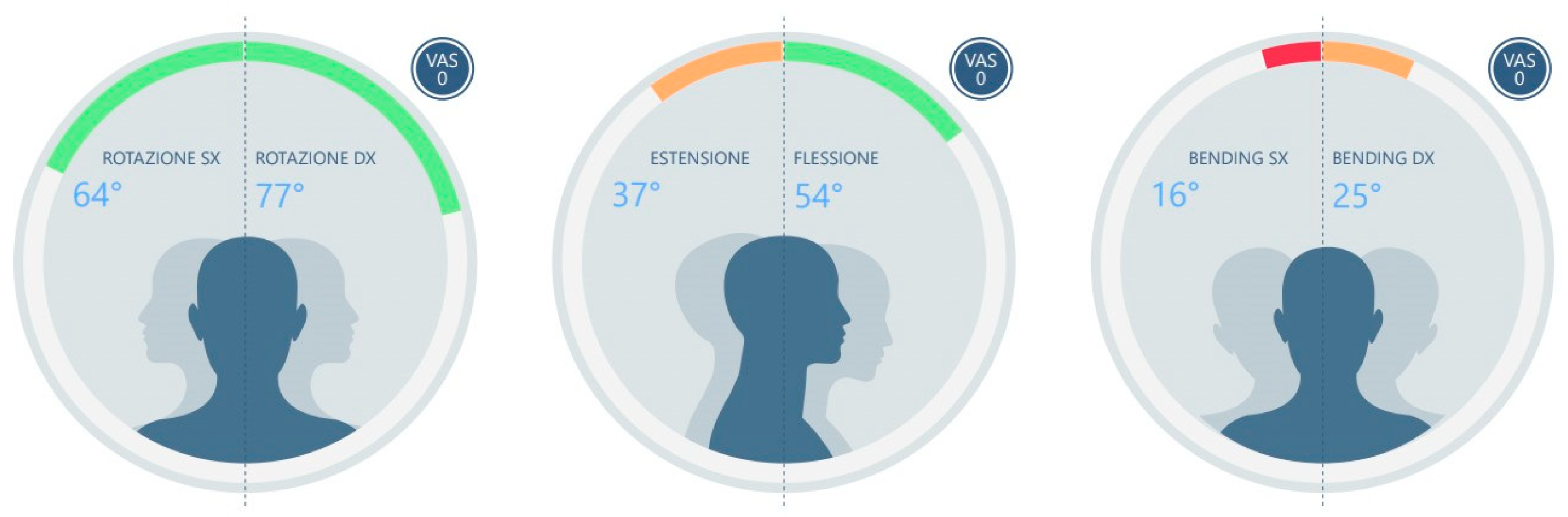
- ROT L (left rotation)
- ROT R (right rotation)
- ASIM ROT (absolute difference between right and left rotation angles)
- EXT (extension)
- FLEX (flexion)
- BEN L (left side bending)
- BEN R (right side bending)
- ASIM BEN (absolute difference between right and left lateral bending angles)
Statistical Analyses
3. Results
4. Discussion
5. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Acknowledgments
Conflicts of Interest
References
- Armijo Olivo, S.L.A. Relationship between Cervical Musculoskeletal Impairments and Temporomandibular Disorders: Clinical and Electromyographic Variables. Ph.D. Thesis, Faculty of Rehabilitation Medicine, Edmonton, AB, Canada, 2010. [Google Scholar]
- Jeon, K.J.; Kim, Y.H.; Ha, E.; Choi, H.S.; Ahn, H.; Lee, G.R.; Hwang, D.; Han, S. Quantitative analysis of the mouth opening movement of temporomandibular joint disorder patients according to disc position using computer vision: A pilot study. Quant. Imaging Med. Surg. 2022, 12, 1909. [Google Scholar] [CrossRef] [PubMed]
- Rauhala, K.; Oikarinen, K.S.; Raustia, A.M. Role of Temporomandibular Disorders (TMD) in Facial Pain: Occlusion, Muscle and TMJ Pain. Cranio J. Craniomandib. Sleep Pract. 1999, 17, 254–261. [Google Scholar] [CrossRef] [PubMed]
- Schiffman, E.; Ohrbach, R.; Truelove, E.; Look, J.; Anderson, G.; Goulet, J.P.; List, T.; Svensson, P.; Gonzalez, Y.; Lobbezoo, F.; et al. Diagnostic Criteria for Temporomandibular Disorders (DC/TMD) for Clinical and Research Applications: Recommendations of the International RDC/TMD Consortium Network* and Orofacial Pain Special Interest Group. J. Oral Facial Pain Headache 2014, 28, 6. [Google Scholar] [CrossRef]
- Valesan, L.F.; Dacas, C.D.; Rèus, J.C.; Denardin, A.C.S.; Garanhaniu, R.R.; Bonotto, D.; Januzzi, E.; De Souza, B.D.M. Prevalence of temporomandibular joint disorders: A systematic review and meta-analysis. Clin. Oral Investig. 2021, 25, 441–453. [Google Scholar] [CrossRef] [PubMed]
- Iodice, G.; Cimino, R.; Vollaro, S.; Lobbezoo, F.; Michelotti, A. Prevalence of temporomandibular disorder pain, jaw noises and oral behaviours in an adult Italian population sample. J. Oral Rehabil. 2019, 46, 691–698. [Google Scholar] [CrossRef] [PubMed]
- Obamiyi, S.; Malik, S.; Wang, Z.; Singh, S.; Rossouw, E.P.; Fishman, L.; Feng, C.; Michelogiannakis, D.; Tallents, R.H. Radiographic features associated with temporomandibular joint disorders among African, White, Chinese, Hispanic, and Indian racial groups. Niger. J. Clin. Pract. 2018, 21, 1495–1500. [Google Scholar] [CrossRef] [PubMed]
- Li, D.T.S.; Leung, Y.Y. Temporomandibular disorders: Current concepts and controversies in diagnosis and management. Diagnostics 2021, 11, 459. [Google Scholar] [CrossRef] [PubMed]
- Almpani, K.; Tran, H.; Ferri, A.; Hung, M. Assessment of condylar anatomy and degenerative changes in temporomandibular joint disorders—A scoping review. J. Oral Biol. Craniofac Res. 2023, 13, 764–780. [Google Scholar] [CrossRef]
- Robertson, C.E.; Benarroch, E.E. The anatomy of head pain. In Handbook of Clinical Neurology; Elsevier: Amsterdam, The Netherlands, 2023; pp. 41–60. [Google Scholar] [CrossRef]
- Barkhordarian, A.; Chiappelli, F.; Demerjian, G.G. Neuroanatomy and neurophysiology of the trigeminal network system. In Temporomandibular Joint and Airway Disorders: A Translational Perspective; Springer: Cham, Switzerland, 2018. [Google Scholar] [CrossRef]
- Vâscu, M.B.; Iordache, C.M.; Antohe, E.; Surlari, Z.; Ancuţa, C.; Fătu, A.M. Research on The Vascular-Nervous Constituents Of The Stomatognathic System and Their Implication in Local Clinical Disfunctions. Rom. J. Funct. Clin. Macro Microsc. Anat. Anthropol. Rev. Româna Anat. Funct. Clin. Macro Microsc. Antropol. 2021, 20, 7–12. [Google Scholar]
- Guo, S.X.; Li, B.Y.; Zhang, Y.; Zhou, L.G.; Liu, L.; Widmalm, S.E.; Wang, M.Q. An electromyographic study on the sequential recruitment of bilateral sternocleidomastoid and masseter muscle activity during gum chewing. J. Oral Rehabil. 2017, 44, 594–601. [Google Scholar] [CrossRef]
- Fuentes, A.D.; Miralles, R.; Santander, H.; Gutiérrez, M.F.; Bull, R.; Martin, C. Effect of natural mediotrusive contact on electromyographic activity of jaw and cervical muscles during chewing. Acta Odontol. Scand. 2015, 73, 626–632. [Google Scholar] [CrossRef] [PubMed]
- Parameswaran, R.; Srimagesh, R.; Parameswaran, A.; Vijayalakshmi, D.R. Evaluating the Plantar Pressure Loading and Its Correlation to Craniocervical Posture in Subjects With Skeletal Class II Malocclusion Before and After Surgical Mandibular Advancement. Cureus 2023, 15, e48250. [Google Scholar] [CrossRef] [PubMed]
- Krishna, S.S.S.; Shashikumar, B.; Naik, R.D. Evaluation and comparison of cervical spine posture in class II division i patients treated with twin block appliances, forsus appliances, and bilateral sagittal split osteotomy: A cephalometric study. Contemp. Clin. Dent. 2023, 14, 157–165. [Google Scholar] [CrossRef] [PubMed]
- Alexa, V.T.; Fratila, A.D.; Szuhanek, C.; Jumanca, D.; Lalescu, D.; Galuscan, A. Cephalometric assessment regarding craniocervical posture in orthodontic patients. Sci. Rep. 2022, 12, 21729. [Google Scholar] [CrossRef] [PubMed]
- Solberg, W.K. Temporomandibular disorders: Physical tests in diagnosis. Br. Dent. J. 1986, 160, 273–277. [Google Scholar] [CrossRef] [PubMed]
- Firestone, A.R. Orofacial Pain: Guidelines for Assessment, Diagnosis, and Management (1996). Jeffrey, P. Okeson (Ed.). Publisher: Quintessence Publishing Co., Inc., Chicago, USA. Price: 22.00. ISBN: 0-86715-312-1. Eur. J. Orthod. 1997, 19, 103–104. [Google Scholar] [CrossRef]
- Grant, R.N.; Mckenzie, R.A. Mechanical diagnosis and therapy for the cervical and thoracic spine. In Physical Therapy of the Cervical and Thoracic Spine; Churchill Livingstone: New York, NY, USA, 1994; pp. 359–377. [Google Scholar]
- Walczyńska-Dragon, K.; Baron, S.; Nitecka-Buchta, A.; Tkacz, E. Correlation between TMD and cervical spine pain and mobility: Is the whole body balance TMJ related? Biomed. Res. Int. 2014, 2014, 582414. [Google Scholar] [CrossRef]
- Chaves, T.C.; Grossi, D.B.; de Oliveira, A.S.; Bertolli, F.; Holtz, A.; Costa, D. Correlation between signs of temporomandibular (TMD) and cervical spine (CSD) disorders in asthmatic children. J. Clin. Pediatr. Dent. 2005, 29, 287–292. [Google Scholar] [CrossRef]
- Wiesinger, B.; Malker, H.; Englund, E.; Wänman, A. Does a dose-response relation exist between spinal pain and temporomandibular disorders? BMC Musculoskelet. Disord. 2009, 10, 28. [Google Scholar] [CrossRef]
- Costa, Y.M.; Conti, P.C.R.; de Faria, F.A.C.; Bonjardim, L.R. Temporomandibular disorders and painful comorbidities: Clinical association and underlying mechanisms. Oral Surg. Oral Med. Oral Pathol. Oral Radiol. 2017, 123, 288–297. [Google Scholar] [CrossRef]
- Walczyńska-Dragon, K.; Baron, S. The biomechanical and functional relationship between temporomandibular dysfunction and cervical spine pain. Acta Bioeng. Biomech. 2011, 13, 93–98. [Google Scholar] [PubMed]
- Silveira, A.; Gadotti, I.C.; Armijo-Olivo, S.; Biasotto-Gonzalez, D.A.; Magee, D. Jaw dysfunction is associated with neck disability and muscle tenderness in subjects with and without chronic temporomandibular disorders. Biomed. Res. Int. 2015, 2015, 512792. [Google Scholar] [CrossRef] [PubMed]
- Grondin, F.; Hall, T.; von Piekartz, H. Does altered mandibular position and dental occlusion influence upper cervical movement: A cross–sectional study in asymptomatic people. Musculoskelet. Sci. Pract. 2017, 27, 85–90. [Google Scholar] [CrossRef] [PubMed]
- Pérez-Fernández, T.; Olivo, S.A.; Lièbana, S.; De la Torre Ortìz, P.J.; Carnero, J.F.; Raya, R.; Zugasti, A.M.-P. A novel use of inertial sensors to measure the craniocervical flexion range of motion associated to the craniocervical flexion test: An observational study. J. Neuroeng. Rehabil. 2020, 17, 152. [Google Scholar] [CrossRef] [PubMed]
- Funakoshi, M.; Fujita, N.; Takehana, S. Relations Between Occlusal Interference and Jaw Muscle Activities in Response to Changes in Head Position. J. Dent. Res. 1976, 55, 684–690. [Google Scholar] [CrossRef] [PubMed]
- Bratzlavsky, M.; Eecken, H.V. Postural reflexes in cranial muscles in man. Acta Neurol. Belg. 1977, 77, 5–11. [Google Scholar] [PubMed]
- Coderre, T.J.; Katz, J.; Vaccarino, A.L.; Melzack, R. Contribution of central neuroplasticity to pathological pain: Review of clinical and experimental evidence. Pain 1993, 52, 259–285. [Google Scholar] [CrossRef]
- Marfurt, C.F. Trigeminal primary afferent projections to, D.M.R. “non-trigeminal” areas of the rat central nervous system. J. Comp. Neurol. 1991, 303, 489–511. [Google Scholar] [CrossRef]
- Al-Abbasi, H.; Mehta, N.R.; Forgione, A.G.; Clark, R.E. The Effect of Vertical Dimension and Mandibular Position on Isometric Strength of the Cervical Flexors. Cranio J. Craniomandib. Sleep Pract. 1999, 17, 85–92. [Google Scholar] [CrossRef]
- Michelotti, A.; Manzo, P.; Farella, M.; Martina, R. Occlusione e postura: Quali le evidenze di correlazione? Minerva Stomatol. 1999, 525, 34. [Google Scholar]
- Strini, P.J.S.A.; Strini, P.J.S.A.; De Souza Barbosa, T.; Gavião, M.B.D. Assessment of thickness and function of masticatory and cervical muscles in adults with and without temporomandibular disorders. Arch. Oral Biol. 2013, 58, 1100–1108. [Google Scholar] [CrossRef] [PubMed]
- Kim, P.; Sarauw, M.T.; Sonnesen, L. Cervical vertebral column morphology and head posture in preorthodontic patients with anterior open bite. Am. J. Orthod. Dentofac. Orthop. 2014, 145, 359–366. [Google Scholar] [CrossRef] [PubMed]
- Vig, P.S.; Rink, J.F.; Showfety, K.J. Adaptation of head posture in response to relocating the center of mass: A pilot study. Am. J. Orthod. 1983, 83, 138–142. [Google Scholar] [CrossRef] [PubMed]
- Baldini, A.; Nota, A.; Tecco, S.; Ballanti, F.; Cozza, P. Influence of the mandibular position on the active cervical range of motion of healthy subjects analyzed using an accelerometer. Cranio J. Craniomandib. Pract. 2018, 36, 29–34. [Google Scholar] [CrossRef] [PubMed]
- Nota, A.; Pittari, L.; Gamba, L.; Monticciolo, F.M.; Lannes, A.; Carta, C.; Beraldi, A.; Baldini, A.; Marzo, G.; Tecco, S. Cervical Range of Motion Analysis Performed with an Accelerometer: A Study of Intersession Reliability for Dental Practice. Healthcare 2023, 11, 1428. [Google Scholar] [CrossRef] [PubMed]
- Tousignant-Laflamme, Y.; Boutin, N.; Dion, A.M.; Vallée, C.A. Reliability and criterion validity of two applications of the iPhoneTM to measure cervical range of motion in healthy participants. J. Neuroeng. Rehabil. 2013, 10, 69. [Google Scholar] [CrossRef] [PubMed]
- Quek, J.; Brauer, S.G.; Treleaven, J.; Pua, Y.H.; Mentiplay, B.; Clark, R.A. Validity and intra-rater reliability of an Android phone application to measure cervical range-of-motion. J. Neuroeng. Rehabil. 2014, 11, 65. [Google Scholar] [CrossRef]
- Nota, A.; Ryakhovsky, A.N.; Bosco, F.; Tecco, S. A full digitalworkflow to design and mill a splint for a patient with temporomandibular joint disorder. Appl. Sci. 2021, 11, 372. [Google Scholar] [CrossRef]
- Tecco, S.; Nota, A.; Pittari, L.; Clerici, C.; Mangano, F.; Gherlone, E.F. Full-Digital Workflow for TMDs Management: A Case Series. Healthcare 2023, 11, 790. [Google Scholar] [CrossRef]
- Grondin, F.; Hall, T.; Laurentjoye, M.; Ella, B. Upper cervical range of motion is impaired in patients with temporomandibular disorders. Cranio J. Craniomandib. Pract. 2015, 33, 9–99. [Google Scholar] [CrossRef]
- Serrao, M.; Cortese, F.; Andersen, O.K.; Conte, C.; Spaich, E.G.; Fragiotta, G.; Ranavolo, A.; Coppola, G.; Perrotta, A.; Pierelli, F. ‘Modular organization of the head retraction responses elicited by electrical painful stimulation of the facial skin in humans. Clin. Neurophysiol. 2015, 126, 2306–2313. [Google Scholar] [CrossRef] [PubMed]
- Yap, A.U.; Kim, S.; Lee, B.; Jo, J.H.; Park, J.W. Correlates of jaw functional limitation, somatization and psychological distress among different temporomandibular disorder diagnostic subtypes. J. Oral Rehabil. 2023; ahead of print. [Google Scholar] [CrossRef] [PubMed]
- Nazzal, H.; Baccar, M.; Ziad, T.; Al-Musfir, T.; Al Emadi, B.; Matoug-Elwerfelli, M.; Narasimhan, S.; Khan, Y.; Reagu, S. Prevalence of anxiety, sleep bruxism and temporomandibular disorders during COVID-19 in Qatari children and adolescents: A cross-sectional study. Eur. Arch. Paediatr. Dent. 2023, 24, 787–795. [Google Scholar] [CrossRef] [PubMed]
- Clark, G.T.; Green, E.M.; Dornan, M.R.; Flack, V.F. Craniocervical dysfunction levels in a patient sample from a temporomandibular joint clinic. J. Am. Dent. Assoc. 1987, 115, 251–256. [Google Scholar] [CrossRef]
- Ciancaglini, R.; Testa, M.; Radaelli, G. Association of neck pain with symptoms of temporomandibular dysfunction in the general adult population. Scand. J. Rehabil. Med. 1999, 31, 17–22. [Google Scholar] [CrossRef]
| Task | Variable | Test Group (TMDs Patients) | Control Group (Healthy Patients) | p-Value |
|---|---|---|---|---|
| T01 (REST) | ROT L | 75.55 ± 11.36 | 75.19 ± 7.17 | 0.451 |
| ROT R | 72.40 ± 11.29 | 74.52 ± 9.31 | 0.260 | |
| ASIM ROT | 6.95 ± 4.43 | 7.26 ± 5.47 | 0.421 | |
| EXT | 45.60 ± 13.90 | 66.17 ± 14.76 | <0.000 Effect size 1.43 | |
| FLE | 61.65 ± 11.25 | 58.30 ± 10.69 | 0.169 | |
| BEN L | 43.30 ± 7.44 | 40.43 ± 7.93 | 0.320 | |
| BEN R | 38.25 ± 7.98 | 43.13 ± 6.67 | 0.021 Effect size 0.66 | |
| ASIM BEN | 7.05 ± 4.70 | 5.74 ± 4.44 | 0.183 | |
| T02 (MAX. INT.) | ROT L | 73.95 ± 10.84 | 75.39 ± 6.69 | 0.309 |
| ROT R | 70.10 ± 10.14 | 73.43 ± 9.60 | 0.144 | |
| ASIM ROT | 6.95 ± 6.34 | 6.65 ± 5.98 | 0.439 | |
| EXT | 49.55 ± 14.02 | 64.17 ± 14.92 | 0.001 Effect size 1.00 | |
| FLE | 60.35 ± 12.61 | 59.22 ± 9.21 | 0.374 | |
| BEN L | 42.65 ± 8.57 | 42.65 ± 7.11 | 0.500 | |
| BEN R | 38.50 ± 8.70 | 40.22 ± 9.06 | 0.270 | |
| ASIM BEN | 6.55 ± 4.99 | 6.78 ± 4.14 | 0.437 | |
| T03 (COTTONS) | ROT L | 75.40 ± 10.89 | 75.04 ± 8.60 | 0.455 |
| ROT R | 70.35 ± 8.77 | 73.74 ± 8.32 | 0.107 | |
| ASIM ROT | 8.45 ± 8.12 | 7.04 ± 4.31 | 0.252 | |
| EXT | 47.45 ± 12.98 | 61.70 ± 17.13 | 0.002 Effect size 0.94 | |
| FLE | 61.60 ± 9.09 | 58.04 ± 11.04 | 0.132 | |
| BEN L | 42.20 ± 7.90 | 42.17 ± 7.08 | 0.496 | |
| BEN R | 37.65 ± 7.95 | 42.04 ± 7.50 | 0.039 Effect size 0.57 | |
| ASIM BEN | 6.65 ± 5.04 | 5.26 ± 4.00 | 0.170 | |
| T04 (CLE. COT.) | ROT L | 76.65 ± 8.84 | 75.35 ± 7.01 | 0.304 |
| ROT R | 70.50 ± 9.29 | 74.96 ± 9.09 | 0.065 | |
| ASIM ROT | 7.65 ± 6.71 | 5.87 ± 4.12 | 0.162 | |
| EXT | 47.95 ± 12.24 | 62.96 ± 14.10 | <0.000 Effect size 1.13 | |
| FLE | 60.85 ± 8.45 | 62.93 ± 9.28 | 0.240 | |
| BEN L | 43.30 ± 6.75 | 42.61 ± 6.40 | 0.370 | |
| BEN R | 37.90 ± 7.96 | 42.00 ± 6.95 | 0.045 Effect size 0.55 | |
| ASIM BEN | 6.60 ± 5.09 | 4.09 ± 4.04 | 0.046 Effect size 0.55 | |
| T05 (CLENCHING) | ROT L | 73.45 ± 9.22 | 75.48 ± 8.48 | 0.235 |
| ROT R | 67.85 ± 9.32 | 74.96 ± 10.84 | 0.015 Effect size 0.70 | |
| ASIM ROT | 7.30 ± 6.44 | 10.17 ± 7.67 | 0.100 | |
| EXT | 49.40 ± 12.65 | 64.83 ± 15.09 | <0.000 Effect size 1.11 | |
| FLE | 56.90 ± 13.60 | 62.22 ± 12.67 | 0.103 | |
| BEN L | 40.10 ± 8.44 | 41.91 ± 7.09 | 0.232 | |
| BEN R | 36.85 ± 7.81 | 41.57 ± 7.20 | 0.026 Effect size 0.63 | |
| ASIM BEN | 6.25 ± 4.70 | 4.43 ± 2.55 | 0.072 |
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2023 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Nota, A.; Pittari, L.; Lannes, A.C.; Vaghi, C.; Calugi Benvenuti, C.; Tecco, S. Analysis of Cervical Range of Motion in Subjects Affected by Temporomandibular Disorders: A Controlled Study. Medicina 2024, 60, 37. https://doi.org/10.3390/medicina60010037
Nota A, Pittari L, Lannes AC, Vaghi C, Calugi Benvenuti C, Tecco S. Analysis of Cervical Range of Motion in Subjects Affected by Temporomandibular Disorders: A Controlled Study. Medicina. 2024; 60(1):37. https://doi.org/10.3390/medicina60010037
Chicago/Turabian StyleNota, Alessandro, Laura Pittari, Alessia Claudia Lannes, Chiara Vaghi, Clarissa Calugi Benvenuti, and Simona Tecco. 2024. "Analysis of Cervical Range of Motion in Subjects Affected by Temporomandibular Disorders: A Controlled Study" Medicina 60, no. 1: 37. https://doi.org/10.3390/medicina60010037
APA StyleNota, A., Pittari, L., Lannes, A. C., Vaghi, C., Calugi Benvenuti, C., & Tecco, S. (2024). Analysis of Cervical Range of Motion in Subjects Affected by Temporomandibular Disorders: A Controlled Study. Medicina, 60(1), 37. https://doi.org/10.3390/medicina60010037








