Virtual Surgical Planning for Temporomandibular Joint Reconstruction with Stock TMJ Prostheses: Pilot Study
Abstract
:1. Introduction
2. Materials and Methods
2.1. Patients
2.2. Preoperative Planning
2.3. Surgical Procedure
2.3.1. Preoperative Management
2.3.2. Surgical Procedure
2.4. Follow-up Visits
3. Results
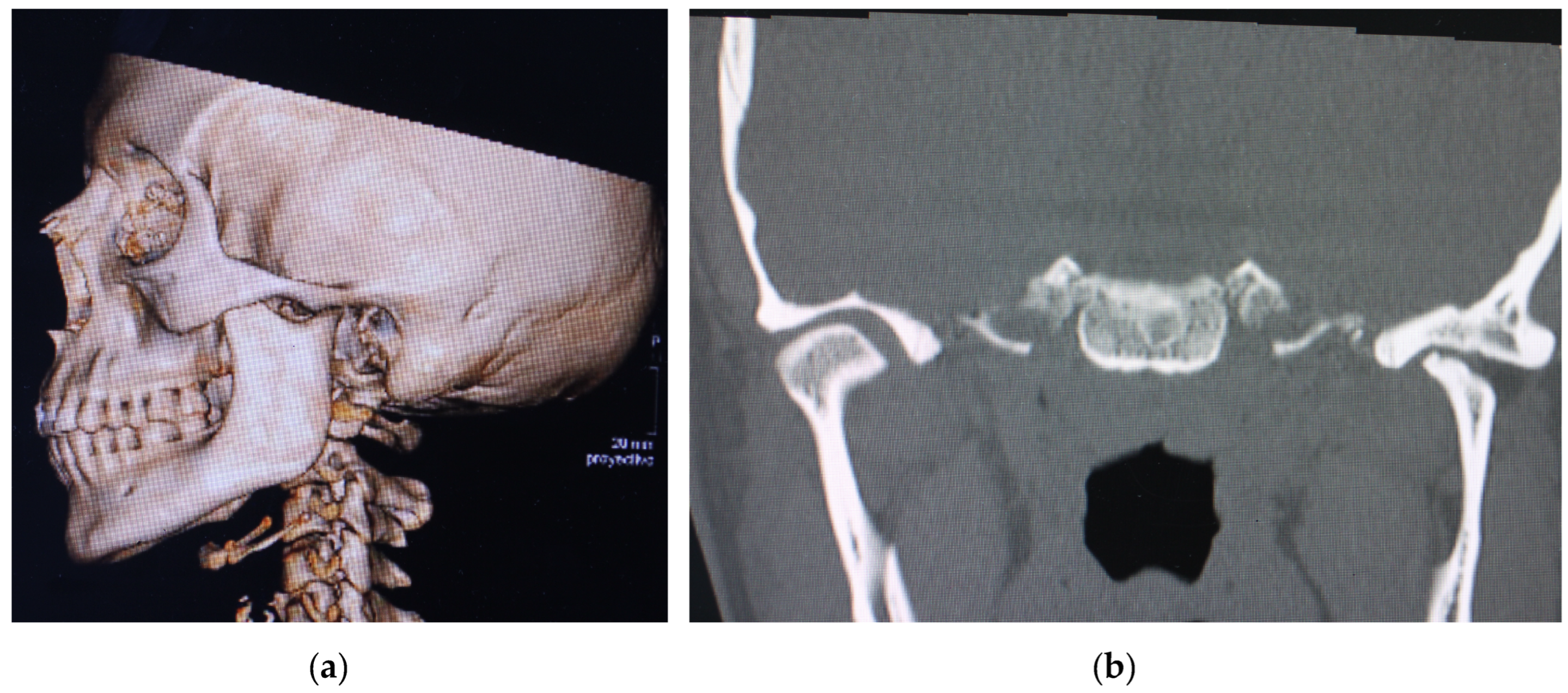
Case Presentation
4. Discussion
5. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Conflicts of Interest
References
- Mercuri, L.G. The use of alloplastic prostheses for temporomandibular joint reconstruction. J. Oral Maxillofac. Surg. 2000, 58, 70–75. [Google Scholar] [CrossRef]
- Wolford, L.; Movahed, R.; Teschke, M.; Fimmers, R.; Havard, D.; Schneiderman, E. Temporomandibular joint ankylosis can be successfully treated with TMJ Concepts patient-fitted total joint prosthesis and autogenous fat grafts. J. Oral Maxillofac. Surg. 2016, 74, 1215–1227. [Google Scholar] [CrossRef]
- Leandro, L.F.; Ono, H.Y.; Loureiro, C.C.; Marinho, K.; Guevara, H.A. A ten-year experience and follow-up of three hundred patients fitted with the Biomet/Lorenz Microfixation TMJ replacement system. Int. J. Oral Maxillofac. Surg. 2013, 42, 1007–1013. [Google Scholar] [CrossRef] [PubMed]
- Wong, R.C.; Tideman, H.; Kin, L.; Merkx, M.A. Biomechanics of mandibular reconstruction: A review. Int. J. Oral Maxillofac. Surg. 2010, 39, 313–319. [Google Scholar] [CrossRef]
- Loveless, T.P.; Bjornland, T.; Dodson, T.B. Efficacy of temporomandibular joint ankylosis surgical treatment. J. Oral Maxillofac. Surg. 2010, 68, 1276–1282. [Google Scholar] [CrossRef] [PubMed]
- Kantanen, D.J.; Closmann, J.J.; Rowshan, H.H. Abdominal fat harvest technique and its uses in maxillofacial surgery. Oral Surg. Oral Med. Oral Pathol. Oral Radiol. Endod. 2010, 109, 367–371. [Google Scholar] [CrossRef] [PubMed]
- Mercuri, L.G.; Giobbie-Hurder, A. Long-term outcomes after total alloplastic temporomandibular joint reconstruction following exposure to failed materials. J. Oral Maxillofac. Surg. 2004, 62, 1088–1096. [Google Scholar] [CrossRef] [PubMed]
- Granquist, E.J.; Quinn, P.D. Total Reconstruction of the Temporomandibular Joint with a Stock Prosthesis. Atlas Oral Maxillofac. Surg. Clin. N. Am. 2011, 19, 221–232. [Google Scholar] [CrossRef]
- Amarista, F.J.; Mercuri, L.G.; Perez, D. Temporomandibular Joint Prosthesis Revision and/or Replacement Survey and Review of the Literature. J. Oral Maxillofac. Surg. 2020, 78, 1692–1703. [Google Scholar] [CrossRef] [PubMed]
- Sembronio, S.; Tel, A.; Costa, F.; Isola, M.; Robiony, M. Accuracy of Custom-Fitted Temporomandibular Joint Alloplastic Reconstruction and Virtual Surgical Planning. Int. J. Oral Maxillofac. Surg. 2019, 48, 1077–1083. [Google Scholar] [CrossRef]
- Amarista, F.J.; Jones, J.P.; Brown, Z.; Rushing, D.C.; Jeske, N.A.; Perez, D.E. Outcomes of Total Joint Alloplastic Reconstruction in TMJ Ankylosis. Oral Surg. Oral Med. Oral Pathol. Oral Radiol. 2022, 134, 135–142. [Google Scholar] [CrossRef] [PubMed]
- Del Castillo, J.L.; Pampín, M.; Guiñales, J.; Rodriguez, J.P.; Cebrián, J.L. Precise modification of surgical and positioning guides for temporomandibular joint prostheses. Br. J. Oral Maxillofac. Surg. 2022, 60, 855–858. [Google Scholar] [CrossRef]
- Guarda-Nardini, L.; Manfredini, D.; Ferronato, G. Temporomandibular joint total replacement prosthesis: Current knowledge and considerations for the future. Int. J. Oral Maxillofac. Surg. 2008, 37, 103–110. [Google Scholar] [CrossRef] [PubMed]
- Dela Coleta, K.E.; Wolford, L.M.; Gonçalves, J.R.; Pinto Ados, S.; Pinto, L.P.; Cassano, D.S. Maxillo-mandibular counter-clockwise rotation and mandibular advancement with TMJ Concepts total joint pro- stheses: Part Ieskeletal and dental stability. Int. J. Oral Maxillofac. Surg. 2009, 38, 126–138. [Google Scholar] [CrossRef] [PubMed]
- Gerbino, G.; Zavattero, E.; Bosco, G.; Berrone, S.; Ramieri, G. Temporomandibular joint reconstruction with stock and custom-made devices: Indications and results of a 14-year experience. J. Craniomaxillofac. Surg. 2017, 45, 1710–1715. [Google Scholar] [CrossRef]
- van Loon, J.P.; de Bont, L.G.M.; Boering, G. Evaluation of temporomandibular joint prostheses: Review of the literature from 1946 to 1994 and implications for the future prosthesis designs. J. Oral Maxillofac. Surg. 1995, 53, 984–996. [Google Scholar] [CrossRef]
- Westermark, A. Total reconstruction of the temporomandibular joint. Up to 8 years of follow-up of patients treated with Biomet (®) total joint prostheses. Int. J. Oral Maxillofac. Surg. 2010, 39, 951–955. [Google Scholar] [CrossRef]
- Mercuri, L.G. Subjective and objective outcomes in patients reconstructed with a custom-fitted alloplastic temporomandibular joint prosthesis. J. Oral Maxillofac. Surg. 1999, 57, 1427–1430. [Google Scholar] [CrossRef]
- Wolford, L.M.; Pitta, M.C.; Reiche-Fishel, O.; Franco, P.F. TMJ Concepts/Techmedica custom-made TMJ total joint prosthesis: 5-year follow-up study. Int. J. Oral Maxillofac. Surg. 2003, 32, 268–274. [Google Scholar] [CrossRef]
- Zheng, J.S.; Liu, X.H.; Chen, X.Z.; Jiang, W.B.; Abdelrehem, A.; Zhang, S.Y.; Chen, M.J.; Yang, C. Customized skull basetemporomandibular joint combined prosthesis with 3D-printing fabrication for craniomaxillofacial reconstruction: A preliminary study. Int. J. Oral Maxillofac. Surg. 2019, 48, 1440–1447. [Google Scholar] [CrossRef]
- Salter, R.B. History of rest and motion and the scientific basis for early continuous passive motion. Hand Clin. 1996, 12, 1–11. [Google Scholar] [CrossRef] [PubMed]
- Qudah, M.A.; Qudeimat, M.A.; Al-Maaita, J. Treatment of TMJ ankylosis in Jordanian children-a comparison of two surgical techniques. J. Craniomaxillofac. Surg. 2005, 33, 30–36. [Google Scholar] [CrossRef] [PubMed]
- Aagaard, E.; Thygesen, T. A prospective, single-centre study on patient outcomes following temporomandibular joint replacement using a custom-made Biomet TMJ prosthesis. Int. J. Oral Maxillofac. Surg. 2014, 43, 1229–1235. [Google Scholar] [CrossRef] [PubMed]







| Gender/Age (Years) | Image | MIO Preop (mm) | MIO at 6 Months (mm) | VAS Preop | VAS at 6 Months | Functional Result | Aesthetic Result | Complications |
|---|---|---|---|---|---|---|---|---|
| F/36 |  | 25.9 | 36.4 | 8 | 3 | 2 | 2 | None |
| F/49 |  | 15.6 | 35.4 | 9 | 4 | 2 | 2 | Partial left facial palsy |
| F/68 |  | 30.5 | 40.3 | 8 | 3 | 2 | 2 | None |
| F/42 |  | 26.4 | 33.5 | 7 | 2 | 2 | 2 | None |
| Average | 24.6 | 36.4 | 8 | 3 | 2 | 2 |
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2024 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
del Castillo Pardo de Vera, J.L.; Cebrián Carretero, J.L.; Aragón Niño, Í.; Pampín Martínez, M.M.; Borjas Gómez, J.T.; Navarro Cuéllar, I.; López López, A.M.; Gómez Larren, E.; Navarro Vila, C.; Montes Fernández-Micheltorena, P.; et al. Virtual Surgical Planning for Temporomandibular Joint Reconstruction with Stock TMJ Prostheses: Pilot Study. Medicina 2024, 60, 339. https://doi.org/10.3390/medicina60020339
del Castillo Pardo de Vera JL, Cebrián Carretero JL, Aragón Niño Í, Pampín Martínez MM, Borjas Gómez JT, Navarro Cuéllar I, López López AM, Gómez Larren E, Navarro Vila C, Montes Fernández-Micheltorena P, et al. Virtual Surgical Planning for Temporomandibular Joint Reconstruction with Stock TMJ Prostheses: Pilot Study. Medicina. 2024; 60(2):339. https://doi.org/10.3390/medicina60020339
Chicago/Turabian Styledel Castillo Pardo de Vera, José Luis, José Luis Cebrián Carretero, Íñigo Aragón Niño, Marta María Pampín Martínez, José Tadeo Borjas Gómez, Ignacio Navarro Cuéllar, Ana María López López, Estela Gómez Larren, Carlos Navarro Vila, Pablo Montes Fernández-Micheltorena, and et al. 2024. "Virtual Surgical Planning for Temporomandibular Joint Reconstruction with Stock TMJ Prostheses: Pilot Study" Medicina 60, no. 2: 339. https://doi.org/10.3390/medicina60020339









